Abstract
The objective of this study was to determine the clinical outcome of combined bone grafting and matrix-supported autologous chondrocyte transplantation in patients with osteochondritis dissecans of the knee. Between January 2003 and March 2005, 21 patients (mean age 29.33 years) with symptomatic osteochondritis dissecans (OCD) of the medial or lateral condyle (grade III or IV) of the knee underwent reconstruction of the joint surface by autologous bone grafts and matrix-supported autologous chondrocyte transplantation. Patients were followed up at three, six, 12 and 36 months to determine outcomes by clinical evaluation based on Lysholm score, IKDC and ICRS score. Clinical results showed a significant improvement of Lysholm-score and IKDC score. With respect to clinical assessment, 18 of 21 patients showed good or excellent results 36 months postoperatively. Our study suggests that treatment of OCD with autologous bone grafts and matrix-supported autologous chondrocytes is a possible alternative to osteochondral cylinder transfer or conventional ACT.
Introduction
Osteochondritis dissecans (OCD) is characterised by subchondral bone necrosis, potentially followed by a separation of an osteochondral fragment from the joint surface [1–3]. Although OCD can arise in several joints, the most common site of OCD lesions is the medial and lateral femoral condyle of the knee [4]. The a etiology of OCD is still unknown but repetitive mechanical stress and repetitive traumas seem to be the most likely cause [1, 2].
Treatment of adult OCD remains controversial. Patients who present with a stable fragment can be treated by arthroscopic drilling, whereas intact and congruous unstable fragments require curettage and an internal fixation [5]. In some cases the fragment is not suitable for refixation. The resultant lesion of the joint surface is supposed to induce a degenerative process. Thus, unstable or loose fragments require surgical procedures that include reconstruction of the joint surface and joint congruity.
Various techniques have been developed for treatment of unsalvageable fragments. The potential of pluripotent stem cells from the bone marrow is the basis for drilling and microfracturing [6]. Autologous periosteal and perichondrial grafts are supposed to have stem cells in the cambium layer to synthesise a hyaline-like cartilage [7]. Other authors prefer autogenous osteochondral grafts including transplantation of osteochondral cylinders from a nonweightbearing region for defect replacement, but donor-site morbidity and incongruence of the surface have been reported [8]. Autologous chondrocyte transplantation (ACT) has been a widely-used technique for treatment of articular lesions [9]. In OCD with deep osteochondral defects, difficulties in restoring joint surface by conventional ACT still remain.
This study investigates clinical efficacy of a new surgical procedure in OCD with autologous bone grafts and matrix-supported autologous chondrocyte transplantation.
Patients and methods
Patients
Between January 2003 and March 2005, 21 of 22 patients (mean age 29.33 years, SD 7.47, age range 17–44 years) with OCD lesions of the medial (17) or lateral (4) femoral condyle were treated by autologous bone grafts and matrix-supported autologous chondrocytes (Table 1). All osteochondral lesions were grade III or IV on the ICRS scale (International Cartilage Repair Society) [10]. The size of OCD lesions ranged from 3 to 12 cm2 (mean 6.57 cm2, SD 2.14). Fifteen patients had undergone previous surgical procedures including arthroscopic drilling, microfracturing and excision of fragments. Six patients had no prior surgical history. All femoral lesions were symptomatic.
Table 1.
Patient profiles
| Case | Age (y) | Gender | Location | Condyle | Defect size (cm2) | Primary surgery | OCD grade (ICRS) | Period of symptoms (months) |
|---|---|---|---|---|---|---|---|---|
| 1 | 19 | M | Left | Medial | 4 | AD | III | 12 |
| 2 | 29 | F | Left | Medial | 5 | AD | III | 25 |
| 3 | 37 | M | Right | Medial | 7.5 | AD | III | 30 |
| 4 | 17 | F | Left | Lateral | 3 | - | IV | 8 |
| 5 | 33 | F | Left | Medial | 6.25 | MF | III | 48 |
| 6 | 44 | M | Right | Lateral | 6 | AD, MF | III | 60 |
| 7 | 27 | M | Right | Medial | 7.5 | MF | III | 30 |
| 8 | 24 | M | Left | Medial | 5 | AD | III | 18 |
| 9 | 31 | F | Right | Medial | 6 | EF | IV | 12 |
| 10 | 34 | F | Right | Medial | 8 | - | III | 24 |
| 11 | 38 | M | Right | Medial | 10.5 | AD, EF | IV | 84 |
| 12 | 22 | F | Left | Medial | 4 | AD | III | 13 |
| 13 | 32 | M | Right | Medial | 6 | MF, MF | III | 30 |
| 14 | 23 | M | Right | Lateral | 7.5 | - | III | 6 |
| 15 | 19 | M | Left | Medial | 6 | - | III | 12 |
| 16 | 42 | M | Right | Medial | 12 | AD, MF, MF | III | 100 |
| 17 | 28 | F | Left | Medial | 6.25 | AD, MF | III | 42 |
| 18 | 29 | M | Left | Medial | 7.5 | AD | IV | 18 |
| 19 | 31 | M | Right | Lateral | 9 | MF | III | 24 |
| 20 | 34 | M | Right | Medial | 6 | - | IV | 4 |
| 21 | 23 | M | Right | Medial | 5 | - | III | 12 |
OCD osteochondritis dissecans, ICRS International Cartilage Repair Society, M male, F female, AD arthroscopic drilling, MF microfracturing, EF excision of fragment
Surgical procedure
The surgical treatment was carried out in two hospitals by two surgeons. During an initial arthroscopy the defect was examined and type of OCD lesion was confirmed. A small biopsy was taken from the nonweightbearing area of the trochlea using an arthroscopic cartilage cutter (ArthroKinetics, Esslingen, Germany). Cartilage samples were transferred into a serum-free transport medium and sent to ArthroKinetics for culturing and processing. Chondrocytes were isolated by enzyme digestion and resuspended into a soluble collagen-I matrix (CaRes, ArthroKinetics). After the collagen matrix was jelled matrix-supported chondrocytes were cultured for two weeks in a culture medium containing serum of the patient. Cell viability and production of collagen type II (PCR) were routinely tested.
Patients were readmitted two weeks after initial arthroscopy for the second operation. Surgery was done in a tourniquet-controlled bloodless field. A single shot cephazolin (Kefzol) was given half an hour before surgery. A medial or lateral mini-arthrotomy was performed. The chondral lesion was excised with a curette as far as normal surrounding cartilage and defect size was estimated. A small separate incision or an extension of the medial arthrotomy was performed at the metaphyseal area of the medial site of the tibial head. Depending on the size of the femoral lesion one to three cylindrical bone grafts with a length of 2–3 cm were harvested using a water-cooled diamond cutter. The cortical area of the graft was cut off in order to achieve a cancellous bone plug. Sclerotic subchondral bone of the OCD lesion was then removed using the same diamond cutter with a smaller diameter. Bone grafts were transferred to the femoral defect and were pushed into the defect until the bone graft reached the surface of the surrounding subchondral plate (press-fit). Finally, the matrix-supported chondrocyte transplant was cut to size. The transplant was fixed by fibrin glue (Tissuecol, Baxter International) at the boundary of the defect. The knee was flexed and extended to confirm stability of the transplant.
Postoperative treatment
All patients were immobilised with a brace for 48 hours before starting physiotherapy and continuous passive motion. For six weeks patients were permitted only touch-down weight-bearing using crutches. After 12 weeks normal daily activities were allowed. Sporting activities were not allowed until 12 months after surgical treatment.
Evaluation
Patients were followed up prospectively. Clinical status was evaluated after three, six, 12 and 36 months using the Lysholm score [11], IKDC score [10], and ICRS score [10]. Follow-up examination included clinical scoring, conventional X-ray and magnetic resonance imaging. Magnetic resonance imaging (MRI) was performed by various radiology departments using different imaging protocols.
Statistics
Statistical analysis was performed by a hospital statistician using Statistica 6.0 (StatSoft Inc.). For parametric data, Friedmans ANOVA test and the Wilcoxon test were used. A significant difference was defined as p < 0.05. Statistical comparison of outcome between the groups (nonparametric data) was by Kruskal-Wallis test and Mann-Whitney U test. A p value <0.05 was taken to be statistically significant.
Results
Out of the 22 patients with OCD of the medial or lateral femoral condyle treated by autologous bone grafts and matrix-supported autologous chondrocytes, 21 (95.5%) could be re-examined after three, six, 12 and 36 months. One patient was excluded because he only returned for the three-month follow-up. The mean age at surgery was 29.33 years (SD 7.4, range 17–44). The male to female ratio was 66 to 34%. There were 14 males with mean age of 30.14 years (SD 8.13, range 19–44) and seven females with mean age of 27.71 years (SD 6.16, range 17–34).
There were 12 right (57%) and nine left (43%) knees. The epiphyseal plates were already closed. Lesions were located on the medial femoral condyle in 17 knees (81%); in four patients (19%) the lateral condyle was affected.
The mean size of the joint surface lesions was 6.57 cm2 (SD 2.14, range 3–12 cm2). Sixteen (76%) of the lesions were ICRS OCD type III, and five (24%) were ICRS OCD type IV. Patients had an average duration of symptoms of 29 months (SD 25.0, range 4–100 months), and underwent one to three previous operations in 15 cases (71.4%) (the mean number of previous operations of all patients was 1.0, range 0–3).
The average number of bone grafts inserted was 2.1 (range 1–3, i.e. five cases of three grafts, 13 cases of two grafts, three cases of one graft).
Initial arthroscopies and cartilage biopsies were done without any complications (swelling, pain or infection). Postoperatively two patients required prolonged rehabilitation due to swelling and a limited range of motion. Eventually, both patients regained full strength and range of motion.
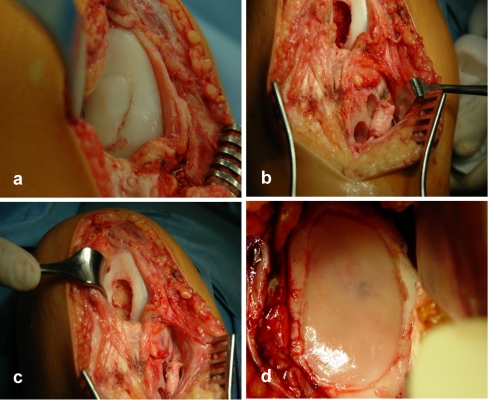
One patient progressed without complications postoperatively, but developed knee pain and swelling approximately 11 months after surgery. MRI on this patient suggested a loose OCD body in the joint. An arthroscopic revision was done and a loose body was removed. The OCD defect of the femoral condyle was still covered with the transplant. The patient recovered well (Fig. 1).
Fig. 1.
A 29-year-old female with osteochondritis dissecans of the medial condyle. Patient underwent arthroscopic drilling 3 years previously. a Intraoperative view showed an unstable fragment with sclerotic subchondral bone. b After debridement of the defect down to the subchondral bone two cylindrical bone grafts were harvested from the tibia. c Bone grafts were transferred to the femoral condyle. d Finally, matrix-supported autologous chondrocyte transplant (CaRes; ArthoKinetics, Esslingen, Germany) was fixed with fibrin glue (Tissuecol, Baxter International)
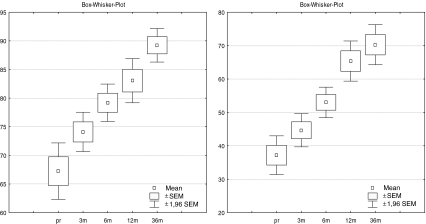
Lysholm score
Median Lysholm score increased between all follow-up times over 36 months (Fig. 2a). At the first follow-up three months postoperatively we found a median score of 64.1 points (p = 0.0008) which increased significantly over time to 79.19 points (6 months, p < 0.0001) and to 87.9 points (12 months, p = 0.0001). No significant change of Lysholm score was found in the period 12–36 months postoperatively (90.14 points) (12→36 months, p = 0.11). There were no significant differences between males and females.
Fig. 2.
Overall results of Lysholm score (a) and IKDC score (b) preoperatively and at three, six, 12 and 36 months (SEM standard error of the mean)
Regarding the preoperative period of symptoms (pos), patients were categorised into three groups (A: pos ≤ 12 months, B: 12 months < pos < 60 months, C: pos ≥ 0 months). Twelve months postoperatively, statistical analysis showed that patients who had a short duration of previous symptoms did significantly better in Lysholm score than patients with a longer period (A→B, p = 0.0073; A→C, p = 0.0160). However, duration of symptoms did not influence the results after 36 months (A→B p = 0.28; A→C p = 0.24).
Patients were also categorised by defect size (ds) (A: ds ≤ 4 cm2, B: 4 cm2 < ds ≤ 6 cm2, C: ds > 6 cm2). There was a trend towards a difference in Lysholm score for those who had defects ≤4 cm2, with the smaller defects doing better, but this did not reach statistical significance (A→C, p = 0.075 preoperatively versus p = 0.08 at 36 months).
IKDC
Before operation mean IKDC score was 37.19 (SD 13.56) points (Fig. 2b). During follow-up after three, six and 12 months patients showed significant improvement with a mean score of 70.29 points after 36 months (SD 14.04, p < 0.0001). Increase was highest between six and 12 months (12.38 points, SD 14.76). Twelve to 36 months after treatment we found a stagnation of IKDC score with only a slight improvement in this period (4.9 points, SD 6.99). There were no significant differences between males and females.
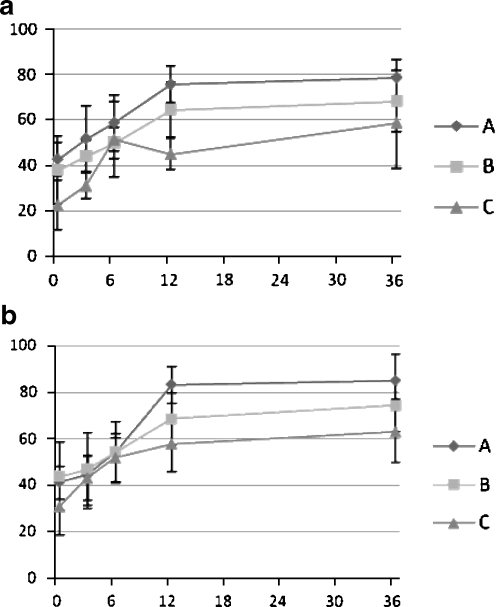
There were differences in early-term clinical outcome regarding the duration of symptoms (Fig. 3a). Patients with a short period of previous symptoms showed better results after 12 months (A→B, p = 0.07; A→C, p = 0.016). In concordance with the results of Lysholm score 36 months after operation there were no significant differences in IKDC score (A→B, p = 0.12; A→C, p = 0.2).
Fig. 3.
a IKDC score regarding period of symptoms (pos) (A: pos ≤ 12 months, B: 12 months < pos < 60 months, C: pos ≥ 60 months). Graph shows IKDC score preoperatively and at three, six, 12 and 36 months. b Graph showing the influence of defect size (ds) (A: ds ≤ 4 cm2, B: 4 cm2< ds ≤ 6 cm2, C: ds >6 cm2) regarding IKDC score preoperatively and at three, six, 12 and 36 months
The size of the defect is an influencing variable regarding IKDC score (Fig. 3b). The mean IKDC score was 85.0 points for defects ≤4 cm2 (group A) and 74.13 points for defects between 2 and 6 cm2 (group B) after 36 months. Defects larger than 6 cm2 (group C) showed a significantly inferior outcome (62.80). Analysis comparing IKDC scores between the groups after 36 months showed (significant) differences (A→C, p = 0.04; B→C, p = 0.08).
There was no correlation between the stage of OCD lesion (ICRS grade III or IV) and IKDC score.
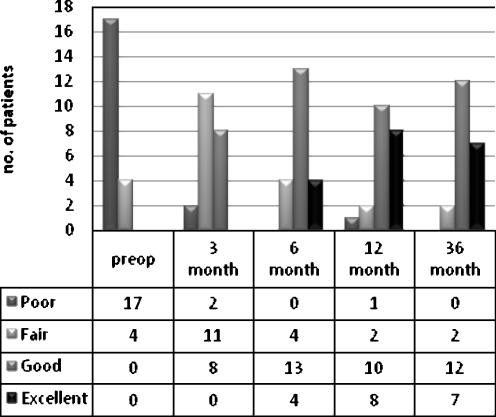
Global assessment of patient
The overall clinical grading score (Fig. 4) was evaluated pre- and postoperatively to reflect patients' assessments. Initially, 17 patients (81%) had a poor and four patients (19%) a fair rating. Three months postoperatively, ratings switched to eight good (38%), 11 fair (52.5%) and two poor (9.5%) results. One-year follow-up showed one patient with a poor (4.8%) result. Two patients (9.5%) rated fair, ten good (47.7%) and eight excellent (38%). Patients assessments at 12 versus 36 months postoperatively showed a slight increase without significance (p = 0.66).
Fig. 4.
Clinical results at 36 months for 21 patients who received autologous bone grafts and matrix-supported chondrocyte transplantation
Discussion
Many surgical options have been proposed for the treatment of stage III and IV OCD lesions. Obviously, simple excision or fixation of symptomatic fragments shows good early-term results. On the other hand long-term results are still debated and several authors have reported that simple excision of OCD fragments results in an unacceptable outcome [12–19].
Incongruence of the fragment or too many fragmented loose bodies are contraindications for internal fixation. These patients, as well as patients with persisting symptoms after refixation, require new options for surgical treatment. Recently, OCD treatment with autologous periosteum or perichondrium [20], osteochondral autograft transfer (OATS) and transplantation of autologous chondrocytes (ACT) have been reported [7–9].
Transplantation of osteochondral cylinders (autograft, allograft) have been used with reported success [8, 21, 22]. Using the OATS technique, Laprell and Petersen [21] found a normal function in 12 of 35 patients, a nearly normal function in 14 of 35 and an abnormal function in 3 of 35 after a mean follow-up of 8.1 years.
Bentley et al. [8] reported a prospective randomized comparison between mosaicplasty versus autologous chondrocyte transplantation where 19% of the defects developed from OCD. The authors found better results using ACT.
Peterson et al. [9] have shown encouraging results using ACT for treatment of OCD in 58 patients. After a mean follow-up of 5.6 years they achieved 91% good or excellent results on the basis of clinician evaluation. Interestingly, they used two different surgical procedures. Normally, care was taken not to provoke bleeding from the subchondral bone but in cases of deep defects (>8 mm, 7 of 58 patients) Peterson et al. removed the subchondral bone, filled the defect with cancellous bone and performed a “sandwich technique” of two layers of periosteal flaps. Although results of ACT were encouraging in both OCD and traumatic osteochondral lesions some problems like treatment of the subchondral bone, hypertrophy of the periosteal flap and dedifferentiation of chondrocytes still remain. This was our starting point to evaluate treatment of OCD stages III and IV with a combination of autologous bone grafts and matrix-supported autologous chondrocytes.
Obviously, the follow-up time of our study was not long enough to prove the long-term durability of patient assessment and graft integration, but we were able to show that our technique is safe without any loss of transplanted grafts 36 months postoperatively.
Results of Lysholm score were similar to those of Peterson et al. [20] (92.4 points, mean follow-up 5.6 years). Patient selection was close to ours with respect to mean age, mean defect size and number of previous operations. Interestingly, in our study a significant increase of Lysholm score was only observed during the first 12 months. Between 12 and 36 months significant changes were not detectable.
After 36 months, 85% of our patients showed good or excellent results. Bentley et al. [8] found 88% good and excellent results after a mean duration of 19 months using conventional ACT. Fourteen of 58 lesions suffered were from OCD. Interestingly, they performed no transplantation of cancellous bone or bone cylinders to fill up subchondral defects.
The first clinical experiences with the 3D-collagen gel which were used in our study were published by Andereya et al. [23] where eight of 22 patients suffered from OCD. Overall clinical outcome after 24 months showed very good and good results in 84.6% and fair results 15.4%.
Ochs et al. [24] reported the outcome of surgical treatment of osteochondral defects with bone grafting and matrix-supported autologous chondrocyte transplantation in 22 patients. Their technique is very similar to our procedure. The average follow-up was 16 months (range 6–36). Mean Lysholm score increased from 50.1 points (SD 15.7) to 84.5 (SD 10.9).
Maus et al. [25] reported the results of matrix-supported treatment of osteochondral defects of the knee using the same matrix-supported chondrocyte transplant which was used in our study (CaRes). Depending on defect size the lesions were reconstructed by cancellous bone cylinders or chips from cancellous bone. Out of 13 patients, ten showed good or very good clinical results. Mean IKDC score improved from 38.4 (SD 12.7) to 66.1 (SD 17.0), which was less distinct than our results. In comparison to our study, the mean defect size was larger (8.1 cm2 versus 6.57 cm2), the average age was higher (34.9 versus 29.33 years) and patients had undergone more previous operations (1.5 versus 1.0).
Some variables influenced our results. Clinical improvement depends on both duration of symptoms and defect size. Patients with a long period of pain and functional disorder showed an inferior clinical outcome in early-term results but mid-term results did not show significant differences. An important aspect is that the duration of symptoms is associated with a higher number of previous surgical treatments. We suggest that previous surgical procedures rather than duration of symptoms can compromise clinical outcome.
In our study, clinical outcome of bone grafting and matrix-supported chondrocyte transplantation decreases if the defect size is larger than 6 cm2. This was also reported by Krishnan et al. [26] for collagen-covered ACT. They concluded that the healing potential of larger defects in adult-onset disease is inferior because they could not find a relationship between defect size and clinical outcome in juvenile-onset disease of OCD.
In conclusion, treatment of OCD with autologous bone grafts and matrix-supported autologous chondrocytes is a possible alternative to osteochondral cylinder transfer or conventional ACT. The best results are associated with smaller defects and a short duration of previous symptoms.
Contributor Information
Joern Steinhagen, Phone: +49-40-4280353670, FAX: +49-40-4280355518, Email: steinhagen@uke.uni-hamburg.de.
Juergen Bruns, Email: J.bruns@d-k-h.de.
Georg Deuretzbacher, Email: deuretzb@uke.uni-hamburg.de.
Wolfgang Ruether, Email: ruether@uke.uni-hamburg.de.
Martin Fuerst, Email: mfuerst@uke.uni-hamburg.de.
Oliver Niggemeyer, Email: niggemey@uke.uni-hamburg.de.
References
- 1.Clanton TO, DeLee JC. Osteochondritis dissecans. History, pathophysiology and current treatment concepts. Clin Orthop Relat Res. 1982;167:50–64. [PubMed] [Google Scholar]
- 2.Aichroth P. Osteochondritis dissecans of the knee. A clinical survey. J Bone Jt Surg Br. 1971;53(3):440–447. [PubMed] [Google Scholar]
- 3.Glancy GL. Juvenile osteochondritis dissecans. Am J Knee Surg. 1999;12(2):120–124. [PubMed] [Google Scholar]
- 4.Cahill BR, Phillips MR, Navarro R. The results of conservative management of juvenile osteochondritis dissecans using joint scintigraphy. A prospective study. Am J Sports Med. 1989;17(5):601–605. doi: 10.1177/036354658901700502. [DOI] [PubMed] [Google Scholar]
- 5.Nakagawa T, Kurosawa H, Ikeda H, et al. Internal fixation for osteochondritis dissecans of the knee. Knee Surg Sports Traumatol Arthrosc. 2005;13(4):317–322. doi: 10.1007/s00167-004-0521-9. [DOI] [PubMed] [Google Scholar]
- 6.Steadman JR, Miller BS, Karas SG, et al. The microfracture technique in the treatment of full-thickness chondral lesions of the knee in National Football League players. J Knee Surg. 2003;16(2):83–86. [PubMed] [Google Scholar]
- 7.Bouwmeester PS, Kuijer R, Homminga GN, et al. A retrospective analysis of two independent prospective cartilage repair studies: autogenous perichondrial grafting versus subchondral drilling 10 years post-surgery. J Orthop Res. 2002;20(2):267–273. doi: 10.1016/S0736-0266(01)00099-7. [DOI] [PubMed] [Google Scholar]
- 8.Bentley G, Biant LC, Carrington RW, et al. A prospective, randomised comparison of autologous chondrocyte implantation versus mosaicplasty for osteochondral defects in the knee. J Bone Jt Surg Br. 2003;85(2):223–230. doi: 10.1302/0301-620X.85B2.13543. [DOI] [PubMed] [Google Scholar]
- 9.Peterson L, Minas T, Brittberg M, et al. Two- to 9-year outcome after autologous chondrocyte transplantation of the knee. Clin Orthop Relat Res. 2000;374:212–234. doi: 10.1097/00003086-200005000-00020. [DOI] [PubMed] [Google Scholar]
- 10.International Cartilage Repair Society (2008) ICRS evaluation. Available at: www.cartilage.org Site accessed 10 July 2009
- 11.Lysholm J, Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med. 1982;10(3):150–154. doi: 10.1177/036354658201000306. [DOI] [PubMed] [Google Scholar]
- 12.Green WT, Banks HH. Osteochondritis dissecans in children. J Bone Jt Surg Am. 1953;35-A(1):26–47. [PubMed] [Google Scholar]
- 13.Koch S, Kampen WU, Laprell H. Cartilage and bone morphology in osteochondritis dissecans. Knee Surg Sports Traumatol Arthrosc. 1997;5(1):42–45. doi: 10.1007/s001670050023. [DOI] [PubMed] [Google Scholar]
- 14.Michael JW, Wurth A, Eysel P, Konig DP. Long-term results after operative treatment of osteochondritis dissecans of the knee joint – 30 year results. Int Orthop. 2008;32(2):217–221. doi: 10.1007/s00264-006-0292-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Anderson AF, Pagnani MJ. Osteochondritis dissecans of the femoral condyles. Long-term results of excision of the fragment. Am J Sports Med. 1997;25(6):830–834. doi: 10.1177/036354659702500617. [DOI] [PubMed] [Google Scholar]
- 16.Wright RW, McLean M, Matava MJ, et al. Osteochondritis dissecans of the knee: long-term results of excision of the fragment. Clin Orthop Relat Res. 2004;424:239–243. doi: 10.1097/01.blo.0000128216.10732.d8. [DOI] [PubMed] [Google Scholar]
- 17.Aglietti P, Ciardullo A, Giron F, et al. Results of arthroscopic excision of the fragment in the treatment of osteochondritis dissecans of the knee. Arthroscopy. 2001;17(7):741–746. doi: 10.1053/jars.2001.25336. [DOI] [PubMed] [Google Scholar]
- 18.Murray JR, Chitnavis J, Dixon P, et al. Osteochondritis dissecans of the knee; long-term clinical outcome following arthroscopic debridement. Knee. 2007;14(2):94–98. doi: 10.1016/j.knee.2006.11.011. [DOI] [PubMed] [Google Scholar]
- 19.Twyman RS, Desai K, Aichroth PM. Osteochondritis dissecans of the knee. A long-term study. J Bone Jt Surg Br. 1991;73(3):461–464. doi: 10.1302/0301-620X.73B3.1670450. [DOI] [PubMed] [Google Scholar]
- 20.Bouwmeester SJ, Beckers JM, Kuijer R, et al. Long-term results of rib perichondrial grafts for repair of cartilage defects in the human knee. Int Orthop. 1997;21(5):313–317. doi: 10.1007/s002640050175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Laprell H, Petersen W. Autologous osteochondral transplantation using the diamond bone-cutting system (DBCS): 6–12 years' follow-up of 35 patients with osteochondral defects at the knee joint. Arch Orthop Trauma Surg. 2001;121(5):248–253. doi: 10.1007/s004020000217. [DOI] [PubMed] [Google Scholar]
- 22.Horas U, Pelinkovic D, Herr G, et al. Autologous chondrocyte implantation and osteochondral cylinder transplantation in cartilage repair of the knee joint. A prospective, comparative trial. J Bone Jt Surg Am. 2003;85-A(2):185–192. doi: 10.2106/00004623-200302000-00001. [DOI] [PubMed] [Google Scholar]
- 23.Andereya S, Maus U, Gavenis K, et al. First clinical experiences with a novel 3D-collagen gel (CaReS) for the treatment of focal cartilage defects in the knee. Z Orthop Ihre Grenzgeb. 2006;144(3):272–280. doi: 10.1055/s-2006-933445. [DOI] [PubMed] [Google Scholar]
- 24.Ochs BG, Muller-Horvat C, Rolauffs B, et al. Treatment of osteochondritis dissecans of the knee: one-step procedure with bone grafting and matrix-supported autologous chondrocyte transplantation. Z Orthop Unfall. 2007;145(2):146–151. doi: 10.1055/s-2007-965167. [DOI] [PubMed] [Google Scholar]
- 25.Maus U, Schneider U, Gravius S, et al. Clinical results after three years use of matrix-associated ACT for the treatment of osteochondral defects of the knee. Z Orthop Unfall. 2008;146(1):31–37. doi: 10.1055/s-2007-989353. [DOI] [PubMed] [Google Scholar]
- 26.Krishnan SP, Skinner JA, Carrington RW, et al. Collagen-covered autologous chondrocyte implantation for osteochondritis dissecans of the knee: two- to seven-year results. J Bone Jt Surg Br. 2006;88(2):203–205. doi: 10.1302/0301-620X.88B2.17009. [DOI] [PubMed] [Google Scholar]