Abstract
Isolated subtalar disorders often require subtalar arthrodesis. In this retrospective study of 28 in situ subtalar arthrodeses reviewed with a median follow-up of 56 months (range, 20–115), the authors attempted to detail the outcomes of in situ subtalar fusion, the consequences on adjacent joints and to determine clinical or radiological factors of failure. Clinical evaluation was realised with the AOFAS (American Orthopaedic Foot and Ankle Society) ankle hindfoot score. Radiographic evaluation included assessment of hindfoot alignment, subtalar fusion and arthritic evolution in the adjacent joints. The median functional score was 76.5/94 (range, 36–94). All 28 arthrodeses achieved union. Mild arthritic changes occurred in 43–65% in the different adjacent joints. These changes were not symptomatic. Varus malunion and clinical nonunion seem to be the most important causes of failure.
Introduction
Isolated subtalar arthrodesis is now considered an effective treatment for pathology of the hindfoot including post traumatic arthritis, talocalcaneal coalition, posterior tibial tendon dysfunction, isolated subtalar joint instability or inflammatory arthritis [1, 2]. Traditionally, triple arthrodesis has been favoured because of the close relationship between subtalar and midtarsal joints. However, midtarsal joint preservation provides a more functional outcome: isolated subtalar arthrodesis conserves residual motion at the transverse tarsal joint [3, 4] and limits tarsometatarsal joint stress. It also simplifies the operative procedure and avoids midtarsal nonunion or malunion.
The purposes of this retrospective study were to specify the outcomes of isolated subtalar arthrodesis in the treatment of isolated subtalar disorder, to assess the arthritic evolution in the adjacent joints and to determine clinical or radiological factors that influence the outcome.
Materials and methods
Description of patients
Between March 1999 and January 2007, 37 consecutive isolated subtalar arthrodeses were performed in 35 adults (19 men and 16 women) who had a median age of 48 years (25–75 percentile: 33–53) at the time of the procedure. The pathological findings leading to subtalar arthrodesis included post traumatic arthritis following a fracture of the calcaneus (19 cases) or a fracture of the talus (two cases), residual talocalcaneal coalition (six cases), talar cyst (three cases), subtalar instability (two cases), flatfoot secondary to posterior tibial tendon dysfunction (two cases), residual clubfoot deformity (two cases) and inflammatory arthritis (one case). Four procedures were revision arthrodeses for failure of a previous subtalar arthrodesis. Twenty-three patients were smokers at the time of the procedure. Of these 35 patients, three patients required a secondary procedure. A patient with rheumatoid arthritis developed mid-tarsal arthritis nine months after subtalar arthrodesis and required a mid-tarsal arthrodesis. A patient who had a talar fracture also developed symptomatic ankle arthritis and required an ankle arthrodesis. A patient who had a calcaneal fracture achieved nonunion at the site of the subtalar arthrodesis and developed symptomatic ankle arthritis. He also required an ankle arthrodesis. These three patients were excluded from the analysis of the results because the outcomes assessed at final follow-up were the results of a triple arthrodesis in one case and ankle arthrodesis in two cases. Six patients (six cases) were lost to follow-up. The results were established on 26 patients (28 cases).
Operative technique
All procedures were performed under general anaesthesia. The patients were placed in a lateral position on the unaffected side and tourniquet applied to the thigh. Each patient received a prophylactic dose of intravenous antibiotics preoperatively. A lateral approach was used through a horizontal incision from one centimetre behind the tip of the fibula to the lateral border of the extensor digitorum brevis. Care was taken to avoid the peroneal tendons and the sural nerve, especially in patients who had had previous open reduction and internal fixation of a calcaneal fracture. Capsular tissue was removed to expose the subtalar joint. A lamina spreader was used to improve visualisation of the subtalar joint. The residual cartilage and sclerotic subchondral bone of the talar and calcaneal joint surfaces were removed with an osteotome until a bleeding surface was achieved. Care was taken to avoid the posterior tibial neurovascular bundle. A cancellous bone graft was packed into the subtalar joint space in 33 cases (ipsilateral iliac crest autograft in 20 cases, bone graft substitute in 11 cases and allograft in two cases). The subtalar joint was reduced and the tibiocalcaneal alignment was assessed. One or two bone staples were used to fix the arthrodesis (Fig. 1). The wound was irrigated and closed in layers. A compression dressing and short leg splint were applied. Postoperative radiographs were taken. The patient was placed in a short leg non weight-bearing cast for six weeks. Check radiographs were assessed and partial weight-bearing was permitted in a short leg walking cast for an additional six weeks. Three months after the operation, the cast was removed and radiographs were taken. If union was present, full weight-bearing was permitted and rehabilitation initiated.
Fig. 1.
Talocalcaneal joint fixation with staples
Methodology
The functional results were evaluated preoperatively and postoperatively using the AOFAS (American Orthopaedic Foot and Ankle Society) ankle hindfoot rating system [5]. The six points for the subtalar motion were not assigned; the maximal score at final follow-up was 94 points. A score between 90 and 94 points was rated as excellent, good from 75 to 89, fair from 50 to 74 and poor was less than 50. The physical examination included pain assessment on sub talar stress, pain at the ankle or transverse tarsal joint and hindfoot alignment. The ankle range of motion was evaluated with a goniometer. Limitation of activities, shoe wear and patient satisfaction were assessed. Details of prominent hardware, use of walking aids, and sural nerve symptoms completed the evaluation.
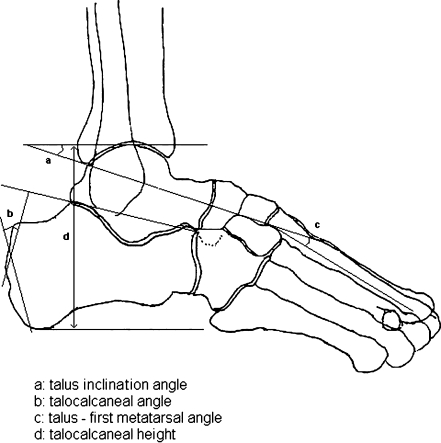
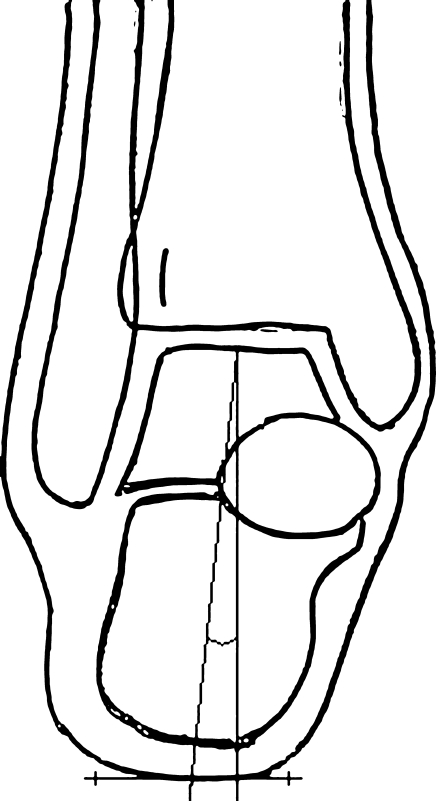
The radiographic assessment at the final follow-up included weight-bearing lateral and anteroposterior radiographs of the foot, weight-bearing anteroposterior radiograph of the ankle with metallic malleolar landmarks and dorsoplantar radiograph of the foot. The same radiographs were performed preoperatively and a CT scan was used in one third of cases to assess arthritis in the subtalar joint or to specify a talo-calcaneal coalition or a talar cyst. The bony union, the talus inclination angle, the talocalcaneal angle, the talus-first metatarsal angle and the talocalcaneal height were assessed from the lateral weight-bearing radiograph (Fig. 2). Tibiocalcaneal alignment was evaluated on the anteroposterior ankle radiograph with metallic malleolar landmarks (Fig. 3). Dorsoplantar radiograph of the foot was used to identify arthritic changes in the adjacent joints. The arthritic changes in the ankle and midtarsal joints were evaluated using the Bargon scale [6]. Grade 1 of Bargon indicated the absence of arthritic changes. Grade 2 indicated mild arthritis with subchondral sclerosis, lateral osteophytes and mild narrowing of the joint space. Grade 3 indicated severe arthritis with severe to complete narrowing of the joint space, subchondral cysts and uneven joint surfaces.
Fig. 2.
Measurements assessed on lateral weight-bearing radiograph
Fig. 3.
Evaluation of tibio calcaneal alignment on radiograph
Statistical analysis was performed with the SPSS software package v17.0 (SPSS Inc., Chicago, IL). The chi-square test and Fisher’s exact test were used to analyse qualitative data. When quantitative values were evaluated, ANOVA was performed to determine significance. A p-value of 0.05 or less was considered significant. The correlations were determined using the Pearson correlation law.
Results
The median follow-up was 56 months (25–75 percentile: 31–71). The postoperative complications included one residual varus malalignment that required a calcaneal osteotomy, four sural neuralgia, one deep infection, one deep vein thrombosis and four reflex sympathetic dystrophies. The diagnosis of reflex sympathetic dystrophy was made after a clinical evaluation of patients who presented pain and persistent skin changes. Two of four were assessed by scintigraphy. Three patients required removal of their staple.
Clinical outcomes
The median AOFAS hindfoot score improved significantly from 49 (25–75 percentile: 36–61) before to 76.5 (25–75 percentile: 67.5–82) after operation (p < 0.001). At final follow-up, the median pain score (maximum, 40 points) was 30, the median function score (maximum, 50 points) was 37 and the median alignment score (maximum, 10 points) was 10. There was no significant score variation between the different aetiologies. The objective results were excellent in two cases, good in 15, fair in ten and poor in one. Subjectively, 19 patients were satisfied without reservation, four were satisfied with reservations and three were not satisfied. Pain was absent in five cases, occasional in 19 and daily in four. There was pain with stress at the site of subtalar arthrodesis in two cases, at the mid-tarsal joint in five and at the ankle joint in one. All 26 patients had a stable hindfoot subjectively and clinically. Nineteen patients felt they had no limitation of their daily activities. Six had some mild limitation of daily activities and four used a cane. One patient had severe limitation of daily activities. In addition, 11 of 26 patients felt they had no limitation of recreational activities. Residual ankle and hindfoot oedema was present in seven cases. Thirteen patients continued to wear larger shoes after the correction. Three patients needed orthopaedic shoes. The median ankle dorsiflexion was 7.5° (25–75 percentile: 0–10) and the median ankle plantar flexion was 35° (25–75 percentile: 25–42.5).
Bony union
All 28 arthrodeses achieved bony union in a median time of 13 weeks (25–75 percentile: 12–14). A total bony fusion was achieved in 21 cases. The remaining seven cases had persistent images of incomplete fusion on the final radiographs without clinical evidence of nonunion (pain or mobility at the site of subtalar arthrodesis).
Bone graft was used in 26 of 28 cases. A cancellous autograft (iliac crest) was used in 16 cases, bone substitute in eight and cancellous allograft in two. We did not detect any significant relationships between the type of bone graft and the rate of radiological fusion or the time to union (Table 1).
Table 1.
Rate of radiological fusion and median time to union (25–75 percentile) according to type of bone graft
| Type of bone graft | Number of cases | Rate of complete radiological fusion | Time to union (weeks) |
|---|---|---|---|
| None | 2 | 0 | |
| Cancellous autograft | 16 | 13 (81%) | 13 (12–16) |
| Bony substitute | 8 | 6 (75%) | 13 (11–15) |
| Cancellous allograft | 2 | 2 (100%) | 13 |
| p-value | 0.07 | 0.79 |
Patients who were smokers at the time of surgery achieved union in a median time of 13 weeks (25–75 percentile: 12–16). Five of 21 (24%) had an incomplete bony fusion on radiographs. Non smokers achieved union in a median time of 13 weeks (25–75 percentile: 12–15). Two of seven (29%) had an incomplete bony fusion on radiographs.
Radiological findings
Preoperatively, six patients had 15° of hindfoot valgus or more, and three had at least 5° of hindfoot varus. Postoperatively, 12 patients had at least 10° of hindfoot valgus and the median AOFAS score was 74 (25–75 percentile: 62–76). Fifteen patients had less than 10° of hindfoot valgus and the median AOFAS score was 80 (25–75 percentile: 76–82). One patient had 11° of hindfoot varus and the AOFAS score was 36 (p = 0.01).
The median preoperative and postoperative radiological measurements are given in Table 2.
Table 2.
Median (25–75 percentile) radiological measurements before and after correction
| Radiological measurement | Before correction | After correction | p-value |
|---|---|---|---|
| Talocalcaneal angle (°) | 40 (29–45) | 35 (23–40) | 0.09 |
| Talus declination angle (°) | 18 (11–23) | 14 (9.5–18) | 0.09 |
| Talus-first metatarsal angle (°) | 7 (0–12) | 11 (3–17) | 0.11 |
| Talocalcaneal height (mm) | 69 (64–78) | 70 (64–80) | 0.97 |
While the talus became more horizontal, there was no loss of talocalcaneal height. There was no correlation between ankle dorsiflexion and the talus inclination angle (r = 0.01).
Arthritis increased one stage in 12 tibio-talar joints, 15 calcaneo-cuboid joints and 18 talonavicular joints. We did not detect a significant relationship between the grade of arthritis in the adjacent joints and the AOFAS hindfoot score (Table 3).
Table 3.
Median (25–75 percentile) AOFAS score according to Bargon grade of arthritis in the adjacent joints
| Joint | Grade 1 | Grade 2 | Grade 3 | p-value |
|---|---|---|---|---|
| Tibio-talar joint | 76 (74–78) | 78 (62–82) | 71 | 0.78 |
| Talonavicular joint | 76 (74–78) | 80 (65–82) | 75 (70–77) | 0.89 |
| Calcaneo-cuboid joint | 78 (76–82) | 78 (64–82) | 71 (61–75) | 0.07 |
Discussion
This retrospective study details the long-term results of in situ subtalar arthrodesis. The progression of the arthritis in the adjacent joints was frequent but not symptomatic in most cases. Bone grafting seemed to have a positive effect on achieving bony fusion. Bony union and tibiocalcaneal alignment seem to be the most important clinical factors.
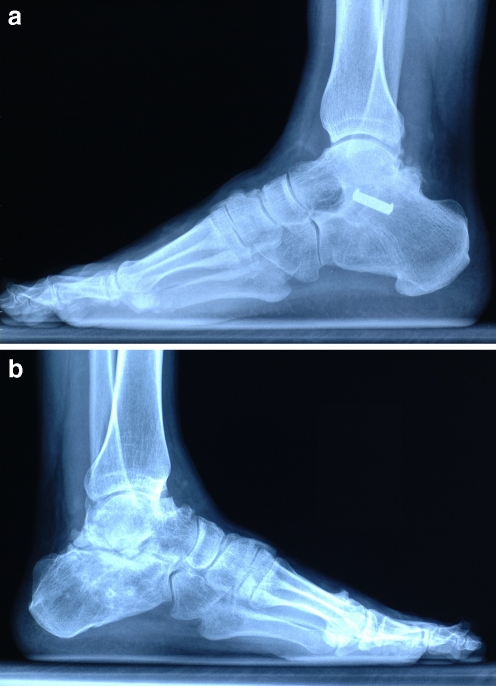
In this study, all patients achieved bony union. Most authors indicate the same results [7–10]. However, estimation of the bony union after an isolated subtalar arthrodesis is not always obvious and needs clinical and radiological examination. Indeed, there are authentic nonunions with clinical and radiographic evidence which require revision arthrodesis [1, 11–13], whereas some patients have the appearance of incomplete fusion on radiographs without clinical evidence of nonunion (Fig. 4a, b). There are not many studies that mention this matter. Easley et al. presented their experience with 184 cases and reported 23% of radiographic evidence of nonunion and 16% of associated radiological and symptomatic nonunion [1]. Davies et al., found no correlation between clinical and radiographic findings and they recommend use of a CT scan to evaluate the union rate [2]. They estimated that arthrodesis is completed when more than 50% of the posterior subtalar joint is fused on the CT scan. In their study of about 95 cases, two arthrodeses were fused despite persistent radiographic evidence of nonunion and hindfoot pain and one nonunion was found despite radiographic evidence of bony union for a patient with persistent hindfoot pain. In the same way, Jones et al. showed that standard X-rays were not sufficiently reliable to estimate the union of subtalar arthrodesis and suggested use of a CT-scan for patients with persistent hindfoot pain [14].
Fig. 4.
a Talocalcaneal arthrodesis with total bony fusion. b Talocalcaneal arthrodesis with radiographic evidence of nonunion
The effect of bone grafting on the union rate seems to be a controversial matter. Scranton recommended bone graft to avoid nonunion [15] whereas Kitaoka et al. and Tasto showed 100% union without bone grafting and considered that graft is not necessary [16, 17]. We think that bone grafting is an important factor for union because the two cases without bone graft in our series developed radiographic evidence of nonunion. Moreover, the four revision arthrodeses in this series did not receive bone grafting during the first procedure. Our statistical analysis did not find any correlation between the type of graft and the union rate or the time to union. However, Jardé et al. and McGarvey and Braly recommend using autograft [11, 12]. For Easley et al., the most important parameter to consider was the preoperative bone vascularity, and they observed that all nonunions occurred when there was more than 2 mm of avascular subchondral bone at the subtalar joint [1]. This particularly concerns arthrodesis following the failure of a previous subtalar arthrodesis or a calcaneal fracture because subchondral sclerosis is more severe [1]. This may explain the lower union rate and outcome in these cases. Soft tissue problems (peroneal and subfibular impingement, heel pad tenderness or shoe wear difficulties) may also explain why arthrodeses following calcaneal fracture have lower outcome scores [10]. Most authors insist on the need to eliminate residual cartilage and avascular bone during preparation of the bone surfaces [7, 8, 16].
In the literature, smoking seems to be a risk factor of nonunion. Easley et al. assessed 92% of bony union for nonsmokers against 73% for smokers (p < 0.01) [1]. Ishikawa et al. showed an increase of nonunion risk of about 2.7 for smokers [18]. We did not find such significant correlations in our study.
The use of staples enables a stable osteosynthesis with a union rate similar to screw fixation. Introduction of the staple can be achieved through the same surgical approach avoiding additional incisions or the use of fluoroscopy. The rate of hardware removal seems to be similar with both techniques [9, 16]. However, staple removal is sometimes more difficult.
The talocalcaneal relationship is greatly affected by a calcaneal fracture; the hindfoot alignment is modified, the talus is horizontalised and the talo-calcaneal height is decreased. Most authors agree that these anatomical modifications have biomechanical consequences and need to be corrected during subtalar arthrodesis. The talus horizontalisation results in impingement between tibial anterior rim and the talar neck [8, 19, 20]. The decrease of the talo-calcaneal height leads to a relative lengthening of the Achilles tendon and shoe wear difficulties [20, 21]. In hindfoot alignment, varus malunion is the worst deformity. In our study, the only poor result occurred in a patient with more than 10° of varus malunion; this patient required orthopaedic shoes and walking distance was less than 100 metres.
Distraction bone-block arthrodesis was first described by Gallie in 1943 [22] and was upgraded by Carr et al. in 1988 [21]. This technique permits a significant improvement of the talo-calcaneal relationship. The improvement of the talo-calcaneal height, of the talar slope and of the talo-calcaneal angle were increased from 2 to 6 mm, from 3 to 18° and from 4 to 14°, respectively [7, 8, 13, 23]. However, these anatomical improvements did not seem to have clinical benefits. Clinical outcomes obtained with distraction subtalar arthrodesis are similar to those obtained with in situ subtalar arthrodesis [7, 8, 10, 11]. Several studies did not show statistical correlation between the heel height and the global outcomes [10, 19] or between the talar slope and the ankle dorsiflexion [7, 8, 10, 23].
The physiological valgus of the calcaneus is the most important anatomical parameter of the hindfoot. Distraction is not necessary to restore this valgus. Reached through a lateral approach in lateral decubitus, distraction may cause an iatrogenic varus of the calcaneus and poor results can occur [19, 21]. Only shoe wear is regularly improved by an elevation effect of the malleolus [20]. Most of the authors do not recommend distraction routinely. Myerson and Quill claim that distraction is necessary for a loss of heel height at least 8 mm [19], whereas for Chandler, the best indication of this technique is anterior tibio-talar impingement with an ankle dorsiflexion less than 10° [10].
In our study, rate of osteoarthritis increased in 43 to 65% in the different adjacent joints but this progression was always moderate (stage 1 according to Bargon). In the literature, osteoarthritis is less common, about 10–20%, and is mostly of mild degree [8, 11, 13]. We found two patients who needed revision surgery for serious aggravation of osteoarthritis in adjacent joints. In 1997, De Heus et al. reported that the progression of osteoarthritic changes which occurred after subtalar arthrodesis appeared to be based mainly on pre-existing degeneration of adjacent joints [24]. They considered it a relative contraindication to perform subtalar arthrodesis. We did not find any correlation between arthritis severity in adjacent joints and clinical outcomes. Most authors conclude that osteoarthritis progression in the ankle or in the midfoot is not symptomatic [8, 11, 23].
Conclusion
The in situ subtalar arthrodesis permits significant clinical improvements in cases of isolated subtalar pathology. Correct hindfoot alignment is the most important parameter. This parameter depends on maintainance of the calcaneal valgus during the procedure. The increase of the osteoarthritis rate in the adjacent joints seems to be common, moderate and asymptomatic. We believe that correction of the talo-calcaneal height is not always necessary. It should be considered if the heel height is markedly decreased with shoe wear difficulty.
References
- 1.Easley ME, Trnka MD, Schon LC, Myerson MS. Isolated subtalar arthrodesis. J Bone Joint Surg Am. 2000;82(5):613–624. doi: 10.2106/00004623-200005000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Davies MB, Rosenfeld PF, Stavrou P, Saxby TS. A comprehensive review of subtalar arthrodesis. Foot Ankle Int. 2007;28(3):295–297. doi: 10.3113/FAI.2007.0295. [DOI] [PubMed] [Google Scholar]
- 3.Astion DJ, Deland JT. Motion of the hindfoot after simulated arthrodesis. J Bone Joint Surg Am. 1997;79(2):241–246. doi: 10.2106/00004623-199702000-00012. [DOI] [PubMed] [Google Scholar]
- 4.Wülker N, Stukenborg C, Savory KM, Alfke D. Hindfoot motion after isolated and combined arthrodeses : measurements in anatomic specimens. Foot Ankle Int. 2000;21(11):921–927. doi: 10.1177/107110070002101106. [DOI] [PubMed] [Google Scholar]
- 5.Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle, hindfoot, midfoot, hallux and lesser toes. Foot Ankle Int. 1994;15:349–353. doi: 10.1177/107110079401500701. [DOI] [PubMed] [Google Scholar]
- 6.Bargon G, Henkemeyer H. Ergebnisse röntgenologischer und klinischer Langzeitbeobachtungen nach operativ versorgten Läsionen der tibiofibularen Syndesmose im oberen Sprunggelenk. Fortschr Röntgenst. 1977;126:542–545. doi: 10.1055/s-0029-1230633. [DOI] [PubMed] [Google Scholar]
- 7.Amendola A, Lammens P. Subtalar arthrodesis using interposition iliac crest bone graft after calcaneal fracture. Foot Ankle Int. 1996;17(10):608–614. doi: 10.1177/107110079601701004. [DOI] [PubMed] [Google Scholar]
- 8.Rammelt S, Grass R, Zawadski T, Biewener A, Zwipp H. Foot function after subtalar distraction bone-block arthrodesis. J Bone Joint Surg Br. 2004;86:659–668. doi: 10.1302/0301-620X.86B5.14205. [DOI] [PubMed] [Google Scholar]
- 9.Huang PJ, Chen SK, Chen YW, Cheng YM, Lin SY, Hsu CY. Subtalar arthrodesis for subtalar arthritis. Kaohsiung J Med Sci. 1997;13:677–681. [PubMed] [Google Scholar]
- 10.Chandler JT, Bonar SK, Anderson RB, Davis H. Results of in situ subtalar arthrodesis for late sequelae of calcaneus fractures. Foot Ankle Int. 1999;20(1):18–24. doi: 10.1177/107110079902000104. [DOI] [PubMed] [Google Scholar]
- 11.Jardé O, Trinquier JL, Renaux P, Mauger S, Vives P. Arthrodèse sous-astragalienne pour séquelles de fracture du calcanéum: à propos de 57 cas. Rev Chir Orthop. 1994;80:728–733. [PubMed] [Google Scholar]
- 12.McGarvey WC, Braly WG. Bone graft in hindfoot arthrodesis: allograft vs autograft. Orthopedics. 1996;19(5):389–394. doi: 10.3928/0147-7447-19960501-08. [DOI] [PubMed] [Google Scholar]
- 13.Trnka HJ, Easley ME, Lam PWC. Subtalar distraction bone block arthrodesis. J Bone Joint Surg Br. 2001;83(6):849–854. doi: 10.1302/0301-620X.83B6.10537. [DOI] [PubMed] [Google Scholar]
- 14.Jones CP, Coughlin MJ, Shurnas PS. Prospective CT scan evaluation of hindfoot nonunions treated with revision surgery and low-intensity ultrasound stimulation. Foot Ankle Int. 2006;27:229–235. doi: 10.1177/107110070602700401. [DOI] [PubMed] [Google Scholar]
- 15.Scranton PE. Results of arthrodesis of the tarsus : talocalcaneal, midtarsal and subtalar joints. Foot Ankle. 1991;12(3):156–164. doi: 10.1177/107110079101200305. [DOI] [PubMed] [Google Scholar]
- 16.Kitaoka HB, Patzer GL. Subtalar arthrodesis for posterior tibial tendon dysfunction and pes planus. Clin Orthop. 1997;345:187–194. [PubMed] [Google Scholar]
- 17.Tasto JP. Arthroscopy of the subtalar joint and arthroscopic subtalar arthrodesis. Instr Course Lect. 2006;55:555–564. [PubMed] [Google Scholar]
- 18.Ishikawa SN, Murphy GA, Richardson EG. The effect of cigarette smoking on hindfoot fusions. Foot Ankle Int. 2002;23(11):996–998. doi: 10.1177/107110070202301104. [DOI] [PubMed] [Google Scholar]
- 19.Myerson M, Quill GE. Late complications of fractures of the calcaneus. J Bone Joint Surg Am. 1993;75(3):331–341. doi: 10.2106/00004623-199303000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Huang PJ, Fu YC, Cheng YM, Lin SY. Subtalar arthrodesis for late sequelae of calcaneal fractures : fusion in situ versus fusion with sliding corrective osteotomy. Foot Ankle Int. 1999;20(3):166–170. doi: 10.1177/107110079902000305. [DOI] [PubMed] [Google Scholar]
- 21.Carr JB, Hansen ST, Benirschke SK. Subtalar distraction bone block fusion for late complications of os calcis fractures. Foot Ankle. 1988;9:81–86. doi: 10.1177/107110078800900204. [DOI] [PubMed] [Google Scholar]
- 22.Gallie WE. Subastragalar arthrodesis in fractures of the os calcis. J Bone Joint Surg. 1943;25:731–736. [Google Scholar]
- 23.Burton DC, Olney BW, Horton GA. Late results of subtalar fusion. Foot Ankle Int. 1998;19(4):197–202. doi: 10.1177/107110079801900402. [DOI] [PubMed] [Google Scholar]
- 24.Heus JAC, Marti RK, Besselaar P. The influence of subtalar and triple arthrodesis on the tibiotalar joint: a long-term follow-up study. J Bone Joint Surg Br. 1997;79(4):644–647. doi: 10.1302/0301-620X.79B4.7194. [DOI] [PubMed] [Google Scholar]