Abstract
In recent years, the locked plating system has gained favour in the treatment of certain fractures in adults; however, there is not much information regarding its use in children. We think there could be some advantages and applications such as: an alternative to external fixation, the bridge plating technique, unicortical screws, removal of hardware, metadiaphyseal fractures, periarticular fractures, poor quality bone, and allograft fixation. However, there are some disadvantages to keep in mind and the final decision for using it should be based on the osteosynthesis method principle the surgeon would like to apply. In this review article we discuss the up-to-date possible clinical applications and issues of this system.
Introduction
Musculoskeletal trauma, although rarely fatal, accounts for 10–25% of all childhood injuries [1]. The chance of a child sustaining a fracture during childhood is 42% in boys and 27% in girls. The most common sites of fracture are the distal forearm and hand, which account for 50% of paediatric fractures. Overall, the radius is the most commonly fractured long bone [2], followed by the humerus. In the lower extremity, the tibia is more commonly affected than the femur. The fracture rate increases as children grow, with the incidence peaking in early adolescence [3].
The principles of fracture treatment are the same for all ages, with anatomical alignment the primary concern. The fracture should not be malaligned or malrotated. Although some angulation is acceptable, it is best to keep the amount of angulation as small as possible by routine fracture treatment methods, whatever the patient’s age [4]. There are several methods that can be used; in most cases, closed reduction and cast immobilisation restores normal function to a paediatric extremity. Other widely accepted treatment options are the use of smooth pins, flexible and rigid intramedullary nails, and compressive plating [5]. However, one must know when to intervene and when to allow nature to take its course [6].
In recent years, the locked plating system has gained favour in the treatment of certain fractures in adults; however, there is not much information regarding its use in children. In this review article we discuss the up-to-date possible clinical applications and issues of this system.
Characteristics of the immature skeleton
There are some musculoskeletal differences in biomechanics, anatomy, and physiology between children and adults.
Biomechanical features
The bones of children are less mineralised and have more vascular channels than adult bones. This results in a lower modulus of elasticity, which allows for greater energy absorption before failure. Paediatric bone also has the plastic deformation capacity, in which the bone does not return to its original shape after sustaining a load.
The diaphyseal cortex is more rigid than the metaphyseal region. Comminuted fractures are less common in children than in adults, because paediatric bone can dissipate energy before failure and porosity inhibits fracture line propagation. The paediatric bone resists torsional load less than the adult bone, because of its smaller diameter.
Mechanical properties of the epiphysis vary with age. Increasing ossification in the epiphysis occurs with age and imparts more rigidity. This increased rigidity partially explains why epiphyseal fractures and displacements are more commonly seen in older children [7].
Anatomical features
The presence of growth plates and the thick periosteum are major anatomical features that distinguish childrens’ bones from adults. Growth plate injuries can lead to growth disturbances; fixation devices must avoid the physis to reduce the risk of iatrogenic physeal injury and subsequent growth arrest.
The periosteum in children is much thicker, more active, and more easily stripped from the bone than in adults. It helps in the maintenance of reduction and contributes to rapid fracture healing. The periosteum is vital for fracture healing, and should be preserved as much as possible [8].
Physiological features
Fractures in children heal more rapidly than in adults [2]. This is explained in part by the osteogenic potential of the periosteum and the magnitude of the vascular response in children.
Remodelling of angulated fractures in children is a well-recognised phenomenon. The majority of remodelling occurs by reorientation of the growth plates. Asymmetrical and longitudinal growth of the physis contribute to it [9]. Remodelling capacity depends on the number of years of growth remaining ahead, the proximity of the fracture to a rapidly growing physis, the magnitude of angular deformity, and the plane of angulation relative to adjacent joints.
Another physiological response to bone healing in children is the potential for growth stimulation after fracture. Transverse sectioning of the periosteum produces overgrowth; possible mechanisms for this are an increased blood flow to the growth plate and release of periosteal tension after fracture [10].
Fracture healing
Two types of fracture healing are classically described: primary and secondary. The former results from rigid stabilisation (i.e. plate immobilisation) and involves a direct attempt by the cortex to bridge the fracture gap through direct Haversian remodelling by intramembranous ossification. Secondary healing results from treatment of fractures with less rigid methods (i.e. fracture bracing). Motion at the fracture site, the presence of a fracture gap, and an intact tissue envelope encourage the formation of abundant callus, which undergoes endochondral ossification.
The majority of paediatric fractures unite by secondary fracture healing. Fracture results in cellular injury and haematoma formation, which stimulate inflammation and the proliferation of stem cells; this process is more active within the paediatric bone explained by its higher vascularity. Stem cells produce bone morphogenetic proteins, which lead to cellular differentiation. The highly vascular periosteum surround the haematoma which contributes to the production of new bone around the fracture site as well as the formation of bone through membranous ossification [8]. During the second phase of consolidation, angiogenesis takes place, and is followed by formation of soft callus [11]. Low oxygen tension and fracture motion promote cartilage formation as the initial stage of endochondral ossification. This cartilage is subsequently removed and replaced by hard callus with woven bone. Finally, the ossification phase allows a more prolonged phase for fracture remodelling.
Absolute rigid fixation is rarely necessary; such rigidity may decrease the prolific subperiosteal callus formation which contributes to fracture stability in children. The more flexible the frame, the better the stress transfers across the fracture site to facilitate healing and, more importantly, remodelling. The most important target of fixation devices in children is achieving relative stability and secondary healing [12].
General principles for use of the locked plating system
The locking plate system provides relative stability for fracture fixation as seen with casting, intramedullary nailing or external fixation. The screws are designed to lock into the plate, eliminating screw toggle and creating a fixed-angle, single-beam construction.
Biomechanically, the locked plating system is designed to convert shear forces experienced at the implant with the application of load into compressive forces at the screw–bone interface [13]. Biomechanical testing of locking plates has shown favourable outcomes compared with nonlocking plates. Locked plating offers greater fixation stability in axial loading, both before and after cyclic loading compared to nonlocked plating [14].
The locking plate system preserves local blood supply and periosteum, because there is no frictional force between the plate and bone. Moreover, a locked plating system can be placed through minimally invasive incisions with less periosteal and vascular damage.
Locked plating system in children—clinical application
The first locking plates were introduced about two decades ago for use in spinal and maxillofacial surgery [15–18]. In the late 1980s and into the 1990s, experimentation with various types of internal fixation devices led to the development of locking plates for fracture care [19–21]. They have been available in North America for general orthopaedic applications only in the last six or seven years [15, 22].
Although little has been reported in the literature on the use of this system in children.
One application is as an alternative to external fixation. External fixation is a good option for the treatment of open fractures [5, 23], fractures with compartment syndrome, long-bone fractures with significant comminution [23, 24] or bone loss [5] as well as for limb lengthening and bone transport [25, 26]. However, concerns about delayed healing, pin track infections, joint stiffness and re-fracture have blunted the broad acceptance of these devices. In that sense, locked plating may be an alternative because it offers some advantages such as minimising pin track infections and re-fracture after removal [5, 27] as well as greater biomechanical stability [24]. The large incisions required for standard plating increase the infection rate and may contribute to overgrowth at the time of plate application and removal [5, 28, 29]. With regards to limb lengthening it permits early removal of external fixation [25] or it could be used as an alternative method for doing so [26]. It is mainly indicated for children with open physeal plates, narrow canal diameter, or short length of the bone [25, 26].
Some clinical applications of this concept can be seen in articles such as the one published by Yusof et al. [24] who described a series of 16 children including eight open tibial fractures; a percutaneous locked plating technique was used as an alternative to external fixation. The mean age was 10 years and 9 months and other indications for this technique in the entire group were presence of associated injuries, compartment syndrome and nonunions. All patients achieved excellent or satisfactory clinical outcomes (Table 1).
Table 1.
Summary of findings from the study articles retrieved and reviewed using locked plating as an alternative to external fixation
| Author | Year | Number of patients | Methods | Use | Characteristics | Results | Conclusions |
|---|---|---|---|---|---|---|---|
| Yusof et al. [24] | 2009 | 16 (8 open fx)a | Percutaneous plating technique | Open fracture (tibiae) | Age: 10 years, 9 months (range 6–16 years) Follow-up: 1 year, 8 months Other indications: associated injuries, compartment syndrome, nonunions |
Mean time to union: 13 weeks (range 8–24) No major complications No leg discrepancy >10 mm Excellent or satisfactory clinical outcome |
This is a safe alternative treatment for paediatric tibial fractures that are difficult to manage using other methods |
| Oh et al. [25] | 2008 | 8 (4 lengthening, 4 bone transport) | Early removal of Ilizarov EF. Percutaneous plating after achieving the target length | Limb lengthening and bone transport (3 femurs, 5 tibiae) | Age: 11.62 years Mean distraction: 5.47 cm Follow-up: 28 months (range 18–62) |
Distraction callus healed on maintaining its length or correcting original alignment One superficial pintrack infection No deep infection or implant failure |
May be a successful method that permits early removal of fixator with fewer complications Useful alternative when nailing is difficult |
| Iobst et al. [26] | 2007 | 6 | Lengthening with EF assisted by percutaneous inserted locking plate | Limb lengthening | Mean age: 7.6 years Follow-up: 10 months Mean distraction: 3.52 cm |
All achieved solid union All achieved unassisted weightbearing Excellent range of motion Few complications |
Alternative method to lengthening over an IM |
a These open fractures are included in a larger study group
Fx fracture, EF external fixator
Oh et al. [25] used this system for the early removal of the external fixation for limb lengthening and bone transport. Eight patients with a mean age of 11.62 years were included and percutaneous plating was used after achieving the target length. They reported no major complications, and a decrease in those associated with a prolonged use of an external fixation; this is also an alternative method when nailing is difficult (Table 1).
Iobst et al. [26] reported a series of six patients in whom a lower limb lengthening with external fixation followed by a percutaneously inserted locking plate was performed. The mean age was 7.6 years and the mean distraction was 3.52 cm. All patients achieved solid union with excellent range of motion and few complications (Table 1). Locking plates prevent loss of fixation and protect against bending of the regenerate bone after frame removal.
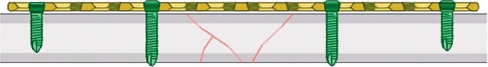
There has been a trend toward the use of more minimally invasive techniques [5]. More biological plating techniques have been developed: reductions are indirect, implants are introduced through small incisions and placed beneath the muscles but above the preserved periosteum with maintenance of vascularity to small bone fragments. This is what we call the bridge plating technique (Fig. 1) and it is based on bypassing central comminuted fragments without damaging remaining soft tissue attachments [23]. Bridge plate fixation allows for maximum biological healing while at the same time creating an internal splint and stable fixation [23, 30]. A locking plate may be a good alternative for bridging severely comminuted fractures as we can see in the following articles (Table 2).
Fig. 1.
Biomechanics of locked internal fixator (LIF): bridging technique—internal fixator principle
Table 2.
Summary of findings from the study articles retrieved and reviewed for the bridge plating technique
| Author | Year | Number of patients | Methods | Use | Characteristics | Results | Conclusions |
|---|---|---|---|---|---|---|---|
| Oh et al. [31] | 2007 | 13 fx (6 comminuted) LCP® plates | Minimally invasive percutaneous bridge plating | Complex femoral fx | Mean age: 9 years Associated injuries in 9 px Follow-up: 22 months |
All fx united without bone graft Time to union: 11 weeks No rx angulation > 10° or length discrepancy >5 mm No major complications Excellent final outcome |
The technique provided adequate stability for early functional treatment and predictable healing with maintenance of leg length and alignment |
| Sink et al. [32] | 2006 | 27 fx (6 w/locking plates) | Submuscular bridge plating | Unstable femoral fx | Mean age: 9 years Follow-up: 11 months |
There were no intraoperative or postoperative complications No hardware failure No loss of reduction Time to union: 11.7 weeks (stable bridging callus) |
Submuscular plating is a reasonable option for operative stabilization of comminuted and unstable pediatric femoral fractures |
| Kanlic et al. [23] | 2004 | 51 fx (55% had unstable patterns) (1 with locking plate) | Submuscular bridge plating | Unstable femoral fx | Mean age: 10 years 67% high energy injuries Follow-up: 14.2 months |
All fx united with excellent clinical results Complications: one peri-plate fx, one refracture Four px with leg length discrepancy |
This technique offers the advantage of adequate stability for early functional treatment and predictable healing |
fx fractures, px patients, rx radiological
Oh et al. [31] described a series of 13 femoral fractures including six comminuted fractures; a bridge plating technique was performed and LCP® plates were used. The mean age was nine years. All fractures united without bone graft; no major complications were reported and there was an excellent final outcome.
Sink et al. [32] included 27 unstable femoral fractures in which locking plates were used in six. The mean age of all the series was nine years. There were no intraoperative or postoperative complications. There was no hardware failure and no loss of reduction.
Kanlic et al. [23] reported a series of 51 unstable femoral fractures, a submuscular bridge plating technique was performed and only in one case a locking plate was used. The mean age was ten years. All fractures united with excellent clinical results; there were some minor complications (Table 2).
Clinical evidence shows that the bridging technique using locking plates may provide good functional and radiological outcomes.
One of the biomechanical advantages of locking plates over conventional ones is that using unicortical screws in good quality bone still maintains an adequate stable construction. This may provide some advantages to the surgeon; for example, the need to measure for screw lengths is eliminated and surgical time may be minimised [5].Theoretically, the risk of re-fracture may be reduced by decreasing stress risers [5, 33]. It may facilitate removal of hardware and can decrease the chance of neurovascular injuries.
A controversial topic is the removal of hardware after fracture healing. There is no clear data in the literature regarding routine removal of paediatric implants, even though, it is a procedure offered as a general practice at many institutions [34]. Kahle et al. [35] reported an overall complication rate of 13%; they stated that there was very little clinical or experimental evidence to support a policy of routinely removing asymptomatic implants. On the other hand, implants left in the growing child could be buried deep inside of the bone, or cause “periprosthetic” fractures and/or eventually impede adult reconstruction procedures; other concerns are stress shielding, risk of corrosion, metal allergy, and potential carcinogenesis [34]. Using locking plates may have some advantages; besides the one mention in the above paragraph (unicortical screws), the fact that the placement is extraperiosteal may reduce the prevalence of incorporation of the hardware being easier to remove. It is important to emphasise that this could not be a primary reason for choosing a locking implant; it should be based on the principles of osteosynthesis that the surgeon would wish to apply.
One of the most important indications for locking plates in children is in metadiaphyseal fractures, particularly when they are in close proximity to the growth physis and there is resultant limited space available for internal fixation [23, 24]; this could also be complicated by a poor bone quality. Restoration of alignment in the coronal plane is important because of its limited potential for remodelling. Based on this characteristic, a fixed angle device would be an excellent implant to use because it allows for restoration of alignment, avoids the physis and provides fracture stability [5].
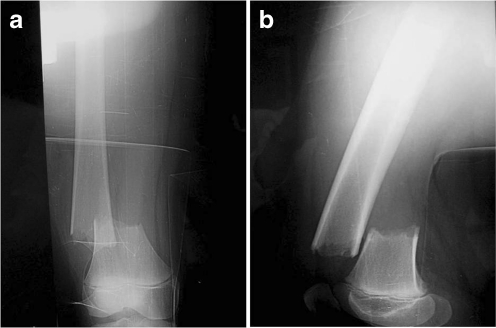
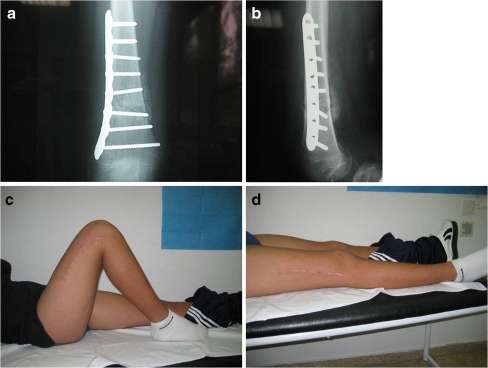
Another possible indication is for periarticular fractures, such as unstable subtrochanteric fractures or supracondylar fractures of the femur (Fig. 2a, b) that could be fixed with bride plating with or without locked screws with the advantage that screws could be placed avoiding the physis (Fig. 3a–d).
Fig. 2.
A 13-year-old boy with a distal right femoral fracture sustained after a casual fall. a Anteroposterior view. Open physis. b Lateral view. Open physis
Fig. 3.
Six-week postoperative radiograph after fixation with a locking plate (LCP®). Fixation with locked screws of the distal fragment can be seen. a Anteroposterior view. b Lateral view. c More than 90° flexion of the ipsilateral knee. d Full extension of the ipsilateral knee
As in adults, there is a group of children with poor quality bone (osteopenia/osteoporosis), e.g. in cases of cerebral palsy, neuromuscular disorders, and osteogenesis imperfecta. Children with cerebral palsy have a significantly increased risk of fractures; Leet et al. [36] reported an incidence of 12%. Fractures heal quickly with abundant callus, and closed treatment is very difficult. An important complication is the formation of decubitus ulcers and conversion to open fractures because of the spasticity. Symptoms of fracture must be carefully differentiated from those of osteomyelitis, septic joints, and bone tumours. A pre-existing contracture in contiguous joints is a potent factor in the production of many of these fractures [37]. Other predictive factors are older age at first fracture and valproic acid use [36]. McIvor et al. [37] conducted a study including 92 patients with 134 fractures, and claimed that once union occurred, functional status restored to pre-fracture status. Immobilisation must be sufficient to prevent gross motion at the fracture site and should permit periodic inspection to detect incipient decubitus ulcer formation (Table 3). Using a locking plate may help to achieve this target.
Table 3.
Summary of findings from the study articles retrieved and reviewed concerning osteopenic/osteoporotic bone
| Author | Year | Number of patients | Method | Use | Characteristics | Results | Conclusions |
|---|---|---|---|---|---|---|---|
| Enright et al. [38] | 2006 | 4 (6 femurs, 2 tibias) | Bone plating (non-locking plates) | Osteogenesis imperfecta type III | Mean age (operation): 44 months 13 bone platings (8 bones studied) Follow-up: 4 years Mean time to revision 27 months |
Indications for revision: fracture (6), deformity (3), hardware failure (3) and nonunion (1) One compartment syndrome All were revised to elongating IM Bailey-Dubow rods |
Bone plating in skeletally immature patients with osteogenesis imperfect does not provide better outcome than elongating rods |
| McIvor et al. [37] | 1966 | 92 px (134 fx) | Different osteosynthesis methods and closed treatment | Cerebral palsy | No correlation between type of cerebral palsy and incidence or location of fracturea | Once union occurred, functional status restored to prefracture status There were three nonunions and several malunionsb 19 px sustained refractures Complications (+freq): 17 decubitus ulcersc Two px with significant growth disturbances |
Severe preexistent deformity obviates the use of conventional immobilization in a plaster cast Immobilization must be sufficient to prevent gross motion at the fracture site Should permit periodic inspection to detect incipient decubitus ulcer formation |
a A contracture or paralytic dislocation of the hip was found to predispose to fracture of the femur. Contractures in near joints predisposed to fractures
b Severity of malunion correlates with severity of contracture
c More frequent in femoral fractures treated by a hip spica or traction
Another group of patients with poor bone quality are those with osteogenesis imperfecta. Enright et al. [38] used a bone plating technique in these type of patients. There was a high rate of complications; however, bone plating was done with conventional plates and all were revised to elongating IM Bailey-Dubow rods. His conclusion was that this technique does not provide better outcome than elongating rods (Table 3). In this poor quality bone the primary mode of failure is the bone, and locking plates allow for the creation of a single-beam construction, requiring larger areas of bone failure to bring about loss of reduction. In this sense, this type of implant could be a possible alternative even though more studies need to be made.
Another possible field of application is the post-resection reconstruction with allografts after oncological treatment. The greatest barriers for allograft survival are fractures, nonunions and infection [39]. There are some theoretical advantages when using locking plates for allograft fixation such as reducing the fracture rate, because using unicortical screws can help reduce stress risers, and provide a stable construction which helps to achieve an optimum healing time [39–41].
Up to this point we have seen all the possible applications and advantages of this system; however, there are some potential disadvantages that we have to keep in mind.
Locking plates are designed to maintain, not to obtain, fracture reduction [5]. This is a very important concept because the reduction has to be obtained before using the plate. This differs from the conventional plating technique in which reduction can be achieved during its application.
The rigidity of the locked screw-plate construction prevents load sharing [5, 15, 22]. If it is subjected to repetitive loading, it may fracture and fixation will be lost.
In children's fractures, it is not uncommon to observe an overgrowth phenomenon [10] associated with younger patients. This is believed by some authors [24] to be related to the age more than with the operative method. Implant irritation of the skin is another issue, related to the subcutaneous location. This is most seen with tibial fractures treated by this method as described by Yusof et al. [24] who had one case in his series of 16 children.
One of the most important issues of this system is the cost of the implants. This could prevent a wider use, particularly in developing countries. These implants can cost up to four times that of the conventional plates [5]; so they should be reserved for instances in which they are known to be advantageous.
There is a trend to remove implants used in children, and a disadvantage of these plates is that although they can be inserted through small incisions, removal may require larger ones. Also, using titanium plates could make removal difficult because of the cold welding of screws to the plate [5], and stripping of screw heads is common with a percutaneous attempt.
Conclusion
In most cases closed reduction and immobilisation restores normal function to a pediatric extremity. However, there are some traumatic as well as orthopaedic situations in which fixation devices have to be used. Different examples of these have been seen through this article and, based on the biology of fracture healing and the target of the fixation devices used in children, locked plating systems appear as a good alternative, even though there are some disadvantages that must be taken into account.
Acknowledgement
Figure reprinted from Injury [Wagner M (2003) General principles for the clinical use of the LCP. Injury; 34(Suppl 2):31–42] with permission from Elsevier.
The authors appreciate the contribution of Dra. Maria Teresa Menéndez for the photographs used to illustrate this manuscript.
References
- 1.Worlock P, Stower M. Fracture patterns in Nottingham children. J Pediatr Orthop. 1986;6(6):656–660. doi: 10.1097/01241398-198611000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Pretell Mazzini J, Rodriguez Martin J. Paediatric forearm and distal radius fractures: risk factors and re-displacement—role of casting indices. Int Orthop. 2009 doi: 10.1007/s00264-009-0904-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Landin LA. Epidemiology of children’s fractures. J Pediatr Orthop B. 1997;6(2):79–83. doi: 10.1097/01202412-199704000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Slongo TF. The choice of treatment according to the type and location of the fracture and the age of the child. Injury. 2005;36(Suppl 1):A12–A19. doi: 10.1016/j.injury.2004.12.008. [DOI] [PubMed] [Google Scholar]
- 5.Vander Have K, Herrera J, Kohen R, Karunakar M. The use of locked plating in skeletally immature patients. J Am Acad Orthop Surg. 2008;16(8):436–441. doi: 10.5435/00124635-200808000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Rodríguez-Merchán EC. Pediatric skeletal trauma: a review and historical perspective. Clin Orthop Relat Res. 2005;432:8–13. doi: 10.1097/01.blo.0000155377.95940.81. [DOI] [PubMed] [Google Scholar]
- 7.Currey J, Butler G. The mechanical properties of bone tissue in children. J Bone Joint Surg Am. 1975;57:811–814. [PubMed] [Google Scholar]
- 8.Jacobsen J. Periosteum: its relation to pediatric fractures. J Pediatr Orthop Br. 1997;6:84–90. [PubMed] [Google Scholar]
- 9.Wallace M, Hoffman E. Remodelling of angular deformity after femoral shaft fractures in children. J Bone Joint Surg Br. 1992;74:765–769. doi: 10.1302/0301-620X.74B5.1527131. [DOI] [PubMed] [Google Scholar]
- 10.Zafra Jimenez JA, Moratinos Palomero P, Resines Erasun C. Effects of metaphyseal periosteum section of the growth cartilage and tibial development. Experimental study in New Zealand rabbits. Rev Orthop Traumatol. 2002;46(4):341–350. [Google Scholar]
- 11.Pretell Mazzini JA, Ruiz Semba C, Rodriguez Martín J. Bone defect healing: delay of consolidation and pseudoarthrosis. Rev Med Hered. 2009;20:31–39. [Google Scholar]
- 12.McKibbin B. The biology of fracture healing in long bones. J Bone Joint Surg Br. 1978;60:150–162. doi: 10.1302/0301-620X.60B2.350882. [DOI] [PubMed] [Google Scholar]
- 13.Strauss EJ, Schwarzkopf R, Kummer F, Egol KA. The current status of locked plating: the good, the bad, and the ugly. J Orthop Trauma. 2008;22:479–486. doi: 10.1097/BOT.0b013e31817996d6. [DOI] [PubMed] [Google Scholar]
- 14.Gautier E, Perren SM, Cordey J. Effect of plate position relative to bending direction on the rigidity of a plate osteosynthesis: a theoretical analysis. Injury. 2000;31(suppl 2):C14–C20. doi: 10.1016/S0020-1383(00)80027-3. [DOI] [PubMed] [Google Scholar]
- 15.Smith WR, Ziran BH, Anglen JO, Stahel PF. Locking plates: tips and tricks. J Bone Joint Surg Am. 2007;89:2298–2307. doi: 10.2106/JBJS.F.00615. [DOI] [PubMed] [Google Scholar]
- 16.Morscher E, Sutter F, Jenny H, Olerud S. Anterior plating of the cervical spine with the hollow screwplate system of titanium. Chirurg. 1986;57:702–707. [PubMed] [Google Scholar]
- 17.Arnold W. Initial clinical experiences with the cervical spine titanium locking plate. Unfallchirurg. 1990;93:559–561. [PubMed] [Google Scholar]
- 18.Söderholm AL, Lindqvist C, Skutnabb K, Rahn B. Bridging of mandibular defects with two different reconstruction systems: an experimental study. J Oral Maxillofac Surg. 1991;49:1098–1105. doi: 10.1016/0278-2391(91)90145-C. [DOI] [PubMed] [Google Scholar]
- 19.Miclau T, Remiger A, Tepic S, Lindsey R, McIff T. A mechanical comparison of the dynamic compression plate, limited contact-dynamic compression plate, and point contact fixator. J Orthop Trauma. 1995;9:17–22. doi: 10.1097/00005131-199502000-00003. [DOI] [PubMed] [Google Scholar]
- 20.Kolodziej P, Lee FS, Patel A, Kassab SS, Shen KL, Yang KH, Mast JW. Biomechanical evaluation of the Schuhli nut. Clin Orthop Relat Res. 1998;347:79–85. doi: 10.1097/00003086-199802000-00010. [DOI] [PubMed] [Google Scholar]
- 21.Borgeaud M, Cordey J, Leyvraz PE, Perren SM. Mechanical analysis of the bone to plate interface of the LC-DCP and of the PC-FIX on human femora. Injury. 2000;31(Suppl 3):C29–C36. doi: 10.1016/S0020-1383(00)80029-7. [DOI] [PubMed] [Google Scholar]
- 22.Wagner M, Frenk A, Frigg R. New concepts for bone fracture treatment and the locking compression plate. Surg Technol Int. 2004;12:271–277. [PubMed] [Google Scholar]
- 23.Kanlic EM, Anglen JO, Smith DG, Morgan SJ, Pesántez RF. Advantages of submuscular bridge plating for complex pediatric femur fractures. Clin Orthop Relat Res. 2004;426:244–251. doi: 10.1097/01.blo.0000138961.34810.af. [DOI] [PubMed] [Google Scholar]
- 24.Yusof NM, Oh CW, Oh JK, Kim JW, Min WK, Park IH, Kim HJ. Percutaneous plating in paediatric tibial fractures. Injury. 2009 doi: 10.1016/j.injury.2009.02.020. [DOI] [PubMed] [Google Scholar]
- 25.Oh CW, Shetty GM, Song HR, Kyung HS, Oh JK, Min WK, Lee BW, Park BC. Submuscular plating after distraction osteogenesis in children. J Pediatr Orthop B. 2008;17(5):265–269. doi: 10.1097/BPB.0b013e32830688d8. [DOI] [PubMed] [Google Scholar]
- 26.Iobst CA, Dahl MT. Limb lengthening with submuscular plate stabilization: a case series and description of the technique. J Pediatr Orthop. 2007;27(5):504–509. doi: 10.1097/01.bpb.0000279020.96375.88. [DOI] [PubMed] [Google Scholar]
- 27.Skaggs DL, Leet AI, Money MD, Shaw BA, Hale JM, Tolo VT. Secondary fractures associated with external fixation in pediatric femur fractures. J Pediatr Orthop. 1999;19:582–586. doi: 10.1097/00004694-199909000-00005. [DOI] [PubMed] [Google Scholar]
- 28.SongKM SB, Benirschke S, Browne R. Open fractures of the tibia in children. J Pediatr Orthop. 1996;16:635–639. doi: 10.1097/00004694-199609000-00016. [DOI] [PubMed] [Google Scholar]
- 29.Highland TR, LaMont RL. Deep, late infections associated with internal fixation in children. J Pediatr Orthop. 1985;5:59–64. doi: 10.1097/01241398-198501000-00010. [DOI] [PubMed] [Google Scholar]
- 30.Ağuş H, Kalenderer O, Eryanilmaz G, Omeroğlu H. Biological internal fixation of comminuted femur shaft fractures by bridge plating in children. J Pediatr Orthop. 2003;23(2):184–189. doi: 10.1097/00004694-200303000-00010. [DOI] [PubMed] [Google Scholar]
- 31.Oh CW, Song HR, Jeon IH, Min WK, Park BC. Nail-assisted percutaneous plating of pediatric femoral fractures. Clin Orthop Relat Res. 2007;456:176–181. doi: 10.1097/BLO.0b013e31802f583a. [DOI] [PubMed] [Google Scholar]
- 32.Sink EL, Hedequist D, Morgan SJ, Hresko T. Results and technique of unstable pediatric femoral fractures treated with submuscular bridge plating. J Pediatr Orthop. 2006;26(2):177–181. doi: 10.1097/01.bpo.0000218524.90620.34. [DOI] [PubMed] [Google Scholar]
- 33.Frigg R, Appenzeller A, Christensen R, Frenk A, Gilbert S, Schavan R. The development of the distal femur less invasive stabilization system (LISS) Injury. 2001;32(suppl 3):SC24–SC31. doi: 10.1016/s0020-1383(01)00181-4. [DOI] [PubMed] [Google Scholar]
- 34.Busam ML, Esther RJ, Obremskey WT. Hardware removal: indications and expectations. J Am Acad Orthop Surg. 2006;14(2):113–120. doi: 10.5435/00124635-200602000-00006. [DOI] [PubMed] [Google Scholar]
- 35.Kahle WK. The case against routine metal removal. J Pediatr Orthop. 1994;14:229–237. doi: 10.1097/01241398-199403000-00019. [DOI] [PubMed] [Google Scholar]
- 36.Leet AL, Mesfin A, Pichard C, Launay F, et al. Fractures in children with cerebral palsy. J Pediatr Orthop. 2006;26(5):624–627. doi: 10.1097/01.bpo.0000235228.45539.c7. [DOI] [PubMed] [Google Scholar]
- 37.McIvor WC, Samilson RL. Fractures in patients with cerebral palsy. J Bone Joint Surg Am. 1966;48(5):858–866. [PubMed] [Google Scholar]
- 38.Enright WJ, Noonan KJ. Bone plating in patients with type III osteogenesis imperfecta: results and complications. Iowa Orthop J. 2006;26:37–40. [PMC free article] [PubMed] [Google Scholar]
- 39.Buecker PJ, Berenstein M, Gebhardt MC, Hornicek FJ, Mankin HJ. Locking versus standard plates for allograft fixation after tumor resection in children and adolescents. J Pediatr Orthop. 2006;26(5):680–685. doi: 10.1097/01.bpo.0000230333.73286.06. [DOI] [PubMed] [Google Scholar]
- 40.Enneking WF, Campanacci DA. Retrieved human allografts: a clinicopathological study. J Bone Joint Surg. 2001;83A(7):971–986. [PubMed] [Google Scholar]
- 41.Enneking WF, Mindell ER. Observations on massive retrieved human allografts. J Bone Joint Surg. 1991;73-A(8):1123–1142. [PubMed] [Google Scholar]