Abstract
The aim of this prospective study was to assess the clinical outcomes of an unstable fracture of the lateral end of the clavicle treated with an arthroscopic-assisted locking compressive plate (LCP) clavicular hook plate. Twenty-three patients underwent arthroscopic assisted LCP clavicular hook plate fixation for these fractures. All patients achieved clinical and radiological union over a mean of 4.2 months (range, 3.4–5 months). Four patients (17%) showed some degree of acromial osteolysis. Three patients (13%) showed radiological signs of arthrosis of the acromioclavicular joint. In one patient, a second fracture (stress) was observed between the medial two screws of the plate without an additional injury. Five patients (22%) showed subacromial bursitis on dynamic ultrasonography. The mean Constant and Murley score was 91 points (range, 81–98). The average level of pain in the shoulder at rest and on abduction was 1 (range, 0–2) and 2.4 (range, 0–4), respectively. Based on our experience, arthroscopic-assisted LCP hook plate fixation for the treatment of unstable fractures of the lateral end of the clavicle is not without complications. However, it is an acceptable alternative method that is easy to apply with good results. Furthermore, it prevents rotator cuff impingement, allows early mobilisation and maintains the acromioclavicular joint biomechanics.
Introduction
Fractures of the lateral end of the clavicle account for 12–15% of all clavicle fractures [4]. Types I and III fractures can be treated conservatively. However, type II fractures (distal clavicular fracture with a disruption of the coracoclavicular ligaments) are unstable due to the four displacing forces that retard union [22]. The weight of the arm pulls the lateral fragment away from the medial fragment [4]. The rate of non-union in these fractures is as high as 22–50% [14, 24]. Non-surgical treatments for these fractures are associated with a higher incidence of residual shoulder dysfunction and non-union compared to those treated surgically [6, 15]. Many studies recommend an open reduction and internal fixation [1, 6, 8, 17], but there is no consensus regarding the ideal method to produce the best functional outcome. Various types of fixation techniques have been recommended, such as transarticular or extraarticular Kirschner wire fixation [7, 22], coracoclavicular screw fixation [26], and tension band wire fixation [23]. However, these techniques are associated with considerable risk of complications, particularly the loss of reduction, pin migration, skin ulceration due to pin irritation, and acromioclavicular (AC) joint degeneration [17, 19]. It is difficult to achieve rigid fixation and early mobilisation because the distal fragment is usually small, comminuted, and the metaphysis bone is soft. Therefore, a hooked plate with an extension under the acromion has been developed to provide more stable fixation. In 1983, the clavicular hook plate was first used in two patients with distal clavicular fractures with substantial advantages over conventional methods, including a low risk of complications [25]. Thereafter, other types of clavicular hook plates have been developed with good clinical results [5, 9, 10]. However, some studies have raised issues, such as the high rate of serious complications including subacromial impingement, rotator cuff injury, fracture of the clavicle at the medial end of the plate, and fixation failure of the hook plate in elderly people with osteoporosis [2, 16, 18, 20].
Recently, the locking compressive plate (LCP) clavicular hook plate was introduced. Angular stable fixation of the fragments regardless of the bone quality and the lower risk of primary and secondary loss of reduction are possible using this LCP plate. Moreover, an arthroscopic confirming procedure was added to the surgical procedure after temporary fixation of the plate to prevent rotator cuff injury by the hook of the plate.
The purpose of this study was to evaluate the clinical outcome of unstable fractures of the lateral end of the clavicle treated with an arthroscopic-assisted LCP clavicular hook plate. The functional recovery and the surgical complications including subacromial impingement, rotator cuff damage, and fixation failure were also analysed.
Materials and methods
Our Institutional Review Board approved this study, and all patients who had been treated with the procedure under study were available for review.
Twenty-three consecutive patients with unstable fractures of the lateral end of clavicle were treated surgically between January 2008 and April 2009. The patients were treated with a LCP clavicular hook plate (Synthes, Oberdorf, Switzerland). The inclusion criteria for this study were (1) Neer type II fractures, (2) unilateral fractures, (3) more than a six-month follow-up after surgery, and (4) normal shoulder function before injury. The exclusion criteria included patients with acromioclavicular joint dislocation, pathological fractures, previous surgery on the affected clavicle or shoulder, and hemiparesis. All procedures were performed by one of two surgeons.
Specifics of implant design
The LCP clavicular hook plate comes in both stainless steel and titanium versions. The titanium version was used in this study. The LCP clavicular hook plate is an anatomically pre-contoured plate that facilitates optimal implant placement to provide an improved outcome. The shaft of the plate undercuts and reduces the impairment of blood supply to the bone. The shaft is bent 12° to make implant placement easier. The LCP clavicular hook plate is available in four different lengths (4- to 7-hole plates) and three different hook depths (12, 15, and 18 mm) with a left and right version for optimal sizing and screw (3.5 mm) positioning for each individual patient (Fig. 1). The lateral end of the plate is broad and has two screw holes that can potentially offer good stability and allow early mobilisation. The posterior half of the lateral end of the plate extends further as a hook. Anatomically, the hook is placed under the acromion, which acts as a lever to elevate the lateral fragment and maintain firm anatomical reduction without damaging the acromioclavicular joint. Unlike the conventional form of a plate, which involves the application of a locking compressive plate, the LCP clavicular hook plate has advantages in that stable angular fixation of the fragments, regardless of bone quality and good purchase, is also possible in osteoporotic bone and multifragment fractures (Synthes).
Fig. 1.
The LCP clavicular hook plates. The plate is available in four different lengths (4- to 7-combi-hole plates) and three different hook depths (12, 15, and 18 mm) with a left and right version for optimal sizing and screw fixation
Surgical technique
Under general or regional (interscalene) anaesthesia, the patient is placed in the beach chair position on a radiolucent operating table. A curved incision is made on the lateral third of the clavicle. The deltoid insertion over the clavicle is detached partially with a periosteal elevator. The fracture site is exposed and reduced with temporary Kirshner wire fixation. The plate is selected based on the fracture length and thickness of the acromion process, as measured by preoperative radiographs of the acromion or application of intraoperative trial implants (12, 15, and 18 mm depth). The appropriate plate is selected and the hook is passed under the acromion posterior to the acromioclavicular joint. When necessary, the plate is bent between the combi-holes to fit the shape of the clavicle. The plate is fixed temporarily using a screw through the most medial plate hole. The plate position is assessed fluoroscopically to confirm that full shoulder motion, particularly in abduction and external rotation, can be achieved without impinging on the humeral head by the hook. However, these procedures did not accurately evaluate the presence of impingement of the hook of the plate and rotator cuff. Accordingly, an arthroscopic evaluation procedure was also performed in this study. A 3.5 mm, 30° angled arthroscope (ConMed Linvatec, Largo, FL) was inserted using a standard posterior or lateral portal. In this setting, passive full shoulder motion was performed. Definitive fixation with screws was performed after confirming that the hook was not impinged on the rotator cuff. In fixing two screws on the lateral part, both cortices (near and far cortex) were predrilled in all cases for stable fixation because the bone is soft. A locking screw, whose length was identical to that of both cortices, was then inserted. Depending on the type of fracture, an interfragmentary screw was also used if necessary. However, wiring or Kirshner wires were not used (Fig. 2). A sling was applied in the immediate postoperative period for comfort. Active mobilisation was allowed from the second postoperative day, and full range of motion was usually achieved after three to four weeks. Heavy manual work was not permitted until solid union of the fracture was observed.
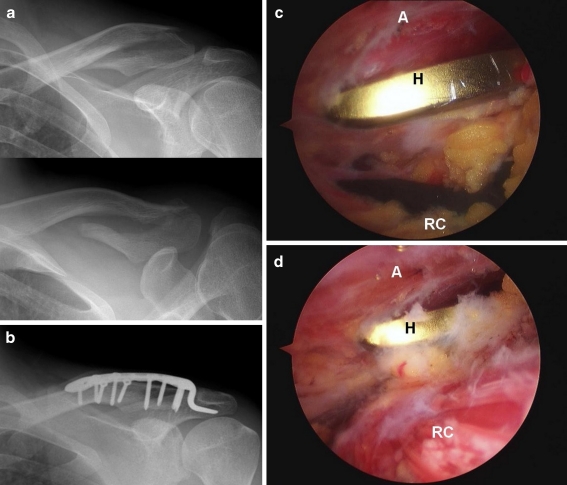
Fig. 2.
a Two radiographic views of a 31-year-old man with a type II fracture of the left distal clavicle. b Radiographic view taken postoperatively, demonstrating satisfactory fracture reduction. c, d Shoulder arthroscopy was performed immediately after temporary hook plate fixation. The arthroscopic views showed no impingement between the hook of the plate and the rotator cuff in the shoulder neutral position (c), and in shoulder abduction and the external rotation position (d). Abbreviations: A acromion, H hook of the plate, RC rotator cuff
Patients and evaluations
There were 23 patients, 19 men and four women, with a mean age of 43 years (range, 21–74 years). The right and left shoulder was involved in 15 and eight patients, respectively. The causes of injury were a simple fall in 12 cases, a bicycle accident in six, a traffic accident in four, and a fall from height in one case. All patients were operated on within seven days of the injury using a LCP clavicular hook plate. The patients were evaluated clinically and radiologically, and the mean follow-up period was 13 months (range, 6–21 months).
The functional outcomes were assessed using the shoulder scoring system described by Constant and Murley [3]. In this system, both the subjective and objective clinical data were included, with a maximum score of 100 points. Pain (15 points), the activities of daily living (20 points), range of shoulder motion (40 points), and muscle power (25 points) were evaluated. Furthermore, the patients were asked to evaluate the shoulder function of the injured shoulder compared to the other shoulder on a visual analogue scale (VAS) and patient satisfaction rating with the shoulder. After osteosynthesis, plain radiographs (anteroposterior and axial radiographs) were taken once every four weeks for all patients. The radiographs were examined for any evidence of fracture healing, implant failure or plate migration. Radiographic healing was defined as any evidence of bridging callus across the fracture sites or the obliteration of fracture lines.
Results
Radiographic bony union was obtained in all patients, and the mean period required for healing was 4.2 months (range, 3.4–5 months). The hook plate was removed from all patients after bony union, and the mean period between surgery and plate removal was 5.1 months (range, 3.6–7 months). Four patients (17%) showed some degree of acromial osteolysis. However, these were not symptomatic clinically. Three (13%) of the 23 patients showed radiological signs of arthrosis of the acromioclavicular joint (irregularities of the clavicle joint surface/mild osteophyte). Only one of these patients (4%) experienced clinical symptoms of arthrosis. No fractures of the acromion were encountered. In one patient, on week seven after the initial operation, a second fracture occurred between two screws of the medial portion of a plate without a new injury and the screws were cut-out (Fig. 3). The shoulder was immobilised in a broad arm sling until both fractures healed. The plate was removed three months later. Plate bending to fit the shape of the clavicle was performed in 16 patients (70%).
Fig. 3.
A 52-year-old man sustained a type II fracture of the left distal clavicle. The fracture was fixed using a hook plate with six holes and a 15 mm depth without plate bending. Radiographic view taken seven weeks after surgery, showing cut-out of the screws and a second fracture (stress) between two medial screws
In this study, after fracture union, but prior to removal of the plate, an evaluation of the rotator cuff injury was also performed. An ultrasonographic examination was used to assess the impingement of the rotator cuff and hook of the plate in 21 patients. As a result, there were no cases of rotator cuff injury. The ultrasonographic findings revealed five patients (22%) with bursitis. Of these, three cases had concurrent of acromial osteoylsis due to hook migration and bursitis. In the cases in which the clinical symptoms were manifested, there was only one case in which bursitis only was present without hook migration. However, after plate removal, the symptoms improved without specific treatment (Fig. 4). One case of a superficial wound infection was treated successfully with oral antibiotics and local wound care.
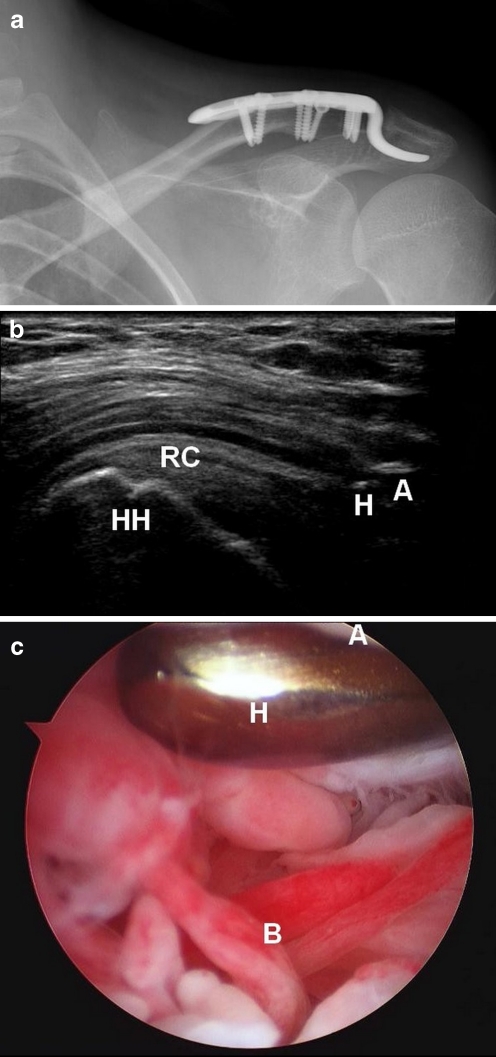
Fig. 4.
A 22-year-old woman sustained a type II fracture of the left distal clavicle. a Radiographic view taken five months postoperative shows complete bony union. b Ultrasonographic view taken five months postoperative prior to plate removal. The patient achieved a full range of shoulder motion, but she complained of mild shoulder discomfort. Ultrasonography showed subacromial bursitis. Abbreviations: A acromion, H hook of the plate, RC rotator cuff, HH humeral head. c Arthroscopic view shows subacromial bursitis. The plate was removed and a combined arthroscopic debridement and partial bursectomy was performed. Abbreviations: A acromion, H hook of the plate, B subacromial bursitis
The mean score for the affected shoulder using the scoring system of Constant and Murley was 91 points (range, 81–98), and the mean score for the contralateral shoulder was 95 points (range, 89–100). The average pain in the shoulder at rest and on abduction was 1 (range, 0–2) and 2.4 (range, 0–4), respectively. The patients were asked to grade their shoulder. All but two cases (91%) had returned to their previous work four months after surgery. Twenty patients (87%) could perform the same athletic activities six months after surgery.
Discussion
This study demonstrates that good treatment outcomes can be achieved for unstable fractures of the lateral end of the clavicle using an arthroscopic-assisted LCP clavicular hook plate.
Fractures of the lateral end of the clavicle represent 10% of clavicular fractures [15] that are associated with a non-union rate of 22–50% if treated conservatively [14, 15, 24]. This high incidence of non-union may be due to the underlying soft tissue damage and/or soft tissue interposition between the fracture fragments [6, 15]. Therefore, surgery is recommended for unstable distal clavicular fractures. Several surgical methods have been proposed; however, all are associated with problems and there is no consensus regarding the best method to provide the optimal clinical results.
In 1983, the clavicular hook plate (Balser plate) was first used in two patients with distal clavicular fractures [25]. Various clavicular hook plates have since been developed to stabilise distal clavicular fractures. Initially, during surgery for a fracture, the presence of impingement of the hook of the plate and humeral head can be determined by fluoroscopy. However, impingement of the hook and rotator cuff cannot be examined. Accordingly, in this study, only one screw was inserted temporarily into the most medial part of the plate and this was followed by an arthroscopic evaluation in order to prevent rotator cuff injury due to the hook of the plate. An arthroscopy examination was performed through the standard posterior or lateral portal. Passive mobilisation of the shoulder was attempted. It was confirmed that there was no impingement of the hook and rotator cuff in exercises from all directions. Following this confirmation, the other screws were fixed. At this time, when impingement was identified, a plate with another hook depth was used or a hook portion was bent to prevent impingement. In addition, after bone union was achieved prior to removing the plate at an outpatient clinic, 21 patients were tested for the presence of rotator cuff injury using dynamic ultrasonography. There was no rotator cuff injury in any of the patients. Ultrasonography revealed five patients (22%) with bursitis. Of them, only one case showed clinical symptoms. After removing the plate, the symptoms improved without specific treatment. These results show that the arthroscopic-assisted procedure plays a very important role in preventing rotator cuff injury.
Biomechanical studies have shown that rotational movement occurs between the clavicle and scapula during flexion and abduction of the humerus [11]. This causes problems with rigid fixation methods. The hook plate is designed to address this problem [11, 12]. Because hook plate fixation maintains the biomechanics of the acromioclavicular joint, it allows some degree of early mobilisation [12] and avoids the need for a reconstruction of the coracoclavicular ligaments. However, subacromial impingement or bony erosion of the acromion tip can occur due to the concentration of stress on the hook of a plate. Some authors maintain that only a restricted range of movement should be permitted before removing the plate [2, 12]. However, other authors report that an early and full range of motion did not affect hook migration. In contrast, the unstable fragment is fixed with a lever on the hook. Therefore, some degree of hook migration may be unavoidable [21]. In this study, four patients (17%) developed some degree of hook migration. All of these four cases were in the group of seven cases in which the plate had not been bent. It was assumed that forced fixation of the plate to the clavicle caused a pressure concentration to the hook itself and then produced hook migration. The appropriate bending of the hook was performed to prevent forced fixation of the plate to the clavicle and the hook was engaged securely under the acromion. A hook plate with a greater depth can be used (hook depth is 12, 15, and 18 mm) to easily apply a plate without plate bending. However, in this setting, there is a higher likelihood that the impingement of the hook of a plate and rotator cuff or humeral head might occur. Therefore, the plate was used after bending. However, long-term hook plate fixation has a considerable risk of complications, such as hook impingement, rotator cuff damage and acromial fracture. Accordingly, early removal of the plate was performed in all cases (mean 5.1 months) once bone union had been achieved.
Screw loosening and fixation failure have been reported with the use of a clavicular hook plate, particularly in elderly people (over 60 years old) [2, 13, 18]. This has been reported to occur as a result of poor bone quality. Accordingly in elderly people, delayed rehabilitation was performed, which led to shoulder stiffness [2]. However, a locking plate was used in our study. Two locking screws were inserted through the wide lateral part of the plate into the lateral fragment of the fracture. Therefore, firm and stable fixation could be achieved in elderly people, and there were no complications, such as fixation failure. In these people, an early range of motion can be performed. In one patient, a displaced fracture of the lateral end of the clavicle was sustained, which was managed using fixation using a six-hole hook plate. Seven weeks later, a second fracture (stress) was observed between the medial two screws of the plate without an additional injury. A review of the literature showed that after plate fixation, a second fracture can occur at the medial end of a plate because of a new injury. In addition, screw cut-out from the clavicle can occur in patients with osteoporosis [2, 13]. However, there was no new injury or osteoporosis in our cases. In this patient, no plate bending was performed to fix the plate, and fixation was performed using forceful levering. This was assumed to be the cause of the second stress fracture due to the concentration of stress on the medial portion of a plate in the clavicle.
The LCP clavicular hook plate is designed anatomically precontoured to fit the acromion and clavicle. However, further improvements in plate design may be necessary because bending of the plate was required in 16 patients (70%) where it did not fit the curve of the acromioclavicular joint. The need for a second surgical procedure to remove the implant in order to avoid progressive acromial osteolysis is a significant disadvantage of this technique. To our knowledge, this is the first report of arthroscopic-assisted LCP clavicular hook plate fixation for unstable fractures of the lateral end of the clavicle.
These results suggest that the treatment of unstable fractures of the lateral end of the clavicle using arthroscopic-assisted LCP clavicular hook plate fixation is not without complications. However, it is an acceptable alternative method that is easy to apply with good results. In addition, it prevents rotator cuff impingement, allows early mobilisation and maintains the acromioclavicular joint biomechanics.
References
- 1.Ballmer FT, Gerber C. Coracoclavicular screw fixation for unstable fractures of the distal clavicle. A report of five cases. J Bone Jt Surg Br. 1991;73(2):291–294. doi: 10.1302/0301-620X.73B2.2005158. [DOI] [PubMed] [Google Scholar]
- 2.Charity RM, Haidar SG, Ghosh S, Tillu AB. Fixation failure of the clavicular hook plate: a report of three cases. J Orthop Surg (Hong Kong) 2006;14(3):333–335. doi: 10.1177/230949900601400320. [DOI] [PubMed] [Google Scholar]
- 3.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–164. [PubMed] [Google Scholar]
- 4.Craig EV. Fractures of the clavicle. In: Rockwood CA Jr, Green DP III, editors. The shoulder. Philadelphia: W.B. Saunders; 1990. pp. 367–412. [Google Scholar]
- 5.Eberle C, Fodor P, Metzger U. Hook plate (so-called Balser plate) or tension banding with the Bosworth screw in complete acromioclavicular dislocation and clavicular fracture. Z Unfallchir Versicherungsmed. 1992;85(3):134–139. [PubMed] [Google Scholar]
- 6.Edwards DJ, Kavanagh TG, Flannery MC. Fractures of the distal clavicle: a case for fixation. Injury. 1992;23(1):44–46. doi: 10.1016/0020-1383(92)90125-C. [DOI] [PubMed] [Google Scholar]
- 7.Eskola A, Vainionpää S, Pätiälä H, Rokkanen P. Outcome of operative treatment in fresh lateral clavicular fracture. Ann Chir Gynaecol. 1987;76(3):167–169. [PubMed] [Google Scholar]
- 8.Fann CY, Chiu FY, Chuang TY, Chen CM, Chen TH. Transacromial Knowles pin in the treatment of Neer type 2 distal clavicle fractures. A prospective evaluation of 32 cases. J Trauma. 2004;56(5):1102–1106. doi: 10.1097/01.TA.0000082649.57981.F9. [DOI] [PubMed] [Google Scholar]
- 9.Faraj AA, Ketzer B. The use of the hook-plate in the management of acromioclavicular injuries. Report of ten cases. Acta Orthop Belg. 2001;67(5):448–451. [PubMed] [Google Scholar]
- 10.Flinkkilä T, Ristiniemi J, Hyvönen P, Flinkkilä HM. Surgical treatment of unstable fractures of the distal clavicle: a comparative study of Kirschner wire and clavicular hook plate fixation. Acta Orthop Scand. 2002;73(1):50–53. doi: 10.1080/000164702317281404. [DOI] [PubMed] [Google Scholar]
- 11.Fung M, Kato S, Barrance PJ, Elias J, McFarland EG, Nobuhara K, Chao EY. Scapular and clavicular kinematics during humeral elevation: a study with cadavers. J Shoulder Elbow Surg. 2001;10(3):278–285. doi: 10.1067/mse.2001.114496. [DOI] [PubMed] [Google Scholar]
- 12.Hackenbruch W, Regazzoni P, Schwyzer K. Surgical treatment of lateral clavicular fracture with the “clavicular hooked plate”. Z Unfallchir Versicherungsmed. 1994;87(3):145–152. [PubMed] [Google Scholar]
- 13.Haidar SG, Krishnan KM, Deshmukh SC. Hook plate fixation for type II fractures of the lateral end of the clavicle. J Shoulder Elbow Surg. 2006;15(4):419–423. doi: 10.1016/j.jse.2005.11.012. [DOI] [PubMed] [Google Scholar]
- 14.Hessmann M, Kirchner R, Baumgaertel F, Gehling H, Gotzen L. Treatment of unstable distal clavicular fractures with and without lesions of the acromioclavicular joint. Injury. 1996;27(1):47–52. doi: 10.1016/0020-1383(95)00156-5. [DOI] [PubMed] [Google Scholar]
- 15.Jupiter JB, Leffert RD. Non-union of the clavicle. Associated complications and surgical management. J Bone Jt Surg Am. 1987;69(5):753–760. [PubMed] [Google Scholar]
- 16.Kashii M, Inui H, Yamamoto K. Surgical treatment of distal clavicle fractures using the clavicular hook plate. Clin Orthop Relat Res. 2006;447:158–164. doi: 10.1097/01.blo.0000203469.66055.6a. [DOI] [PubMed] [Google Scholar]
- 17.Kona J, Bosse MJ, Staeheli JW, Rosseau RL. Type II distal clavicle fractures: a retrospective review of surgical treatment. J Orthop Trauma. 1990;4(2):115–120. doi: 10.1097/00005131-199004020-00002. [DOI] [PubMed] [Google Scholar]
- 18.Lee YS, Lau MJ, Tseng YC, Chen WC, Kao HY, Wei JD. Comparison of the efficacy of hook plate versus tension band wire in the treatment of unstable fractures of the distal clavicle. Int Orthop. 2009;33(5):1401–1405. doi: 10.1007/s00264-008-0696-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lyons FA, Rockwood CA., Jr Migration of pins used in operations on the shoulder. J Bone Jt Surg Am. 1990;72(8):1262–1267. [PubMed] [Google Scholar]
- 20.Meda PV, Machani B, Sinopidis C, Braithwaite I, Brownson P, Frostick SP. Clavicular hook plate for lateral end fractures: a prospective study. Injury. 2006;37:277–283. doi: 10.1016/j.injury.2005.10.017. [DOI] [PubMed] [Google Scholar]
- 21.Muramatsu K, Shigetomi M, Matsunaga T, Murata Y, Taguchi T. Use of the AO hook-plate for treatment of unstable fractures of the distal clavicle. Arch Orthop Trauma Surg. 2007;127(3):191–194. doi: 10.1007/s00402-006-0284-5. [DOI] [PubMed] [Google Scholar]
- 22.Neer CS., 2nd Fractures of the distal third of the clavicle. Clin Orthop Relat Res. 1968;58:43–50. [PubMed] [Google Scholar]
- 23.Neviaser RJ. Injuries to the clavicle and acromioclavicular joint. Orthop Clin North Am. 1987;18(3):433–438. [PubMed] [Google Scholar]
- 24.Nordqvist A, Petersson C, Redlund-Johnell I. The natural course of lateral clavicle fracture. 15 (11–21) year follow-up of 110 cases. Acta Orthop Scand. 1993;64(1):87–91. doi: 10.3109/17453679308994539. [DOI] [PubMed] [Google Scholar]
- 25.Schmittinger K, Sikorski A. Experiences with the Balser plate in dislocations of the acromioclavicular joint and lateral fractures of the clavicle. Aktuelle Traumatol. 1983;13(5):190–193. [PubMed] [Google Scholar]
- 26.Yamaguchi H, Arakawa H, Kobayashi M. Results of Bosworth method for unstable fractures of the distal clavicle. Int Orthop. 1998;22(6):366–368. doi: 10.1007/s002640050279. [DOI] [PMC free article] [PubMed] [Google Scholar]