Abstract
During throwing motion the athlete puts enormous stress on both the dynamic and the static stabilisers of the shoulder. Repetitive forces cause adaptive soft tissue and bone changes that initially improve performance but ultimately may lead to shoulder pathologies. Although a broad range of theories have been suggested for the pathophysiology of internal impingement, the reasons are obviously multifactorial. This review aims to critically analyse the current literature and to summarise clinically important information. The cardinal lesions of internal impingement, articular-sided rotator cuff tears and posterosuperior labral lesions, have been shown to occur in association with a number of other findings, most importantly glenohumeral internal rotation deficit and SICK scapula syndrome, but also with posterior humeral head lesions, posterior glenoid bony injury and, rarely, with Bankart and inferior glenohumeral ligament lesions. Extensive biomechanical and clinical research is necessary before a complete understanding and reconciliation of the varying theories of the pathomechanisms of injury can be developed.
Introduction
The shoulder is significantly stressed in overhead athletes, especially during distinct phases of throwing motion [1]. Patients typically present with complaints of posterior shoulder pain during abduction and maximum external rotation of the arm (late cocking and acceleration phases of throwing) [2]. Symptoms may be vague and the athlete may report only a gradual onset of loss of velocity or control during competition, often known as dead arm syndrome [3].
Baseball pitchers are most commonly afflicted, although athletes of other sports requiring repetitive shoulder abduction and external rotation such as tennis, volleyball, javelin throwing, and swimming are also at risk [2, 4–7]. It has been suggested that internal impingement is most likely caused by fatigue of the muscles of the shoulder girdle resulting from a lack of conditioning or from over-throwing [8]. As the shoulder girdle muscles become fatigued, the humerus drifts out of the scapular plane [9]. This has been termed hyperangulation or opening up, which can lead to tensile stressing of the anterior aspect of the shoulder capsule. Loss of the integrity of the anterior capsule may compromise the obligatory posterior rollback of the humeral head, leading to an anterior translation and therefore causing the undersurface of the rotator cuff to abut the margin of the glenoid and labrum. However, internal impingement has also been described in non-athletic individuals [1, 10].
In order to achieve a maximum recovery of the athlete an accurate understanding together with a sophisticated diagnostic and therapeutic algorithm is necessary. In this context the present work aims to critically review the current literature and discuss the aetiology, diagnosis and therapy of this entity.
Kinematics of throwing
A complete throw lasts less than two seconds. Fleisig et al. defined six phases of the throwing motion. During phase I (wind-up) the centre of gravity is raised and minimal stress is put on the shoulder [11]. In phase II (early cocking) the arm is abducted to 90° and prepared for maximum external rotation [12]. During phase III (late cocking) the shoulder is rotated externally to a maximum extent. Elite athletes reach up to 170°. This position leads to a posterior translation of the humeral head exerting maximum stress on the anterior capsule. The first three phases take approximately 1.5 seconds [13]. Phase IV is the acceleration phase. Although the duration of the fourth phase accounts for only 0.05 seconds, the highest angular velocities and the largest rotational movement happens during this phase, reaching a peak rotational velocity close to 7.000°/s [7]. Phase V is the deceleration phase and represents the most violent phase of the throwing motion. Deceleration occurs from the point of ball release to the point of 0° of rotation. It is a point of marked eccentric contraction of the rotator cuff to slow down the arm motion being a point of maximal posterior capsule stress. Joint loads approach posterior shear of 400 N, inferior shear of 300 N, and compressive forces of nearly 1,000 N [14]. Phase VI is the follow through. This is the rebalancing phase in which the muscles return to resting levels. The final two phases last approximately 0.35 seconds. The velocity of the ball depends on a variety of biomechanical factors but is most directly related to the amount of external rotation that the shoulder achieves. Elite pitchers can generate ball velocities exceeding 144.8 km/h. At ball release, the shoulder of a professional pitcher can be exposed to distractive forces of up to 950 N. In the deceleration phase, the compressive forces created by the rotator cuff and the deltoid muscle is in the range of 1090 N with posterior shear forces of up to 400 N. These forces approach the ultimate tensile strengths of the soft tissues that support the shoulder. In addition to the glenohumeral motion, scapular function has to be seen as a major contributor to transfer the kinetic energy from the lower limbs and trunk to the upper extremity. In this context Kibler et al. presented an excellent characterisation of the scapular dynamics [15]. Only half of the kinetic energy imparted to the ball results from the arm and shoulder action. The remaining half is generated by lower-limb and trunk rotation and is transferred to the upper limb through the scapulo-thoracic joint, making that articulation an important, but frequently overlooked, part of the kinetic chain [12].
Internal impingement
Unlike “external” or “subacromial” impingement, often simply called “impingement syndrome,” there is not a single pathophysiological process at work in the painful thrower’s shoulder. Internal impingement syndrome is thought to be of fundamentally more complex character and dependent on multiple factors [16–18]. In 1993 Walch et al. published a landmark article in which 30 athletes were assessed for shoulder pain [19]. Seventeen (16 of whom were throwing athletes) of the original 30 athletes underwent an arthroscopic shoulder examination; typical findings included the presence of posterior labral lesions and articular surface sided rotator cuff tears, in the absence of a Bankart or SLAP lesion. The authors differentiated the labral lesions from SLAP lesions which extended anteriorly to the biceps anchor at the supraglenoid tubercle, concluding that internal impingement may be responsible for a subset of patients with isolated posterior SLAP tears. In each case, the impingement of the posterior aspect of the humeral head was directly observed via arthroscopy on the posterosuperior rim of the glenoid. This area of impingement corresponded precisely with the location of the lesions of the rotator cuff and the labrum respectively when the arm was brought into the abducted, externally rotated throwing position.
Posterosuperior impingement (PSI)
Bennett et al. first described posterior shoulder pain in throwers in 1959. Lombardo et al. identified the late cocking phase of the thrower’s motion as a possible cause of posterior shoulder pain in this group of athletes [4]. This phenomenon, which is distinct from subacromial impingement syndrome, is known as posterosuperior impingement (PSI) [20]. A posterior capsular thickening and contracture have been reported as common findings [21]. The biomechanical aetiology for injury to these structures is controversial. Two possible causes for PSI have been reported, although neither of them is generally accepted. We favour the theory of rotational instability, which describes the ability of the throwing shoulder to over rotate into a position of hyper-external rotation during the late cocking and acceleration phase of the throwing motion. Thereby the anterior capsule is stressed during the late cocking phase whereas the posterior capsule is widened and traumatised during the deceleration phase. The consequence is that microinstability with corresponding posterior capsular hypertrophy develops leading to an increased external and a reduced internal rotation. In this context Burkhart et al. formed the term glenohumeral internal rotation deficit (GIRD) [22]. They described the first step in this cascade as the development of a contracture of the posterior band of the inferior glenohumeral ligament (PIGHL) and the posteroinferior capsule. Thereby the central contact point of the glenohumeral articulation is shifted in a postero-superior direction possibly leading to a greater arc of external rotation before the normal contact of internal impingement. These changes lead to an increase in the pathological peel-back mechanism with an increased vector of the biceps in the cocking position transmitting heightened shearing of the biceps anchor, leading to SLAP tears [23]. This notion is supported by several authors, who report an increased incidence of SLAP-lesions (superior labrum from anterior to posterior) [24–26]. Following the undersurface of the rotator cuff the supraspinatus tendon is significantly entrapped between the humeral head and the posterior superior labrum. So that findings typical for PSI include articular-sided partial thickness rotator cuff tears and concomitant posterosuperior or posterior labral injuries. However, Burkhart et al. suggest a second theory claiming the posterosuperior contact to be physiological [13]. They suggest that rotator cuff tears originate from repetitive injury to the supraspinatus tendon during the deceleration phase. This theory is supported by the fact that a non-pathological interposition of the rotator cuff and the posterosuperior labrum between the glenoid rim and the greater tuberosity occurs in throwers and non-throwers alike. Cadaveric, MRI, and arthroscopic studies have consistently shown that contact of the rotator cuff with the posterosuperior labrum is physiological [27, 28].
Anterosuperior impingement (ASI)
In contrast to PSI, the anterosuperior impingement (ASI) is significantly less common. It involves an impingement of the subscapularis tendon between the anterior humeral head and the anterosuperior glenoid and labrum during forward flexion of the arm. When the arm is in a position of horizontal adduction and internal rotation, the undersurface of the reflection pulley and the subscapularis tendon impinges against the anterosuperior glenoid rim. In this context, lesions of the long head of the biceps (LHB), the pulley, and the rotator cuff have been associated with an ASI of the shoulder. Habermeyer et al. stated that a forcefully stopped overhead throwing motion might generate a pulley lesion [29]. During active contraction of the biceps muscle in internal rotation, the strain increases while the elbow extension is decelerated. A maximal contraction of the LHB is provoked by this deceleration and can cause tears in the rotator interval capsule. Gerber and Sebesta described the pulley lesions resulting from repetitive forceful internal rotation above the horizontal plane [30]. This leads to frictional damage between the pulley system and the subscapularis tendon on the one hand and the anterior superior glenoid rim on the other. As a result of intrinsic degenerative changes, the rotator interval shows partial tears involving the superior glenohumeral ligament (SGHL) and the articular side of the supraspinatus tendon. In 1996 Habermeyer and Walch showed that 50% of cases of biceps tendon subluxation were associated with degenerative changes in the anterosuperior aspect of the labrum, suggestive of a correlation between these intrinsic structural changes [31, 32]. In a previous work we reported on another possible aetiology of ASI [33]. In a large series of young patients with paraplegia of the lower extremity (using wheel chairs) we observed a significant number of lesions of the anterior-superior complex. This most likely originates from repetitive active contraction of the biceps muscle in internal rotation during wheel turning. Similar to the theory of Habermeyer et al. this deceleration may lead to tears in the rotator interval capsule [29].
Clinical evaluation
Internal impingement typically affects young to middle-aged adults; in most major case series of internal impingement, patients are under 40 years of age and participate in activities involving repetitive abducting and externally rotating arm motions or positions [12, 34, 35]. The majority of patients who have been identified with internal impingement are overhead athletes [36, 37]. For example, the first major series by Walch et al. primarily consisted of volleyball and tennis players [19]. The largest athletic group with internal impingement studied has been the throwing athletes, in particular baseball players [19, 38, 39]. Medial evaluation of a thrower begins with a good thorough history of the problem. In eliciting the history of the injury, determining if the resulting symptoms are of vague character and of gradual onset or occurred as the result of an acute incident is important [23, 40–42]. Most patients present with a progressive decrease in throwing velocity or a loss of control and performance [43–45]. Chronic, diffuse posterior shoulder girdle pain is common in terms of the presenting complaint, but the pain may be localised to the joint line. Despite posterior shoulder pain being the most common complaint among patients with internal impingement, patients may also present with symptoms similar to those associated with classic rotator cuff disease [7, 30]. Alternatively, patients may also have instability symptoms, such as apprehension or the sensation of subluxation with the arm in an abduction and external rotation position. Notably, Burkhart et al. reported an 80% rate of anterior coracoid pain in their series of 96 athletes with a disabled throwing shoulder, rather than isolated posterior shoulder pain, described as the most common presenting symptom [46].
Posterior glenohumeral joint line tenderness, increased external rotation, and decreased internal rotation are the most common physical examination findings in throwing athletes (see Fig. 1). However, all patients suspected for internal impingement should be evaluated with a complete shoulder examination due to the high rate of other pathological shoulder conditions associated with internal impingement. During physical examination, the relative hypertrophy of the dominant arm versus areas of atrophy, especially in the infraspinatus fossa, can sometimes be palpated. In addition, for the documentation of bilateral active and passive motion of the shoulders, testing for SLAP lesions, “classic” impingement signs such as the Neer and Hawkins tests, cross-body adduction tests, and instability testing should be performed [47, 48]. As for the assessment of laxity, which does not automatically correspond to instability, the sulcus-sign should be determined. Additionally, the other parameters of the Beighton score should be analysed. For evaluation of anteroposterior translation of the humeral head the “anterior-and-posterior-drawer-test” as well as the “load-and-shift-test” should be used. Despite significant controversy regarding the validity of various physical examination manoeuvres for detecting SLAP tears the performance of a combination of these tests is generally indicated because superoposterior labral tears are a cardinal feature of internal impingement [49, 50]. We favour the O’Brien test, which was reported by the author with 100% sensitivity and 98.5% specificity for the active compression test. It is performed with the arm positioned in 90° forward flexion, 20° adduction, and in maximal internal rotation. Resistance creates pain in the anterior superior shoulder being relieved by resistance with maximal external rotation or supination of the forearm. Meister et al. investigated the ability of a single manoeuvre, referred to as the “posterior impingement sign,” to detect the presence of articular-sided rotator cuff tears and posterior labrum lesions [51]. The subjects were tested for the presence of deep posterior shoulder pain when the arm was brought into a position similar to that noted during the late cocking phase of throwing. The sensitivity and specificity of the posterior impingement sign were 75.5% and 85%, respectively. Notably all patients with noncontact injuries with a positive test had arthroscopic findings amenable to surgical treatment. Regarding conventional impingement tests, Mithöfer et al. reported that subacromial impingement tests are usually negative in patients with known internal impingement [52]. In contrast, one study reported that of the 41 professional throwing athletes arthroscopically evaluated, over 25% demonstrated a positive Neer or Hawkins sign. In our opinion one of the absolute typical findings is GIRD, defined by a loss of greater than 30–40° of internal rotation relative to the expected gain in external rotation, compared to the contralateral side. With regard to concomitant increased external rotation, Myers et al. recently emphasised that throwers with pathological internal impingement exhibiting significantly increased posterior shoulder tightness and glenohumeral internal rotation deficits do not necessarily gain significantly increased external rotation [9]. In addition, scapular dyskinesis is a commonly reported finding. Characteristic features include a prominent inferior medial border of the scapula and the appearance of an inferiorly dropped throwing shoulder compared to the non-throwing side [53].
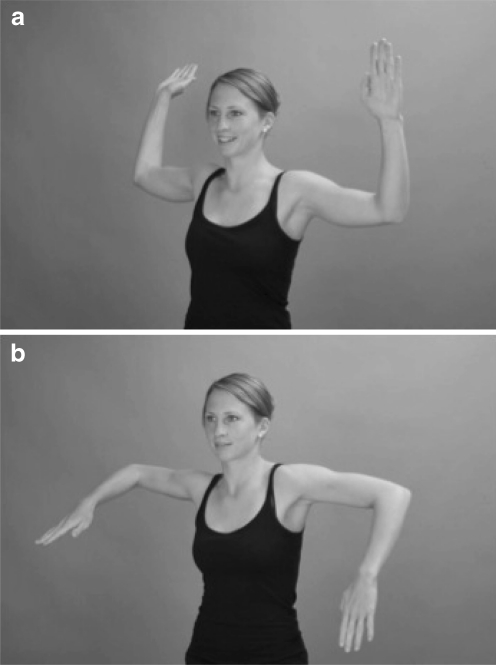
Fig. 1.
The typical clinical finding of a patient with glenohumeral internal rotation deficit (GIRD) is demonstrated. In figure a the increased external rotation of the right shoulder is visible. In contrast in figure b the loss of internal rotation is demonstrated
Imaging modalities
Radiographic findings
Radiographic evaluation of patients with internal impingement include true AP, axillary and Y-view radiographs of the shoulder [54]. Usually only minimal findings are present. Regarding typical signs, Bennett et al. described an exostosis of the posteroinferior glenoid rim (Bennett lesion) in baseball players [2]. He postulated that this occurs secondary to triceps traction [1, 51]. In this context Ferrari et al. reported on baseball pitchers with posteroinferior ossifying lesions, none of which were located in the region of the triceps tendon [55]. Changes of the greater tuberosity are also commonly found on the radiographs of internal impingement patients. Mithöfer et al. stressed the importance of radiographically assessing the greater tuberosity for sclerotic and cystic changes; these findings are present in approximately half of the patients with internal impingement [52]. Interestingly, a recent radiographic study analysing 57 asymptomatic professional baseball pitchers demonstrated that cystic changes in the humeral head were present in 39% of the shoulders examined [56]. Walch et al. noted a further lesion, the so-called posterior humeral head geodes, corresponding to osteochondral defects located superiorly close to the insertion of the supraspinatus tendon [19]. Another finding that may be seen on radiographs of internal impingement patients is rounding or remodelling of the posterior glenoid rim, although MRI is the optimal modality to appreciate this phenomenon [52].
MRI findings
MRI is considered the gold standard in the work-up of any young patient presenting with shoulder pain [1]. When labral lesions are suspected, we recommend direct MR-arthrography using either gadolinium contrast material or combined with saline [57–59]. MR findings in internal impingement include articular-sided partial-thickness rotator cuff tears of the supraspinatus, infraspinatus, or both tendons, and posterior or superior labral lesions [60]. The tears of the rotator cuff tendons are usually small and involve the articular surface. Internal impingement tears are better diagnosed on MR arthrography as a small undersurface linear contrast extension into the tendon. Abduction and external rotation (ABER) positioning may be useful for tear detection in these patients [61], since a relaxation of the posterior superior rotator cuff may allow for gadolinium to seep into an otherwise occult or subtle tear (see Fig. 2). Interestingly, Halbrecht et al. performed non-contrast MRI of the shoulder in an ABER-position in the throwing and non-throwing arm of asymptomatic college baseball players and observed contact between the rotator cuff and the posterosuperior glenolabral complex in all shoulders [62]. In addition, these athletes often present with associated posterosuperior labral abnormalities. Repetitive stress encountered in pitchers also speeds up the normal aging process of the rotator cuff leading to an early tendinosis. Rim-rent tears from tensile overload can be seen at the articular surface at the humeral tendinous insertion [63]. These tears show high signal intensity extending between the greater tuberosity tendon insertion (supraspinatus foot print) and the tendon itself on fluid-sensitive sequences. In most cases they are located in the anterior half of the supraspinatus tendon and can be mistaken for intratendinous signal. Other tensile overload injuries usually present as tiny tears at the articular surface of the supraspinatus and infraspinatus tendon. These tears are often small and best recognised on MR arthrography in the ABER position as fluid intensity or extension of intra-articular contrast medium into the hypointense line on the articular surface of the rotator cuff tendons. The glenoid labrum is often torn in pitchers without perceptible underlying shoulder instability [64]. SLAP tears with significant posterior extension can be disabling for pitchers, because of associated posterior superior laxity [65]. The appearance of SLAP tears on MRI includes intermediate hyperintense labral degeneration and linear fluid or gadolinium undercutting the superior labrum extending posteriorly to the biceps tendon’s origin. Cysts and impaction deformity are also seen at the posterior greater tuberosity and can increase diagnostic confidence in the diagnosis of internal impingement.
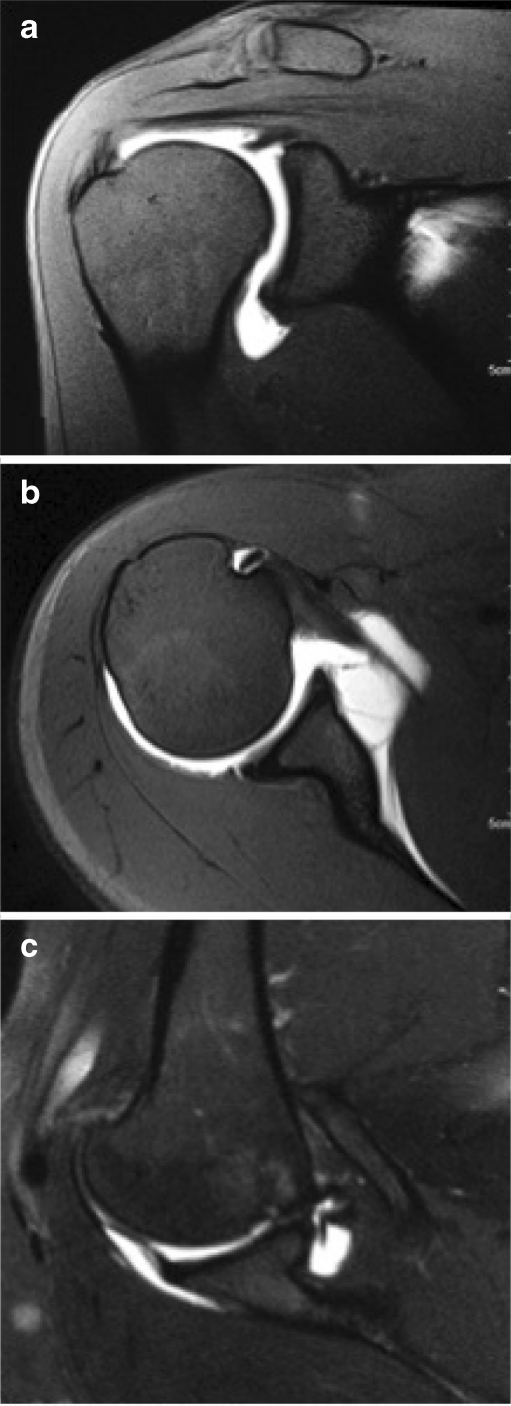
Fig. 2.
Posterior superior glenohumeral impingement. T1-weighted fat-saturated abduction and external rotation (ABER) image of shoulder MR arthrogram shows an articular surface tear at the posterior supraspinatus. There is also a superior labral tear and small cyst at the greater tuberosity
Therapy
The vast majority of shoulder injuries in throwers should initially be treated with a conservative, non-operative regime. Only significant structural injuries such as an acute rotator cuff tear, dislocation or SLAP lesion deserve early surgical intervention.
Nonoperative treatment
Every overhead athlete requires a training program that strengthens all elements of the kinetic chain of the throwing motion. Patients with mild symptoms and early phases of the disorder need active rest, including a complete break from throwing along with physical therapy. Axe et al. propose a two days off-period for every day symptoms have been present (maximum break of 12 weeks) [66]. Anti-inflammatory measures to “cool down” the irritated shoulder can be beneficial in accelerating the rehabilitation process. This includes nonsteroidal anti-inflammatory drugs (NSAIDs), occasionally a corticosteroid injection, and physical therapy modalities such as iontophoresis. For patients with longer-lasting problems, Wilk et al. suggested the following phased progression of the rehabilitation program, emphasising dynamic stability, rotator cuff strengthening and a scapular stabilisation program [67].
Phase I: Acute phase The primary aims of the initial stage are aimed at allowing the injured tissue to heal, plus modification of activity, decreasing pain and inflammation, and on the re-establishment of a baseline dynamic stability, correction of the muscle balance, and restoration of proprioception. Reduction of the athlete’s pain and inflammation is accomplished through the use of local therapeutic modalities such as ice, ultrasound, and electrical stimulation. In addition, the athlete’s activities (such as throwing and exercises) must be modified to a pain-free level. Active-assisted motion exercises may be used to normalise shoulder motion, particularly shoulder internal rotation and horizontal adduction. The thrower should perform specific stretches and flexibility exercises for the benefit of the posterior rotator cuff muscles.
Phase II: Intermediate phase When pain and inflammation have decreased, the athlete may proceed to phase II. The primary goals are to intensify the strengthening program, continue to improve flexibility, and facilitate neuromuscular control. During this phase, the rehabilitation program is progressed to more aggressive isotonic strengthening activities with emphasis on restoration of the muscle balance. Selective muscle activation is also used to restore muscle balance and symmetry. Contractures of the posterior structures, the pectoralis minor muscle, and the short head of the biceps muscle also contribute to a glenohumeral internal rotation deficit and increase the anterior tilting of the scapula. McClure et al. showed the use of the cross-body stretch for the treatment of patients with posterior shoulder tightness leading to a significantly greater increase of the internal rotation compared to a control group with normal shoulder motion not performing exercises [68]. Borstad et al. found the sleeper stretch (see Fig. 3) and the supine manual stretch to be effective for lengthening of the pectoralis minor muscle [69]. In the overhead thrower, the shoulder external rotator muscles, scapular retractor muscles, and protractor and depressor muscles are frequently isolated due to structural weakness. Several authors have emphasised the importance of scapular muscle strength and neuromuscular control as a contribution to normal shoulder function [53]. Isotonic exercise techniques are used to strengthen the scapular muscles. Overhead throwing athletes often exhibit external rotator muscle weakness. Also during this second rehabilitation phase, the overhead-throwing athlete is instructed to perform core-strengthening exercises for the abdominal and lower back musculature. In addition, the athlete should perform lower extremity strengthening and participate in a running program including jogging and sprints. Upper extremity stretching exercises are continued as needed to maintain soft tissue flexibility.
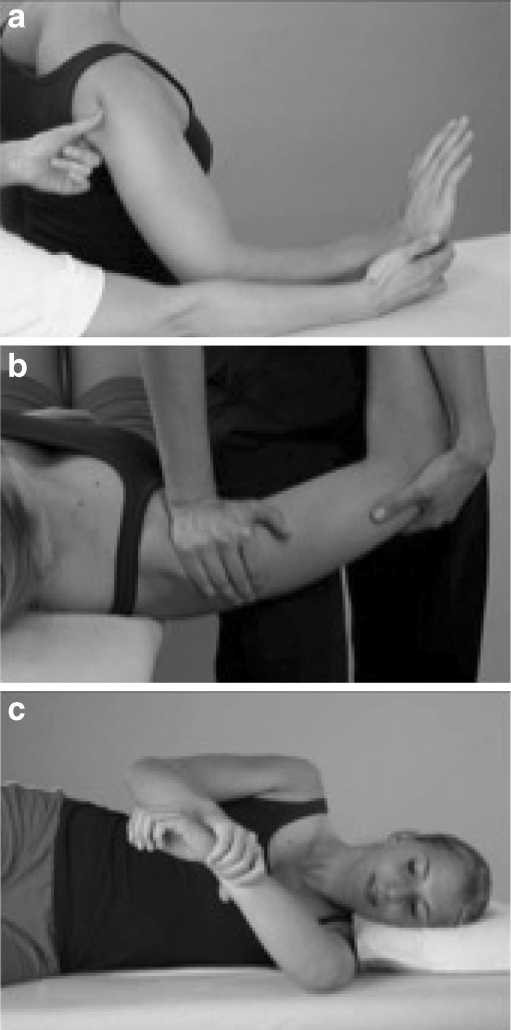
Fig. 3.
The sleeper stretch: the patient on the involved side with the shoulder in 90° of forward elevation. The contralateral arm internally rotates the involved shoulder until a stretch on the posterior aspect of the shoulder
Phase III: Advanced strengthening phase The goals are to initiate aggressive strengthening drills, enhance power and endurance, perform functional drills, and gradually initiate throwing activities. During this phase, the athlete performs the “thrower’s ten” exercise program, continues manual resistance stabilisation drills, and starts with plyometric drills. Dynamic stabilisation drills are also performed to enhance proprioception and neuromuscular control. These drills include rhythmic stabilisation exercise drills. Plyometric training may be used to enhance dynamic stability and proprioception as well as to gradually increase the functional stress put on the shoulder joint. Plyometric exercises entail a rapid transfer of eccentric to concentric contraction to allow for stimulation of muscle spindles, which facilitates a recruitment of muscle fibres. An interval throwing program may be initiated in this phase of rehabilitation. This program begins with short, flat ground throwing at variable distances. When the throwing program is initiated, a less-intensive, high-repetition, low-weight program to avoid overtraining should replace intensive strengthening.
Phase IV: Return-to-throwing phase This phase usually involves progression of the interval throwing program as well as neuromuscular maintenance. While the athlete is performing the interval-throwing program, the clinician should carefully monitor the thrower’s mechanics and throwing intensity. The athlete advances to position-specific throwing provided that he or she remains asymptomatic. The goal is to return to the full throwing velocity over the course of three months. To prevent the effects of overtraining or throwing, it is essential to instruct the athlete what to do through specific exercises throughout the year. A lack of improvement after three months, or an inability to return to competition within six months constitutes failure of the non-operative conservative management and thus should result in an additional diagnostic testing and, if necessary, operative intervention should be considered.
Surgical treatment
Indications for surgery include the failure of conservative treatment with an inability to return to competition despite a prolonged rehabilitation protocol geared towards a correction or resolution of the pathology diagnosed by physical examination and imaging [12, 70]. The operative approach to patients with signs and symptoms of internal impingement should be pursued in a deliberate, methodical fashion. The final therapeutic plan in symptomatic throwing shoulders depends on the specific examination findings under anaesthesia because physical findings in the alert patient may be confusing. The following arthroscopic examination is performed in terms of a systematic review of the entire shoulder. In addition, injury of many other structures of the shoulder besides the postero-superior labrum and the rotator cuff has been associated with pathological internal impingement. Jobe has suggested that as many as five anatomical structures are at risk: the postero-superior labrum, the rotator cuff tendon (articular surface), the greater tuberosity, the inferior glenohumeral ligament (IGHL) complex, and the postero-superior glenoid [21]. He noted that the majority of patients with internal impingement present with an injury of more than one of the five structures at the time of arthroscopic assessment, underscoring the importance of a thorough diagnostic arthroscopic assessment of the shoulder joint in the setting of suspected internal impingement or in cases when a typical internal impingement lesion is unexpectedly detected. The surgeon should carefully evaluate the entire shoulder and look for evidence of instability in the biceps tendon, biceps anchor, labrum, and capsule. Presence of a drive-through sign should be elicited by sweeping the arthroscope from superior to inferior to assess laxity. The surgeon should evaluate the rotator interval and the rotator cuff insertion consecutively. The examined arm should then be removed from traction and an ABER examination should be performed with the arm in a position of abduction and external rotation. During this manoeuvre the arthroscope is located in the posterior portal, just off the posterior superior labrum, and then the arm is carefully abducted and externally rotated. The surgeon evaluates evidence of kissing lesions between the undersurface of the rotator cuff and the posterior superior labrum as seen in pathological internal impingement. Repetitive microtrauma to the greater tuberosity or the posterosuperior rim of the glenoid may represent extremes of the spectrum of injury caused by the abducted, externally rotated position associated with internal impingement, but even fracture of these structures have been reported. Although osteochondral lesions of the humeral head have also been described, it is likely that these originate from a similar mechanism to greater tuberosity changes, with subtle variations in the anatomy or the throwing motion accounting for a different site of humeral head contact with the glenoid rim. Surgical intervention should be directed towards specific pathological lesions believed to correspond to the patient’s symptoms or play a role in the complex pathophysiology of internal impingement. Subacromial bursectomy may be warranted in cases when substantial degrees of subacromial inflammation and bursitis are noted at the time of surgery [71, 72]. Mithöfer et al. also suggested that internal impingement represents a relative contraindication to acromioplasty [52].
Return to sports
A formal throwing mechanics evaluation may be helpful, particularly in the younger athlete with less specialised training. The mature athlete with altered or poor throwing mechanics may also benefit from biomechanical and professional evaluation. Once an appropriate rest period has passed and symptoms are relieved, throwing is resumed with an interval throwing program; however, the shoulder should be completely free of pain prior to resuming any throwing activities. Intensity is advanced based on symptoms, or the lack thereof, with the goal of returning to effective throwing.
Summary
During the throwing motion enormous stress is put on both the dynamic and the static stabilisers of the shoulder. These repetitive forces cause adaptive soft tissue and bone changes which lead in the longer term to shoulder pathologies. Although a broad range of theories have been suggested for the pathophysiology of internal impingement, the causes are obviously multifactorial. The cardinal lesions of internal impingement, articular-sided rotator cuff tears and posterosuperior labral lesions, have been shown to occur in association with a number of other findings, most importantly glenohumeral internal rotation deficit and SICK scapula syndrome, but also with posterior humeral head lesions, posterior glenoid bony injury and, rarely, with Bankart and inferior glenohumeral ligament lesions. In any event the history of symptoms described by the patient is of great importance in order to understand the pathophysiological problems.
As regards therapy, the majority of shoulder injuries in throwers should initially be treated with conservative, non-operative methods including a phase-adapted progressive physical therapy, strengthening all elements of the kinetic chain of the throwing motion, along with anti-inflammatory measures to “cool down” the irritated shoulder possibly being beneficial in accelerating the rehabilitative process.
Only significant structural injuries such as an acute rotator cuff tear, dislocation or SLAP lesion deserve early surgical intervention. Indications for surgery include the failure of conservative treatment with an inability to return to competition despite a prolonged rehabilitation protocol. The operative approach is based on the specific examination findings under anaesthesia because physical findings in the alert patient may be confusing. During arthroscopy the surgeon should carefully evaluate the entire shoulder and look for evidence of instability in the biceps tendon, biceps anchor, labrum, and capsule. Surgical intervention should be directed towards specific pathological lesions believed to correspond to the patient’s symptoms or play a role in the complex pathophysiology of internal impingement.
After an appropriate period of rest and relief of symptoms, throwing is only resumed with an interval-throwing program when the athlete is completely free of pain. Intensity is advanced based on symptoms, or the lack thereof, with the goal of returning to effective throwing.
References
- 1.Heyworth BE, Williams RJ., 3rd Internal impingement of the shoulder. Am J Sports Med. 2009;37:1024–1037. doi: 10.1177/0363546508324966. [DOI] [PubMed] [Google Scholar]
- 2.Bennett GE. Shoulder and elbow lesions distinctive of baseball players. Ann Surg. 1947;126:107–110. doi: 10.1097/00000658-194707000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Budoff JE, Nirschl RP, Ilahi OA, Rodin DM. Internal impingement in the etiology of rotator cuff tendinosis revisited. Arthroscopy. 2003;19:810–814. doi: 10.1016/S0749-8063(03)00732-1. [DOI] [PubMed] [Google Scholar]
- 4.Lombardo SJ, Jobe FW, Kerlan RK, Carter VS, Shields CL., Jr Posterior shoulder lesions in throwing athletes. Am J Sports Med. 1977;5:106–110. doi: 10.1177/036354657700500302. [DOI] [PubMed] [Google Scholar]
- 5.Jobe FW, Moynes DR, Tibone JE, Perry J. An EMG analysis of the shoulder in pitching. A second report. Am J Sports Med. 1984;12:218–220. doi: 10.1177/036354658401200310. [DOI] [PubMed] [Google Scholar]
- 6.Altchek DW, Dines DM. Shoulder injuries in the throwing athlete. J Am Acad Orthop Surg. 1995;3:159–165. doi: 10.5435/00124635-199505000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Fleisig GS, Andrews JR, Dillman CJ, Escamilla RF. Kinetics of baseball pitching with implications about injury mechanisms. Am J Sports Med. 1995;23:233–239. doi: 10.1177/036354659502300218. [DOI] [PubMed] [Google Scholar]
- 8.Burkhart SS, Morgan CD, Kibler WB. Shoulder injuries in overhead athletes. The "dead arm" revisited. Clin Sports Med. 2000;19:125–158. doi: 10.1016/S0278-5919(05)70300-8. [DOI] [PubMed] [Google Scholar]
- 9.Myers JB, Laudner KG, Pasquale MR, Bradley JP, Lephart SM. Glenohumeral range of motion deficits and posterior shoulder tightness in throwers with pathologic internal impingement. Am J Sports Med. 2006;34:385–391. doi: 10.1177/0363546505281804. [DOI] [PubMed] [Google Scholar]
- 10.Burkhart SS. Internal impingement of the shoulder. Instr Course Lect. 2006;55:29–34. [PubMed] [Google Scholar]
- 11.Fleisig GS, Escamilla RF, Andrews JR, Matsuo T, Satterwhite Y, Barrentine SW. Kinematic and kinetic comparison between baseball pitching and football passing. J Appl Biomech. 1996;12:18. [Google Scholar]
- 12.Braun S, Kokmeyer D, Millett PJ. Shoulder injuries in the throwing athlete. J Bone Joint Surg Am. 2009;91:966–978. doi: 10.2106/JBJS.H.01341. [DOI] [PubMed] [Google Scholar]
- 13.Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology. Part I: pathoanatomy and biomechanics. Arthroscopy. 2003;19:404–420. doi: 10.1053/jars.2003.50128. [DOI] [PubMed] [Google Scholar]
- 14.Jobe CM, Coen MJ, Screnar P. Evaluation of impingement syndromes in the overhead-throwing athlete. J Athl Train. 2000;35:293–299. [PMC free article] [PubMed] [Google Scholar]
- 15.Kibler WB. The role of the scapula in athletic shoulder function. Am J Sports Med. 1998;26:325–337. doi: 10.1177/03635465980260022801. [DOI] [PubMed] [Google Scholar]
- 16.Imhoff AB, Agneskirchner JD, Konig U, Temme C, Ottl G, McFarland EG. Superior labrum pathology in the athlete. Orthopade. 2000;29:917–927. doi: 10.1007/s001320050542. [DOI] [PubMed] [Google Scholar]
- 17.Ticker JB, Beim GM, Warner JJ. Recognition and treatment of refractory posterior capsular contracture of the shoulder. Arthroscopy. 2000;16:27–34. doi: 10.1016/S0749-8063(00)90124-5. [DOI] [PubMed] [Google Scholar]
- 18.Rossi F. Shoulder impingement syndromes. Eur J Radiol. 1998;27(Suppl 1):S42–S48. doi: 10.1016/S0720-048X(98)00042-4. [DOI] [PubMed] [Google Scholar]
- 19.Walch G, Liotard JP, Boileau P, Noel E. Postero-superior glenoid impingement. Another impingement of the shoulder. J Radiol. 1993;74:47–50. [PubMed] [Google Scholar]
- 20.Davidson PA, Elattrache NS, Jobe CM, Jobe FW. Rotator cuff and posterior-superior glenoid labrum injury associated with increased glenohumeral motion: a new site of impingement. J Shoulder Elbow Surg. 1995;4:384–390. doi: 10.1016/S1058-2746(95)80023-9. [DOI] [PubMed] [Google Scholar]
- 21.Jobe CM (1996) Superior glenoid impingement. Current concepts. Clin Orthop Relat Res 330:98–107 [PubMed]
- 22.Gumina S, Carbone S, Postacchini F. Scapular dyskinesis and SICK scapula syndrome in patients with chronic type III acromioclavicular dislocation. Arthroscopy. 2009;25:40–45. doi: 10.1016/j.arthro.2008.08.019. [DOI] [PubMed] [Google Scholar]
- 23.Tischer T, Salzmann GM, Imhoff AB. Rotator cuff tears and internal impingement in athletes. Orthopade. 2007;36(950):952–956. doi: 10.1007/s00132-007-1150-z. [DOI] [PubMed] [Google Scholar]
- 24.Liu SH, Boynton E. Posterior superior impingement of the rotator cuff on the glenoid rim as a cause of shoulder pain in the overhead athlete. Arthroscopy. 1993;9:697–699. doi: 10.1016/S0749-8063(05)80510-9. [DOI] [PubMed] [Google Scholar]
- 25.Ludewig PM, Cook TM. Translations of the humerus in persons with shoulder impingement symptoms. J Orthop Sports Phys Ther. 2002;32:248–259. doi: 10.2519/jospt.2002.32.6.248. [DOI] [PubMed] [Google Scholar]
- 26.Mihata T, McGarry MH, Tibone JE, Fitzpatrick MJ, Kinoshita M, Lee TQ. Biomechanical assessment of type II superior labral anterior-posterior (SLAP) lesions associated with anterior shoulder capsular laxity as seen in throwers: a cadaveric study. Am J Sports Med. 2008;36:1604–1610. doi: 10.1177/0363546508315198. [DOI] [PubMed] [Google Scholar]
- 27.Murray PJ, Shaffer BS. Clinical update: MR imaging of the shoulder. Sports Med Arthrosc. 2009;17:40–48. doi: 10.1097/JSA.0b013e31819602a6. [DOI] [PubMed] [Google Scholar]
- 28.Tirman PF, Bost FW, Garvin GJ, Peterfy CG, Mall JC, Steinbach LS, Feller JF, Crues JV., 3rd Posterosuperior glenoid impingement of the shoulder: findings at MR imaging and MR arthrography with arthroscopic correlation. Radiology. 1994;193:431–436. doi: 10.1148/radiology.193.2.7972758. [DOI] [PubMed] [Google Scholar]
- 29.Habermeyer P, Magosch P, Pritsch M, Scheibel MT, Lichtenberg S. Anterosuperior impingement of the shoulder as a result of pulley lesions: a prospective arthroscopic study. J Shoulder Elbow Surg. 2004;13:5–12. doi: 10.1016/j.jse.2003.09.013. [DOI] [PubMed] [Google Scholar]
- 30.Gerber C, Sebesta A. Impingement of the deep surface of the subscapularis tendon and the reflection pulley on the anterosuperior glenoid rim: a preliminary report. J Shoulder Elbow Surg. 2000;9:483–490. doi: 10.1067/mse.2000.109322. [DOI] [PubMed] [Google Scholar]
- 31.Gleyze P, Habermeyer P. [Arthroscopic aspects and chronologic outcome of lesions of the labro-ligament complex in post-traumatic antero-inferior instability of the shoulder. A prospective study of 91 cases] Rev Chir Orthop Reparatrice Appar Mot. 1996;82(4):288–298. [PubMed] [Google Scholar]
- 32.Walch G. Chronic anterior glenohumeral instability. J Bone Joint Surg Br. 1996;78:670–677. [PubMed] [Google Scholar]
- 33.Krzycki J, Tischer T, Imhoff AB. The para-shoulder: lesions of the anterior-superior complex (Labrum, SGHL, SSC) and their arthroscopic treatment. Z Orthop Ihre Grenzgeb. 2006;144:446–448. doi: 10.1055/s-2006-954403. [DOI] [PubMed] [Google Scholar]
- 34.Struhl S. Anterior internal impingement: an arthroscopic observation. Arthroscopy. 2002;18:2–7. doi: 10.1053/jars.2002.29868. [DOI] [PubMed] [Google Scholar]
- 35.Tirman PF, Smith ED, Stoller DW, Fritz RC. Shoulder imaging in athletes. Semin Musculoskelet Radiol. 2004;8:29–40. doi: 10.1055/s-2004-823013. [DOI] [PubMed] [Google Scholar]
- 36.Werner SL, Guido JA, Jr, Stewart GW, McNeice RP, VanDyke T, Jones DG. Relationships between throwing mechanics and shoulder distraction in collegiate baseball pitchers. J Shoulder Elbow Surg. 2007;16:37–42. doi: 10.1016/j.jse.2006.05.007. [DOI] [PubMed] [Google Scholar]
- 37.Sonnery-Cottet B, Edwards TB, Noel E, Walch G. Results of arthroscopic treatment of posterosuperior glenoid impingement in tennis players. Am J Sports Med. 2002;30:227–232. doi: 10.1177/03635465020300021401. [DOI] [PubMed] [Google Scholar]
- 38.Rossi F, Ternamian PJ, Cerciello G, Walch G. Posterosuperior glenoid rim impingement in athletes: the diagnostic value of traditional radiology and magnetic resonance. Radiol Med. 1994;87:22–27. [PubMed] [Google Scholar]
- 39.McFarland EG, Hsu CY, Neira C, O'Neil O. Internal impingement of the shoulder: a clinical and arthroscopic analysis. J Shoulder Elbow Surg. 1999;8:458–460. doi: 10.1016/S1058-2746(99)90076-9. [DOI] [PubMed] [Google Scholar]
- 40.Buss DD, Freehill MQ, Marra G. Typical and atypical shoulder impingement syndrome: diagnosis, treatment, and pitfalls. Instr Course Lect. 2009;58:447–457. [PubMed] [Google Scholar]
- 41.Campbell RS, Dunn A. External impingement of the shoulder. Semin Musculoskelet Radiol. 2008;12:107–126. doi: 10.1055/s-2008-1078699. [DOI] [PubMed] [Google Scholar]
- 42.Carter AB, Kaminski TW, Douex AT, Jr, Knight CA, Richards JG. Effects of high volume upper extremity plyometric training on throwing velocity and functional strength ratios of the shoulder rotators in collegiate baseball players. J Strength Cond Res. 2007;21:208–215. doi: 10.1519/00124278-200702000-00038. [DOI] [PubMed] [Google Scholar]
- 43.Cools AM, Cambier D, Witvrouw EE. Screening the athlete's shoulder for impingement symptoms: a clinical reasoning algorithm for early detection of shoulder pathology. Br J Sports Med. 2008;42:628–635. doi: 10.1136/bjsm.2008.048074. [DOI] [PubMed] [Google Scholar]
- 44.Cools AM, Declercq G, Cagnie B, Cambier D, Witvrouw E. Internal impingement in the tennis player: rehabilitation guidelines. Br J Sports Med. 2008;42:165–171. doi: 10.1136/bjsm.2007.036830. [DOI] [PubMed] [Google Scholar]
- 45.Curtis AS, Deshmukh R. Throwing injuries: diagnosis and treatment. Arthroscopy. 2003;19(Suppl 1):80–85. doi: 10.1016/j.arthro.2003.09.030. [DOI] [PubMed] [Google Scholar]
- 46.Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology. Part III: the SICK scapula, scapular dyskinesis, the kinetic chain, and rehabilitation. Arthroscopy. 2003;19:641–661. doi: 10.1016/S0749-8063(03)00389-X. [DOI] [PubMed] [Google Scholar]
- 47.Hamner DL, Pink MM, Jobe FW. A modification of the relocation test: arthroscopic findings associated with a positive test. J Shoulder Elbow Surg. 2000;9:263–267. doi: 10.1067/mse.2000.105450. [DOI] [PubMed] [Google Scholar]
- 48.Hegedus EJ, Goode A, Campbell S, Morin A, Tamaddoni M, Moorman CT, 3rd, Cook C. Physical examination tests of the shoulder: a systematic review with meta-analysis of individual tests. Br J Sports Med. 2008;92:80–92. doi: 10.1136/bjsm.2007.038406. [DOI] [PubMed] [Google Scholar]
- 49.Jari S, Sallay P. Quantification of posterior capsule tightness and motion loss in patients with shoulder impingement. Am J Sports Med. 2001;29:534. doi: 10.1177/03635465010290042601. [DOI] [PubMed] [Google Scholar]
- 50.Jazrawi LM, McCluskey GM, 3rd, Andrews JR. Superior labral anterior and posterior lesions and internal impingement in the overhead athlete. Instr Course Lect. 2003;52:43–63. [PubMed] [Google Scholar]
- 51.Meister K. Internal impingement in the shoulder of the overhand athlete: pathophysiology, diagnosis, and treatment. Am J Orthop. 2000;29:433–438. [PubMed] [Google Scholar]
- 52.Mithöfer K, Fealey S, Altchek D (2004) Arthroscopic treatment of internal impingement of the shoulder. Tech Shoulder Elbow Surg 5:66–75
- 53.Kibler WB. Scapular involvement in impingement: signs and symptoms. Instr Course Lect. 2006;55:35–43. [PubMed] [Google Scholar]
- 54.Braunstein V, Korner M, Brunner U, Mutschler W, Biberthaler P, Wiedemann E. The fulcrum axis: a new method for determining glenoid version. J Shoulder Elbow Surg. 2008;17:819–824. doi: 10.1016/j.jse.2008.02.018. [DOI] [PubMed] [Google Scholar]
- 55.Ferrari JD, Ferrari DA, Coumas J, Pappas AM. Posterior ossification of the shoulder: the Bennett lesion. Etiology, diagnosis, and treatment. Am J Sports Med. 1994;22:171–175. doi: 10.1177/036354659402200204. [DOI] [PubMed] [Google Scholar]
- 56.Wright RW, Steger-May K, Klein SE. Radiographic findings in the shoulder and elbow of Major League Baseball pitchers. Am J Sports Med. 2007;35:1839–1843. doi: 10.1177/0363546507304493. [DOI] [PubMed] [Google Scholar]
- 57.Huber DJ, Koch E. Magnetic resonance tomography in disorders of the rotator cuff. Orthopade. 1995;24:491–497. [PubMed] [Google Scholar]
- 58.Palmer WE, Brown JH, Rosenthal DI. Labral-ligamentous complex of the shoulder: evaluation with MR arthrography. Radiology. 1994;190:645–651. doi: 10.1148/radiology.190.3.8115604. [DOI] [PubMed] [Google Scholar]
- 59.Sasaki T, Saito Y, Yodono H, Prado GL, Miura H, Itabashi Y, Ishibashi Y. Labral-ligamentous complex of the shoulder. Evaluation with double oblique axial MR arthrography. Acta Radiol. 2003;44:435–439. doi: 10.1080/j.1600-0455.2003.00091.x. [DOI] [PubMed] [Google Scholar]
- 60.Wörtler k. Shoulder injuries in overhead sports. Radiologe. 2010;50(5):453–459. doi: 10.1007/s00117-009-1937-5. [DOI] [PubMed] [Google Scholar]
- 61.Bonutti PM, Norfray JF, Friedman RJ, Genez BM. Kinematic MRI of the shoulder. J Comput Assist Tomogr. 1993;17:666–669. doi: 10.1097/00004728-199307000-00033. [DOI] [PubMed] [Google Scholar]
- 62.Halbrecht JL, Tirman P, Atkin D. Internal impingement of the shoulder: comparison of findings between the throwing and nonthrowing shoulders of college baseball players. Arthroscopy. 1999;15:253–258. doi: 10.1016/S0749-8063(99)70030-7. [DOI] [PubMed] [Google Scholar]
- 63.Giaroli EL, Major NM, Higgins LD. MRI of internal impingement of the shoulder. AJR Am J Roentgenol. 2005;185:925–929. doi: 10.2214/AJR.04.0971. [DOI] [PubMed] [Google Scholar]
- 64.Beltran J, Rosenberg ZS, Chandnani VP, Cuomo F, Beltran S, Rokito A. Glenohumeral instability: evaluation with MR arthrography. Radiographics. 1997;17:657–673. doi: 10.1148/radiographics.17.3.9153704. [DOI] [PubMed] [Google Scholar]
- 65.Chang D, Mohana-Borges A, Borso M, Chung CB. SLAP lesions: anatomy, clinical presentation, MR imaging diagnosis and characterization. Eur J Radiol. 2008;68:72–87. doi: 10.1016/j.ejrad.2008.02.026. [DOI] [PubMed] [Google Scholar]
- 66.Axe MJ. Evaluation and treatment of common throwing injuries of the shoulder and elbow. Del Med J. 1987;59:593–598. [PubMed] [Google Scholar]
- 67.Wilk KE, Meister K, Andrews JR. Current concepts in the rehabilitation of the overhead throwing athlete. Am J Sports Med. 2002;30:136–151. doi: 10.1177/03635465020300011201. [DOI] [PubMed] [Google Scholar]
- 68.McClure P, Balaicuis J, Heiland D, Broersma ME, Thorndike CK, Wood A. A randomized controlled comparison of stretching procedures for posterior shoulder tightness. J Orthop Sports Phys Ther. 2007;37:108–114. doi: 10.2519/jospt.2007.2337. [DOI] [PubMed] [Google Scholar]
- 69.Borstad JD, Ludewig PM. Comparison of scapular kinematics between elevation and lowering of the arm in the scapular plane. Clin Biomech (Bristol, Avon) 2002;17:650–659. doi: 10.1016/S0268-0033(02)00136-5. [DOI] [PubMed] [Google Scholar]
- 70.Imhoff A, Ticker J, Fu FH. An atlas of shoulder arthroscopy. London, New York: Dunitz; 2003. [Google Scholar]
- 71.Tibone JE, Jobe FW, Kerlan RK, Carter VS, Shields CL, Lombardo SJ, Yocum LA (1985) Shoulder impingement syndrome in athletes treated by an anterior acromioplasty. Clin Orthop Relat Res 198:134–140 [PubMed]
- 72.Tibone JE, Elrod B, Jobe FW, Kerlan RK, Carter VS, Shields CL, Jr, Lombardo SJ, Yocum L. Surgical treatment of tears of the rotator cuff in athletes. J Bone Joint Surg Am. 1986;68:887–891. [PubMed] [Google Scholar]