Abstract
It is a great challenge to spare the upper limb with a malignant or invasive benign bone tumour of the shoulder girdle. We retrospectively analysed 35 patients with bone tumours of the shoulder girdle treated with various limb salvage procedures. The tumours included 25 primary malignancies, three metastases and seven giant cell tumours which involved the proximal humerus in 21 patients, scapula in 12 and clavicle in two. The reconstruction procedures included eight prosthetic replacements, four devitalised tumorous bone grafts, three osteoarticular allografts, two autogenous fibular grafts, one intramedullary cemented nail, three Tikhoff-Linberg procedures, two replantation of shortened arms, and four humeral head suspensions. Six partial scapulectomies and two lateral clavicectomies needed no bone reconstruction. With an average follow-up of 71 months, local recurrences occurred in four cases and systemic metastases in six. Nine patients died and 23 remained disease free. The five year Kaplan-Meier survival rate of 28 patients with malignancies was 69.5%. The average Musculoskeletal Tumour Society (MSTS) functional score was 77% (range 40–100%) in all patients.
Introduction
The shoulder girdle, consisting of the proximal humerus, scapula, 1/3 lateral clavicle and the surrounding soft tissue, is the third most common site of predilection for bone tumours [1]. In the shoulder girdle, the proximal humerus is the most common site, followed in descending order by scapula and clavicle. The treatment of malignant or invasive benign bone tumours of the shoulder girdle is a great challenge to orthopaedic oncologists. As a result, before the 1970s, the forequarter amputation and shoulder disarticulation were the main treatment for malignant bone tumours of the shoulder girdle. With better understanding of the biological behaviour of musculoskeletal tumours, application of effective adjuvant therapy and the development of bone defect reconstruction, 80–90% of malignant tumours of the shoulder girdle can be safely resected through some limb salvage procedures. In this paper, we investigate the clinical and functional outcomes of limb salvage operations for bone tumours of the shoulder girdle.
Materials and methods
From January 1993 to December 2007, 35 patients with malignant or aggressive benign bone tumours of the shoulder girdle, including 24 males and 11 females with a mean age of 34 years (range 12–74 years), were treated with limb salvage operations. The tumours involved the proximal humerus in 21 patients, scapula in 12 and clavicle in two. Preoperatively, in addition to general routine examinations and X-ray radiography, CT and MRI scanning on the tumour sites and ECT scanning were performed in all the patients. Angiography was added if necessary. Through an evaluation of these examinations, the local and systemic tumour extent was determined, especially whether or not the neurovascular bundle and rotator cuff had been involved. Needle biopsy was performed in 30 patients, of which three patients had negative results and needed open biopsy. According to clinical features, imaging and pathological examinations, the diagnoses and their Enneking surgical classification were ten osteosarcomas (all IIB stage), seven chondrosarcomas (5 IB stage, 2 IIA stage), three malignant fibrous histiocytomas (all IIB stage), three Ewing’s sarcomas (all IIB stage), one fibrosarcoma (IIB stage), one myeloma (IIA stage), seven giant cell tumours (five recurrent and two combined pathological fractures) and three metastases (the primary malignancies were renal, thyroid and lung carcinoma). Five patients had developed pathological fractures (Table 1).
Table 1.
Histological type and anatomical location of bone tumours of the shoulder girdle
| Tumour | Proximal humerus | Scapula | Clavicle | Total |
|---|---|---|---|---|
| Osteosarcoma | 7 | 3 | - | 10 |
| Chondrosarcoma | 5 | 1 | 1 | 7 |
| Malignant fibrous histiocytoma | 2 | 1 | - | 3 |
| Ewing’s sarcoma | 1 | 1 | 1 | 3 |
| Fibrosarcoma | 1 | - | - | 1 |
| Myeloma | 1 | - | - | 1 |
| Bone giant cell tumour | 4 | 3 | - | 7 |
| Metastasis | - | 3 | - | 3 |
| Total | 21 | 12 | 2 | 35 |
As for other anatomical sites, limb salvage procedures for bone tumours of the shoulder girdle comprise three steps: complete resection of tumours, reconstruction of bone defects and good soft tissue covering. According to the surgical classification system proposed by Malawer et al. [2], tumour resections were classified as 19 type-I, six type-II, four type-III, one type-IV, one type-V and one type-VI. Based on the status of the abduction system of the shoulder (deltoid and rotator cuff), each type was divided into two subtypes: A, whereby abductor muscles were preserved well in 12 patients; and B, where abductor muscles were removed partly or completely in 20 patients. The remaining three cases were lateral clavicle resections in two and single glenoid resection in one. All tumours were resected with wide margins, except for two resections which just reached marginal margins because the tumours were too large to resect widely.
Following resection of the bone tumour, the reconstruction of bone defects depended upon factors such as the patients’ economic status, the tumour type and extension, surgeon’s skills, and the availability of instruments. Reconstruction included eight custom-made tumour prostheses, four alcohol devitalized bone replantations, three osteoarticular allografts, two autogenous fibular grafts, one spacer replacement made from intramedullary nail and bone cement, three classic or modified Tikhoff-Linberg procedures and residual humerus suspension, two segmental limb resections and shortened arm replantations, and four humeral head suspension. Six partial scapulectomies and two lateral clavicectomies needed no bone reconstruction. Soft tissue reconstruction, whose key points were reconstruction of the abduction system and preservation of shoulder stability, was completed mainly through crossed suture and reattachment of the residual muscles around the shoulder girdle to provide static and dynamic stability. The latissimus dorsi musculocutaneous flaps were needed in two patients because too much soft tissue was resected (Figs. 1, 2, and 3).
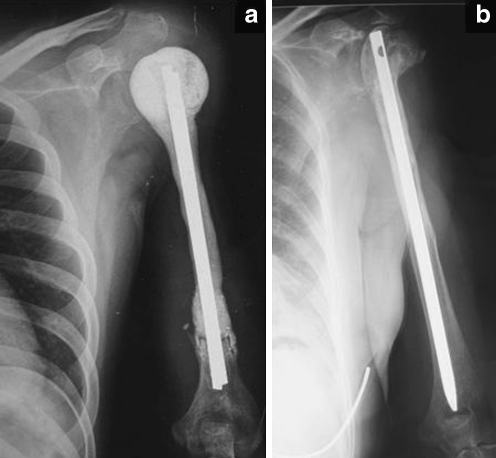
Fig. 1.
Two reconstructive methods after proximal humerus resection (type I resection). a Cemented intramedullary nail acted as a spacer for osteosarcoma of proximal humerus. b Postoperative 15.5-year radiograph of the osteoarticular allograft reconstruction for bone giant cell tumor of proximal humerus shows good union, collapsed humeral head and subsided intramedullary nail
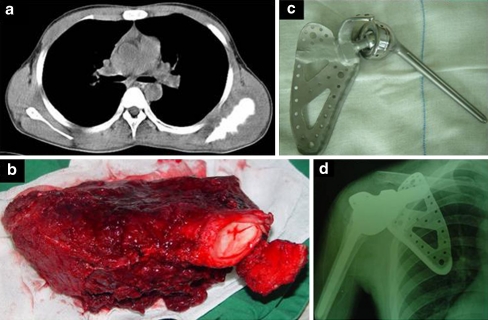
Fig. 2.
One 14-year-old patient with osteosarcoma of the left scapula (a) was treated with total scapulectomy (type III resection) and inverted tumor prosthetic reconstruction. b Resected specimen. c The tumor prosthesis. d Postoperative plain radiograph
Fig. 3.
A patient presented with giant cell tumor of the left humerus accompanied with pathologic fracture. The proximal humerus was resected widely and a tumor endoprosthesis was implanted. a Anteroposterior plain radiograph. b Magnetic resonance imaging (T1WI). c CT three-dimensional reconstruction imaging. d The tumor endoprosthesis was placed and suspended from the residual articular capsule (yellow arrow) with the tendon of the long head of biceps brachii (white arrow). e Postoperative radiograph 1 year later shows good position of endoprosthesis
Postoperatively, a Velpeau dressing was applied to immobilise the involved shoulder for one to two weeks, and then a sling was used for a further two to three weeks. Simultaneous functional exercises of hand, wrist and elbow were started as soon as possible. After the soft tissue had healed and the shoulder joint stabilised, the passive and active motion was started. All the patients were instructed on their functional exercises and their limb function was evaluated according to the MSTS scoring system in regular follow-up. The patients with osteosarcoma, malignant fibrous histiocytoma and Ewing’s sarcoma were treated with neo-adjuvant chemotherapy. The patients with myeloma and metastatic lesions were given other therapies by physicians of related departments.
Results
The postoperative follow-up was done at an out-patient clinic or via telephone interview or letters. The average follow-up period was 71 (range 6–186) months. The patients were examined for complications and oncological and functional outcomes.
Complications
Wound infection or dehiscence occurred in four patients and resolved after dressing change or debridement. Allograft bone fracture occurred in one case five years later and was treated by internal fixation with bone autograft. Collapse and absorption of an allograft humeral head was accompanied by intramedullary nail protrusion in one patient 15.5 years later and was treated by removal of the nail (Fig. 1b). Temporary radial nerve palsy occurred in two cases, both of which recovered three months later, and shoulder subluxation developed in three, was asymptomatic and needed no management.
Oncological outcome
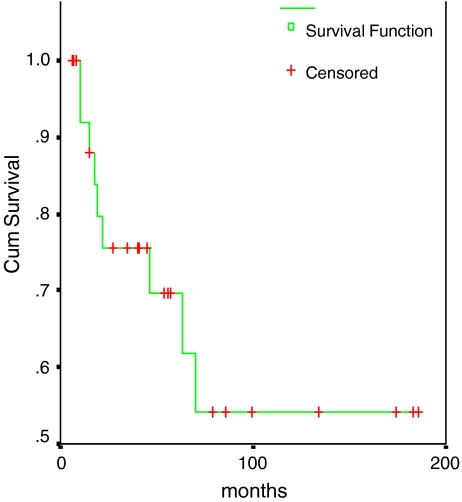
Local recurrences occurred in two patients with osteosarcoma, of these one was treated by local excision and had no evidence of disease and the other needed shoulder disarticulation and died after local relapse two years later. Local recurrences accompanied with distant metastases occurred in two cases, of these one with chondrosarcoma was treated by resection of the recurrent and lung metastatic lesions and had no evidence of disease, and the other with osteosarcoma opted out of therapy and died three months later. Four patients had lung metastases, of these one with malignant fibrous histiocytoma had no evidence of disease after metastasectomies, one with osteosarcoma was living with metastases, one with Ewing’s sarcoma and one with osteosarcomas abandoned therapy and died of their diseases. Three patients with metastases died of primary tumours within one to two years after operation. One with myeloma died of haematopoiesis failure and one elderly patient died of other diseases. Thus, there were 23 disease-free survivals at the latest follow-up. Through Kaplan-Meier survival analysis of SPSS 10.0, the five-year overall survival rate of 28 patients with malignant tumours was 69.5% (Fig. 4).
Fig. 4.
Kaplan–Meier curves showing the five-year survival rate of patients with malignant tumours of the shoulder girdle
Functional outcome
The remaining upper limb function was evaluated according to the MSTS functional evaluation system for the upper limb which consists of six items (pain, function, emotional acceptance, position of the hand, manual dexterity, and lifting ability). The mean overall MSTS score was 77% (range 40–100%) in 35 patients. Respectively, the scores were 88% (range 77–100%) in eight cases with uninvolved glenohumeral joints (six partial scapulectomies and two partial clavicectomies), 78% (range 57–90%) in 18 cases with tumour resection and reconstruction (eight custom-made prosthesis replacements, five osteoarticular auto- or allo-grafts, four devitalised bone replantations, one spacer replacement made of bone cement and nail), and 63% (range 40–77%) in nine patients with no bone reconstruction (shortened arm replantation and humeral head suspension; Table 2).
Table 2.
Type of resection, type of reconstruction, and functional outcomes of 35 bone tumours treated by a limb-sparing resection of the shoulder girdle
| Resection type | Tumour location | Operation and reconstruction methods | Cases | MSTS score |
|---|---|---|---|---|
| I | Proximal humerus | Prosthetic replacement | 7 | 70% (60–87%) |
| Devitalised tumour bone replantation | 4 | 84% (77–90%) | ||
| Osteoarticular allograft | 3 | 70%, 73%, 87% | ||
| Autogenous fibular graft | 2 | 80%, 83% | ||
| Cemented centromedullary nail | 1 | 57% | ||
| Resection of tumorous bone and replantation of shortening arm | 2 | 63%, 77% | ||
| II | Scapula | Partial scapulectomy | 6 | 85% (77–93%) |
| III | Scapula | Prosthetic replacement | 1 | 77% |
| Humeral head suspension | 3 | 57%, 67%, 63% | ||
| IV | Scapula | Modified Tikhoff-Linberg procedure | 1 | 67% |
| V | Proximal humerus | Modified Tikhoff-Linberg procedure | 1 | 73% |
| VI | Proximal humerus | Classical Tikhoff-Linberg procedure | 1 | 40% |
| Unclassified | Scapula | Resection of glenoid cavity, humeral head suspension | 1 | 73% |
| Clavicle | Resection of tumorous bone | 2 | 100%, 97% |
Discussion
Tumours of the shoulder girdle are always adjacent to the neurovascular bundle, and the conflict between shoulder stability and dexterity is difficult to resolve. Local resection of bone and muscle might result in poorer anticipated functional outcomes and place the patient in jeopardy of a local recurrence. Thus, it has long been generally considered that local resection of malignant bone tumours of the shoulder girdle is dangerous [3]. With improved survival rates of patients with sarcomas, the negative effects of radical ablative resection become more and more salient, which motivates the investigation of a less aggressive surgical approach. At present, various limb salvage procedures have been tried to retain the functional limb while the tumour control is not compromised.
In order to describe and compare the tumour resection scope and therapeutic outcomes, Enneking et al. [4] developed a system in 1990 which attempted but could not adequately express the surgical margins, the relationship of the tumour to anatomical compartments, the status of the glenohumeral joint and abductor mechanism and the magnitude of the surgical procedure. Then, in 1991, Malawer et al. [2] proposed a new classification system which was based solely on the structures removed, reflected the type of resection and its relationship to the glenohumeral joint, and indicated a progressive increase in the magnitude of the surgical procedure. Their classification involves six types and, according to the status of the abductor mechanism, each type is subdivided into A, intact, and B, partial or complete resection. The classification system by Malawer et al. is easy to use but information-rich; thus, we employed this classification system to direct tumour resection and reconstruction of the shoulder girdle.
Interscapulothoracic resection was the first limb sparing operation which was first performed by Tikhoff in 1922, and Linberg [5] reported three cases of en bloc upper humeral interscapulothoracic resection in 1928. Therefore, the operation has been known as the Tikhoff-Linberg procedure. Classic surgery includes en bloc resection of the whole scapula, proximal humerus, lateral clavicle and surrounding soft tissue, and then replantation of the shortened limb, that is, type-VI resection. Some modified Tikhoff-Linberg procedures have been developed in order to reduce the extent of resection and improve the function of the remaining extremity, also known as type-IV and type-V resection. The prosthesis or bone graft is applied to keep the normal length of the humerus in these operations.
Following different types of bone tumour resections, many reconstructive strategies are chosen based on various factors. For partial scapulectomy (type-II resection) and clavicectomy, bony reconstruction is not needed, and only the stripped muscles should be sutured and fixed. As the glenohumeral joint is well preserved, the extremity function that is obtained is good. Gibbons et al. [6] reported the mean MSTS score was 71.6% in 14 cases with partial scapulectomy and concluded that the rotator cuff could be removed without a severe functional deficit provided that the deltoid was reattached to the scapular remnant and the trapezius. Mayil Vahanan et al. [7] also reported partial scapulectomy in eight cases and gave superior functional results to total scapulectomy. Kapoor et al. [8] concluded that no bone reconstruction was required following partial or total clavicectomy. In our group, no bone reconstruction was performed in eight cases with partial scapulectomy and partial clavicectomy and the average MSTS functional score was 88%; their daily life and work was not affected severely.
After resection of the entire scapula (type-III or -IV resection), the glenohumeral joint is damaged and the humeral head or remaining humerus can be suspended from clavicle or ribs. However, since 1992, the trend has been reconstruction with a scapular prosthesis in order to obtain better functional and cosmetic results. Pritsch et al. [9] reported the functional and cosmetic results and concluded that scapular endoprosthetic reconstruction led to better functional (78.5% VS 58.5%) and cosmetic results compared to humeral suspension. In our group, one patient with scapular prosthetic replacement achieved satisfactory functional recovery (77%). By contrast, four cases with humeral suspensions (three total scapulectomies and one glenoid cavity resection) had more compromised function (65%) and cosmetic results in terms of symmetry, neckline contour, and residual deformity. However, the expenses for scapular prostheses are so high as to limit its widespread use in developing countries.
The proximal humerus is the location where bone tumours occur most frequently in the shoulder girdle so that more attention is paid to this region for tumour resection and reconstruction. Extra-articular resection of the proximal humerus, including type-VI and -V resections, also known as classic and modified Tikhoff-Linberg resection, is indicated in patients with humeral malignancies which involve the glenohumeral joint or scapula and do not involve the neurovascular bundle. Intra-articular resection of the proximal humerus (type-I resection) is indicated when the proximal humeral tumours do not invade into the glenohumeral joint. After the tumour resection, the residual bone defect can be repaired by osteoarticular allograft, autogenous fibular graft, autogenous clavicle transposition (clavicula pro humero), devitalised tumorous bone replantation, tumour prosthesis replacement, prosthetic allograft composites, arthrodesis and flail shoulder. Every method has its advantages and disadvantages so that there is no optimal reconstructive strategy. Getty et al. [10] reported that the mean MSTS functional score was 70% in 16 patients and concluded that although an osteoarticular allograft was an option for reconstruction of the proximal humerus, they no longer routinely performed this procedure because of the extremely high rate of complications. Rödl et al. [11] reported that among 17 osteoarticular allografts, only seven survived five years and only four needed no additional surgery. They therefore believed the use of allograft in the management of high-grade malignancies should, at best, be considered a temporary solution. Kitagawa et al. [12] reported that for allograft arthrodesis, prosthetic arthroplasty and clavicula pro humero, the mean MSTS functional scores were, respectively, 83%, 76% and 72%. Rödl et al. [13] reported the functional results were the same with a mean functional score of 79% for osteoarticular allografts, clavicula pro humero and tumour prostheses. Meanwhile, they found that prosthetic replacement of the proximal humerus was the safest procedure and the clavicula pro humero procedure needed more revisions and was an alternative in some special situations. Tsukushi et al. [14] found a mean MSTS functional score of 69% in seven patients with clavicula pro humero reconstruction and concluded that this procedure was a useful method, especially in young patients and in patients with involvement of the nondominant arm. Krieg et al. [15] reported 31 patients who were treated with a non-vascularised fibular graft after resection of primary musculoskeletal tumours and concluded that this method was a simpler, less expensive and biological reconstruction with good long-term results. Wada et al. [16] used a free vascularised fibular graft as a functional spacer and a sling procedure to preserve passive scapulohumeral movement in eight patients with a mean MSTS functional score of 79%. Kassab et al. [17] reported that the mean MSTS scores and reconstructive strategies were, respectively, 88% for inverted prostheses in seven patients, 76% for composite prostheses in three, 72.6% for massive prostheses in 15, 75% for scapulohumeral arthrodeses in three and 80% for cemented intramedullary nail in one patient. They thought that the functional outcome after resection–reconstruction for the proximal humerus depended on the type of bony resection, the status of the abduction system and the reconstruction method, and they thus proposed their algorithm for reconstruction. In this group, the reconstructive strategies following proximal humerus resection and their MSTS functional scores were: cemented intramedullary nail in one case (57%), proximal humeral prostheses in seven (mean 70%), osteoarticular allografts in three (70%, 73%, 87%), tumorous bone devitalisation and replantation in four (mean 84%), and autogenous fibular graft in two (80% and 83%). The overall mean functional score was 78%. Thus, despite the small number of cases for the different reconstructions, there are many reconstructive strategies to employ after proximal humeral resection and the spared extremities can regain most of their functions in spite of the discrepant functional scores, even if the reconstructive components only act as spacers.
In the course of bone tumour resection and reconstruction of shoulder girdle, the soft tissue reconstruction and covering are especially important to functional recovery and complication prevention. After tumour resection and bone reconstruction, remaining muscles should be sutured appropriately in order to cover the implants, restore their tension, and enhance both the static and dynamic stability. In the case of excessive muscle resection, especially when the abductor mechanism is sacrificed, the salvaged joint is only a flail shoulder. But, according to Springfield [18], a flail shoulder is often the best alternative for the patient who does not need to use the hand in space. We also find that function of the elbow, wrist and hand remain in a flail limb, and can meet the requirements of daily life with the help of an orthosis or the contralateral hand.
In summary, bone tumours of the shoulder girdle can be treated mainly with various limb-salvage procedures, including prosthetic replacement, osteoarticular auto- or allo-graft, tumorous bone devitalisation and replantation, and the Tikhoff-Linberg procedure that is safe and reliable. Meticulous evaluation and planning of the extent of resection and mode of reconstruction are mandatory. Local tumour control, stable and painless shoulder reconstruction and good function of elbow and hand can be achieved in the majority of patients.
References
- 1.Creighton JJ, Peimer CA, Mindell ER, Boone DC, Karacousis CP, Douglass HO. Primary malignant tumors of the upper extremity: retrospective analysis of one hundred twenty-six cases. J Hand Surg [Am] 1985;10:805–814. doi: 10.1016/s0363-5023(85)80155-6. [DOI] [PubMed] [Google Scholar]
- 2.Malawer MM. Tumors of the shoulder girdle: technique of resection and description of a surgical classification. Orthop Clin North Am. 1991;22:7–35. [PubMed] [Google Scholar]
- 3.Sim FH, Pritchard DJ, Ivins JC. Forequarter amputation. Orthop Clin North Am. 1977;8:921–931. [PubMed] [Google Scholar]
- 4.Enneking WF, Dunham W, Gebhardt M, Malawar M, et al. A system for the classification of skeletal resections. Chir Organi Mov. 1990;75(Suppl 1):217–240. [PubMed] [Google Scholar]
- 5.Linberg BE. Interscapulo-thoracic resection for malignant tumors of the shoulder joint region. J Bone Jt Surg. 1928;10:344–349. [PubMed] [Google Scholar]
- 6.Gibbons CLMH, Bell RS, Wunder JS, et al. Function after subtotal scapulectomy for neoplasm of bone and soft tissue. J Bone Jt Surg [Br] 1998;80:38–42. doi: 10.1302/0301-620X.80B1.8183. [DOI] [PubMed] [Google Scholar]
- 7.Mayil Vahanan N, Mohanlal P, Bose JC, et al. The functional and oncological results after scapulectomy for scapular tumours: 2–16-year results. Int Orthop. 2007;31(6):831–836. doi: 10.1007/s00264-006-0261-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kapoor S, Tiwari A, Kapoor S. Primary tumours and tumorous lesions of clavicle. Int Orthop. 2008;32(6):829–834. doi: 10.1007/s00264-007-0397-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pritsch T, Bickels J, Wu CC, et al. Is scapular endoprosthesis functionally superior to humeral suspension? Clin Orthop Relat Res. 2007;456(5):188–195. doi: 10.1097/01.blo.0000238840.26423.b6. [DOI] [PubMed] [Google Scholar]
- 10.Getty PJ, Peabody TD. Complications and functional outcomes of reconstruction with an osteoarticular allograft after intra-articular resection of the proximal aspect of the humerus. J Bone Jt Surg [Am] 1999;81(8):1138–1146. doi: 10.2106/00004623-199908000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Rödl RW, Ozaki T, Hoffmann C, et al. Osteoarticular allograft in surgery for high-grade malignant tumours of bone. J Bone Jt Surg [Br] 2000;82(7):1006–1010. doi: 10.1302/0301-620X.82B7.10644. [DOI] [PubMed] [Google Scholar]
- 12.Kitagawa Y, Thai DM, Choong PF. Reconstructions of the shoulder following tumour resection. J Orthop Surg (Hong Kong) 2007;15(2):201–206. doi: 10.1177/230949900701500216. [DOI] [PubMed] [Google Scholar]
- 13.Rödl RW, Gosheger G, Gebert C, et al. Reconstruction of the proximal humerus after wide resection of tumours. J Bone Jt Surg [Br] 2002;84(7):1004–1008. doi: 10.1302/0301-620X.84B7.12989. [DOI] [PubMed] [Google Scholar]
- 14.Tsukushi S, Nishida Y, Takahashi M, et al. Clavicula pro humero reconstruction after wide resection of the proximal humerus. Clin Orthop Relat Res. 2006;447:132–137. doi: 10.1097/01.blo.0000201169.80011.ff. [DOI] [PubMed] [Google Scholar]
- 15.Krieg AH, Hefti F. Reconstruction with non-vascularised fibular grafts after resection of bone tumours. J Bone Jt Surg [Br] 2007;89(2):215–221. doi: 10.1302/0301-620X.89B2.17686. [DOI] [PubMed] [Google Scholar]
- 16.Wada T, Usui M, Isu K, et al. Reconstruction and limb salvage after resection for malignant bone tumour of the proximal humerus. A sling procedure using a free vascularised fibular graft. J Bone Jt Surg [Br] 1999;81(5):808–813. doi: 10.1302/0301-620X.81B5.9430. [DOI] [PubMed] [Google Scholar]
- 17.Kassab M, Dumaine V, Babinet A, et al. Twenty nine shoulder reconstructions after resection of the proximal humerus for neoplasm with mean 7-year follow-up. Rev Chir Orthop Reparatrice Appar Mot. 2005;91(1):15–23. doi: 10.1016/s0035-1040(05)84271-0. [DOI] [PubMed] [Google Scholar]
- 18.Springfield DS. Orthopaedic oncology. In: Sledge CB, Poss RP, editors. The year book of orthopedics. St Louis: Mosby; 1997. pp. 98–100. [Google Scholar]