Abstract
The Acutrak plus compression screw (APCS) (Acumed Inc., Beaverton, OR, USA) is an intramedullary implant which can achieve stable fixation with minimum soft tissue dissection. The characteristics of the APCS include fully-threaded length, headless, cannulated, and variable thread pitch. Twenty-three patients with AO type-B2 ankle fractures treated with lateral fixation by an APCS were retrospectively reviewed. Evaluation of postoperative roentgenograms for adequacy of reduction revealed a good reduction in 22 of 23 (95.7%) patients. The average wound incision was 4.1 cm. The operative time was 25.3 minutes. All the ankle fractures showed radiographic evidence of healing within four months. At the final follow-up, the ankle scores of the patients were evaluated for functional outcomes. Good to excellent results were obtained in 21 (91.3%) patients. No patient complained of symptomatic hardware. In conclusion, lateral fixation of AO type-B2 ankle fractures by APCS offers several advantages including stable fixation, a small surgical wound, less dissection of soft tissue, no palpable hardware, and easy application with a short operating time.
Introduction
It is well accepted that a displaced lateral malleolus fracture is best treated with surgical intervention to correct any significant subluxation or dislocation of the tibiotalar joint [3, 12]. The lateral malleolus plays the key role in the stability of the ankles because 1-mm lateral displacement of the talus decreases the tibiotalar contact surface by 42% [9, 15]. For an AO type-B2 ankle fracture (transsyndesmotic fibular fracture with medial lesion), open reduction and internal fixation has been recommended, because the talus is unstable [1, 18]. Although a lateral plate is commonly used to treat a lateral malleolar fracture, more soft tissue dissection may result in wound complication [7]. Internal fixation with minimum dissection that can achieve stable fixation is preferable [11]. The Acutrak plus compression screw (APCS) (Acumed Inc., Beaverton, OR, USA) is designed for use in the upper and lower extremities where larger diameter and longer length screws are needed. In addition, the APCS is an intramedullary implant that can achieve stable fixation with minimum soft tissue dissection, and is the author’s preferred means to stabilise most lateral malleolar fractures. To our knowledge, there is no report documenting the application of APCS in a lateral ankle fracture. It is the purpose of our study to retrospectively review the results in using such an implant and to discuss the surgical technique.
Patients and methods
Between 2008 and 2009, 73 patients with lateral malleolar fractures were surgically treated at two institutions. Inclusion criteria for this study were: (1) AO type-B2 ankle fractures, (2) acute and single-sided fracture, (3) internal fixation with an APCS, and (4) patients with the ability to walk without any assistance before injury. Exclusion criteria for this study were: (1) nonunion or pathological fractures, (2) severe open fractures (Gustilo grade III), (3) severe comminuted fractures (bony contact less than 25%), and (4) patients with syndesmosis instability. There were 26 patients who met the inclusion criteria. However, three patients could not be followed up due to relocation, and they were excluded. Therefore, 23 patients were followed-up for more than ten months and were included in this study. Ten of 23 patients had medial malleolar fractures and 13 had medial tenderness associated with medial clear space ≧4 mm, consistent with a ruptured deltoid ligament. There were four open lateral malleolar fractures including two Gustilo type I and two type II. An open fracture was treated by irrigation, thorough debridement, and appropriate intravenous antibiotics. The injury mechanisms and demographics are shown in Table 1.
Table 1.
Preoperative data
| Descriptive data | Value |
|---|---|
| Injury mechanism | |
| Vehicular trauma | n = 20 |
| High-energy falls | n = 3 |
| Gustilo open type | |
| I | n = 2 |
| II | n = 2 |
| Fracture pattern | |
| Deltoid ligament ruptures | n = 13 |
| Medial malleolar fractures | n = 10 |
| Transverse fractures | n = 2 |
| Oblique & spiral fractures | n = 17 |
| Comminuted fractures | n = 4 |
| Demographics | |
| Gender (female/male) | 10/13 |
| Mean age (years) | 37.4 |
Surgical technique
Operations on the ankle fractures were always performed under spinal anaesthesia. When a medial malleolar fracture was present, a separate incision was made for open reduction and internal fixation. This fixation was either by Kirschner wires augmented by a screw or by two screws. If the medial malleolus was intact and the deltoid ligament was ruptured, the deltoid ligament was not repaired. In our study, the major tools of the APCS system include guide pin, reamer, and compression screw. The characteristics of the APCS include fully-threaded length, headless, cannulated, and variable thread pitch. The screw tip is 5 mm and the tail is 6.5 mm in diameter. The minimum length is 35 mm and the maximum is 80 mm (Fig. 1). For the fractured lateral malleolus, a skin incision was made 1 cm below the distal fibular tip to the fracture site. Soft tissue was dissected and the fracture ends were exposed. A small bone holder or towel clip was used temporarily to hold the attained anatomical reduction. After identifying that there was no syndesmosis instability by using the stress test or intraoperative roentgenograms, the guide pin was inserted. The ideal entry point was 2 mm medial to the fibular tip with the direction of the pin parallel to the medullary canal (Fig. 2). Slight deviation of the ideal entry point was acceptable in most cases (Fig. 3). Fluoroscopy was used to verify the pin site and depth. After reaming, an APCS was placed with an adequate length. The common lengths of fixation screws used were 55–70 mm. Fluoroscopy was used to verify post-reduction joint space. For a comminuted fracture, cerclage wires or sutures could be used in addition to the screw. This procedure could keep the distal fibular alignment before the screw was inserted. Pre- and postoperative single doses of prophylactic antibiotic were given.
Fig. 1.
The tools of the Acutrak plus compression screw (APCS) system include guide pin, reamer, and compression screw. a Guide pin (left) and reamer (right). b Compression screw. The screw tip is 5 mm and the tail is 6.5 mm in diameter. The minimum length is 35 mm and the maximum is 80 mm. The characteristics of the APCS include fully-threaded length, headless, cannulated, and variable thread pitch
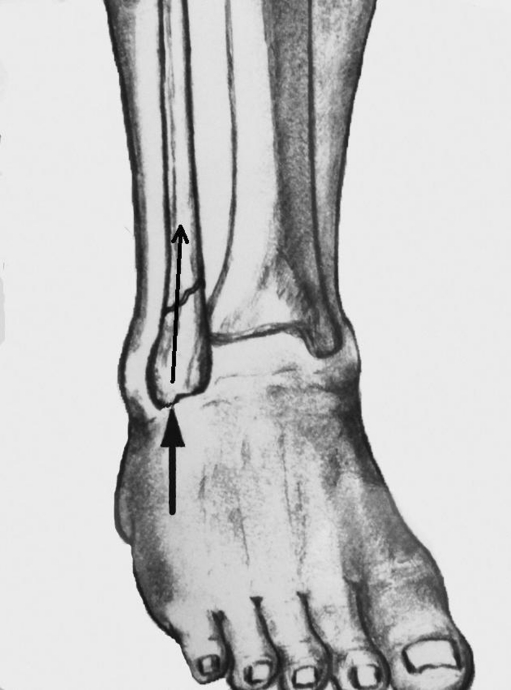
Fig. 2.
The ideal entry point is 2 mm medial to the fibular tip with the direction of the guide pin parallel to the medullary canal
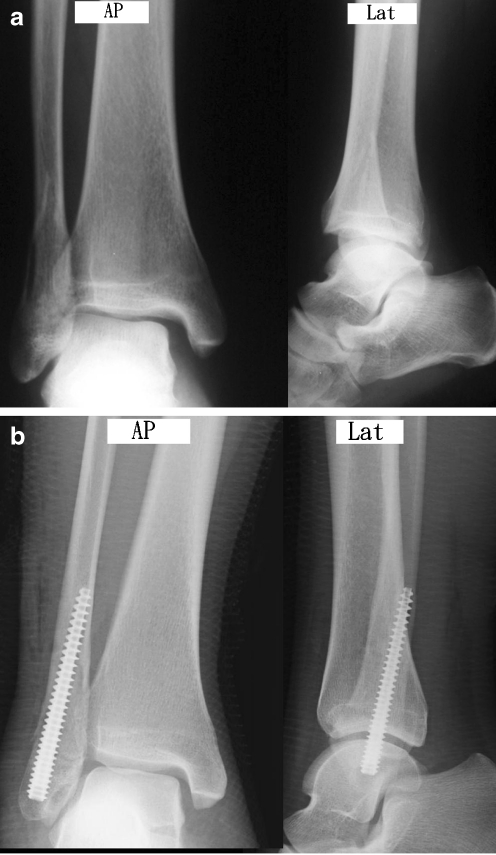
Fig. 3.
A 36-year-old female patient who had right lateral malleolar fracture associated with the wide medial clear space treated with an Acutrak plus compression screw (APCS). a Preoperative anteroposterior and lateral radiographs. b X-rays taken immediately postoperatively showed slight deviation of the ideal entry point. However, a good reduction was obtained
Plain films were taken immediately postoperatively to evaluate reduction, which was graded using a scale modified from that which was published previously [14]. Good reduction was defined as no fibula shortening, a posterior displacement less than 2 mm and a 1 mm increase in medial clear space. A fair reduction represented a fibula shortening ≦2 mm, posterior displacement of 2–4 mm and a 1–3 mm increase in the medial clear space. A poor reduction was defined as a fibula shortening in excess of 2 mm, posterior displacement of over 4 mm and a greater than 3 mm increase in medial clear space.
A short leg splint with the ankle in a neutral position was applied postoperatively for two to four weeks for soft tissue healing. The postoperative rehabilitation process consisted initially of partial weight bearing. Full weight bearing was permitted one month after the splint removal or when union was evident radiographically. Patients were reviewed at one, two, three, four and six months after fracture. AP and lateral roentgenograms were taken for all patients at each follow-up appointment for evaluation of fracture healing and implant position. Radiographic healing was interpreted by the attending surgeon at each follow-up and was verified by all authors of this study during a retrospective review. Radiographic healing was defined as evidence of bridging callus across the fracture sites or the obliteration of the fracture lines on both anteroposterior and lateral views.
At the last follow-up, we evaluated the clinical results according to the ankle scoring system of Baird and Jackson [1], which was modified from Weber and Simpson [19]. In this system, the subjective and objective clinical data are combined with radiographic results, with the maximum score being 100 points. The maximum clinical score is 75 points. Pain, stability of the ankle, ability to run, ability to walk, and motion of the ankle are evaluated. Maximum radiographic results contribute 25 points. An overall score of 96–100 points rank as excellent, 91–95 points as good, 81–90 points as fair, and 0–80 as poor results.
Results
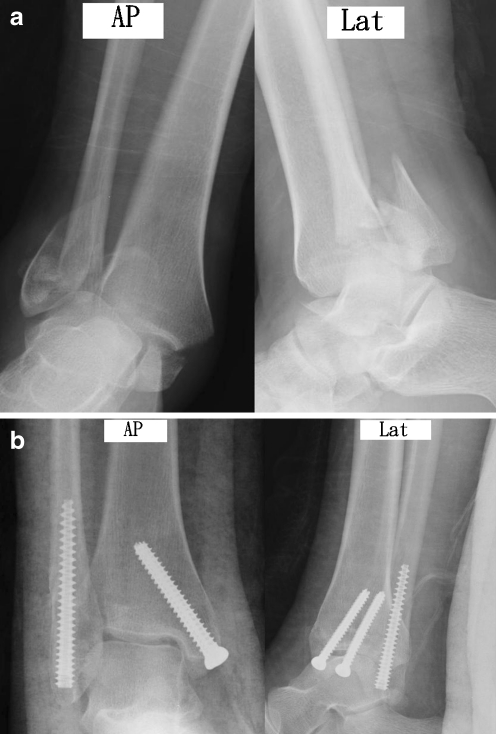
All the ankle fractures showed radiographic evidence of healing within four months. Evaluation of immediate postoperative roentgenograms for adequacy of reduction revealed a good reduction in 22 of 23 (95.7%) patients (Fig. 4) and a fair reduction in one of 23 (4.3%) patients. There was no poor reduction in our study. The average incision length was 4.1 cm (range 3.5–5.5 cm). The operative time was 25.3 minutes (range 17–55 minutes). The average period of follow-up was 12.4 months (range 10–15 months).
Fig. 4.
A 34-year-old female patient with right bilateral malleolar fracture was treated with an Acutrak plus compression screw (APCS) (lateral malleolus) and two cannulated screws (medial malleolus). a Preoperative anteroposterior and lateral radiographs showed an AO type-B2 ankle fracture with subluxation of the tibiotalar joint. b X-rays taken immediately postoperatively showed good reduction of the fracture and the ankle joint
There were no complications associated with peroneal tendon injuries and accidental articular cartilage damage. The only one complication (4.3%) was superficial infection. This female patient had an open type-II fracture. She was diagnosed clinically at the first follow-up visit about seven days after surgery. After seven days of treatment with oral antibiotics, the wound healed uneventfully.
At the final follow-up, the ankle scores of the patients were evaluated for functional outcomes. Good to excellent results were obtained in 21 (91.3%) patients. Two patients (8.7%) had fair results. The mean score for the affected ankle was 93.6 points (range 88–100 points) and the mean score for the contralateral ankle was 94.1 points (range 92–100 points). The mean scores for the involved ankle and the contralateral ankle were not different (p = 0.62). No patient complained of symptomatic hardware. No patient asked to have the hardware removed.
Discussion
Although there are many surgical techniques for fixation of displaced lateral malleolar fractures, studies of intramedullary nailing are relatively few [8, 10, 14, 16, 17]. One criticism of the use of an intramedullary device is that these techniques may not resist proximal migration or rotation of distal fragment [3]. McLennan et al. [14] reported on the Inyo nail, which is an intramedullary device for the treatment of fractures of the distal fibula. However, there are limitations for the use in pronation lateral rotation injuries. Rush nails and cruciate screws have been used, but may allow rotation of the distal fragment [12]. Uniquely, the APCS has variable thread pitch. The wider thread pitch at the tip of the screw penetrates the bone faster than the finer trailing threads, compressing the two fragments gradually as the screw is advanced. In our study, we think that the compressive force by an APCS can make the contact of an oblique surface of cancellous bone stable enough to resist proximal migration or rotation of the fracture site. It could explain why a good radiographic reduction was obtained in 95.7% of patients and union in 100%. In addition, we have not experienced any secondary displacement. Lee et al. [8] used an intramedullary Knowles pin to treat 25 AO type-B2 ankle fractures. They presented a good reduction rate of 96% and union rate of 100%. Although the symptomatic hardware problems were not common in their cases, 22 of 25 (88%) patients asked to have the hardware removed. In our study, no patient complained of symptomatic hardware. No one asked to have the hardware removed.
Extramedullary fixation of lateral malleolus fractures was commonly used in previous studies [2, 5–7, 13]. One or two lag screws were recommended by Kim et al. [5]. However, this technique is only used in oblique or long spiral fractures. Damage to the peroneal tendons by an overly long screw is possible [4]. Although tubular plating was the popular technique in previous reports, more soft tissue dissection and palpable hardware were the common disadvantages [7]. Lateral plating may result in complications of skin and soft tissue due to the double contour of the lateral malleolus and the small amount of overlying subcutaneous tissue [12]. In our study, we determined that an APCS needs a small skin incision and less soft tissue stripping. This could explain why our cases had a low complication rate related to soft tissue problems. In a study by Brown et al. [2], 31% of the 126 patients had pain overlying their fracture hardware with plates and screws, and nearly 50% of patients continued to have pain even after hardware removal. In our study, there is no hardware subcutaneously in the distal fibula because the APCS is headless. We did not experience complaints of discomfort associated with hardware. A headless means of fixation is a valuable tool in patient care as it eliminates traditional hardware prominence complications. On the outer surfaces of the ankle, where limited soft-tissue coverage is available, headed screws can create considerable discomfort and lead to complications and/or hardware removal.
In the study of Lee et al. [10], the average operation time was 43 minutes in 30 patients who had AO type-B2 ankle fractures, treated with lateral plating. In our study, there were 23 patients whose average operation time was 25.3 minutes. We think that the APCS technique is a simple and easy procedure. There is a short operation time in the cases treated by this method.
In conclusion, lateral fixation of AO type-B2 ankle fractures by APCS is a safe and effective technique. It offers several advantages including stable fixation, a small surgical wound, less dissection of soft tissue, a headless device without palpable hardware, and easy application with a short operating time.
References
- 1.Baird RA, Jackson ST. Fractures of the distal part of the fibula with associated disruption of the deltoid ligament. J Bone Joint Surg Am. 1987;69:1346–1352. [PubMed] [Google Scholar]
- 2.Brown OL, Dirschl DR, Obremskey WT. Incidence of hardware-related pain and its effect on functional outcomes after open reduction and internal fixation of ankle fractures. J Orthop Trauma. 2001;15(4):271–274. doi: 10.1097/00005131-200105000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Carr JB, Trafton PG (1998) Malleolar fractures and soft tissue injuries of the ankle. In: Browner BD, Jupiter JB, Levine AM, Trafton PG (eds) Skeletal trauma: fractures, dislocation, ligamentous injuries. W B Saunders, Philadelphia, pp 2327–2401
- 4.Hammacher ER, Schutte PR, Bast TJ. Minimal osteosynthesis of lateral malleolar fractures. Neth J Surg. 1986;38(3):87–89. [PubMed] [Google Scholar]
- 5.Kim SK, Oh JK. One or two lag screws for fixation of Danis-Weber type B fractures of the ankle. J Trauma. 1999;46:1039–1044. doi: 10.1097/00005373-199906000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Kukk A, Nurmi JT. A retrospective follow-up of ankle fracture patients treated with a biodegradable plate and screws. Foot Ankle Surg. 2009;15(4):192–197. doi: 10.1016/j.fas.2009.02.008. [DOI] [PubMed] [Google Scholar]
- 7.Lamontagne J, Blachut PA, Broekhuyse HM, et al. Surgical treatment of a displaced lateral malleolus fracture. J Orthop Trauma. 2002;16:498–502. doi: 10.1097/00005131-200208000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Lee YS, Chen SW. Lateral fixation of open AO type-B2 ankle fractures: the Knowles pin versus plate. Int Orthop. 2009;33:1135–1139. doi: 10.1007/s00264-008-0617-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee YS, Chen SW, Chen SH, et al. Stabilization of the fractured fibula plays an important role in the treatment of Pilon fractures: a retrospective comparison of fibular fixation methods. Int Orthop. 2009;33:695–699. doi: 10.1007/s00264-008-0654-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee YS, Huang HL, Lo TY. Lateral fixation of AO type-B2 ankle fractures in the elderly: the Knowles pin versus the plate. Int Orthop. 2007;31:817–821. doi: 10.1007/s00264-006-0260-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marsh JL, Saltzman CL (2006) Ankle fractures. In: Rockwood CA Jr, Green DP, Bucholz RW (eds) Rockwood and Green’s fractures in adult. Lippincott Williams, Philadelphia, pp 2147–2247
- 12.McDade WC (1975) Treatment of ankle fractures. In: AAOS instructional course lectures, ch 14. Mosby, St. Louis, pp 251–294
- 13.McKenna PB, O’Shea K, Burke T. Less is more: lag screw only fixation of lateral malleolar fractures. Int Orthop. 2007;31:497–502. doi: 10.1007/s00264-006-0216-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mclennan JG, Ungersma JA. A new approach to the treatment of ankle fractures. Clin Orthop. 1986;213:125–136. [PubMed] [Google Scholar]
- 15.Phillips WA, Schwartz HS, Keller CS, et al. A prospective randomized study of the management of severe ankle fractures. J Bone Joint Surg Am. 1985;67:67–78. [PubMed] [Google Scholar]
- 16.Ramasamy PR, Sherry P. The role of a fibular nail in the management of Weber type B ankle fractures in elderly patients with osteoporotic bone. Injury. 2001;32:477–485. doi: 10.1016/S0020-1383(01)00030-4. [DOI] [PubMed] [Google Scholar]
- 17.Ray TD, Nimityongskul P, Aderson LD. Percutaneous intramedullary fixation of lateral malleolus: technique and report of early result. J Trauma. 1994;36(5):669–675. doi: 10.1097/00005373-199405000-00012. [DOI] [PubMed] [Google Scholar]
- 18.Tejwani NC, McLaurin TM, Walsh M, et al. Are outcomes of bimalleolar fractures poorer than those of lateral malleolar fractures with medial ligamentous injury? J Bone Joint Surg Am. 2007;89:1438–1441. doi: 10.2106/JBJS.F.01006. [DOI] [PubMed] [Google Scholar]
- 19.Weber BG, Simpson LA. Corrective lengthening osteotomy of the fibula. Clin Orthop. 1985;199:61–67. [PubMed] [Google Scholar]