Abstract
Pertrochanteric fracture in a group of 41 patients was internally fixed using a DHS with a two-hole side-plate. There were 20 male and 21 female patients with a mean age of 74 years. Thirty-two patients were followed up for more than one year and their final results were evaluated. There were 30 stable (31A1) and only two unstable (31A2) fractures. The average surgical time was 28 minutes, the average length of incision was 5.5 cm. All the patients, with one exception, healed without complications in anatomical position with good function of the hip joint. The only complication was caused by pulling-out of the plate from the femur in the fourth postoperative week when the patient (31A2 fracture) fell out of bed. A DHS with a four-hole side-plate was used at reoperation; subsequently the fracture had healed. Based on the results in this series of patients, the authors recommend fixation of stable pertrochanteric fractures with DHS and a two-hole side-plate. As proven by the authors, the benefit of DHS with a two-hole side-plate as compared to DHS with a four-hole side-plate is a shorter surgical time (28 and 36 minutes, respectively).
Introduction
The dynamic hip screw (DHS) with a four-hole side-plate and four bicortical screws is still considered to be a standard implant for pertrochanteric fractures (AO/ASIF 31A1 + 2) [3, 7, 8, 10, 12–15]. The disadvantage of a four-hole side-plate as compared to a two-hole side-plate, as reported in the literature, is a longer incision, more invasive dissection of soft tissues associated with more intensive bleeding, longer surgical time and greater postoperative pain [1, 4, 6, 9, 16]. All this may also affect the healing of the fracture. These negative effects may be reduced by application of DHS with a two-hole side-plate. In spite of this, the two-hole implant is used only rarely, although the results reported in the literature have been very good [1, 4, 6, 9, 11, 16, 17]. The reason for limited use of the two-hole implant might be a concern of surgeons that a two-hole implant does not provide adequate fixation of the plate to the femoral shaft. The aim of this study was to present experience in using DHS with a two-hole side-plate in a group of 32 patients.
Materials and methods
Patients
Between January 2003 and August 2007, 41 patients with pertrochanteric fractures (AO/ASIF 31A1 + A2) were treated with 135-degree DHS with a two-hole side-plate. The group included 20 male and 21 female patients, with a mean age of 76 years (range, 23–96 years). Patients were operated on by 15 different surgeons.
Thirty-two of these 41 patients, 15 men and 17 women, were followed up for more than one year after the operation. The mean age of this group of patients was 74 years (range, 23 – 94 years); nine patients were younger than 70 years.
Fracture types
Patients with a stable pertrochanteric fracture (31A1) were scheduled for internal fixation with a DHS with a two-hole side-plate and only exceptionally patients with an unstable pertrochanteric fracture (31 A2).
Surgical procedure and postoperative course
A standard procedure was performed with the patient on a radiolucent fracture table. First, closed reduction was performed. Subsequently, a short lateral approach to the proximal femur was done through a longitudinal incision on average 5.5 cm in length extending through the fascia and vastus lateralis of the quadriceps muscle; the fracture was fixed with a 135-degree DHS with a two-hole side-plate (Synthes). The screws fixing the plate to the femoral shaft were in most cases inserted divergently (Fig. 1). The patients were mobilised on the second postoperative day, fully weight-bearing on the operated limb. After discharge from the hospital, the patients were followed up in the clinic at six weeks, three months, six months and one year after the operation; anteroposterior radiographs were obtained at all follow-up visits.
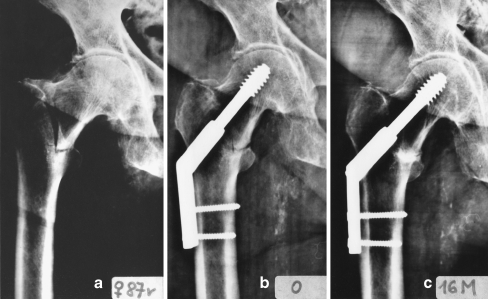
Fig. 1.
Divergent insertion of plate cortical screws. a A 59-year-old male with stable pertrochanteric fracture (31A1). b Internal fixation with 135-degree DHS with a two-hole side-plate; the cortical screws were inserted in divergent fashion. c Healed fracture three months after surgery
Evaluation
The following parameters were analysed:
Type of fracture according to the AO/ASIF classification
Surgical time
X-ray exposure
Length of the sliding screw
Intraoperative complications
Time to heal
Position at healing (varus, valgus, limb shortening)
Postoperative complications
Functional score by Broos et al. [5]
Results
The following parameters were analysed.
Type of fracture
There were 30 fractures of type 31A1 and two fractures of type 31A2.
Length of the sliding screw
The length of the screw ranged between 80 mm and 120 mm, and the most frequently used lengths were 95 and 100 mm (Table 1).
Table 1.
Length of lag screws
| Frequency of use | Length of lag screws (mm) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 80 | 85 | 90 | 95 | 100 | 105 | 110 | 115 | 120 | |
| Number of occurrences | 1 | 3 | 4 | 10 | 8 | 3 | 0 | 2 | 1 |
Surgical time
The surgical time was measured from skin incision until wound closure. The average time was 28 minutes (range, 13–60 minutes).
X-ray exposure at surgery
X-ray exposure was measured during the actual surgery plus the exposure during fracture reduction. The average exposure time was 0.55 minutes (range, 0.15–1.0 minutes).
Time to fracture healing
Fracture healing was achieved after the primary operation in 31 cases (Fig. 2). The average time was ten weeks (range, 6–16 weeks).
Fig. 2.
Healing in anatomical position. a A 79-year-old female with stable pertrochanteric fracture (31A1). b Internal fixation with 135-degree DHS with a two-hole side-plate; the cortical screws were inserted in parallel fashion. c The anatomic position 16 months after surgery
Position of fracture fragments at healing
In 29 cases the fracture healed in anatomical position. In one case the fracture healed in 10 degrees of varus, and in one case the femoral shaft was displaced medially. In both cases it resulted in shortening of the operated limb by 1 cm.
Complications
In one case (3.1%), the patient fell out of bed four weeks after the operation and the plate pulled out of the femoral shaft. Reoperation was required including replacement of the DHS two-hole side-plate by a four-hole side-plate. Subsequently, the fracture healed in three months in the anatomical position without further complications and without limb shortening (Fig. 3).
Fig. 3.
Pull-out of side-plate. a A 55-year-old male with unstable pertrochanteric fracture (31A2) after internal fixation with 135-degree DHS with a two-hole side-plate; the cortical screws were inserted in parallel fashion. b Pull-out of side-plate after patient's fall four weeks after surgery. c The fracture healed after fixation with 135-degree DHS with a four-hole side-plate; the shortening of the leg was 1.5 cm
No postoperative haematoma or infection, cut-out of lag screws or malrotation of the operated limb were encountered in any of the patients.
Functional results
The average Broos functional scores were 46 prior to injury and 38 one year postoperatively.
Discussion
The basic difference between 135-degree DHS with a four-hole side-plate and that with a two-hole side-plate involves security of the implant fixation to the femoral shaft. Other reported differences are length of incision and the associated intraoperative blood loss, duration of surgery and postoperative pain [1, 4, 6, 9, 16]. However, there is no randomised study in the literature that would compare clinical results of DHS with two- and four-hole side-plates. Results of DHS with a two-hole side-plate used in pertrochanteric fractures has been dealt with only in a few studies [1, 4, 6, 9, 11, 16].
Biomechanics of fixation of the DHS plate to the femoral shaft was reported by Yian et al. [17] and McLoughlin et al. [11]. The study by Yian et al. [17] showed that three screws allowed a favourable distribution of tensile forces and adequate side-plate fixation. However, telescoping of the lag screw was prevented and the loading was performed in a non-physiological position. McLoughlin et al. [11] found an equivalent breaking strength between the DHS with two- and four-hole side-plates.
Bolhofner et al. [4] evaluated 70 patients (mean age 79 years) with both stable and unstable fractures (31A1 + 2). They recorded only two cases of screw cut-out, one case of pulling out of the plate and one deep infection. Moderate or severe collapse of fragments occurred in 20% of cases. The average surgical time was 31 minutes, the length of incision 5–6 cm, the average intraoperative blood loss was 77 ml and time to heal was 15 weeks. The authors did not specify limb shortening, follow-up period or functional scores.
Alobaid el al. [1] compared two groups with three- and four-part pertrochanteric fracture treated with DHS with a two-hole side-plate. In the first group (21 patients, mean age 81 years), the DHS was inserted using a minimally invasive surgical technique with a 2.5-cm long incision. The other group (27 patients, average age 82 years) was treated in a standard way. Neither fixation failure nor infection was encountered in either group. In the mini-invasive group of patients there was a slight drop of haemoglobin after the operation and significantly lower consumption of analgesics. On the other hand, significantly different surgical times were reported, namely, 29 minutes in the mini-invasive versus 70 minutes in the standard procedure. The authors did not specify time to heal, medial displacement of the femoral shaft, limb shortening or functional scores.
Di Paola et al. [6] treated 13 patients (mean age 82 years) using a minimally invasive technique for DHS with a two-hole plate for both stable and unstable pertrochanteric fractures in ten cases and for basicervical fractures of the femoral neck in three cases. The average length of incision was 5 cm, the average surgical time was 61 minutes, and the average intraoperative blood loss was 42 ml. All of the patients healed without complications at an average of 13 weeks after the operation. The minimum follow-up period was six months. The authors evaluated functional outcomes, but mostly on the basis of consultation by phone. Medial displacement and limb shortening were not reported.
Verhofstad et al. [16] evaluated 148 patients (mean age 80 years) with a stable pertrochanteric fracture (AO 31A1) treated with DHS with a two-hole side-plate. They recorded three mechanical complications. In two cases the screw cut out, and in one case the side-plate pulled out after the patient fell out of bed on the fifth day after operation. In 1.4% of cases, postoperative haematoma was observed, and in 2.7% infection of the surgical wound developed. In the rest of the patients the fracture healed without any severe complications. As this was a retrospective study, the authors did not evaluate surgical time, length of incision, intraoperative blood loss, time to heal or functional scores.
Laohapoonrungsee et al. [9] treated 83 patients (mean age 72 years) with pertrochanteric fractures (AO 31A1 + 2) using DHS with a two-hole side-plate. The average time to heal was 14.5 weeks. In two cases they recorded cut-out of the lag screw and in two cases pulling-out of the side-plate. The authors did not report length of incision, surgical time, medial displacement, limb shortening, follow-up period or functional scores.
Of great importance for evaluating results of treatment using DHS with a two-hole side-plate is stability of pertrochanteric fractures. Alobaid et al. [1] operated on 48 three- and four-part pertrochanteric fractures and did not encounter any pulling-out of the plate. Similarly, Di Paola et al. [6] operated on 13 stable pertrochanteric fractures and also did not record any pulling-out of the plate. Verhofstad et al. [13] treated 148 stable pertrochanteric fractures (31A1) and the plate was pulled out only once after the patient's fall from bed. Bolhofner et al. [4] used DHS with a two-hole side-plate in 70 stable and unstable pertrochanteric fractures and recorded only one pulling-out of the plate. Laohapoonrungsee el al. [9] treated 83 fractures of which 46 were unstable (31A2). The plate was pulled out twice and always in cases of unstable fractures. We encountered only one plate pull-out in 32 patients, namely, in the case of an unstable fracture (31A2). This proves that the two-hole side-plate only rarely pulls out and more often in unstable fractures.
When analysing these complications, however, none of the above-mentioned authors dealt with the manner of insertion of the cortical screws fixing the side-plate to the femoral shaft or with the impact of the length of the lag screw. In our case of pulling-out of the plate, both cortical screws were inserted parallel to each other; in divergently inserted screws we did not encounter this complication. The longer the lag screw, the greater the tensile force acting on screws fixing the side-plate to the femoral shaft. Thus in lag screws of extreme length, i.e. longer than 120 mm, a greater risk of pulling-out of the plate may be theoretically anticipated. However, this aspect has not been yet analysed in the literature.
The benefit of DHS with a two-hole side-plate is a shorter incision associated with less intensive bleeding, shorter surgical time and less postoperative pain, and perhaps also lower incidence of deep infections. The statement that DHS with a two-hole side-plate is associated with lower intraoperative blood loss and less postoperative pain has so far not been adequately supported in the literature. On the other hand, comparison of data concerning the length of incision and surgical time shows significant differences between individual authors and confirms the importance of the learning curve. Alobaid et al. [1] used the mini-invasive technique with the length of incision of 2.5 cm and a mean surgical time of 29 minutes. Di Paolo et al. [6] also used the mini-invasive technique, but the length of the incision was 5 cm and the mean surgical time was 61 minutes. Bolhofner et al. [4] used the standard operative technique with an incision 5–6 cm long and a surgical time of 31 minutes. We had almost the same values in our group, i.e. the average length of incision 5.5 cm and the surgical time 28 minutes. We studied the impact of both the learning curve and the number of holes in the DHS side-plate as early as in 2001 [2]. In DHS with a two-hole side-plate the mean surgical time was 30 minutes, and for a four-hole side-plate it was 36 minutes. The impact of the learning curve is also proven by the fact that in 1995 our mean surgical time in DHS with a four-hole side-plate was 69 minutes, in 1997 it dropped down to 44 minutes and in 2000 it was only 36 minutes.
Among the advantages of DHS with a two-hole side-plate is a smaller surgical approach. However, we did not follow the length of approach in DHS with a four-hole side-plate [2]. Based on our experience we have come to the conclusion that a correct surgical technique is much more important for the final result than the length of the approach. This applies primarily to reduction and insertion of the lag screw into the proximal fragment. In this respect, the length of the side-plate is irrelevant.
Conclusion
Based on our own results we may state that DHS with a two-hole side-plate is indicated in stable pertrochanteric fractures (31A1). The advantage of DHS with a two-hole side-plate as compared to a four-hole side-plate is a shorter operating time.
Contributor Information
Daniel Říha, Phone: +420-2-67162431, FAX: +420-2-67313372.
Jan Bartoníček, Phone: +420-2-67162431, FAX: +420-2-67313372, Email: bartonicek.jan@seznam.cz.
References
- 1.Alobaid A, Harvey EJ, Elder GM, et al. Minimally invasive dynamic hip screw: prospective randomized trial of two techniques of insertion of a standard dynamic fixation device. J Orthop Trauma. 2004;18:207–212. doi: 10.1097/00005131-200404000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Bartoníček J, Douša P, Košťál R, et al. Duration of surgery in internal fixation of trochanteric fractures. Acta Chir Orthop Traumatol Cech. 2001;68:294–299. [PubMed] [Google Scholar]
- 3.Baumgaertner MR. Intertrochanteric hip fractures. In: Browner BD, Jupiter JB, Levine AM, Trafton PG, editors. Skeletal trauma. 3. Philadelphia: Saunders; 2003. pp. 1776–1816. [Google Scholar]
- 4.Bolhofner BR, Russo PR, Carmen B. Result of intertrochanteric femur fractures treated with a 135-degree sliding screw with a two-hole side-plate. J Orthop Trauma. 1999;13:5–8. doi: 10.1097/00005131-199901000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Broos PLO, Haaften KIK, Stappaerts KH, et al. Hip fractures in the elderly. Mortality, functional results and social readaptation. Int Surg. 1989;74:191–194. [PubMed] [Google Scholar]
- 6.Paola M, Rozbruch SR, Helfet D. Minimal incision technique using a two-hole plate for fixation of stable intertrochanteric hip fractures. Orthopedics. 2004;27:270–274. doi: 10.3928/0147-7447-20040301-10. [DOI] [PubMed] [Google Scholar]
- 7.Ho M, Garau G, Walley G, et al. Minimally invasive dynamic hip screw for fixation of hip fractures. Inter Orthop. 2009;33:555–560. doi: 10.1007/s00264-008-0565-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Koval KJ. Intertrochanteric fractures: Use of a sliding hip screw. In: Wiss DA, editor. Master techniques in orthopaedic surgery. Fractures. 2. Philadelphia: Lippincott Williams and Wilkins; 2006. pp. 233–248. [Google Scholar]
- 9.Laohapoonrungsee A, Arpornchayanon O, Phornputkul C. Two-hole side-plate DHS in the treatment of intertrochanteric fracture: Results and complications. Injury. 2005;36:1355–1360. doi: 10.1016/j.injury.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 10.Lorich DG, Geller D, Nielson JH. Osteoporotic pertrochanteric hip fractures management and current controversies. J Bone Joint Surg Am. 2004;86:398–410. [PubMed] [Google Scholar]
- 11.McLoughlin SW, Wheeler D, Rider J, et al. Biomechanical evaluation of the dynamic hip screw with two- and four-hole side-plates. J Orthop Trauma. 2000;14:318–323. doi: 10.1097/00005131-200006000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Reich SM, Jaffe WL, Kummer FJ. Biomechanical determination of the optimal number of fixation screws for sliding hip screw plate. Bull Hosp Jt Dis. 1993–1995;53:43–44. [PubMed] [Google Scholar]
- 13.Saarenpää I, Heikkinen T, Ristiniemi J, et al. Functional comparison of the dynamic hip screw and the Gamma locking nail in trochanteric hip fractures: a matched-pair study of 268 patients. Inter Orthop. 2009;33:255–260. doi: 10.1007/s00264-007-0458-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sawaia RN, Belangero WD. The treatment of transtrochanteric fractures of the femur with a minimally invasive technique using an extramedullary implant MINUS System. Inter Orthop. 2008;32:159–165. doi: 10.1007/s00264-006-0304-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tennant G, Alonso . Intertrochanteric femur fractures. In: Stannard JP, Schmidtt AH, Kregor PJ, editors. Surgical treatment of orthopaedic trauma. New York: Thieme; 2007. pp. 567–588. [Google Scholar]
- 16.Verhofstadt MHJ, Werken Ch. DHS osteosynthesis for stable pertrochanteric femur fractures with a two-hole side-plate. Injury. 2004;35:999–1002. doi: 10.1016/j.injury.2003.10.030. [DOI] [PubMed] [Google Scholar]
- 17.Yian EH, Banerji I, Matthews LS. Optimal side-plate fixation for unstable intertrochanteric hip fractures. J Orthop Trauma. 1997;11:254–259. doi: 10.1097/00005131-199705000-00003. [DOI] [PubMed] [Google Scholar]