Abstract
We performed a retrospective study on 178 Scarf osteotomies with a mean follow-up of 44.9 months (range 15–83 months). Clinical rating was based on the forefoot score of the American Orthopaedic Foot and Ankle Society (AOFAS). Weight bearing X-rays were used to perform angular measurements and assess the first metatarsophalangeal joint (MTP 1). At follow-up the mean AOFAS score had improved significantly (p < 0.001), but only 55% of the feet showed a perfect realignment of the first ray. Patients with a hallux valgus angle exceeding 30° and pre-existing degenerative changes at the MTP 1 joint displayed inferior clinical results (p < 0.05). Nearly 20% of the patients suffered from pain at the MTP 1 joint. This was clearly attributed to an onset or worsening of distinct radiographic signs of arthritis (p < 0.05) resulting in painfully decreased joint motion. Comparing radiographic appearance three months postoperatively and at follow-up, we found that radiographic criteria (hallux valgus, first intermetatarsal angle, hallux valgus interphalangeus, MTP 1 joint congruency, arthritic lesions at MTP 1) worsened with time.
Introduction
Correction of hallux valgus deformities requires soft tissue procedures and a first ray osteotomy. Apart from accepted standards to realign the soft tissues at the first metatarsophalangeal joint there is ongoing discussion about the various metatarsal osteotomies. Multiplanar diaphyseal metatarsal osteotomies are considered to have some advantages over distal and proximal osteotomies, although modifications of distal osteotomies also allow three dimensional correction [13]. As the transversal plane of the bone cut runs almost parallel to the plantar surface of the foot, plantigrade weight bearing leads to compression and inherent stability at the site of osteotomy. This has been proven biomechanically [23]. Aiming the diaphyseal bone cut plantarwards allows adjustment of the plantar pressure in cases of transfer metatarsalgia. Finally, rotation of the metatarsal head can be performed to realign the distal metatarsal articular surface. As a result of these principal advantages Scarf osteotomy, which was first described by Burutaran in 1976 [4], has gained wide popularity.
Nevertheless, the diaphyseal osteotomy requires an extensive exposure of the entire metatarsal and even a great protagonist of the Scarf osteotomy states that the surgical technique could be technically demanding [3, 8]. Therefore, discussion has arisen as to whether the results of Scarf osteotomy are superior to technically more simple osteotomies at the distal and proximal metatarsal. Although some clinical follow-up studies have been published in the last decade, most of them refer to short-term or mid-term results and others subsumed patients requiring a Scarf osteotomy and additional osteotomies of the lesser metatarsals [2, 7, 12, 16]. To evaluate the long-term results of isolated Scarf osteotomies in patients with isolated hallux valgus deformity the authors decided to perform a multicentre study.
Materials and methods
One hundred and sixty-two patients (156 female, six male) with hallux valgus deformity treated between 1995 and 2001 were included in the study. Thirty-seven patients underwent bilateral surgery resulting in a total number of 199 feet. Complex forefoot malalignment requiring additional osteotomies at the lesser metatarsals, patients with previous forefoot surgery and patients with rheumatoid arthritis or neurological disorders were excluded from the study. The indications referred to a first intermetatarsal angle of less than 20 degrees with no restrictions regarding the hallux valgus angle. Minor radiological signs of arthritis at the first metatarsophalangeal (MT 1) joint were no contraindication as long as the patients were asymptomatic and range of motion was not reduced below 60 degrees. Mean age at the time of operation was 53.8 years (range 17–77 years). After a mean follow-up of 44.9 months (range 15–83 months), 149 patients (91.9%) (178 feet, 91.8%) attended a clinical and radiological follow-up. In the meantime, three patients had died, five moved away, and five refused to further participate in the study.
All feet were exclusively operated and followed-up by the three authors. The surgical technique mainly followed the instructions published by Barouk [3]. A straight incision was performed on the medial side of the first ray. To release the lateral soft tissues a transarticular approach was chosen in 65 feet (36.5%). In 113 feet (63.5%) the lateral release was carried out through a separate incision along the first web space. The distal starting point of the Z-shaped osteotomy was approximately 5 mm proximal to the cartilage surface. Leaving the plantar two thirds of the metatarsal undamaged, the bone cut pointed slightly plantarwards. The proximal end of the osteotomy was located 10 mm distal to the metatarso-cuneiform (MC) joint. To release the two bone fragments the osteotomy was completed by two short transverse cuts at both ends of the longitudinal osteotomy. These two parallel cuts were performed at a 60° angle to the longitudinal axis. After carefully releasing both fragments the plantar metatarsal portion was shifted laterally. In order to obtain correction of the distal metatarsal articular angle the proximal part of the plantar fragment was pivoted to the lateral side. Internal fixation was achieved with two cannulated screws (Herbert type). After the medial border of the bunion was trimmed, a moderate medial capsular reefing was followed by the skin closure. Then a bulky dressing was applied. Patients were asked to stay in bed for 24 hours with the operated foot elevated. Immediate weight bearing was allowed using a forefoot relief orthosis for four weeks. Patients were instructed to perform active and passive exercises of the MTP 1 joint and tape the great toe into a straight position. Four weeks postoperatively a check X-ray was performed. If sufficient healing of the osteotomy was revealed, patients were allowed to wear trainers.
In cases of concomitant hallux valgus interphalangeus deformity of more than 10 degrees, an Akin procedure of the proximal phalanx was additionally carried out in 37 feet (20.8%). To correct fixed hammertoe deformity, resection arthroplasty or arthrodesis (59 feet, 33.1%) was performed at the proximal interphalangeal joint. To address flexible hammer toe deformities a flexor-to-extensor-transfer was indicated in 12 feet (6.7%).
At the latest follow-up clinical evaluation was based on the AOFAS metatarsophalangeal-interphalangeal score [11]. Besides the clinical assessment of the first ray, we looked for signs of central metatarsalgia.
Standardised weight bearing radiographs allowed comparison of preoperative and postoperative findings: first intermetatarsal angle, hallux valgus angle, hallux valgus interphalangeus angle, distal metatarsal articular angle, joint congruency at the first metatarsophalangeal joint, length of the first metatarsal, metatarsal alignment, arthritic changes at the first metatarsophalangeal joint and the alignment of the first metatarso-cuneiform joint [1, 20]. These radiographic parameters were evaluated preoperatively, three months after surgery, and at follow-up.
Statistical assessment included a paired resp. unpaired t-test and a linear regression analysis. Differences in p values less than 0.05 were considered statistically significant.
Results
Clinical assessment
Pain (40 points) decreased from a mean value of 17.9 points preoperatively to 36.8 points postoperatively (p < 0.001) (Table 1).
Table 1.
Assessment of pain according to the American Orthopaedic Foot and Ankle Society (AOFAS) score
| Preoperative pain | Postoperative pain | ||||
|---|---|---|---|---|---|
| Severe | Moderate | Mild | None | ||
| Severe | 20 | 6 | 4 | 10 | 0 |
| Moderate | 139 | 6 | 16 | 0 | 117 |
| Mild | 19 | 0 | 2 | 4 | 13 |
Within the functional assessment (45 points) (Table 2), activity (mean preoperative value 5.4 points and 8.9 points postoperatively, p < 0.001) and footwear requirements (mean preoperative value 5.8 points / 8.6 points postoperatively, p < 0.05) improved significantly.
Table 2.
Assessment of function according to the American Orthopaedic Foot and Ankle Society (AOFAS) score
| Preoperative Activity limitation | Postoperative activity limitation | ||||
|---|---|---|---|---|---|
| Severe limitation | Limitation | No limitation (daily activities) | No limitation | ||
| Severe limitation | 16 | 0 | 6 | 10 | 0 |
| Limitation | 82 | 0 | 7 | 37 | 38 |
| No limitation (daily activities) | 69 | 0 | 0 | 33 | 36 |
| No limitations | 11 | 0 | 0 | 0 | 11 |
| Footwear | Fashionable shoes, no insert | Comfortable shoes, insert | Modified shoes, brace | ||
| Fashionable shoes, no insert | 81 | 75 | 6 | 0 | |
| Comfortable shoes, insert | 92 | 63 | 29 | 0 | |
| Modified shoes, brace | 5 | 0 | 5 | 0 | |
| ROM (MTP 1) | > 75 degrees | 30–74 degrees | < 30 degrees | ||
| > 75 degrees | 88 | 45 | 33 | 0 | |
| 30–74 degrees | 81 | 54 | 20 | 7 | |
| < 30 degrees | 9 | 0 | 5 | 4 | |
| ROM (IP 1) | No restriction | Severe restriction | |||
| No restriction | 167 | 132 | 35 | ||
| Severe restriction | 11 | 0 | 11 | ||
| MTP–IP stability | Stable | Unstable | |||
| Stable | 7 | 7 | 0 | ||
| Unstable | 171 | 107 | 64 | ||
| Callus at MTP-IP | No callus | Symptomatic callus | |||
| No callus | 43 | 38 | 5 | ||
| Symptomatic callus | 135 | 103 | 32 | ||
ROM range of motion, MTP metatarsophalangeal joint, IP interphalangeal joint
Although range of motion at the MTP 1 joint did not reveal significant changes (mean preoperative value 7.2 points and 8.4 points postoperatively; p > 0.05), 22% of the joints showed impaired function at follow-up. Re-evaluating the preoperative X-rays we found a significant correlation (p < 0.05) between signs of arthritic changes and restricted range of motion postoperatively.
Plantarflexion at the first interphalangeal (IP) joint decreased significantly (mean preoperative value 4.9 points and 3.5 points postoperatively; p < 0.05). At follow-up, 19.7% of the patients had impaired IP 1 joint function. We found no correlation to any radiographical findings, hallux valgus angle, hallux valgus interphalangeus angle, or ROM at the MTP 1 joint.
Although MTP 1 stability improved significantly (mean preoperative value 1.9 points and 4.9 points postoperatively; p > 0.01), 35.9% of joints were considered unstable at follow-up. Instability at MTP 1 could be correlated to a recurrent deformity (p < 0.05). Stability at IP 1 was not influenced by the metatarsal osteotomy. Callus was reduced significantly (mean preoperative value 1.3 points and 5.4 points postoperatively, p > 0.001).
Alignment of the great toe also improved significantly (mean preoperative value 1.4 points and 12.7 points postoperatively; p < 0.001) (Table 3). Of the treated feet, 24.2% showed a mild hallux valgus deformity (≤ 20 degrees) and 19.7% revealed a moderate recurrent malalignment (≥ 21 degrees). Hallux varus occurred in 1.6%.
Table 3.
Assessment of alignment according to the American Orthopaedic Foot and Ankle Society (AOFAS) score
| Preoperative alignment | Postoperative alignment | |||
|---|---|---|---|---|
| Good | Fair, no symptoms | Poor | ||
| Good | 0 | 0 | 0 | 0 |
| Fair, no symptoms | 22 | 19 | 7 | 0 |
| Poor | 156 | 101 | 55 | 0 |
Overall the AOFAS score improved significantly (p < 0.001) (Table 4). The mean preoperative value (45.8 points) increased to 89.4 points at follow-up (Fig. 1). Pain, function, and alignment displayed a significant improvement, whereas ROM at MTP 1 / IP 1, stability at MTP 1 and toe alignment revealed a significant (p < 0.05) worsening with time.
Table 4.
American Orthopaedic Foot and Ankle Society (AOFAS) forefoot score at preoperative assessment, three months after surgery and at the latest follow-up (44.9 months)
| Assessment | Preoperative | Three months | 44.9 months | p-values |
|---|---|---|---|---|
| Pain | 17.9 | 37.0 | 36.8 | p < 0.001 |
| Function | 5.4 | 9.2 | 8.9 | p < 0.001 |
| Shoe ware | 5.8 | 8.8 | 8.6 | p < 0.05 |
| ROM (MTP 1) | 7.2 | 9.1 | 8.4 | p > 0.05a |
| ROM (IP 1) | 4.9 | 4.8 | 3.5 | p < 0.05a |
| Stability (MTP 1) | 1.9 | 5.5 | 4.9 | p < 0.01a |
| Calluses | 1.3 | 3.2 | 5.4 | p < 0.001 |
| Alignment | 1.4 | 15.2 | 12.9 | p < 0.001a |
| Total | 45.8 | 92.8 | 89.4 | p < 0.01 |
ROM range of motion, MTP metatarsophalangeal joint, IP interphalangeal joint
a During the follow-up period ROM at MTP 1 / IP 1, stability at MTP 1, and toe alignment worsened significantly (p < 0.05)
Fig. 1.
Follow-up of a 62-year-old woman presenting with an excellent correction over more than five years. a Preoperative radiograph indicating the metatarsus varus and hallux valgus deformity (first intermetatarsal angle 20 degrees, hallux valgus angle 35 degrees, subluxation of the first metatarsophalangeal joint). b Three months after the operation (first intermetatarsal angle 9 degrees, hallux valgus angle 0 degrees, congruent first metatarsophalangeal joint). c Sixty-one months after the operation (first intermetatarsal angle 9 degrees, hallux valgus angle 0 degrees, congruent first metatarsophalangeal joint)
To evaluate the influence of patient’s age we categorised two groups: (A) ≤ 50 years and (B) >51 years. The mean preoperative / postoperative values of the AOFAS score displayed no significant differences in both groups (A: 44.6 / 91.3 points and B: 47.0 / 86.9 points).
Furthermore, we analysed whether the degree of hallux valgus (HV) deformity had influenced the clinical outcome. Therefore we categorised two groups of patients: (A) HV angle ≤ 30° (62 feet), (B) HV angle ≥ 31° (116 feet). For patients in groups A and B the mean AOFAS scores were 50.1 and 43.5 points preoperatively, respectively, and 94.8 / 86.7 points postoperatively. By linear regression analysis we found that the preoperative HV angle had a significant effect on the AOFAS score (p < 0.05).
Finally we examined the influence of the first intermetatarsal (IM) angle on the clinical outcome. Again, two groups were considered: (A) IM 1 angle ≤ 13° (61 feet), (B) IM 1 angle ≥ 14° (117 feet). According to the AOFAS scores, the patients in groups A and B displayed mean preoperative values of 49.9 and 52.4 points, respectively, and 90.8 and 87.7 points postoperatively. These results did not reach statistical significance.
Metatarsalgia
Preoperatively more than half of the patients (99 feet, 55.6%) had no symptoms or clinical signs for metatarsalgia. At follow-up, nine of these patients complained of central metatarsalgia.
Most patients suffering from metatarsalgia preoperatively (79 feet, 44.4%) were free of pain (60 feet) at follow-up. The remaining patients (19 feet) stated that the symptoms had not changed.
Radiological assessment
Hallux valgus (HV) angle measurements (Table 5) were based on the recommendations from the Ad Hoc Committee of the American Orthopaedic Foot & Ankle Society [6, 16].
Table 5.
Time dependent changes in angular measurements of hallux valgus angle (HV), first intermetatarsal angle (IM 1), and hallux valgus interphalangeus angle (HVI)
| Angular measurements | Preoperative | Three months | 44.9 months | p-value |
|---|---|---|---|---|
| HV angle | 39.0° (12°–76°) | 12.5° (−10°–24°) | 24.8 (−10°–39°) | p < 0.001* |
| IM1 angle | 13.8° (9°–21°) | 8.8°(1°–14°) | 10.7° (1°–17.4°) | p< 0.05* |
| HVI angle | 7.4° (0°–25°) | 8.8° (0°–28°) | 9.7° (6°–35°) | p < 0.05* |
| HVI angle (Scarf + Akin) | 15.8° (9°–36°) | 5.4° (−3°–9°) | 4.9° (−5°–8°) | p < 0.001 |
* During the follow-up period HV angle, IM 1 angle and HVI angle worsened significantly (p < 0.05)
The mean HV angle (39° preoperatively / 12.5° postoperatively) was significantly reduced (p < 0.001) after the operation. At the latest follow up we recorded a significant recurrence (mean HV angle 24.8°) (p < 0.05).
The first intermetatarsal (IM) angle was significantly reduced (mean preoperative value 13.8°; 7.8° postoperatively; p < 0.05) after Scarf osteotomy. At follow-up however we noticed a recurrent deformity (mean value 10.7°; p < 0.05).
Joint congruency of the first metatarsophalangeal (MTP) joint was calculated with the help of two lines referring to the base of the proximal phalanx and the estimated cartilage surface of the first metatarsal head. Preoperatively 133 feet (74.7%) presented with an incongruent first MTP joint, which was successfully realigned in 81 feet. The remaining 52 feet revealed a marked improvement, but postoperative MTP joint alignment was not ideal. At follow-up 29 of these feet (55.8%) presented with an impaired joint congruency (p < 0.05) with a recurrent hallux valgus deformity.
Forty-five feet (25.3%) with a congruent joint preoperatively remained unchanged in 41 feet. Four feet developed an incongruent MTP joint, which was associated with a recurrent hallux valgus deformity.
It became evident that joint congruency was not achieved in 31.5%. Correlating the joint congruency with the hallux valgus angle it was obvious that hallux valgus recurrence was correlated to a malaligned MTP joint (p < 0.05).
Hallux valgus interphalangeus (HVI) angle was measured regarding the axis of the proximal and the distal phalanx. One hundred forty-one feet (79.2%) with an isolated Scarf osteotomy presented with a mean preoperative HVI angle of 7.4°, which remained unchanged within the first three months. At the final radiographical assessment the HVI angle had increased significantly (mean value 9.7°; p < 0.05). These results could not be correlated to any radiological or clinical findings.
In 37 feet (20.8%) with an HVI angle exceeding 10 degrees we performed an additional Akin osteotomy (mean preoperative angle 15.8°; 4.9° postoperatively; p < 0.001). In these patients the HVI angle remained unchanged throughout the follow-up period.
Metatarsal alignment was calculated by the relationship of metatarsal length I / II: index plus: 1 > 2; index plus/minus: 1 = 2; index minus: 1 < 2 (Table 6). In 43.8% of all feet Scarf osteotomy had led to a shortening of the metatarsal, which altered the metatarsal alignment. Further analysis illustrated no correlation to metatarsalgia or function at the fist MTP joint.
Table 6.
Metatarsal alignment
| Postoperative | Preoperative | ||
|---|---|---|---|
| Index minus | Index plus / minus | Index plus | |
| 82 | 65 | 31 | |
| Index minus | 82 | 47 (72.3%) | 2 ( 6.4%) |
| Index plus / minus | 18 (27.7%) | 29 (93.6%) | |
Radiographic signs of arthritis (subchondral cysts, narrowing of the joint space and osteophytes) were evaluated. During the preoperative assessment 60 feet revealed early radiographic signs of arthritis. More than half of these patients (37 feet; 61.6%) showed a distinct worsening of the pre-existing degenerative joint lesions (p < 0.05). In 118 feet the MTP 1 joint was assessed as normal. At follow-up 13 feet (11%) had developed distinct signs of arthritis.
We performed a linear regression analysis to evaluate the influence of pre-existing radiographic signs of arthritis at MTP 1 on the clinical outcome. In patients (118 feet) with a regular radiographic appearance of the MTP 1 joint the mean AOFAS score was 48.1 points preoperatively and 94.0 points at follow-up. The patients (60 feet) with pre-existing radiographic signs of MTP 1 joint arthritis displayed significantly (p < 0.05) worse clinical results (mean values: 42.7 points preoperatively, 83.3 points postoperatively).
Complications
Within the first six weeks after surgery we observed five delayed wound healings (2.8%) and five fractures (2.8%) of the first metatarsal. Three fractures occurred at the proximal end of the osteotomy; they healed uneventfully with a large callus formation, but some loss of correction. The remaining two fractures were located distally and obviously associated with a marked troughing (Fig. 2). These two patients underwent revision (hardware removal, internal fixation). Screw malposition and hardware overlength (3 feet, 1.7%) led to early hardware removal. This complication rate corresponds to that in the literature [18]. We observed no pseudarthrosis, algodystrophy, osteonecrosis or deep venous thrombosis.
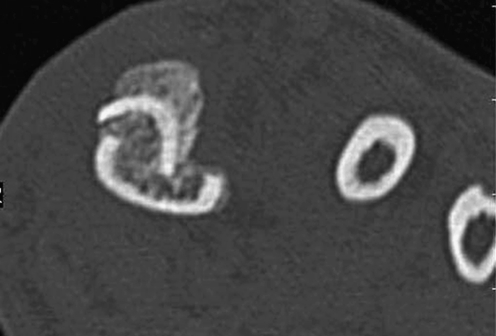
Fig. 2.
CT scan of the distal (transversal plane) metatarsal clearly illustrating the troughing effect
At the final follow-up, 12 patients (6.7%) had undergone a reoperation. Due to symptomatic arthritic changes of the first metatarsophalangeal joint, MTP 1 arthrodesis was performed in three patients. The remaining nine patients presenting with recurrent hallux valgus deformity required another metatarsal osteotomy (two feet) or an arthrodesis of the first MC joint (seven feet).
Discussion
Referring to the AOFAS forefoot score, our results of the Scarf osteotomy were comparable to other studies [2, 7, 12, 16]. As reported by other authors, perioperative complication rate was low (4.5%) [12, 18].
The mean correction of hallux valgus angle (20.2°) and first intermetatarsal angle (4.1°) also corresponded to those in the literature [2, 7, 12, 16].
The most unexpected result of this study was that the radiological outcome of isolated Scarf osteotomies had worsened with time (Figs. 3a–c and 4a–c). Although a time-dependent loss of correction was often estimated for first metatarsal osteotomies, it had not been stated clearly for the Scarf osteotomy. Due to the design of our study we were able to elucidate some aspects that were critical for the outcome of the Scarf osteotomy.
Fig. 3.
Follow-up of a 57-year-old woman presenting with a recurrent deformity after 2.4 years. a Preoperative radiograph indicating the metatarsus varus and hallux valgus deformity (first intermetatarsal angle 19 degrees, hallux valgus angle 35 degrees, subluxation of the first metatarsophalangeal joint). b Three months after the operation (first intermetatarsal angle 7 degrees, hallux valgus angle 20 degrees, congruent first metatarsophalangeal joint). c Twenty-nine months after the operation (first intermetatarsal angle 13 degrees, hallux valgus angle 0 degrees, congruent first metatarsophalangeal joint)
Fig. 4.
Follow-up of a 71-year-old woman presenting with a recurrent deformity after 4.9 years. a Preoperative radiograph indicating the metatarsus varus and hallux valgus deformity (first intermetatarsal angle 16 degrees, hallux valgus angle 38 degrees, subluxation of the first metatarsophalangeal joint). b Three months after the operation (first intermetatarsal angle 8 degrees, hallux valgus angle 5 degrees, congruent first metatarsophalangeal joint). c Fifty-nine months after the operation (first intermetatarsal angle 12 degrees, hallux valgus angle 20 degrees, incongruent first metatarsophalangeal joint)
Compared to the results we evaluated three months after surgery, we found that some radiographical findings (hallux valgus angle, hallux valgus interphalangeus angle, first intermetatarsal angle, MTP joint congruency) had worsened after a mean follow-up period of 44.9 months. Systematically reviewing these patients, we realised that the preoperative degree of HV deformity had a significant influence on the final clinical outcome. Patients with a HV angle exceeding 30 degrees preoperatively presented with worse results compared to patients with a HV angle less than 30 degrees. This correlation had only been mentioned once in the literature [12]. On the other hand the first IM angle did obviously not affect the final outcome.
Further assessment showed that joint congruency was also crucial for the outcome. Retrospectively we realised that most of those feet, which did not display a perfect joint congruency after three months, had developed a recurrent hallux valgus deformity at follow-up. Only 55% of the great toes were assessed as perfectly aligned. Discussing these results leads back to the surgical technique. Pivoting the first metatarsal head is required to correct the distal metatarsal articular angle and obtain a congruent joint. Due to the Z-shaped design of the osteotomy, rotating the distal fragment is technically demanding and requires shortening of the first metatarsal by removing bone wedges from the two transverse cuts. However this procedure will inevitably reduce the correction of the IM 1 angle, which is counter to the goals of treatment.
On the other hand the lateral release, which is essential in severe hallux valgus deformity with an incongruent joint, was probably not done adequately via the intraarticular approach. The inherent limitations of the transarticular approach have also been mentioned by other authors [21].
As a consequence we recommend limiting the indication for a classic Scarf osteotomy to patients with a normal distal metatarsal articular angle. In patients with a distinct lateral tilt of the metatarsal cartilage surface, alternative osteotomies (e.g. Chevron-type cut) should be taken into consideration to facilitate rotation of the distal metatarsal fragment [13].
Scarf osteotomy has been demonstrated to effectively restore a normal plantar pressure distribution [2]. In our patients metatarsalgia had improved in more than 70% of the affected feet. Nevertheless, 5% of patients complained of the onset of metatarsalgia after the operation. Critically reviewing these patients we considered elevation of the first metatarsal to be responsible for the metatarsalgia. Troughing of the two diaphyseal fragments has often been suggested to be critical in Scarf osteotomy [5]. On the other hand this is a well known problem even in distal metatarsal osteotomies [15]. In two patients suffering from a distal fracture we were able to clearly illustrate the troughing effect on CT scans (Fig. 1). While a huge amount of troughing (35%) was reported in a small series of patients [5], this complication was rare in our series as in other published series [18].
In 19% of our patients the pain level did not change or became worse after the operation. Retrospectively, 96% of these feet displayed a decreased range of motion at the first MTP joint, frequently corresponding to severe or moderate signs of arthritis on X-rays preoperatively. As mean reduction of metatarsal length (3.2 mm) did not differ from other studies [12] a decreased joint pressure could be expected even in these patients. However, 11% of our patients developed arthritic changes at the MTP joint postoperatively and more than 60% of those feet with pre-existing radiological signs of arthritis demonstrated a distinct worsening of degenerative changes. Since comparable results have been known even from open-wedge osteotomies of the cuneiform, the development of arthritis does not seem to be specific to metatarsal osteotomies [10].
The range of motion at the MTP 1 joint is considered to be a very important variable in assessing the postoperative outcome [17]. Nevertheless, we observed an impairment of joint function after Scarf osteotomy, which has also been mentioned by other authors [7, 14]. In conclusion, the metatarsal shortening alone is not sufficient to prevent arthritic changes at MTP 1 and to alleviate pain in patients with pre-existing arthritic changes at the first MTP joint. We therefore recommend that the Scarf osteotomy should be avoided in patients with pre-existing clinical and radiological signs of arthritis. Further shortening of the first metatarsal in combination with a phalangeal osteotomy will probably lead to a more successful outcome.
Range of motion at the MTP 1 joint worsened in more than 20% of our patients. This functional impairment after Scarf osteotomy has also been mentioned by other authors [7, 9]. However, the decreased range of motion does not seem typical of diaphyseal osteotomies, because this phenomenon has also been described for distal osteotomies [13, 14, 19].
From our clinical experience we did not anticipate that the isolated Scarf osteotomy had an influence on function and alignment of the first interphalangeal (IP) joint. In 14% of the feet presenting primarily with a normal range of motion at the first IP joint we noticed a significant reduction in joint function. These results did not reveal any correlation to the alignment of the first ray, the function at the MTP 1 joint or radiographic signs of arthritis at both joint levels. The radiographically assessed hallux valgus interphalangeus (HVI) angle, which remained unaffected within the first three months, developed a significant increase at the latest follow-up. The impaired joint function at the IP level may be attributed to the altered course of the extrinsic tendons attached at the base of the distal phalanx.
Critically assessing the results of our study we found various problems that were identified after thoroughly evaluating the clinical and radiological results. It was not surprising that the AOFAS scale did not reflect the outcome of hallux valgus surgery properly [22]. Radiological parameters should always be assessed to encompass all aspects.
In advising to the classical Scarf osteotomy we suggest a meticulous selection of patients.
Patients with obvious signs of arthritis do not respond well to the classical type of Scarf osteotomy with limited shortening of the metatarsal. Additional shortening osteotomy of the proximal phalanx or further shortening of the first metatarsal should be considered.
Subsequent enlargement of the HVI angle, which may result in an impingement of the second toe and impairs cosmetic appearance, should be routinely addressed with a phalangeal osteotomy.
As joint congruency has been evaluated to be crucial for the great toe alignment, the classical Scarf osteotomy should not be recommended in patients with an increased lateral tilt of the metatarsal articular surface. Alternate osteotomies, e.g. Chevron type osteotomy, are thought to be superior.
Acknowledgments
Conflict of interest The authors declare that they have no conflict of interest.
Contributor Information
Renée A. Fuhrmann, Phone: +49-36691-81020, FAX: +49-36691-81013, Email: RAEFuhrmann@aol.com
Hans Zollinger-Kies, Email: h.zollinger-kies@access.uzh.ch.
Hans-Peter Kundert, Email: hpkundert4foot@bluewin.ch.
References
- 1.Allen DM, Nunley JA. Measurement of the first/second intermetatarsal angle following proximal oblique metatarsal osteotomy. Foot Ankle Int. 2001;23:64–67. doi: 10.1177/107110070202300113. [DOI] [PubMed] [Google Scholar]
- 2.Aminian A, Kelikian A, Moen T. Scarf osteotomy for hallux valgus deformity: an intermediate follow up of clinical and radiological outcomes. Foot Ankle Int. 2006;27:883–886. doi: 10.1177/107110070602701103. [DOI] [PubMed] [Google Scholar]
- 3.Barouk LS. Scarf osteotomy for hallux valgus correction. Local anatomy, surgical technique, and combination with other forefoot procedures. Foot Ankle Clinics. 2000;5:525–558. [PubMed] [Google Scholar]
- 4.Burutaran JM. Hallux valgus y cortedad anatomica del primer metatarsano (correction quingica) Actual Med Chir Pied. 1976;13:261–266. [Google Scholar]
- 5.Coetzee JC. Scarf osteotomy for hallux valgus repair: the dark side. Foot Ankle Int. 2003;24:29–33. doi: 10.1177/107110070302400104. [DOI] [PubMed] [Google Scholar]
- 6.Coughlin MJ, Saltzman CL, Nunley JA. Angular measurements in the evaluation of hallux valgus deformities: a report on the Ad Hoc Committee of the American Orthopaedic Foot & Ankle Society on angular measurements. Foot Ankle Int. 2002;23:68–74. doi: 10.1177/107110070202300114. [DOI] [PubMed] [Google Scholar]
- 7.Crevoisier X, Mouhsine E, Ortolano V, Udin B, Dutoit M. The Scarf osteotomy for the treatment of hallux valgus deformity: a review of 84 cases. Foot Ankle Int. 2001;22:970–976. doi: 10.1177/107110070102201208. [DOI] [PubMed] [Google Scholar]
- 8.Dereymaeker G. Scarf osteotomy for correction of hallux valgus. Surgical technique and results as compared to distal chevron osteotomy. Foot Ankle Clin. 2000;5:513–524. [PubMed] [Google Scholar]
- 9.Jarde O, Trinquier-Lautard JL, Gabrion A, Ruzik JC, Vives P. Hallux valgus treated by first metatarsal scarf osteotomy. A series of 50 cases with a minimum follow up of 2 years. Clin Orthop Reparatrice App Mot. 1999;85:374–380. [PubMed] [Google Scholar]
- 10.Jawish R, Assoum H, Saliba E. Opening wedge osteotomy of the first cuneiform for the treatment of hallux valgus. Int Orthop. 2009 doi: 10.1007/s00264-009-0825-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kitaoka HB, Alexander IJ, Adelaar RS, Nunley J, Myerson M, Sanders M. Clinical rating system for the ankle-hindfoot, midfoot, hallux and lesser toes. Foot Ankle Int. 1984;15:349–353. doi: 10.1177/107110079401500701. [DOI] [PubMed] [Google Scholar]
- 12.Kristen KH, Berger C, Stelzig S, Thalhammer E, Posch M, Engel A. The Scarf osteotomy for the correction of hallux valgus deformities. Foot Ankle Int. 2002;23:221–229. doi: 10.1177/107110070202300306. [DOI] [PubMed] [Google Scholar]
- 13.Lucijanic I, Bicanic G, Sonicki Z, Mirkovic M, Pecina M. Treatment of hallux valgus with three-dimensional modification of Mitchell’s osteotomy. Technique and results. J Am Podiatr Med Assoc. 2009;99:162–172. doi: 10.7547/0980162. [DOI] [PubMed] [Google Scholar]
- 14.Magnan B, Bortolazzi R, Samaila E, Pezzè L, Rossi N, Bartolozzi P. Percutaneous distal metatarsal osteotomy for correction of hallux valgus. J Bone Joint Surg [Am] 2006;88:135–148. doi: 10.2106/JBJS.E.00897. [DOI] [PubMed] [Google Scholar]
- 15.Nikolaou VS, Korres D, Xypnitos F, Lazarettos J, Lallos S, Sapkas G, Efstathopoulos N. Fixation of Mitchell’s osteotomy with bioabsorbable pins for treatment of hallux valgus deformity. Int Orthop. 2009;33:701–706. doi: 10.1007/s00264-008-0664-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Perugia D, Basile A, Gensini A, Stopponi N, Simeonibus AUM. The Scarf osteotomy for severe hallux valgus. Int Orthop. 2003;27:103–106. doi: 10.1007/s00264-002-0413-x. [DOI] [PubMed] [Google Scholar]
- 17.Schneider W, Knahr K. Surgery for hallux valgus. The expectations of patients and surgeons. Int Orthop. 2001;25:382–385. doi: 10.1007/s002640100289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smith AM, Alwan T, Davies MS. Perioperative complications of the Scarf osteotomy. Foot Ankle Int. 2003;24:222–227. doi: 10.1177/107110070302400304. [DOI] [PubMed] [Google Scholar]
- 19.Schneider W, Knahr K. Keller procedure and Chevron osteotomy in hallux valgus: five-year results of different surgical philosophies in comparable collectives. Foot Ankle Int. 2002;23:321–329. doi: 10.1177/107110070202300406. [DOI] [PubMed] [Google Scholar]
- 20.Schneider W, Csepan R, Knahr K. Reproducibility of the radiographic metatarsophalangeal angle in hallux valgus surgery. J Bone Joint Surg [Am] 2003;85:494–499. doi: 10.2106/00004623-200303000-00015. [DOI] [PubMed] [Google Scholar]
- 21.Stamatis ED, Huber MH, Myerson MS. Transarticular distal soft-tissue release with an arthroscopic blade for hallux valgus correction. Foot Ankle Int. 2004;25:13–18. doi: 10.1177/107110070402500104. [DOI] [PubMed] [Google Scholar]
- 22.Thordarson D, Ebramzadeh E, Moorthy M, Lee J, Rudicel S. Correlation of hallux valgus surgical outcome with AOFAS forefoot score and radiological parameters. Foot Ankle Int. 2005;26:122–127. doi: 10.1177/107110070502600202. [DOI] [PubMed] [Google Scholar]
- 23.Trnka HJ, Parks BG, Ivanic G, Chu IT, Easley ME, Schon LC, Myerson MS. Six first metatarsal shaft osteotomies: mechanical and immobilization comparisons. Clin Orthop Rel Res. 2000;381:256–265. doi: 10.1097/00003086-200012000-00030. [DOI] [PubMed] [Google Scholar]