Abstract
A retrospective study was conducted to evaluate displaced proximal humeral fractures treated with a non-plate head-preserving fixation and to detect factors predicting functional outcome. After a median follow-up period of 79.7 months, 105 patients with nine A-fractures, 36 B-fractures and 60 C-fractures (nine two-part-fractures, 41 three-part fractures and 55 four-part fractures) were assessed. Functional outcome was measured based on the Constant and UCLA scores. Of all patients, 70–75% had excellent or good Constant and UCLA scores. In 74% a good or satisfactory quality of initial reduction fracture was achieved. About one-fifth (21%) of the fractures showed a secondary displacement. Twenty-seven percent of the patients had signs of humeral head necrosis and 22% had implant related problems. There were significant correlations between a high final score and young age, low AO fracture severity, good quality of fracture reduction and residual osseous deformity, absence of secondary fracture displacement, implant-related complications, shoulder arthrosis and humeral head necrosis at the time of follow-up. In conclusion, the non-plate head-preserving fixation of proximal humeral fractures is an alternative treatment for displaced proximal humeral fractures. Especially in severely displaced C-fractures in older patients, non-anatomical reduction leads to a high rate of secondary displacement, residual osseous deformity and only a fair shoulder function. For these cases alternative methods such as prosthetic replacement should be chosen.
Introduction
Epidemiological studies have shown a dramatic increase of humeral head fractures of about 13% per year between 1970 and 2002, especially in the elderly population [1]. Complex three- and four-part fractures occur in more than 50% of patients older than 60 years [2]. Therefore, the management of these fractures is challenging in terms of the epidemiological trend of an aging population.
Common classifications are the Neer and AO classifications, which are based on displacement, number of fractured parts and vascularity of the proximal humerus [3, 4]. Decisions regarding the surgical treatment are often based on the surgeon’s opinion and preference and are still a significant challenge especially for complex displaced fractures [4].
Minimal invasive fixation techniques for the management of proximal humeral fractures have been promulgated by different authors [5–10]. With this technique, the reduction of the fracture is established either by closed techniques or with the aid of elevators and hook retractors that are inserted via stab incisions. The fixation is mainly performed with percutaneously inserted K-wires and/or cannulated screws. Potential advantages of this technique are less soft tissue dissection, a higher union rate, and presumably a lower incidence of humeral head necrosis. Disadvantages are inferior fracture stability and therefore delay in the initiation of physiotherapy after surgery in comparison to other internal fixation methods such as plates or nails [11]. However, the minimal invasive technique is technically demanding because the reduction of the fracture is achieved by indirect manoeuvres.
The authors performed a minimally invasive non-plate head preserving technique in which a closed reduction and stabilisation by K-wires was performed for simple fractures. Complex fractures were reduced and stabilised by a short incision and K-wires, cannulated screws or tension band wiring.
However, it is not entirely clear which types of fractures or how much displacement may be suitable for this technique. The purpose of this retrospective study was to assess the clinical and radiological outcome after proximal humerus fractures treated with a non-plate head preserving technique. In addition, we postulate that certain factors may allow the prediction of the clinical and radiological end result.
Patients and methods
We included 172 adult patients with displaced not-comminuted two-part surgical neck fractures, as well as three- and four-part-fractures including fracture dislocations of the proximal humerus. These fractures were treated with a non-plate head preserving fixation from June 1996 to March 2005 at a level one trauma centre. All patients were initially diagnosed by X-ray with anteroposterior and axillary views. Details about patients age, gender, mechanism of injury (low energy trauma, e.g. fall from a standing height, or high energy trauma), fracture type according to AO classification [4], number of fractured parts (Neer classification [3]), initial neurological or vascular deficits, and the presence of osteoporosis on the fractured side (score of Tingart) were evaluated [12]. All postoperative complications were recorded. Routinely, clinical and radiographic examinations were performed four to six weeks and three months after surgery. After a median follow-up-period of 79 months, 67 patients (39%) had died or moved and could not be contacted via telephone or mail. With informed consent of the patients and in accordance with the local institutional review board, the remaining 105 patients were available for a clinical and radiological follow-up.
Surgical technique of the non-plate head-preserving fixation and postoperative treatment:
A closed reduction of the displaced surgical neck/anatomical neck fracture was performed to reduce the shaft-head area under image intensifier control. In all displaced surgical neck fractures percutaneous stabilisation with three K-wires was performed. In all other cases minimally-invasive reduction was established. Therefore, an incision of about 5 cm was performed starting at the anterolateral corner of the acromion. After minimal dissection of the fracture the head fragment was pushed or levered to an anatomical position. Afterwards, associated fractures of the tuberosity were reduced without any direct exposure. All patients were managed with two to three K-wires for the surgical neck/anatomical neck fracture, augmented with cannulated screws for treatment of the tuberosities and occasional tension band fixation for comminuted tuberosity fractures. All patients were immobilised for three to four weeks in a sling. Passive movements of the shoulder joint without rotation of the arm were initiated on the first postoperative day out of the sling. Active motions of the elbow and the wrist were allowed. After radiological signs of bony healing were visible, the K-wires were removed under local anaesthesia four to six weeks after injury. Physiotherapy was then continued with an active range of motion program in all planes including rotation. Strengthening exercises for the deltoid and the rotator cuff muscles were than added.
Clinical and radiological evaluation:
The global shoulder function was graded with the Constant and UCLA scoring systems by an independent examiner (see Table 1) [13, 14]. The muscle power was measured with a spring balance in both shoulders using the technique described by Constant. At the time of follow-up, X-rays of the shoulders were taken in anteroposterior and axillary views. The complete sets of available X-rays were used for consensus evaluation by three experienced orthopaedic surgeons.
Table 1.
Shoulder scores grouped according to Constant-Murley and UCLA
| Rating | Constant-Murley score (max. 100 points) | UCLA score (max. 35 points) |
|---|---|---|
| Very good | 86–100 | 34–35 |
| Good | 71–85 | 28–33 |
| Fair | 56–70 | 21–27 |
| Poor | <56 | <21 |
Adapted from our recently developed radiographic score for the evaluation of proximal humeral fractures [15], we included the following parameters (Table 2): quality of fracture reduction, residual deformities of the head fragment and/or greater tuberosity at time of follow-up, secondary displacement of the fracture after surgery, implant-related complications, delayed healing or non-union, post-traumatic humeral head necrosis, and post-traumatic shoulder arthrosis.
Table 2.
Radiographic score for the evaluation of proximal humeral fractures
| Category description | Scoring |
|---|---|
| Quality of initial fracture reduction Residual bony deformities at time of follow-up | (a) Greater tuberosity below the level of the cortex or a side-to-side difference <5 mm |
| (b) No increased varus or valgus (+/-15°) of the head fragment in the anteroposterior view | |
| (c) No increased retro- or ante torsion (+/-15°) of the head fragment in the axial projection | |
| Score 0 (good): all 3 criteria (a–c) are met | |
| Score 1 (satisfactory): two of the three criteria are met | |
| Score 2 (unsatisfactory): one of the criteria is met | |
| Secondary displacement of the fracture after surgery | Score 0: Good quality of fracture reduction without change during healing period |
| Score 1: Secondary fracture displacement after initial good quality of fracture reduction | |
| Score 2: Secondary displacement of the fracture after satisfactory or unsatisfactory quality of fracture reduction | |
| Implant-related complications | Score 0: No implant related complications during healing period |
| Score 1: Implant-related impingement | |
| Score 2: Implant-related complications due to loosening, perforation or breakage | |
| Delayed healing/non-union | Score 0: Normal bony healing |
| Score 1: Fracture gap visible but stable implant fixation | |
| Score 2: Fracture gap visible and implant loosening | |
| Post-traumatic humeral head necrosis | (a) Subchondral sclerosis |
| (b) Subchondral collapse and irregularity of the head | |
| (c) Total collapse of the head and destruction of the joint | |
| Score 0 (good): none of the 3 criteria (a–c) are met | |
| Score 1 (satisfactory): one of the three criteria are met | |
| Score 2 (unsatisfactory): two of the criteria are met | |
| Post-traumatic omarthrosis | (a) Narrowing of the joint space (mild) |
| (b) Existence of osteophytes | |
| (c) Significant subchondral sclerosis | |
| Score 0: no criteria (a–c) are met | |
| Score 1: one of the three criteria apply (mild) | |
| Score 2: two of the criteria are met (severe) |
Statistical methods:
Statistical analysis was performed using JMP 7.0.2 (SAS Institute, Cary, NC, USA). The Constant score and the UCLA score were logit transformed in order to assess the Pearson correlation with age [16]. For the assessment of the association of the Constant and UCLA scores with score values we calculated Spearman’s correlation coefficient. Statistical significance was adjusted according to Bonferroni-Holm for multiple testing. Therefore only p-values less than 0.00625 were considered significant. Continuous and ordinal variables were summarised with medians and ranges. Associations between ordinal variables were calculated using the Spearman rank correlation. The nominal variables such as gender and fracture type were summarised as percentages. The results were considered to be significant at p < 0.05.
Results
Patients:
We evaluated 105 patients (median age 55 years, range 18–87), of which 59 were female (56.2%) and 46 male (43.8%). Forty-one patients (39%) had suffered a low-energy trauma and 64 patients (61%) a high-energy trauma. The median follow-up period was 79.7 months (range 20–125 months).
At the time of injury, nine of the 105 patients (9%) had local nerve palsy without any vascular injuries. During the follow-up period, the nerve palsy completely resolved. According to the AO and Neer classifications, nine A-fractures, 36 B-fractures and 60 C-fractures comprising nine two-part fractures, 41 three-part fractures and 55 four-part fractures were included in the study. Eight patients had suffered a fracture dislocation. Seventy-eight patients (74%) had an accompanying osteoporosis.
After initial fracture stabilisation in a minimally invasive non-plate head-preserving technique, three revisions for haematoma of the injured shoulder (n = 2) or a low-grade infection were performed.
Shoulder function scoring:
At time of the follow-up examination, the mean Constant score for the fractured shoulder was 80 points (range 14–100, median 91 points) and for the non-injured shoulder 97 points (range 54–100 points, median 100 points). Seventy-four of 105 patients (70%) had an excellent or good Constant score of the injured shoulder whereas 31 patients (30%) showed a fair or poor Constant score.
The fractured shoulder registered a mean UCLA score of 30 points (range 3–35 points, median 34 points), and the mean score for the contra-lateral shoulder was 34.7 points (range 27–35 points, median score 35 points). Seventy-nine of the patients (75%) achieved a good or excellent UCLA score, and 26 (25%) showed a fair or poor UCLA score.
Radiological assessment:
The radiological assessment showed a good or satisfactory quality of initial fracture reduction in 78 of the 105 cases (74%). In 27 of the 105 fractures (26%) with an unsatisfactory quality of initial fracture reduction there were mainly C-fractures and fracture dislocations (n = 21/60, 35%) rather than A or B-fractures (n = 6/45, 13.3%) (p < 0.05).
Overall, 22 of the 105 fractures (21%) showed a secondary fracture displacement. Of these 22 fractures one fracture initially had a good reduction quality, and 21 fractures initially had a satisfactory or unsatisfactory reduction quality (p < 0.05).
Eighty-two (78%) of the patients showed no implant-related problems during the healing period. In 23 of the 105 fractures (22%), implant-related problems occurred, mainly in C-fractures (28%, n = 17/60) and occasionally in A -or B-fractures (13.3%, n = 6/45) (p < 0.05). Furthermore, these implant-related problems occurred in 36% of fractures (n = 18/50) that were initially not good quality reductions, whereas only 9% near anatomically reduced fractures (n = 5/55) had suffered implant-related problems (p < 0.05).
After completed bony healing, the radiological fracture assessment at follow-up showed a good or satisfactory quality of fracture alignment in 75 of 105 fractures. In 30 cases there was a residual deformity of the head fragment (>15°) and/or tuberosity deformity of more than 5 mm.
Altogether, 28 patients (27%) had signs of humeral head necrosis. Eleven of these 28 patients showed mild (11%) and 17 (16%) severe signs of humeral head necrosis (Table 2). The presence of humeral head necrosis was significantly associated with four-part fractures and fracture-dislocations (40%, n = 22/55) rather than with two-part and three-part-fractures (12%, n = 6/50) (p < 0.05). Severity of humeral head necrosis was also associated with fracture severity according to AO classification (A- and B-fractures, 3.8%, n = 5/45; C-fractures 38.3%, n = 23/60) (p < 0.05). Furthermore, the presence of humeral head necrosis was higher in those 50 fractures (46%, n = 23) that were not good quality reductions rather than in those 55 fractures (10%, n = 5) that were reduced near anatomically (p < 0.05).
Seventeen of 105 patients (17%) had signs of post-traumatic omarthrosis (n = 7, 7% mild; n = 10, 10% severe) (see Table 3).
Table 3.
Relevant parameters including the rate, corresponding median/mean Constant and UCLA scores and Spearman ρ-values
| Description | n | Constant score (median/mean) | Spearman ρ (p-value) | UCLA score (median/mean) | Spearman ρ (p-value) |
|---|---|---|---|---|---|
| Neer 2 parts | 9 | 99/92 | −0.131 | 35/33 | −0.082 |
| Neer 3 parts | 41 | 90/81 | (0.1830) | 34/30 | 0.4048 |
| Neer 4 parts | 55 | 91/77 | 34/29 | ||
| AO A | 9 | 99/92 | −0.266 | 35/33 | −0.253 |
| AO B | 36 | 95/86 | (0.0061) | 35/32 | 0.0091 |
| AO C | 60 | 85/75 | 33/28 | ||
| Quality fracture reduction: Good | 55 | 98/90 | −0.486 | 35/33 | −0.516 |
| Quality fracture reduction: satisfactory | 23 | 93/80 | (<0.0001) | 35/30 | <0.0001 |
| Quality fracture reduction: unsatisfactory | 27 | 59/60 | 24/24 | ||
| Secondary displacement fracture | 22 | 51/66 | −0.574 | 27/27 | −0.612 |
| No secondary displacement fracture | 83 | 96/88 | (<0.0001) | 35/32 | <0.0001 |
| Implant-related complications | 23 | 54/54 | −0.483 | 23/22 | −0.517 |
| No implant-related complications | 82 | 94/87 | (<0.0001) | 35/32 | <0.0001 |
| Delayed healing/non-union | 5 | 20/34 | −0.315 | 14/14 | −0.331 |
| No delayed healing/non-union | 100 | 93/82 | (0.0011) | 35/31 | 0.0006 |
| Osseous deformity at follow-up | 51 | 77/72 | −0.493 | 30/32 | −0.529 |
| No osseous deformity at follow-up | 54 | 98/90 | (<0.0001) | 35/28 | <0.0001 |
| Omarthrosis at follow-up | 18 | 47/51 | −0.523 | 20/21 | −0.549 |
| No omarthrosis at follow-up | 87 | 94/87 | (<0.0001) | 35/32 | <0.0001 |
| Humeral head necrosis | 28 | 64/61 | −0.558 | 25/25 | −0.508 |
| No humeral head necrosis | 77 | 95/88 | (<0.0001) | 35/32 | <0.0001 |
Statistical results:
There were significant correlations between the logit transformed final Constant score (−0.341) and the UCLA score of the injured shoulder (−0.348 ) and the age of the patient at time of injury (p = 0.0004; p = 0.00031). There was a significant correlation between the final Constant and UCLA score of the injured shoulder and the fracture topography according to AO classification (ABC), the existence of fracture dislocation, the quality of initial reduction of the fracture, secondary fracture displacement after surgery, presence of implant-related complications, delayed or non-union of the fracture, residual bony deformity at follow-up, presence of humeral head necrosis and shoulder arthrosis. There was no significant association between the result of the Constant and UCLA scores and the parameters including gender, mechanism of injury, classification according to Neer, and osteoporosis at time of injury (see Table 2).
Discussion
This study assessed the clinical and radiological outcome after proximal humerus fractures that were treated with a non-plate head preserving technique. Our data showed that 70–75% of the patients had excellent or good Constant and UCLA scores whereas fair or unsatisfactory results occurred in 25–30% of the patients. We also showed that an excellent or good final outcome was associated with young age at time of injury, low fracture severity according to AO but not Neer, good quality of initial fracture reduction, no secondary fracture displacement, no implant-related complications, low residual osseous deformity and absence of humeral head necrosis, arthrosis and delayed/non-union healing.
A general consensus regarding the treatment algorithm of displaced proximal humeral fractures has not been established [17]. Whereas several studies support either conservative or surgical therapy [18–20], it is nevertheless generally accepted that initial fracture reduction and early postoperative functional therapy are relevant factors for a satisfactory end result [21–23].
This study showed that several factors influence the functional outcome. Whereas some factors such as fracture severity and patient situation (such as age) are pre-defined, other factors such as good initial and maintained fracture reduction, low residual osseous deformity and the absence of implant-related complications are to some extent determined by the treatment.
Our study showed that displaced proximal humeral A- and B-fractures can be treated with a minimally invasive non-plate head preserving technique, with the potential achievement of near anatomical fracture reconstruction. Good initial reconstruction (less than 15° deviation) led to significantly better clinical results, especially when the reconstruction was maintained. Whereas studies on radiographic analysis are rare, one study showed a good reduction quality even of severe (C-) fractures in 72%. However, the scoring system was liberal because a good reduction quality was defined as less than 45° angulation or 1 cm displacement [26]. In contrast, our study showed that a fracture reduction quality of less than 15° remaining angulation and less than 5-mm tuberosity displacement presaged an excellent or good functional end result.
Similar to our results, Calvo et al. also showed a significant association between any residual deformity and the functional score result at follow-up [26]. In contrast, after initial anatomical reduction, only one fracture showed a secondary displacement. Surprisingly, the rate of secondary displacement and implant-related problems in the non anatomically reduced fractures were 42% and 36%, respectively, and were associated with fair to worse functional end results.
Minimal invasive techniques are recommended because soft-tissue dissection is minimal and blood supply to the humeral head is preserved, potentially leading to lower rate of humeral head necrosis [24, 25]. In our study, we observed 16% severe humeral head necrosis with collapse of the head. Humeral head necroses were predominately detected in severe fracture types (C-fractures, four-part-fractures and fracture dislocations) and were detected in those fractures in which a good reduction result was not established. In other studies, a rate of 3.2–26% after a mean follow-up 13.6–36 months is described [5, 9, 26]. Although none of these patients with a humeral head necrosis was treated with a secondary humeral head replacement, the Constant and UCLA score results were low. Therefore, the complication of humeral head necrosis seems to be influenced by fracture severity and the surgical trauma. Resch et al. pointed out that it is important to study the relationship and amount of displacement of the various fragments to each other and to identify possible intact soft tissue links between the fragments. This knowledge is important to gain benefit from the ligamentotaxis to achieve and preserve anatomical reduction after fixation and reduce the risk of humeral head necrosis in the follow-up period. Therefore, good indications for minimally invasive and percutaneus reduction are A- and B-fractures and displaced humeral head fractures with or without impaction (C1- and C2-fractures). Humeral head fractures with severe displacement or fracture dislocations (C2- and C3-fractures) are less good indications, which can be supported by the results of our study [8].
In conclusion, the non-plate head-preserving fixation of proximal humeral fractures is an alternative treatment for displaced proximal humeral fractures. But this technique is only suitable for younger patients with good bone stock and if a near anatomical fracture reduction was achieved prevented secondary displacement and implant-related problems and long-term complications such as humeral head necrosis (Fig. 1). In contrast, especially for severely displaced C-fractures in older patients, non-anatomical reduction leads to a high rate of secondary displacement, residual osseous deformity and only a fair shoulder function. For these cases alternative methods such as prosthetic replacement should be chosen.
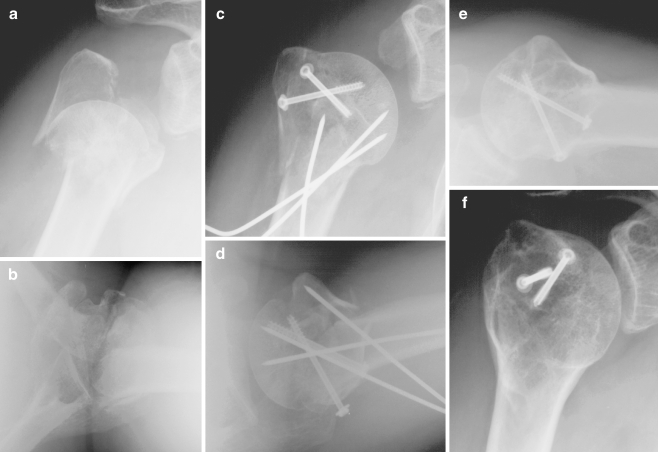
Fig. 1.
a–f Four-part-fracture in a 52-year-old male treated with minimally invasive reduction and K-wire and screw fixation. After 68 months he had a Constant-Murley score of 97 points and a UCLA score of 34 points
Acknowledgments
Conflict of interest The authors declare that they have no conflicts of interest.
Contributor Information
Christian Bahrs, Email: C.Bahrs@gmx.de.
Andreas Badke, Phone: +49-7071-6060, FAX: +49-7071-6061002, Email: abadke@bgu-tuebingen.de.
Bernd Rolauffs, Email: brolauffs@bgu-tuebingen.de.
Kuno Weise, Email: kweise@bgu-tuebingen.de.
Sebastian Zipplies, Email: s.zipplies@gmx.net.
Klaus Dietz, Email: klaus.dietz@uni-tuebingen.de.
Christoph Eingartner, Email: Christoph.Eingartner@ckbm.de.
References
- 1.Palvanen M, Kannus P, Niemi S, Parkkari J. Update in the epidemiology of proximal humeral fractures. Clin Orthop Relat Res. 2006;442:87–92. doi: 10.1097/01.blo.0000194672.79634.78. [DOI] [PubMed] [Google Scholar]
- 2.Court-Brown CM, Garg A, McQueen MM. The epidemiology of proximal humeral fractures. Acta Orthop Scand. 2001;72(4):365–371. doi: 10.1080/000164701753542023. [DOI] [PubMed] [Google Scholar]
- 3.Neer CS., 2nd Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am. 1970;52(6):1077–1089. [PubMed] [Google Scholar]
- 4.Jakob R, Kristiansen T, Mayo K, Ganz R, Muller ME. Classifications and aspects of treatment of fractures of the proximal humerus. In: Bateman JE, Welsh RP, editors. Surgery of the shoulder. Philadelphia: CV Mosby Co; 1984. pp. 330–343. [Google Scholar]
- 5.Keener JD, Parsons BO, Flatow EL, Rogers K, Williams GR, Galatz LM. Outcomes after percutaneous reduction and fixation of proximal humeral fractures. J Shoulder Elbow Surg. 2007;16(3):330–338. doi: 10.1016/j.jse.2006.09.006. [DOI] [PubMed] [Google Scholar]
- 6.Fenichel I, Oran A, Burstein G, Perry Pritsch M. Percutaneous pinning using threaded pins as a treatment option for unstable two- and three-part fractures of the proximal humerus: a retrospective study. Int Orthop. 2006;30(3):153–157. doi: 10.1007/s00264-005-0058-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Soete PJ, Clayson PE, Costenoble VH. Transitory percutaneous pinning in fractures of the proximal humerus. J Shoulder Elbow Surg. 1999;8(6):569–573. doi: 10.1016/S1058-2746(99)90091-5. [DOI] [PubMed] [Google Scholar]
- 8.Resch H, Hubner C, Schwaiger R. Minimally invasive reduction and osteosynthesis of articular fractures of the humeral head. Injury. 2001;32(Suppl 1):SA25–SA32. doi: 10.1016/s0020-1383(01)00058-4. [DOI] [PubMed] [Google Scholar]
- 9.Jaberg H, Warner JJ, Jakob RP. Percutaneous stabilization of unstable fractures of the humerus. J Bone Joint Surg Am. 1992;74(4):508–515. [PubMed] [Google Scholar]
- 10.Lau TW, Leung F, Chan CF, Chow SP (2007) Minimally invasive plate osteosynthesis in the treatment of proximal humeral fracture. Int Orthop 31(5):657–664 [DOI] [PMC free article] [PubMed]
- 11.Koval KJ, Blair B, Takei R, Kummer FJ, Zuckerman JD. Surgical neck fractures of the proximal humerus: a laboratory evaluation of ten fixation techniques. J Trauma. 1996;40(5):778–783. doi: 10.1097/00005373-199605000-00017. [DOI] [PubMed] [Google Scholar]
- 12.Tingart MJ, Apreleva M, Stechow D, Zurakowski D, Warner JJ. The cortical thickness of the proximal humeral diaphysis predicts bone mineral density of the proximal humerus. J Bone Joint Surg Br. 2003;85(4):611–617. doi: 10.1302/0301-620X.85B4.12843. [DOI] [PubMed] [Google Scholar]
- 13.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–164. [PubMed] [Google Scholar]
- 14.Ellman H, Hanker G, Bayer M. Repair of the rotator cuff. End-result study of factors influencing reconstruction. J Bone Joint Surg Am. 1986;68(8):1136–1144. [PubMed] [Google Scholar]
- 15.Bahrs C, Oehm J, Rolauffs B, Eingartner C, Weise K, Dietz K, Helwig P. T-plate osteosynthesis—an obsolete osteosynthesis procedure for proximal humeral fractures? Middle-term clinical and radiological results. Z Orthop Ihre Grenzgeb. 2007;145(2):186–194. doi: 10.1055/s-2007-965169. [DOI] [PubMed] [Google Scholar]
- 16.Ashton WD. The logit transformation: with special reference to its uses in bioassay. Griffin's statistical monographs and courses. 1972;32 VIII:87 S. [Google Scholar]
- 17.Misra A, Kapur R, Maffulli N. Complex proximal humeral fractures in adults—a systematic review of management. Injury. 2001;32(5):363–372. doi: 10.1016/S0020-1383(00)00242-4. [DOI] [PubMed] [Google Scholar]
- 18.Hessmann MH, Rommens PM. Osteosynthesis techniques in proximal humeral fractures. Chirurg. 2001;72(11):1235–1245. doi: 10.1007/s001040170026. [DOI] [PubMed] [Google Scholar]
- 19.Zyto K, Ahrengart L, Sperber A, Tornkvist H. Treatment of displaced proximal humeral fractures in elderly patients. J Bone Joint Surg Br. 1997;79(3):412–417. doi: 10.1302/0301-620X.79B3.7419. [DOI] [PubMed] [Google Scholar]
- 20.Ilchmann T, Ochsner PE, Wingstrand H, Jonsson K. Non-operative treatment versus tension-band osteosynthesis in three- and four-part proximal humeral fractures. A retrospective study of 34 fractures from two different trauma centers. Int Orthop. 1998;22(5):316–320. doi: 10.1007/s002640050268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gerber C, Hersche O, Berberat C. The clinical relevance of posttraumatic avascular necrosis of the humeral head. J Shoulder Elbow Surg. 1998;7(6):586–590. doi: 10.1016/S1058-2746(98)90005-2. [DOI] [PubMed] [Google Scholar]
- 22.Hertel R. Fractures of the proximal humerus in osteoporotic bone. Osteoporos Int. 2005;16(Suppl 2):S65–S72. doi: 10.1007/s00198-004-1714-2. [DOI] [PubMed] [Google Scholar]
- 23.Fuchtmeier B, Brockner S, Hente R, Maghsudi M, Nerlich M, Prantl L (2007) The treatment of dislocated humeral head fractures with a new proximal intramedullary nail system. Int Orthop 32(6):759–765 [DOI] [PMC free article] [PubMed]
- 24.Jaberg H, Jakob RP. Compound fractures of the proximal humerus. Orthopade. 1987;16(4):320–335. [PubMed] [Google Scholar]
- 25.Munst P, Kuner EH. Osteosynthesis in dislocated fractures of the humerus head. Orthopade. 1992;21(2):121–130. [PubMed] [Google Scholar]
- 26.Calvo E, Miguel I, Cruz JJ, Lopez-Martin N. Percutaneous fixation of displaced proximal humeral fractures: indications based on the correlation between clinical and radiographic results. J Shoulder Elbow Surg. 2007;16(6):774–781. doi: 10.1016/j.jse.2007.03.019. [DOI] [PubMed] [Google Scholar]