Abstract
Two groups of patients were treated for pertrochanteric fractures (AO/ASIF 31A1+A2) with an intramedullary hip nail. In the first group of 44 patients distal dynamic locking was used, and in the second group of 74 patients the nail was not distally locked. Comparison of the two groups of patients did not show any difference in terms of the period of fracture healing, radiological and functional results or frequency of complications. In the group with a distally locked nail the surgery took 40.4 minutes, while in the group without distal locking only 34.4 minutes. In total, we recorded only seven complications, none of which were caused by absence of distal locking of the nail. This study has shown that distal locking of IMHN is unnecessary in most pertrochanteric fractures (AO/ASIF 31A1+2). The only exceptions are comminution of the lateral wall of the greater trochanter, secondary diaphyseal fracture line, large posteromedial fragment extended distally below the level of the lesser trochanter and broad intramedullary canal.
Introduction
The introduction of the gamma nail (GN) into clinical practice opened a new era in the treatment of trochanteric fractures. Apart from positive reports, articles also appeared pointing out problems associated with distal locking of the GN [1, 3, 10, 12, 17, 19]. As a result, some authors reduced their indications for distal locking in trochanteric fractures [6, 19, 20, 23] or they did not use it at all [3, 23]. Thanks to increasing experience with intramedullary hip nails (IMHN) and the improved design of the new generation of these implants, the number of complications caused by distal locking decreased but were not completely eliminated [7, 11, 13, 14, 16, 21, 22].
We have used the GN since 1994 and, within the learning curve, we also concentrated on the problems with distal locking [1, 7, 16]. Later, we started to use the second generation of the intramedullary hip nails (IMHN), i.e. PFN-Synthes and PFH-Medin. When evaluating complications associated with distal locking in pertrochanteric fractures treated with PFN and with PFH, we recorded three cases of failure of distal locking [7, 16]. However, these fractures healed without problems. This fact gave rise to the question whether pertrochanteric fractures require distal locking.
Patients and methods
Group of patients Between January 2006 and December 2007 we used PFH-Medin in a total of 118 patients with a pertrochanteric fracture (AO/ASIF 31A1+A2) who were followed-up for at least one-year postoperatively. The whole cohort of patients was subdivided into two groups. In group I comprising 44 patients, we performed distal dynamic locking of the nail while in group II including 74 patients, the distal locking was not performed. Basic characteristics of both groups (gender, average age, fracture type) are shown in Table 1.
Table 1.
Comparison of groups of patients with and without distal locking
| Description | Group I - distal locking | Group II - without distal locking | |||
|---|---|---|---|---|---|
| Male | 10 | 17 | |||
| Female | 34 | 57 | |||
| Total patients | 44 | 74 | |||
| Average age (y) | 79.6 | 79.8 | |||
| Stable fractures (31.A1) | 14 | 38 | |||
| Unstable fractures (31.A2) | 30 | 36 |
Method In all the patients we used the intramedullary hip nail PFH-Medin. The total length of this unreamed implant is 240 mm with the diameter of its proximal part 15 mm and the diameter of its distal part either 11 mm or 13 mm. Both lag screws have the same diameter of 7.9 mm and a thread length of 25 mm. Lag screws may be inserted at an angle of 130˚ or 135˚. Two holes are available for distal locking—dynamic and static. All the patients were operated upon by the authors of this study who have long-term experience with the IMHN in trochanteric fractures.
Indication Both displaced stable and unstable pertrochanteric fractures (AO/ASIF 31A1+A2) were included for operative treatment but pathological fractures and osteoarthritic hips were excluded.
Surgical technique Closed reduction of the fracture was performed on the fracture table to restore anatomical position of fragments. The intramedullary canal of the femur was opened through the apex of the greater trochanter and reamed for the proximal part of the nail only. After seating of the nail, two K-wires were inserted into the femoral head under image intensifier control in both views, serving as guide wires for insertion of two lag screws into the subchondral bone of the femoral head.The distal dynamic locking was indicated only in cases of a broad intramedullary canal, comminution of the lateral wall of the greater trochanter extending below the vastus lateralis ridge, a large posteromedial fragment extending distally below the lesser trochanter and in cases when the secondary fracture line extended to the femoral diaphysis.The final position of both the fragments and the implant was checked by image intensifier in the anteroposterior (AP) and lateral views. The same views were used for the first postoperative radiographs.
Postoperative care and follow-up Patients were mobilised as soon as possible. The patients were followed-up at six weeks, three, six and 12 months after surgery, including AP radiograph of the hip.
Evaluation In both groups of patients the following items were recorded.
Type of the fracture according to AO/ASIF classification
Operation time (starting from skin incision until wound suture)
Fluoroscopy time
Time to union
Backing out of lag screws from the lateral cortex of the femur caused by compression of main fragments
Anatomy of the proximal femur, length and rotation of the limb after healing
Intraoperative, early and late postoperative complications, if any
Functional score according to Broos [4] before fracture and one year postoperatively
In group I (with distal locking), the position of the screw in the dynamic locking hole was compared on AP postoperative radiograph and AP radiograph after healing
The fracture type, period of healing, position of fragments at the time of healing and axial compression of fragments in group II were evaluated by two independent observers not involved in the study. We evaluated statistical differences in the operation time, fluoroscopy time and functional score in both groups using the t-test. The study was approved by the ethical board of our hospital.
Results
Type of fracture Group I involving 44 patients with distal locking included 14 stable fractures of 31A1 type and 30 unstable fractures of 31A2 type. Group II of 74 patients without distal locking included 38 stable fractures of 31A1 type and 36 unstable fractures of 31A2 type (Table 1).
Operation time Average operation time in the whole cohort of 118 patients was 36.6 minutes (range, 13–100), in group I with distal locking 40.4 minutes (range, 18–100) while in group II without distal locking it was 34.4 (13–70), i.e. six minutes less. The statistical t-test showed p < 0.001, i.e. the difference in operation time was statistically very significant (Table 2).
Table 2.
Comparison of operative and fluoroscopy time in both groups of patients
| Number of fractures, N = 118 | Distal locking, n = 44 | Without distal locking, n = 74 | p-value |
|---|---|---|---|
| Operative time (min) | 40.4 | 34.4 | 0.000395 |
| Fluoroscopy time (s) | 53 | 43 | 0.0079 |
Fluoroscopy time Average fluoroscopy time in the whole cohort was 47 seconds (range, 15–180 seconds), in group I with distal locking 53 seconds (range, 20–180) and in group II without distal locking 43 seconds (range, 15–120). Also in this comparison the t-test showed statistically a significant difference of p < 0.01 (Table 2).
Time to union We recorded no delayed healing or non-union. All fractures healed without loss of reduction greater than 5 degrees within three months after surgery (Figs. 1 and 2).
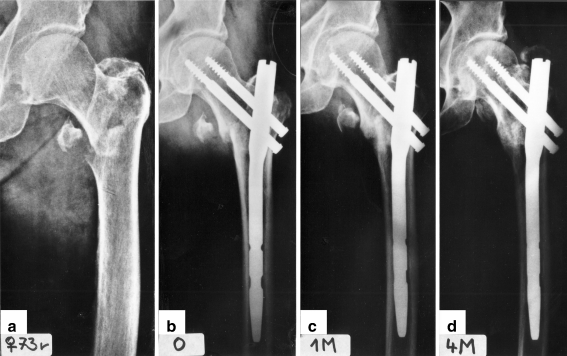
Fig. 1.
a Stable pertrochanteric fracture (31A1). b Fixation with PFH. c One month after surgery. d Fracture has healed four months after surgery
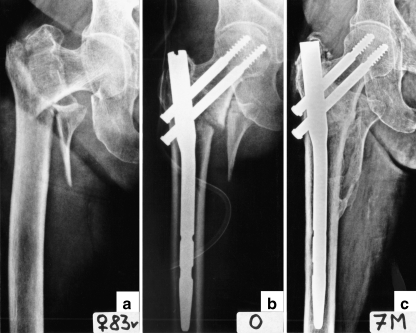
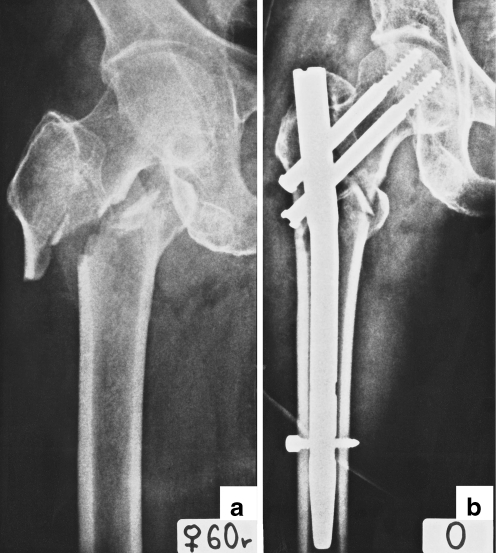
Fig. 2.
a Unstable pertrochanteric fracture (31A2), fixation with nail. c Complete fracture healing seven months after surgery
Compression of the two main fragments Compression of the two main fragments evaluated according to the backing out of lag screws from the lateral cortex of the diaphyseal fragment depended on the stability of the fracture (p = 0.0014). In group I with dynamic locking, the backing out of lag screws in stable fractures was on average 4.0 mm and in unstable fractures 9.6 mm. In group II without distal locking the backing out of lag screws in stable fractures was 3.5 mm and in unstable fractures 9.0 mm (Fig. 3). According to the statistical t-test, distal locking had no impact on compression on the fracture site (p = 0.7).
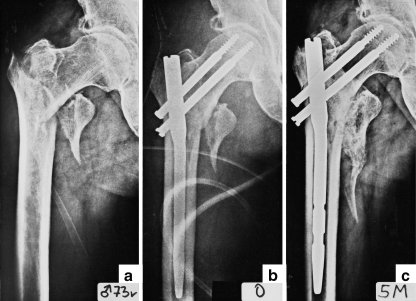
Fig. 3.
a Unstable pertrochanteric fracture. b Fixation with nail (31A2). c Fracture healing five month after surgery. Note the compression of fragments and the backing out of lag screws
Axial compression along the axis of the nail In group I comprised 44 patients with dynamic distal locking we recorded three cases (6.8 %) of axial compression along the nail axis that were manifested by a change in the position of the locking screw in the dynamic locking hole.In all three cases, the fracture was evaluated as unstable (31A2) and the axial compression was recorded within the first six weeks postoperatively. In two cases comminution of the lateral wall of the greater trochanter was already present prior to the surgery, and in the third case the lateral wall was fractured intraoperatively during nail insertion. In none of the three cases did axial compression have an impact on the course of healing and position of fragments and the limb shortening did not exceed 1 cm.
Anatomy of proximal femur, leg length and rotational alignment after healing In all patients compression of both the main fragments and medial displacement of the femoral shaft occurred (see above). This resulted in a greater or lesser shortening of the operated limb which, however, never exceeded 1 cm. We did not record varus rotation of the proximal fragment greater than 5° and malrotation of the operated limb of more than 10°.
Functional score according to Broos In both groups, evaluation of the functional score showed a decrease when comparing the score prior to fracture and 12 months postoperatively (Table 3). However, the type of distal locking had no significant impact on the change of the functional score and p-value was 0.92.
Table 3.
Broos functional score
| Evaluation | Distal locking | Without distal locking | p-value |
|---|---|---|---|
| Before fracture | 43.4 | 43.1 | 0.78 |
| 12 months after surgery | 34.8 | 34.6 | 0.92 |
Complications We did not encounter any cases of cut out of lag screws, non-union or infection. In total, we recorded only seven complications (5.9%), of these three occurred intraoperatively, three developed during the first three months postoperatively and one complication appeared one-year postoperatively.In two cases, hammering of the nail caused a diaphyseal split at the level of the nail tip. In the first case (nail without distal locking), both the diaphyseal fissure and the pertrochanteric fracture healed without reoperation in three months without any complications. In the second case (dynamically locked nail), the diaphyseal fissure was treated non-operatively at first but three weeks later the patient fell and sustained a displaced fracture of the femoral shaft just below the nail tip. Therefore internal fixation was performed using a locking plate. The pertrochanteric fracture healed in anatomical position after three months and the diaphyseal fracture four months after reoperation.In one case, the distal lag screw missed the nail but this had no impact on the position of fragments and healing of the fracture.In three patients of group I (with distal locking) we recorded temporary pain in the thigh during the first three months postoperatively that disappeared after the fracture had healed.In one case of a stable pertrochanteric fracture (31A1) without distal locking which healed three months postoperatively, the patient developed avascular necrosis of the femoral head 12 months after surgery. The situation was addressed by hardware removal and total hip arthroplasty.
Discussion
Since the introduction of the GN into clinical practice, the most frequently reported complications have been problems with distal locking [1, 3, 5, 6, 8, 12, 15, 19, 23]. Such a high frequency of these problems was not seen later in any other IMHN [7, 11, 13, 14, 16, 22]. Thigh pain and especially very frequent fractures in the region of the nail tip were even considered by some authors as contraindication of GN in pertrochanteric fractures [6, 18, 19, 25]. There were two reasons for this. GN was the first IMHN used globally and most authors used it to master the learning curve [1, 3, 5, 8–10, 17–20]. Another cause was the nail design. The distal part of the nail had to be pre-reamed, which caused thinning of the diaphyseal cortex at the level of the tip of the nail. The short distance between the two locking screws and the nail tip and the shape of the tip contributed to stress concentration in this area.
However, in most cases the problems with distal locking were caused by incorrect surgical technique. Incorrect incision of the fascia may force out the targeting device off the distal locking hole [15]. Lacroix et al. [17] pointed out the damage that may be caused to the lateral cortex by awl. Hesse et al. [12] saw the cause of fracture of the femur in repeated drilling for the distal locking, locking screw inserted outside the nail or excessive tightening of the distal locking screw.
The frequency and severity of these complications gave rise to a legitimate question about the necessity to use distal locking in the GN. Among the first authors to deal with this problem in a biomechanical study were Rosenblum et al. [20]. They stated that “insertion of distal interlocking screws did not change the pattern of proximal femoral strain” and therefore “distal interlocking screw may not be necessary for stable intertrochanteric fractures.” They recommended distal locking in “comminuted intertrochanteric-subtrochanteric fractures, reverse obliquity and high obliquity fractures, where rotational control of the distal fragment is more problematic and shortening is more likely to occur”.
Radford et al. [19] came to the conclusion that distal locking was performed only when indicated for longitudinal or rotational instability. Valverde et al. [25] used distal locking only in 24% of 224 patients treated with the GN for a trochanteric fracture and only for fractures susceptible to shortening or rotation. Bellabarba et al. [2] did not use distal locking in any of their 90 patients with a fracture of the proximal femur. In three patients they recorded thigh pain postoperatively, but did not relate it to the absence of distal locking. Shen [23] recommended distal locking of GN “only in highly unstable fractures or in broad medullary canal. In this case, one screw in the upper of the two distal locking holes is sufficient”. According to De Lucas et al. [6], locking of stable pertrochanteric fractures is not necessary “but, if needed, then only a proximal screw, in nail with two holes, should be used”. Utrilla et al. [24] used in their 104 trochanteric fractures treated with GN distal locking by one screw only if the rotational instability of the diaphyseal fragment was present. They concluded “that routine distal locking is unnecessary for trochanteric fractures. It should be used only where there is a subtrochanteric extension of the fractures”.
The distal locking should eliminate longitudinal or rotational instability and, in cases of a wide canal, also prevent movement of the tip of the nail in the canal. However, both longitudinal and rotational instability depends on the type of fracture. This fact is neglected by the above-mentioned authors. They generalise their recommendations concerning distal locking for all types of trochanteric fractures, although there are important anatomical differences between pertrochanteric (AO/ASIF 31A1+2) and intertrochanteric fractures (AO/ASIF 31A3) that have a significant impact on distal locking.
In the pertrochanteric fractures (31A1+A2), the main fracture line passes obliquely between the femoral neck and the trochanteric segment. The distal, diaphyseal fragment projects proximolaterally into the spike carrying the base of the greater trochanter including the vastus ridge. The lag screw(s) pass at the same time through the lateral cortex of the distal fragment (Fig. 4) and thus stabilise both fragments and prevent their mutual rotation and longitudinal compression along the nail.
Fig. 4.

Postmortem specimen of patient with pertrochanteric fracture treated with PFH-Medin. Both lag screws penetrated the lateral cortex of the distal (diaphyseal) fragment
In the (reverse) intertrochanteric fractures (AO/ASIF 31A3), the proximal fragment is formed by the femoral head and neck and the greater trochanter including its base with the vastus ridge. Thus, in intertrochanteric fractures the compression of both main fragments occurs along the femoral shaft axis, i.e. along the axis of the nail. With regard to anatomy of the proximal fragment the lag screw(s) pass almost through the lateral cortex of the proximal fragment (Fig. 5). Therefore without distal locking, most of these fractures are rotationally and longitudinally unstable.
Fig. 5.
a The intertrochanteric fractures (31A3). b Fixation with PFH; both lag screws penetrated the lateral cortex of proximal fragment
As to the cause of thigh pain in the three patients in group I, we consider instability of fracture, although it may be partially caused also by stress concentration around the locking screw. In group II we recorded no complication caused by absence of distal locking. Comparison of the two groups showed that absence of distal locking had no negative impact on complications nor on radiological and functional results. On the contrary it contributed to a statistically significant reduction of operation and fluoroscopy time.
Thus, our study has shown that distal locking of IMHN is unnecessary in most pertrochanteric fractures (AO/ASIF 31A1+2). Distal locking is indicated only in cases of comminution of the lateral wall of the greater trochanter, a secondary diaphyseal fracture line, a large posteromedial fragment extended distally below the level of the lesser trochanter and a broad intramedullary canal. In these cases, a mere placement of the nail in the diaphyseal fragment would be insufficient.
Footnotes
This article is original, it is not under consideration by another journal, and it has not been previously published.
Contributor Information
Jiří Skála-Rosenbaum, Phone: +420-2-67162431, FAX: +420-2-67313372, Email: skala@fnkv.cz.
Jan Bartoníček, Phone: +420-2-67162431, FAX: +420-2-67313372, Email: bartonicek.jan@seznam.cz.
References
- 1.Bartoníček J, Douša P, Krbec M. Short gamma nail for internal fixation of proximal femur fractures. Acta Chir Orthop Traum Cechoslov. 1998;65:74–83. [PubMed] [Google Scholar]
- 2.Bellabarba C, Herscovici D, Ricci WM. Percutaneous treatment of peritrochanteric fractures using the gamma nail. Clin Orthop Rel Res. 2000;375:30–42. doi: 10.1097/00003086-200006000-00005. [DOI] [PubMed] [Google Scholar]
- 3.Bridle SH, Patel AD, Calvert PT. Fixation of intertrochanteric fractures of the femur. A randomized prospective comparison of the gamma nail and the dynamic hip screw. J Bone Joint Surg [Br] 1991;73-B:330–334. doi: 10.1302/0301-620X.73B2.2005167. [DOI] [PubMed] [Google Scholar]
- 4.Broos, PLO, van Haaften, KIK, Stappaerts et al (1989) Hip fractures in the elderly. Mortality, functional results and social readaptation. Int Surg 74:191–194 [PubMed]
- 5.Calvert PT. The gamma nail—a significant advance or a passing fashion? J Bone Joint Surg [Br] 1992;74-B:329–331. doi: 10.1302/0301-620X.74B3.1587869. [DOI] [PubMed] [Google Scholar]
- 6.Lucas P, Seral B, Beano Á, et al. Fractures of the proximal femur. The gamma nail versus plate. Osteo Trauma Care. 2005;13:18–25. doi: 10.1055/s-2005-836371. [DOI] [Google Scholar]
- 7.Douša P, Bartoníček J, Jehlička D, et al. Proximal femoral nail (PFN Synthes) for internal fixation of trochanteric fractures. Acta Chir Orthop Traum Cechoslov. 2002;69:22–30. [PubMed] [Google Scholar]
- 8.Halder SC. The gamma nail for peritrochanteric fractures. J Bone Joint Surg [Br] 1992;74-B:340–344. doi: 10.1302/0301-620X.74B3.1587873. [DOI] [PubMed] [Google Scholar]
- 9.Hardy DC, Descamps PY, Krallis P, et al. Use of intramedullary hip-screw compared with a compression hip-screw with a plate for intertrochanteric femoral fractures. J Bone Joint Surg [Am] 1998;80-A:618–630. doi: 10.2106/00004623-199805000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Heinz T, Vécsei V. Komplikationen und Fehler bei der Anwendung des Gammanagels. Chirurg. 1994;65:943–952. [PubMed] [Google Scholar]
- 11.Herrera A, Domingo J, Martinez A. Results of osteosynthesis with the ITST nail in fractures of the trochanteric region of the femur. Int Orthop. 2008;32:767–772. doi: 10.1007/s00264-007-0411-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hesse B, Gächter A. Complications following the treatment of trochanteric fractures with the Gamma nail. Arch Ortho Trauma Surg. 2004;124:692–698. doi: 10.1007/s00402-004-0744-8. [DOI] [PubMed] [Google Scholar]
- 13.Hohendorff B, Meyer P, Menezes D, et al. Behandlungsergebnisse und Komplikationen nach PFN-Osteosynthese. Unfallchirurg. 2005;108:938–953. doi: 10.1007/s00113-005-0962-8. [DOI] [PubMed] [Google Scholar]
- 14.Gadegone WM, Salphale YS. Proximal femoral nail—an analysis of 100 cases of proximal femoral fractures with an average follow up of 1 year. Int Orthop. 2007;31:403–408. doi: 10.1007/s00264-006-0170-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Klanke J, Franke J, Westermann K. The titanium gamma nail as routine treatment of pertrochanteric femoral fractures. Osteo Trauma Care. 2005;13:26–33. doi: 10.1055/s-2005-836372. [DOI] [Google Scholar]
- 16.Košťál R, Douša P, Bartoníček J. PFH (Proximální femorální hřeb) - Another possibility for internal fixation of trochanteric fractures. Rozhl Chir. 2003;82:28–31. [PubMed] [Google Scholar]
- 17.Lacroix H, Arwert H, Snijders CJ, et al. Prevention of fracture at the distal locking site of the gamma nail. J Bone Joint Surg [Br] 1995;77-B:274–276. [PubMed] [Google Scholar]
- 18.Leung KS, So WS, Shen WY, et al. Gamma nails and dynamic hip screw for pertrochanteric fractures. J Bone Joint Surg [Br] 1992;74-B:345–351. doi: 10.1302/0301-620X.74B3.1587874. [DOI] [PubMed] [Google Scholar]
- 19.Radford JP, Needorf M, Webb JK. A prospective randomised comparison of the dynamic hip screw and the gamma locking nail. J Bone Joint Surg [Br] 1993;75-B:789–793. doi: 10.1302/0301-620X.75B5.8376441. [DOI] [PubMed] [Google Scholar]
- 20.Rosenblum SH, Zuckerman JD, Kummer FJ, et al. A mechanical evaluation of the gamma nail. J Bone Joint Surg [Br] 1992;74-B:352–357. doi: 10.1302/0301-620X.74B3.1587875. [DOI] [PubMed] [Google Scholar]
- 21.Saarenpää I, Heikkinen T, Ristiniemi J, et al. Functional comparison of the dynamic hip screw and the gamma locking nail in trochanteric hip fractures: a matched-pair study of 268 patients. Int Orthop. 2009;33:255–260. doi: 10.1007/s00264-007-0458-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schipper IB, Steyerberg EW, Castelein RM, et al. Treatment of unstable trochanteric fractures. Randomised comparison of the gamma nail and the proximal femoral nail. J Bone Joint Surg [Br] 2004;86-B:86–94. [PubMed] [Google Scholar]
- 23.Shen WY. Complications with the gamma nail and long gamma nail, and their prevention. Osteo Trauma Care. 2005;13:34–41. doi: 10.1055/s-2005-836301. [DOI] [Google Scholar]
- 24.Utrilla AL, Reig JS, Muňoz FM, et al. Trochanteric gamma nail and compression hip screw for trochanteric fractures. J Orthop Trauma. 2005;19:229–233. doi: 10.1097/01.bot.0000151819.95075.ad. [DOI] [PubMed] [Google Scholar]
- 25.Valverde JA, Alonso MG, Porro JG, et al. Use of the gamma nail in the treatment of fractures of the proximal femur. Clin Orthop Rel Res. 1998;350:56–61. [PubMed] [Google Scholar]