Abstract
Displaced acetabular fractures should be treated surgically. Over the past decade, surgical approaches to the acetabulum and the surgical technique for repair of common fracture patterns have advanced. Excellent outcomes after repair of these injuries can be achieved. The aim of this study was to assess the medium-term results of reconstruction of acetabular fractures by using shape-memory alloy designed by the authors. This is a retrospective review conducted at a level 1 trauma centre. From October 1999 to July 2009, 19 patients with acetabular fractures were treated with our patented Ni-Ti shape-memory alloy acetabular tridimensional memory alloy-fixation system (ATMFS). The ATMFS device was cooled with ice before implantation and then warmed to 40–50°C after implantation to produce balanced axial and compression forces that would stabilise the fracture three dimensionally. Our results are as follows; according to the D’Aubigne−Postel scoring system: Fifteen cases out of 19 (79%) achieved excellent or good clinical results. In two patients, late complications included avascular necrosis of the femoral head (ANFH) associated with posterior dislocation of the hip joint two years after the operation. We also observed two cases of grade II or III ectopic ossification, with good hip function, and one case of traumatic arthritis. In conclusion, these results demonstrate the effectiveness of the ATMFS device for the management of acetabular fracture. The device provides continuous compression of the fracture with minimal disruption to the local blood supply.
Introduction
In the last 20 years with the rapid development of industry, China has seen an increased incidence of acetabular fractures due to traffic accidents. Complicated acetabular fractures combined with bone defects are increasingly common. However, the treatment of acetabular fractures, especially complicated acetabular fractures, remains a major challenge for orthopaedic surgeons. The most important challenges are rehabilitation of the patients and the rising incidence of post-traumatic complications. Remodelling the anatomical morphology of the head socket and effective fixation are the key to hip function rehabilitation, whereas incorrect handling can lead to disability of varying degree, joint replacement or reoperation. Letournel suggested that it was crucial to restore the anatomy of the articular surface in the context of acetabular fracture, based on the observation that in 82% of patients who underwent intraoperative anatomical reduction, satisfactory results were obtained [1]. Open reduction and internal fixation have been recognised as the gold standard for the treatment of complicated acetabular fractures [1–4]. The main purpose of intraoperative anatomical reduction and strong internal fixation is articular stability and early patient mobilisation.
Nitinol (NiTi) shape-memory alloy, as a functional metal material, has many advantages, such as shape-memory effect, remarkable resistance to wear and corrosion and good histocompatibility. Since its approval into the medical market by the US Food and Drug Administration (FDA) in 1990, NiTi shape-memory alloy has been applied extensively. NiTi shape-memory alloy is regarded as an important discovery in medical material science and a valuable “biological memory material”. The NiTi heamofilter designed by Simon was demonstrated to be effective following application in 147 patients at 19 cardiovascular centres [5]. Later on, with further studies, shape-memory alloys were gradually applied in clinical practices such as the department of stomatology and orthopaedics and gained huge success [6, 7].
Operations on acetabular fractures aim at anatomical reconstitution of the acetabular articular surface. Decreased incidence of traumatic arthritis and hip ankylosis facilitate early patient mobilisation via strong internal fixation. Unfortunately, the deep location and irregular shape have challenged internal fixation with the use of the plate and screw, especially in complicated acetabular fractures. In view of this, we developed the acetabular tridimensional memory alloy-fixation system (ATMFS) (Chinese Patent: ZL 01 3 52647.2) according to the specific mechanical properties of biological memory material, nitinol alloy, and the anatomical and biomechanical features of the acetabulum [8]. This study aims to introduce the characteristics of the new internal fixation device for acetabular fractures. We relate our experience retrospectively analysing 19 acetabular fracture cases treated using ATMFS from October 1999 to July 2009.
Materials and methods
Inclusion criteria
All patients met Letournel fracture diagnostic classification criteria, were between 18–75 years of age and provided written informed consent.
Exclusion criteria
We excluded patients with severe lung and heart diseases, hypertension, or history of a psychiatric disorder; with neurological deficits associated with tetraplegia; who did not meet Letournel fracture diagnostic classification criteria; with pre-existing avascular necrosis of the femoral head; who were primarily fixed with nickel-clad devices in the ATMFS series; who could not objectively fill in the effect items of the study; or who declined to provide informed consent forms.
In all, 19 cases were included in the study: 13 men and six women; ages ranging from 21–68 (mean 44.1) years. Injuries arose from traffic accidents in 12 cases and falling from a height in seven. They involved the left side in nine cases and the right in ten. Mean Injury Severity Score (ISS) was 18.5 ± 9.3. All injuries were evaluated preoperatively with radiographs in the anteroposterior view, obturator oblique view, iliac oblique view, with two-dimensional computed tomography (CT) and three-dimensional CT reconstruction analysis. According to the Letournel−Judet classification, there were five cases of simple fracture and 14 of complicated fracture, including three of injuries following dislocation of the hip joint and two of sciatic nerve injury. There was >3 mm of displacement in the acetabular articular surface of each case, revealed by imaging. The length of time between injury and surgery was one to three weeks in 12 cases, four to eight weeks in three, eight to 11 in two and more than 12 weeks in two. Patients with posterior dislocation of the hip joint were treated by closed reduction within eight hours under general anaesthesia, and those with fresh fracture underwent surgery within seven days. Skeletal traction via the femoral condyles was applied in all patients for joint distraction.
Structure and working principle of the ATMFS device
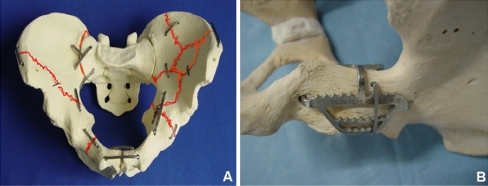
The ATMFS device (Figs. 1, 2) (Huzhou Swan Biological Memory Medical Devices Co., Ltd., Zhejiang, China) is made of NiTi shape-memory alloy in a design based on the variations of pelvic anatomy and biomechanical features of the acetabulum. It is 50–53% nickel and the rest titanium, with plate thickness ranging from 1 to 5 mm in different types of assembly units. There are four ATMFS series (Fig. 1), with distinctions based on the anatomical features of the acetabulum: Series A for anterior column or wall, series B for posterior column or wall, series C for connection of two displaced fragments, and series D for the greater trochanter. Each series consists of several versions. Series A consists of the anterior column arch, the arm, and a square-area top panel. In series B, type Ba I consists of a posterior column arch, fossa net and square-area back panel. Type Ba II and III differ in that they contain either a square-area back panel or fossa network. Type Bb I consists of the guidance suppository and posterior wall hook, whereas type Bb II is made up of one more posterior wall hook. In series C, type I consists of a forward arc and symmetry arm tooth, type II consists of a forward arc and asymmetric arm tooth and type III consists of a reverse arc and asymmetric arm tooth. Series D consists of a guide pin for great the trochanter and arc tooth. The ATMFS series exhibits a unilateral memory effect. The memory distances between arms are 3–40 mm, and the recovery temperature at phase change is 33 ± 2°C.
Fig. 1.
Acetabular tridimensional memory alloy-fixation system (ATMFS) device of four series
Fig. 2.
Structure and working principle of the acetabular tridimensional memory alloy-fixation system (ATMFS) device
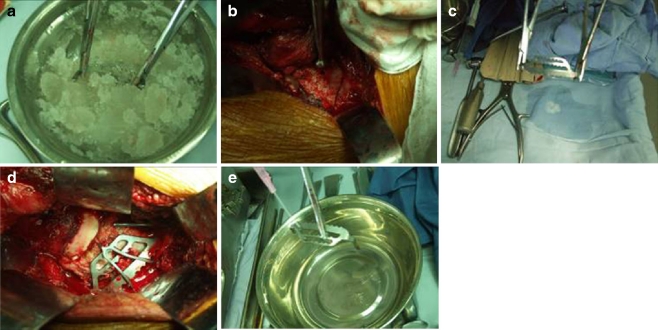
When in use, the ATMFS should first be placed in cold water of 0−4°C (Fig. 3) to allow the plastic deformation of the NiTi alloy. Then the arm should be unfolded using needle forceps, and a hole should be drilled to the intended fixed position, around the two sides of the fracture point, with the middle part of the arm aiming at the fracture fragment. After the fracture sites are reduced, ATMFS should be implanted and reheated in warm (40−50°C) water to generate the appropriate mechanical behaviour. The memory alloy creates three-dimensional stereo fixation by maintaining the bone block in a system driven by temperature.
Fig. 3.
a Step one: extend the selected acetabular tridimensional memory alloy-fixation system (ATMFS) in the mixture of ice and water; unfold the arms in sequence. b, c, d Step two: drill at the appropriate position of the acetabulum for the extended arm; insert the two arms into the hole. e Step three: spray hot water on the memory alloy to allow morphological recovery, making sure that the recovery stress has an influence on the noncontinuous end of the bone
Surgical procedures
All operations were performed by the same group of surgeons using general anaesthesia. According to the specifics of each case, we applied the Kocher−Langenbeck approach, the combined anterior and posterior approach or the improved ilioinguinal approach using a corresponding ATMFS device. The posterior hip approach was the first approach attempted for the fresh fracture, and greater trochanter second half osteotomy was performed to ensure sufficient exposure. We exposed the fracture ends of the posterior column fossa to identify the relationship between fractured bones and perform the initial reduction. We cooled the B and C series in ice water ( 0–4°C) to expand the branches and arms. To do this: (1) We found the fixation point of the displaced greater fragments, fixed the fragments and obtained anatomical reduction using the C series. (2) With regard to the acetabular fracture of the square area, we drilled two bone holes at a distance of 1 cm from the greater sciatic notch and lesser sciatic notch to insert the arm of Ba. We placed the square-area back panel over the posterior column ridge line to limit the posterior wall of the square area so that the fossa net sticks to the back wall of the diaplastic fossa (Fig. 3). We then sprayed warm salt water (40–50°C) on the ATMFS device following the anatomical reduction and fixation of ATMFS to ensure its shape recovery and its correct mechanical role. (3) In terms of the acetabular posterior wall fracture, at the edge of the acetabulum, we drilled a tunnel at a 10°–15° angle to the posterior acetabular wall after the fixation of Ba, pointing to the anterior inferior part of the posterior column ridge line, making sure to avoid penetration of the tunnel into the joint. According to the length of the tunnel, we inserted Bb of suitable length, and hung the posterior fossa hook on the concave face of Ba or inserted it through the drill hole in order to fix the bones of the acetabular posterior wall after rewarming Bb (Fig. 3). (4) As for the cases of greater trochanter osteotomy, we performed a reduction and internal fixation of the greater trochanter using series D. There are no differences between the anterior and the posterior approach for old acetabular fractures. Finally, we combined solution and reduction for fractures of the anterior and posterior column of the acetabulum.
Postoperative treatment
Postoperative prophylactic antibiotics were used regularly for five to seven days. No drugs or radiation were used to prevent heterotopic ossification. A drainage tube was used for one to three days and removed when the drainage flow within 24 hours remained <20 ml. Isometric contraction training of the lower limbs was performed right after the patient awoke from anaesthesia. The next day, the patients were asked to gradually initiate extension and flexion of the hip while on the bed with gradually increasing degrees of flexion. All patients were mobilised non-weight bearing for four weeks. Partial, toe-touch weight bearing with crutches or a walker was allowed for a period of three months. Subsequently, full weight bearing was allowed. Postoperative radiographs were used to determine the congruency of fracture reduction. All fractures with a displacement of 2 mm or less on any of the three views were considered congruent. Follow-up was performed in the second week, sixth week, third month, and first year after the operation. The functional outcome was evaluated according to D’Aubigne−Postel scoring system [9], which is based on the level of pain, the patient’s walking ability and the range of motion of the hip joint. Furthermore, outcome was evaluated radiologically based on the criteria described by Matta [3]. The results were considered excellent when the hip joint had a normal appearance on plain X-rays, good when there was minimal subchondral sclerosis and joint-space narrowing, fair when 50% of joint-space narrowing existed and poor when >50% of joint-space narrowing, head collapse or acetabular wear were present.
Results
The average operation time was 3.6 hours (range 1.50–6.55 h); average blood loss was 430 ml (range 350–3800 ml); average length of hospital stay was ten days (range seven to 21 days). In 17 (89%) cases, congruent reduction was achieved, and in the remaining two cases, the reduction was considered incongruent. These two patients were operated upon more than eight weeks after injury. None of the patients in this study lost reduction after surgery, and there were no cases of implant failure. The average follow-up time was 58.5 (range 25–103) months. By an average of 5.3 months after the operation, hip function on the injury side had almost reached that of the normal side in 14 cases. At the final follow-up, D’Aubigne−Postel scores were excellent in seven cases (17–18), good in eight (15–16), fair in two (12–14) and poor in one (<12). According to Matta’s X-ray evaluation, evaluations were excellent in 12 cases, good in four, fair in two and poor in one. Ten cases of complicated acetabular fracture and five of simple fracture obtained excellent or good scores. Patient characteristics are shown in Table 1. Two typical cases are shown in Figs. 4 and 5.
Table 1.
Patients’ clinical details
| No. | Sex/age | Mechanism of injury type | Side | Fracture type | Postoperative complications | Follow-up (months) | Merle d’Aubigne scoring |
|---|---|---|---|---|---|---|---|
| 1 | M/21 | Traffic accident | L | Posterior wall | 25 | Excellent (17) | |
| 2 | M/35 | Traffic accident | R | Transverse, posterior wall | Grade III Heterotopic ossification | 58 | Fair (12) |
| 3 | M/45 | Traffic accident | L | T-shaped | 28 | Excellent (18) | |
| 4 | F/27 | Fall | L | Posterior wall | Superficial infection | 32 | Excellent (17) |
| 5 | F/41 | Traffic accident | L | Both column | 42 | Good (15) | |
| 6 | M/68 | Traffic accident | R | Transverse, posterior wall | 66 | Good (15) | |
| 7 | F/41 | Fall | L | Transverse | 69 | Excellent ( 18) | |
| 8 | M/56 | Traffic accident | R | Posterior column, posterior wall | ANFH | 41 | Poor (7) |
| 9 | F/33 | Fall | R | Both column | 86 | Good (15) | |
| 10 | M/57 | Fall | R | Posterior wall | Posttraumatic arthritis | 103 | Good (15) |
| 11 | M/34 | Traffic accident | L | Both column | 61 | Fair (13) | |
| 12 | M/62 | Traffic accident | R | Transverse, posterior wall | 49 | Excellent (18) | |
| 13 | M/45 | Fall | L | Both column | 95 | Excellent (17) | |
| 14 | F/54 | Traffic accident | L | Transverse, posterior wall | ANFH | 33 | Poor (6) |
| 15 | F/28 | Fall | R | Both column | 42 | Good (16) | |
| 16 | M/57 | Traffic accident | R | Transverse, posterior wall | 84 | Good (17) | |
| 17 | M/36 | Traffic accident | L | T-shaped | 78 | Good (16) | |
| 18 | M/54 | Traffic accident | R | Transverse | 50 | Excellent (18) | |
| 19 | M/43 | Fall | R | Transverse posterior wall | Grade II heterotropic ossification | 69 | Good (16) |
ANFH avascular necrosis of the femoral head
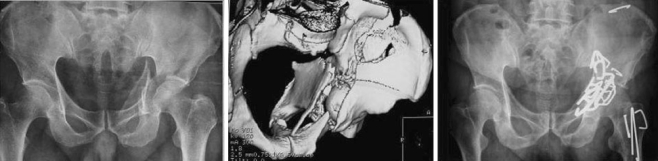
Fig. 4.
Typical case one: A 41-year-old woman presented with double column fractures of the left acetabulum, rib fracture and diaphragmatic hernia following a traffic accident. The operation was performed 13 days after the injury. The patient could walk by herself, and the function of the injured joint was similar to the normal side 12weeks after the acetabular tridimensional memory alloy-fixation system (ATMFS) internal fixation. Matta’s X-ray evaluation was scored asexcellent, and d’Aubigne and Postel’s clinical outcome evaluation was scored as good at the last follow-up (42 months postoperatively)
Fig. 5.
Typical case two: A 45-year-old man presented with double column fractures of the left acetabulum following a fall from a height. The operation was performed 23 days after the injury. The function of the injured joint was similar to the normal side 12weeks after acetabular tridimensional memory alloy-fixation system (ATMFS) internal fixation. Matta’s X-ray evaluation was scored as excellent, and d’Aubigne and Postel’s clinical outcome evaluation was scored as excellent at the last follow-up (95 months postoperatively). a, b X-ray and three-dimensional computed tomography (CT) of the complicated acetabular fracture before the operation; c postoperative X-ray
The early complications included deep infection, pulmonary embolism (PE), and deep venous thrombosis (DVT). One case of superficial wound infection was cured by changing the dressings and intravenously administering antibiotics. Two cases of sciatic nerve injury recovered within two months after the operation. Late complications included avascular necrosis of the femoral head (ANFH) in two patients who exhibited posterior dislocation of the hip joint at two years after the operation; two cases of grade II or grade III heterotopic ossification, with good hip function; and one case of traumatic arthritis. Among those with late complications, two patients asked for a prosthetic hip replacement due to poor hip function.
Discussion
The treatment of acetabular fracture has become a major focus in recent years. The medical community has reached a consensus that the surgery should aim at anatomical reduction of the hip-joint surface. Whereas strong fixation enables early movement among patients and reduces the development of traumatic arthritis or hip ankylosis, the results of middle- and long-term follow-up varied. Letournel and Matta [1, 10] suggested that even with a 94–100% anatomical reduction rate, the percentage of hip function scores that were excellent and good remained only 68–82%. Some of the recent studies [11] showed 30% reduction loss within the first year of follow-up, whereas other studies reported >80% [12, 13]. Stockle et al. [14] performed internal fixation with lag screws in 45 cases of acetabular fracture. Although 38 patients scored excellent and good scores, the reconstruction plate is needed to support patients with severe comminuted fracture or osteoporosis. Among 262 acute acetabular fracture patients treated by Matta, 22 cases had posterior wall involvement and were followed up at 2–14 years [3]. Postoperative X-ray evaluation revealed 22 cases of anatomical reduction. Only 15 cases (68%) had excellent and good scores, whereas the other seven cases had a fair and poor outcome. Pantazopoulos et al. [13] followed up 52 patients with acetabular fracture for 2–15 years; 44 cases (85%) had excellent and good scores, consistent with an accurate reduction. In this study, 15 cases out of 19 had excellent and good scores, in accordance with the previous studies.
In our study, 79% of patients had excellent to good outcome in the medium term, which is comparable with other studies. The authors postulate that damage to the articular cartilage at the time of initial injury may play an important role in post-traumatic arthritis. The severity of this injury may not be of a grade high enough to cause necrosis of cartilage in the early period but, instead, may cause slow degeneration over a longer period of time. This may be the reason for poor outcome, even in anatomical reconstruction of the joint when cases are followed up for a prolonged period. Further basic science research is needed to assess injury to the cartilage and perhaps predict prognosis, depending upon the severity, if the joint is reconstructed anatomically.
It is important to achieve stable fixation of the acetabulum considering the amount of force delivered to it, especially during the immediate postoperative period and the early part of rehabilitation when range of motion is started. Studies by Goulet et al. [15] have demonstrated that fixation with spring plates and reconstruction plates have a higher load to failure than reconstruction plates alone, especially in concentrically comminuted fractures. Im et al. [16] in their study of 15 patients, used only screws for posterior wall fractures with single-fragment or moderate communition. Though they had good results, a description of the exact percentage of communition or the minimum size of the fragments amenable to screw fixation was not reported. They also emphasised that using screws alone can interfere with early weight bearing compared with buttress-plate fixation.
The ATMFS is designed according to the changeable and irregular arc anatomical characteristics of the pelvis and can be applied in various kinds of acetabular fractures. As ATMFS is made of NiTi memory alloy, which has proven biocompatibility [17–20], there is no absolute contraindication for the operation. After massive experimental study in animals, the patented device was officially approved for clinical use in China (State of Intellectual Property Office, China. Certificate No. 244171). Due to the inherent property of shape-memory alloy, the compression arms in the device yielded evenly distributed compression forces. These forces provide continuous axial compression on the fractured ends, which can be transmitted across the fracture to ensure the stable biomechanical environment that allows smooth healing of the fracture. The ATMFS device has direct contact with the acetabular bone surface at multiple points to establish a three-dimensional stabilisation of the fracture. This three-dimensional fixation confers strong resistance on the fracture against rotation and shearing stress and also protects the blood supply crucial for bone healing. We consider that, compared with plate or lag screws, the ATMFS has the advantage of accurately reducing and stabilising broken bones to the anatomical position. The memory effects of ATMFS facilitate aggregation of the fragments to a compressive stress state, ensuring accurate anatomical reduction and stability. In addition, the main plate of the device bridging the fracture offers optimal sites for bone-graft implantation.
Due to the nature of shape-memory alloys, the manipulation and implantation of ATMFS must proceed with the following precautions. Prior to implantation, the ATMFS device is immersed in ice-cold water at 0–4°C, and after reduction of the fracture, the ATMFS is implanted and warmed with water of 40–50°C. Ideally fixation of the fracture with ATMFS is performed in a single attempt, and repeated cooling and warming of the device, once implanted, must be totally avoided. In all the subsequent procedures after ATMFS implantation, the device has to be washed, when necessary, with warm water >40°C. Ice-cold water or water <40°C should never be used for washing the implanted device, or the fixation performance of the device can be lowered.
There were two cases (10.5%) of heterotopic ossification of grades II and III in our study, which were less than in other studies [21, 22] in which nonsteroidal anti-inflammatory drugs (NSAIDS) or radiological therapy was used. In preventing heterotopic ossification, the authors did not use NSAIDS or radiological therapy that many experts administer, and instead have adopted the following methods: irrigate thoroughly, remove the cancellous bone residues, in situ suture the soft tissues of the joint capsule and start early mobilisation exercises. The authors recommend that patients start postoperative function exercises gradually and increasingly. It is good for the development of enhancing muscle strength, promoting blood circulation, modulating secretion of joint synovia and improving overall health. Our experiences provided new references for orthopaedic surgeons as far as preventing heterotopic ossification and recovering postoperative hip function as soon as possible.
In conclusion, reconstruction of fractures of the acetabulum via the ATMFS can be expected to produce good results. The advantages of ATMFS in the treatment of acetabular fractures, as we presume, lie mainly in the continuous compression of the fracture, stable biomechanical environment, and less trauma to the local blood supply. The above-mentioned features enable the ATMFS not only to fix the fractures in anatomical position and guarantee early patient movement, but also lead to bone union eight weeks postoperatively, allowing satisfactory movement and weight loading. Based on the encouraging results of our clinical trials, we believe that ATMFS can serve as an effective means for managing acetabular fractures.
Competing Interests
The authors declare that they have no conflicting interests.
References
- 1.Letournel E, Judet R. Classification. In: Elson RA, editor. Fractures of the acetabulum. New York: Springer-Verlag; 1993. pp. 63–66. [Google Scholar]
- 2.Giannoudis PV, Grotz MR, Papakostidis C, Dinopoulos H. Operative treatment of displaced fractures of the acetabulum. A meta-analysis. J Bone Joint Surg Br. 2005;87:2–9. [PubMed] [Google Scholar]
- 3.Matta JM. Fractures of the acetabulum: Accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Joint Surg Am. 1996;78:1632–1645. [PubMed] [Google Scholar]
- 4.McLaren AC. Prophylaxis with indomethacin for heterotopic bone. After open reduction of fractures of the acetabulum. J Bone Joint Surg Am. 1990;72:245–247. [PubMed] [Google Scholar]
- 5.Levi DS, Kusnezov N, Carman GP. Smart materials applications for pediatric cardiovascular devices. Pediatr Res. 2008;63:552–558. doi: 10.1203/PDR.0b013e31816a9d18. [DOI] [PubMed] [Google Scholar]
- 6.Oh KT, Joo UH, Park GH, Hwang CJ, Kim KN. Effect of silver addition on the properties of nickel-titanium alloys for dental application. J Biomed Mater Res B Appl Biomater. 2006;76:306–314. doi: 10.1002/jbm.b.30369. [DOI] [PubMed] [Google Scholar]
- 7.Zhang CC. Design of the scorpion-like dynamic nitinol osteo-connector and its use in the treatment of fractures and the nonunion of the upper extremity tubular bones. Zhonghua Wai Ke Za Zhi. 1993;31:269–271. [PubMed] [Google Scholar]
- 8.Zhang CC, Xu SG, Yu BQ. Application of acetabular tridimensional memory fixation system (ATMFS) to treat complex acetabular fractures and its clinical significance. Chinese Journal of Orthopaedic Trauma. 2004;6:364–368. [Google Scholar]
- 9.d’Aubigne RM, Postel M. The classic: Functional results of hip arthroplasty with acrylic prosthesis. 1954. Clin Orthop Relat Res. 2009;467:7–27. doi: 10.1007/s11999-008-0572-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Letournel E. Diagnosis and treatment of nonunions and malunions of acetabular fractures. Orthop Clin North Am. 1990;21:769–788. [PubMed] [Google Scholar]
- 11.Saterbak AM, Marsh JL, Nepola JV, Brandser EA, Turbett T. Clinical failure after posterior wall acetabular fractures: The influence of initial fracture patterns. J Orthop Trauma. 2000;14:230–237. doi: 10.1097/00005131-200005000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Müller ME. The comprehensive classification of fractures of long bones, spine and pelvis. 2. Berlin: Springer; 1996. [Google Scholar]
- 13.Pantazopoulos T, Nicolopoulos CS, Babis GC, Theodoropoulos T. Surgical treatment of acetabular posterior wall fractures. Injury. 1993;24:319–323. doi: 10.1016/0020-1383(93)90055-B. [DOI] [PubMed] [Google Scholar]
- 14.Stockle U, Hoffmann R, Nittinger M, Sudkamp NP, Haas NP. Screw fixation of acetabular fractures. Int Orthop. 2000;24:143–147. doi: 10.1007/s002640000138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goulet JA, Rouleau JP, Mason DJ, Goldstein SA. Comminuted fractures of the posterior wall of the acetabulum. A biomechanical evaluation of fixation methods. J Bone Joint Surg Am. 1994;76:1457–1463. doi: 10.2106/00004623-199410000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Im GI, Shin YW, Song YJ. Fractures to the posterior wall of the acetabulum managed with screws alone. J Trauma. 2005;58:300–303. doi: 10.1097/01.TA.0000149329.86361.CE. [DOI] [PubMed] [Google Scholar]
- 17.Kapanen A, Ryhanen J, Danilov A, Tuukkanen J. Effect of nickel-titanium shape memory metal alloy on bone formation. Biomaterials. 2001;22:2475–2480. doi: 10.1016/S0142-9612(00)00435-X. [DOI] [PubMed] [Google Scholar]
- 18.Ryhanen J, Kallioinen M, Serlo W, Peramaki P, Junila J, Sandvik P, Niemela E, Tuukkanen J. Bone healing and mineralization, implant corrosion, and trace metals after nickel-titanium shape memory metal intramedullary fixation. J Biomed Mater Res. 1999;47:472–480. doi: 10.1002/(SICI)1097-4636(19991215)47:4<472::AID-JBM3>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 19.Wever DJ, Veldhuizen AG, Sanders MM, Schakenraad JM, Horn JR. Cytotoxic, allergic and genotoxic activity of a nickel-titanium alloy. Biomaterials. 1997;18:1115–1120. doi: 10.1016/S0142-9612(97)00041-0. [DOI] [PubMed] [Google Scholar]
- 20.Assad M, Lemieux N, Rivard CH, Yahia LH. Comparative in vitro biocompatibility of nickel-titanium, pure nickel, pure titanium, and stainless steel: Genotoxicity and atomic absorption evaluation. Biomed Mater Eng. 1999;9:1–12. [PubMed] [Google Scholar]
- 21.Kumar A, Shah NA, Kershaw SA, Clayson AD. Operative management of acetabular fractures. A review of 73 fractures. Injury. 2005;36:605–612. doi: 10.1016/j.injury.2004.11.022. [DOI] [PubMed] [Google Scholar]
- 22.Ebraheim NA, Patil V, Liu J, Sanford CG, Jr, Haman SP. Reconstruction of comminuted posterior wall fractures using the buttress technique: a review of 32 fractures. Int Orthop. 2007;31:671–675. doi: 10.1007/s00264-006-0246-0. [DOI] [PMC free article] [PubMed] [Google Scholar]