Abstract
First metatarsophalangeal joint replacement is an alternative surgical procedure to arthrodesis in the treatment of moderate-to-severe hallux rigidus. However, few studies have been published about functional outcome after joint reconstructive procedures for hallux rigidus. The purpose of this study was to assess clinical, radiological and functional outcome, with special regard to recreational and sports activity, after first metatarsophalangeal joint replacement in patients affected by hallux rigidus grade III. Twenty-three patients who had undergone total joint replacement of the first metatarsophalangeal joint were examined preoperatively and three, six, 12 and 18 months postoperatively. All patients (mean age of 57.0 ± 3.7 years) received a non-cemented TOEFIT-PLUS™ implant by one surgeon. Clinical scores (AOFAS score and VAS), radiological examination, patient satisfaction and sport participation were used to evaluate treatment outcome and radiolucent lines. The mean AOFAS score showed a significant improvement from 44.6 ± 7.2 points preoperatively to an average of 82.5 ± 14.4 points at last follow-up (p < 0.001). The mean total ROM of the first MTP joint increased from 28.1 ± 4.9 degrees preoperatively to 52.7 ± 15.7 degrees postoperatively (p < 0.001). After surgery, 91.3% of the patients were able to resume at least one recreational activity. Total arthroplasty for the treatment of hallux rigidus in an active patient population revealed good clinical and functional results. However, postoperative recreational sport activity showed a decrease in comparison to the pre-arthritic state. Further follow-up is necessary to quantify loosening risk in active patients after total hallux arthroplasty.
Introduction
Total first metatarsophalangeal (first MTP) arthroplasty is a surgical procedure for treatment of moderate-to-severe hallux rigidus in patients for whom arthrodesis of the first MTP joint may not provide adequate satisfaction due to the inherent stiffness of the hallux [10, 11]. The clinical outcomes after first MTP arthroplasty are satisfactory, even though controversial results have been reported concerning revision rates of hemi- and total arthroplasty [10, 12, 13, 23, 24, 27, 30, 32].
Currently, arthrodesis is the most accepted surgical procedure for advanced-stage hallux rigidus that has been demonstrated to provide effective pain relief and restore function [6]. Even though function and pain levels improve, patients may be concerned about potential limitations in sports participation and physical activity.
Several studies reported sports participation after various joint arthroplasties [3, 19, 20, 25, 26, 33]. The good clinical long-term results and the high level of satisfaction enable the subjects to resume sports and recreational activities after total joint replacement.
To the best of our knowledge, no information is available in literature concerning patients sports activity after total first MTP arthroplasty. The purpose of this prospective study was to determine the amount and type of sports activities that are possible after first MTP arthroplasty, as well as to correlate sports participation and clinical and radiological outcome after the procedure.
Methods
Between January 2006 and January 2007, 23 consecutive first MTP arthroplasties were performed by one senior surgeon using the TOEFIT-PLUS™ (Plus Orthopedics, Switzerland) joint replacement system in 23 patients (16 females and seven males, mean age of 57.0 ± 3.7 years). The inclusion criteria was hallux rigidus grade III with fulfilment of general first MTP arthroplasty indications (good bone stock, normal neuronal and vascular status, immunocompetent status) [5]. Absolute contraindications included acute or chronic infections, fungal foot disease, previous surgical procedure to the forefoot, severe deformity of the foot and diabetes.
The range of motion (ROM) of the first metatarsophalangeal joint was measured with a goniometer.
All patients gave an informed consent to participate in the study. The study was carried out in accordance with the World Medical Association Declaration of Helsinki.
Surgical procedure
All surgical procedures were performed by a single surgeon using a standardised technique, with the patients supine and under general anaesthesia. A mid-thigh pneumatic tourniquet was used. The first MTP joint was approached through a dorsomedial skin incision. A longitudinal capsulotomy was performed in line with the skin incision. All osteophytes were removed from the distal metatarsal and proximal phalanx, followed by sesamoid mobilisation from the plantar aspect of the joint. The base of the proximal phalanx was excised 3–5 mm from the articular surface using an oscillating saw as recommended in the manufacturer’s instructions, while being careful not to damage soft tissue or sesamoids. The medullary cancellous bone was then removed to the endosteum with a reamer.
For the proximal component, the osteotomy was made 8–10 mm from the articular surface in a dorsoplantar direction, perpendicular to the plantar plane. The centre of the medullary canal was opened using a 3.2-mm drill. A reamer was used to remove the cancellous bone of the metatarsal.
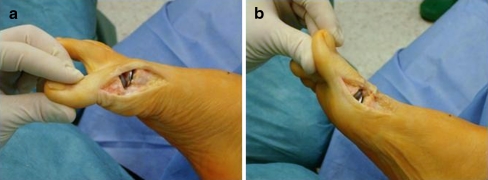
The appropriate trials were inserted and a trial reduction was performed to check toe length, soft tissue tension, and mobility. With axial traction applied to the big toe, the joint space should be at least 5 mm. Finally, the chosen implants and polyethylene phalangeal insert was placed in the prepared canals using appropriate impactors (Fig. 1).
Fig. 1.
Intraoperative view of the implant. Plantarflexion (a) and dorsiflexion (b) of the first metatarsopahalangeal joint after prosthesis implantation
Antibiotic prophylaxis (a second-generation cephalosporine) was given intraoperatively as a single-shot dose. Enoxaparin sodium was administered subcutaneously 40 mg once daily, for two weeks. Early postoperative mobilisation started on the first postoperative day, and full weight-bearing was allowed with a postoperative shoe for six weeks. Full weight-bearing without limitations was permitted at six weeks when patients were clinically asymptomatic and when they presented no radiological signs of loosening or implant malalignment.
Outcome measures
After surgery, all patients underwent clinical and radiographic follow-up at six weeks, three, six, 12 and 18 months (Figs. 2 and 3). Preoperative and follow-up measurements were performed by the same investigator. To eliminate surgeon bias, the investigations were done by an independent researcher. Standard anteroposterior and lateral radiographs were performed to assess implant alignment, any evidence of loosening, and bone loss. A radiolucent line of more than 2 mm was considered as implant loosening [9].
Fig. 2.
Preoperative anteroposterior (a) and lateral (b) radiographs in a patient affected by hallux rigidus grade III
Fig. 3.
Anteroposterior (a) and lateral (b) radiographs 12 months after TOEFIT-PLUS™ system implantation
Pain was quantified with a visual analogue scale (VAS) from 0 to 10, with 0 representing no pain and 10 representing the worst pain imaginable. The clinical outcome was assessed using the American Orthopaedic Foot and Ankle Society (AOFAS) scoring system [21]. Patients subjectively evaluated the success of the operation with the follow categories: “very satisfied”, “satisfied” and “not satisfied”.
Type of sport and participation were documented for each patient preoperatively and at follow-up visits. The frequency of sports participation (sessions per week and duration per session) was recorded before the onset of restricting symptoms and at follow-up visits. To facilitate patients answers, ranges were provided for sessions per week (1, 2, 3, ≥ 4 sessions per week) and duration per session (15–30 min, 30–60 min, 60–120 min, >120 min per session) [33]. Patients were asked how long it took to resume partial or normal participation in each activity and if they had to modify their sports activity because of the surgery. Furthermore, pain experienced during sports participation was recorded.
For statistical analysis of the data, a one-way analysis of variance (ANOVA) for repeated measures was performed with SPSS software (version 13.0, SPSS Inc., Chicago, Ill.). A Wilcoxon-test was performed for ordinal data. To identify the significance of radiolucent zones for the clinical outcome, a correlation test was performed between radiolucencies and AOFAS score using the Spearman’s correlation coefficient (ρ). The significance level was set at p < 0.05.
Results
According to the AOFAS score, clinical results revealed an improvement from 44.6 ± 7.2 points preoperatively to an average of 82.5 ± 14.4 points at last follow-up (p < 0.001, Table 1). The VAS decreased significantly from 7.0 ± 0.8 preoperatively to 2.0 ± 1.7 at last follow-up (p < 0.001).
Table 1.
Clinical results at the follow-up visits. Means and standard deviations are reported
| Variable | Preoperative | Three months | Six months | 12 months | 18 months | p-value* |
|---|---|---|---|---|---|---|
| AOFAS | 44.6 (7.2) | 69.9 (10.6) | 79.2 (14.3) | 81.5 (12.4) | 82.5 (14.4) | p < 0.001 |
| VAS | 7.0 (0.8) | 5.2 (1.0) | 2.5 (1.9) | 2.0 (1.6) | 2.0 (1.7) | p < 0.001 |
| ROM-dorsiflexion (degrees) | 9.6 (2.3) | 17.2 (7.3) | 25.1 (9.8) | 29.1 (7.3) | 29.0 (10.8) | p < 0.001 |
| ROM-total (degrees) | 28.1 (4.9) | 33.8 (6.4) | 44.5 (10.7) | 50.5 (13.0) | 52.7 (15.7) | p < 0.001 |
AOFAS American Orthopaedic Foot and Ankle Society, VAS visual analogue scale, ROM range of motion
* Based on analysis of variance (ANOVA) results
There was a significant increase of dorsiflexion and total ROM of first MTP joint compared to the preoperative values. The mean preoperative dorsiflexion of the first MTP joint increased from 9.6 ± 2.3 degrees to 29 ± 10.8 degrees postoperatively (p < 0.001). The mean total ROM of the first MTP joint increased from 28.1 ± 4.9 degrees preoperatively to 52.7 ± 15.7 degrees postoperatively (p < 0.001).
Component loosening was not observed in any patient. However, three patients (13.0%) presented phalangeal radiolucent lines (<2 mm) at the last radiographic follow-up (Fig. 4), which did not correlate with our clinical results (p = 0.33).
Fig. 4.
Radiograph showing periprosthetic radiolucent zones (arrow) six months postoperatively
At 18 months of follow-up, 12 patients (52.2%) were very satisfied with the procedure, seven (30.4%) were satisfied and four patients (17.4%) were not satisfied. In the not-satisfied group, two patients presented with persistent joint pain during walking, with an inability to participate in sport and recreational activities. One patient showed varus malalignment with metatarsalgia under the central metatarsals. Conservative treatment with an orthotic insole partially relieved the pain and no revision surgery was necessary. One patient presented superficial wound infection that was effectively treated with oral antibiotic.
Recreation sport activity participation
Each patient was active before surgery in 2.0 ± 0.5 (range, 1–3) sports and recreational activities and in 1.2 ± 0.6 (range, 0–2) after surgery at the last follow-up (p = 0.001). Concerning sports activity, the most frequently reported preoperative activities were: walking (18.8%), skiing (14.6%), hiking (14.6%), jogging (12.5%), tennis (10.5%), soccer (8.3%) and swimming (8.3%).
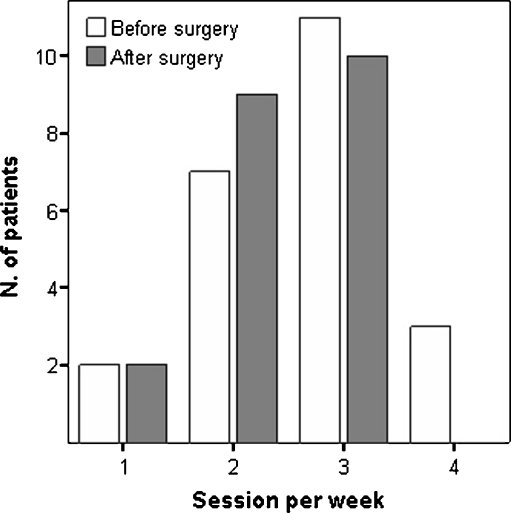
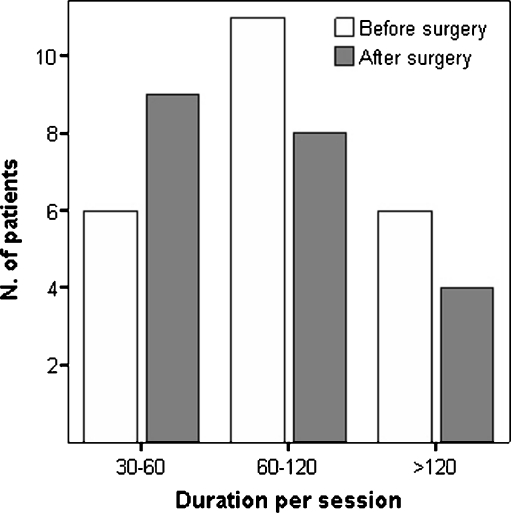
After surgery, 21 patients (91.3%) were able to resume at least one recreational activity. Within three months of surgery, 34.7% of the patients returned to sport, and 82.6% returned to sport within 12 months. The mean number of sport sessions per week was 2.7 ± 0.8 preoperatively and at the last follow-up was 2.1 ± 0.9 (p = 0.07, Fig. 5). The mean session duration revealed a significant decrease from preoperative to postoperative (p = 0.04). After surgery, 39.1% of the patients participated in sport activities for up to 60 minutes each session, 34.8% for up to 120 minutes and only 17.3% for more than 120 minutes (Fig. 6).
Fig. 5.
Frequency participation in sporting activities before and after surgery
Fig. 6.
Sports session duration (in minutes) before and after surgery. A significant decrease was detected for patients who participated for more than 60 minutes per session
High impact activities showed a postoperative decrease in patient participation. No patients were able to resume soccer, and only two patients resumed jogging. The other frequently reported activities at the last follow-up were: walking (32.1%), hiking (14.3%), cycling, dancing and swimming (10.7%). The following reasons for the change in sport activities were mentioned: pain, anxiety, and protection.
After first MTP joint replacement, twelve patients (57.1% of patients still active in sport) felt excellent or good during sports activities, seven patients (33.3%) reported experiencing a limited range of motion and two patients (9.5%) felt anxious and unconfident. At the time of last follow-up, 13 patients (61.9%) were pain free with a pain score of 0, with no limitations during sports participation; six (28.5%) reported slight pain with a pain score ranging from 1 to 3, requiring occasional pain medication; and two (9.5%) patients required pain killers for sports participation with a pain score ranging from 4 to 6.
Discussion
The goal of hallux rigidus surgery is relief of pain and restoration of function by preserving joint mobility. Total first MTP joint replacement arthroplasties have been developed in recent years to overcome the disadvantages presented by arthrodesis, which is still considered the treatment of choice for advanced-stage hallux rigidus [6, 7, 14, 28]. However, loss of first MTP joint motion may not be acceptable for active patients who aim to resume recreational and sports activities. Furthermore, a functional great toe is important considering its role during gait. In healthy subjects, the forces during the push-off phase under the first metatarsal head and hallux, taken together, account for about 53% of the body weight [16].
In this investigation, the clinical outcome after 18 months of follow-up was satisfactory in 82.6% of the patients. The majority of clinical improvement in AOFAS score, pain and total ROM occurred within six months after the procedure, but a slight general improvement was detected up to 18 months after surgery. These results are similar to previous studies that reported a satisfaction rate greater than 75%. In a recent study, Seeber and Knessl recorded the results in 52 patients followed-up for an average of three years after TOEFIT-PLUS™ implantation [32]. Revision surgery was necessary for 11 patients due to infection, dislocation, chronic pain, aseptic loosening, persistent stiffness and traumatic loosening. Pulavarti et al. [30] prospectively followed 48 patients, treated by Bio-Action great toe implant (Osteomed, Addison, TX), for an average of 47 months. Seventy-seven percent of patients rated their satisfaction as either excellent or good. Two patients underwent revision surgery: one was treated with arthrodesis and one with resection arthroplasty [30]. Olms and Dietze performed a review of 21 patients after Bio-Action great toe implantation with a minimum follow-up of 24 months. It was found that 85% of the patients were satisfied with the procedure and no implant required salvage [27].
Despite these results, concerns about loosening and implant survivorship still persist.
In our series, mild phalangeal radiolucent lines (<2 mm) were detected in 13% of the patients; however, the clinical outcome did not correlate with the radiological findings. In literature, the rate of radiolucent lines around the implants after total first MTP joint replacement varies between 3.1% and 33% [9, 12, 13, 24, 30, 32]. It can be argued that, in our series, a longer follow-up is required in order to fully assess the clinical and radiological outcomes.
Although several studies have reported the effectiveness of first MTP joint replacement for the treatment of hallux rigidus [10, 22, 23, 27, 30, 32], there is little data available in the literature regarding evaluation and recommendations for sports participation after hallux rigidus surgery. It can be argued that, in our series, a longer follow-up is required in order to fully assess the clinical and radiological outcomes. Compared with the pre-arthritic state, no significant differences were observed concerning sport engagement and number of sessions per week. About 86.9% of the patients were able to resume sports activities after the procedure. However, the number of sports and activities that the patients were engaged in were significantly decreased, mainly due to the fact that patients tended to perform less demanding sports and recreational activities, such as walking, hiking, cycling, dancing and swimming.
It is well known that sports activities can help to maintain and improve a good mental and general health and sense of well-being [1, 29]. Furthermore, limited first MTP joint mobility can lead to calf atrophy, impairing the calf muscle pump function, which should be considered a risk factor for chronic venous insufficiency of the lower limbs [2, 28]. On the other hand, the possible influence of sport on the rate of implant loosening and failure after first MTP arthroplasty should be evaluated in long-term follow-up studies. Previous research has been controversial concerning the effect of sports activities on the survival rate in more or less active patients after joint arthroplasty [8, 15, 20, 31]. Dubs et al. reported higher failure rate in inactive patients in comparison to active patients after total hip arthroplasty (THA) [8]. At five years of follow-up Gschwend et al. found that winter sports (alpine and cross country skiing) did not increase the risk of loosening after THA compared to the inactive group of patients [15]. Kilgus et al. observed higher loosening rates after THA in patients who regularly participated in sports activities compared to more inactive patients [20]. However, these results cannot simply be transferred to patients with first MTP joint arthroplasty. At the present time, in accordance with the recommendations of the Hip and Knee Society for sport activities after hip and knee arthroplasty, we recommend low-impact sports activities after first MTP joint replacement such as walking, hiking, swimming, dancing, golf, and cycling [17]. Furthermore, every patient should be educated regarding the possible risk of loosening and early failure associated with higher physical and sports ability [18, 31].
In a non-comparative study, Brodsky et al. reported a 94% satisfaction rate with effective pain relief after arthodesis of the first metatarsophalangeal joint. Most of the patients were able to return to jogging, golf, hiking and tennis. However, most of the patients had shoe-wearing limitation after the procedure [4].
We acknowledge that this study has some limitations. The short-term follow-up did not allow conclusions regarding the effect of sports on the rate of loosening, revision and progression of periprosthetic radiolucencies. We can only suggest that the arthroplasty of the first MTP is an interesting treatment option in selected cases of active and younger patients. Further research is warranted to compare the clinical and functional outcome of first MTP replacement with other accepted surgical procedures, such as cheilectomy and arthrodesis, in active patients with long-term follow-up.
Total arthroplasty of the first metatarsophalangeal joint provides pain relief and acceptable clinical outcomes in patients affected by hallux rigidus grade III. Although patients participation in recreational sport activity did not significantly decrease after surgery, activity modification was detected, mainly due to the shift away from high-impact activities. Further follow-up is required to assess the influence of repetitive activities on loosening and revision rates in total first metatarsophalangeal joint replacement.
References
- 1.American College of Sports Medicine Physicians Statement The recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness in healthy adults. Med Sci Sports Exerc. 1990;22(2):265–274. [PubMed] [Google Scholar]
- 2.Anderson RJ. Hallux rigidus and atrophy of calf muscles. N Engl J Med. 1999;340(14):1123. doi: 10.1056/NEJM199904083401419. [DOI] [PubMed] [Google Scholar]
- 3.Bradbury N, Borton D, Spoo G, Cross MJ. Participation in sports after total knee replacement. Am J Sports Med. 1998;26(4):530–535. doi: 10.1177/03635465980260041001. [DOI] [PubMed] [Google Scholar]
- 4.Brodsky JM, Passmore RN, Fe P, Shabat S. Functional outcome of arthrodesis of the first metatarsophalangeal joint using parallel screw fixation. Foot Ankle Int. 2005;26(2):140–146. doi: 10.1177/107110070502600205. [DOI] [PubMed] [Google Scholar]
- 5.Coughlin MJ. Arthritides. In: Coughlin MJ, Mann RA, editors. Surgery of the foot and ankle. St. Louis: Mosby; 1999. pp. 605–650. [Google Scholar]
- 6.Coughlin MJ, Shurnas PS. Hallux rigidus. Grading and long-term results of operative treatment. J Bone Joint Surg Am. 2003;85(11):2072–2088. [PubMed] [Google Scholar]
- 7.DeFrino PF, Brodsky JW, Pollo FE, Crenshaw SJ, Beischer AD. First metatarsophalangeal arthrodesis: a clinical, pedobarographic and gait analysis study. Foot Ankle Int. 2002;23(6):496–502. doi: 10.1177/107110070202300605. [DOI] [PubMed] [Google Scholar]
- 8.Dubs L, Gschwend N, Munzinger U. Sport after total hip arthroplasty. Arch Orthop Trauma Surg. 1983;101(3):161–169. doi: 10.1007/BF00436765. [DOI] [PubMed] [Google Scholar]
- 9.Ess P, Hämäläinen M, Leppilahti J. Non-constrained titanium-polyethylene total endoprosthesis in the treatment of hallux rigidus. A prospective clinical 2-year follow-up study. Scand J Surg. 2002;91(2):202–207. doi: 10.1177/145749690209100213. [DOI] [PubMed] [Google Scholar]
- 10.Fadel G, Abboud R, Rowley D. Implant arthroplasty of the hallux metatarsophalangeal joint. The Foot. 2002;12(1):1–9. doi: 10.1054/foot.2001.0717. [DOI] [Google Scholar]
- 11.Fitzgerald J. A review of long terms results of arthrodesis of the first metatarsophalangeal joint. J Bone Joint Surg Br. 1969;51(3):488–493. [PubMed] [Google Scholar]
- 12.Fuhrmann RA, Wagner A, Anders JO. First metatarsophalangeal joint replacement: the method of choice for end stage hallux rigidus? Foot Ankle Clin. 2003;8(4):711–721. doi: 10.1016/S1083-7515(03)00146-3. [DOI] [PubMed] [Google Scholar]
- 13.Gibson AJN, Thomson CE. Arthrodesis or total replacement arthroplasty for hallux rigidus: a randomized controlled trial. Foot Ankle Int. 2005;26(9):680–690. doi: 10.1177/107110070502600904. [DOI] [PubMed] [Google Scholar]
- 14.Goucher NR, Coughlin MJ. Hallux metatarsophalangeal joint arthrodesis using dome-shaped reamers and dorsal plate fixation: a prospective study. Foot Ankle Int. 2006;27(11):869–876. doi: 10.1177/107110070602701101. [DOI] [PubMed] [Google Scholar]
- 15.Gschwend N, Frei T, Morscher E, Nigg B, Loehr J. Alpine and cross country skiing after total hip replacement: 2 cohorts of 50 patients each, one active, the other inactive in skiing, followed for 5–10 years. Acta Orthop Scand. 2000;71(3):243–249. doi: 10.1080/000164700317411825. [DOI] [PubMed] [Google Scholar]
- 16.Hayafune N, Hayafune Y, Jacob H. Pressure and force distribution characteristics under the normal foot during the push-off phase in gait. The Foot. 1999;9(2):88–92. doi: 10.1054/foot.1999.0518. [DOI] [Google Scholar]
- 17.Healy WL, Sharma S, Schwartz B, Iorio R. Athletic activity after total joint arthroplasty. J Bone Joint Surg Am. 2008;90(10):2245–2252. doi: 10.2106/JBJS.H.00274. [DOI] [PubMed] [Google Scholar]
- 18.Heisel C, Silva M, Skipor AK, Jacobs JJ, Schmalzried TP. The relationship between activity and ions in patients with metal-on-metal bearing hip prostheses. J Bone Joint Surg Am. 2005;87(4):781–787. doi: 10.2106/JBJS.D.01820. [DOI] [PubMed] [Google Scholar]
- 19.Huch K, Müller KA, Stürmer T, Brenner H, Puhl W, Günther KP. Sports activities 5 years after total knee or hip arthroplasty: the Ulm Osteoarthritis Study. Ann Rheum Dis. 2005;64(12):1715–1720. doi: 10.1136/ard.2004.033266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kilgus DJ, Dorey FJ, Finerman GA, Amstutz HC. Patient activity, sports participation, and impact loading on the durability of cemented total hip replacements. Clin Orthop Rel Res. 1991;269:25–31. [PubMed] [Google Scholar]
- 21.Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15(7):349–353. doi: 10.1177/107110079401500701. [DOI] [PubMed] [Google Scholar]
- 22.Knessl J, Frank SE, Kundert HP, Zollinger-Kies H, Jacob HAC. Ground reaction forces under the great toe after implantation of the TOEFIT-PLUS™ prosthesis. Foot Ankle Surg. 2005;11(3):131–134. doi: 10.1016/j.fas.2005.03.001. [DOI] [Google Scholar]
- 23.Koenig RD, Horwitz LR. The Biomet Total Toe system utilizing the Koenig score: A five-year review. J Foot Ankle Surg. 1996;35(1):23–26. doi: 10.1016/S1067-2516(96)80008-1. [DOI] [PubMed] [Google Scholar]
- 24.Kundert HP, Zollinger-Kies H. Endoprothetik bei Hallux rigidus. Orthopaede. 2005;34(8):748–757. doi: 10.1007/s00132-005-0827-4. [DOI] [PubMed] [Google Scholar]
- 25.Naal FD, Fischer M, Preuss A, et al. Return to sports and recreational activity after unicompartmental knee arthroplasty. Am J Sports Med. 2007;35(10):1688–1695. doi: 10.1177/0363546507303562. [DOI] [PubMed] [Google Scholar]
- 26.Naal FD, Maffiuletti NA, Munzinger U, Hersche O. Sports after hip resurfacing arthroplasty. Am J Sports Med. 2007;35(5):705–711. doi: 10.1177/0363546506296606. [DOI] [PubMed] [Google Scholar]
- 27.Olms K, Dietze A. Replacement arthroplasty for hallux rigidus. 21 patients with a 2-year followup. Int Orthop. 1999;23(4):240–243. doi: 10.1007/s002640050360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Orsted HL, Radke L, Gorst R. The impact of musculoskeletal changes on the dynamics of the calf muscle pump. Ostomy Wound Manage. 2001;47(10):18–24. [PubMed] [Google Scholar]
- 29.Pescatello LS, Franklin BA, Fragard R, et al. American College of Sports Medicine position stand. Exercise and hypertension. Med Sci Sports Exerc. 2004;36(3):533–553. doi: 10.1249/01.MSS.0000115224.88514.3A. [DOI] [PubMed] [Google Scholar]
- 30.Pulavarti RS, McVie JL, Tullochn CJ. First metatarsophalangeal joint replacement using the Bio-Action great toe implant: intermediate results. Foot Ankle Int. 2005;26(12):1033–1037. doi: 10.1177/107110070502601206. [DOI] [PubMed] [Google Scholar]
- 31.Schmalzried TP, Shepherd EF, Dorey FJ et al (2000) The John Charnley Award. Wear is a function of use, not time. Clin Orthop Rel Res (381):36–46 [DOI] [PubMed]
- 32.Seeber E, Knessl J. Treatment of hallux rigidus with the TOEFIT-PLUS™ joint replacement system. Interact Surg. 2007;2(1):77–85. doi: 10.1007/s11610-007-0013-y. [DOI] [Google Scholar]
- 33.Valderrabano V, Pagenstert G, Horisberger M, Knupp M, Hintermann B. Sports and recreation activity of ankle arthritis patients before and after total ankle replacement. Am J Sports Med. 2006;34(6):993–999. doi: 10.1177/0363546505284189. [DOI] [PubMed] [Google Scholar]