Abstract
Non-union of femoral neck fractures may occur due to mechanical and biological factors. Valgus intertrochanteric osteotomy (VITO) alters hip biomechanics and enhances fracture union. The double-angled 120° plate is usually used for internal fixation of the osteotomy. It allows the osteotomy to heal with medialisation and verticalisation of the femoral shaft. This deformity causes medial ligament strain of the knee joint, genu valgum and ultimately osteoarthritis. This work presents our experience in treating vertical fractures and non-unions of the femoral neck by VITO and fixation by a single-angled 130º plate. Thirty-six patients presented with 19 recent vertical femoral neck fractures, and 17 non-unions were included. They were 26 men and ten women, and their ages averaged 37 years. Preoperative planning and VITO technique are described. Union was achieved in 35 patients (97%), and one recent fracture failed to unite (3%). Time to fracture union averaged four months in recent fractures and eight months in un-united fractures. All patients with united fractures had an almost normal configuration of the upper femur. Avascular necrosis of the femoral head was reported in five patients. Twenty-two patients (61%) were pain free, nine (25%) had hip pain on lengthy walks and the remaining five (14%) had persistent pain. Preoperative limb shortening averaged 2.5 cm, and post-operative shortening averaged 0.5 cm. We recommend VITO and fixation by a single-angled 130º plate for vertical femoral neck fractures and non-unions in relatively young adult patients.
Introduction
Femoral neck fractures in relatively young patients should be treated by reduction and rigid fixation to preserve the patient’s own hip [7, 9]. However, this treatment may result in non-union because of mechanical and biological factors [5]. Intertrochanteric osteotomy alters the biomechanical environment of the fracture site and enhances fracture union [4]. Although this procedure is well described in the orthopaedic literature [2, 12–15], many young orthopaedic surgeons may have little awareness of this procedure. This can be attributed to the recent advances in hip replacement.
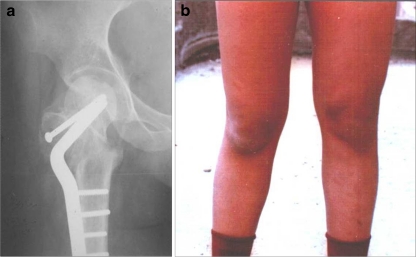
Intertrochanteric osteotomy was first introduced by Pauwels [15] in 1927. It was used as a method to treat many hip problems [1, 9–12] and succeeded in avoiding or delaying hip replacement or hip resurfacing in young patients. In vertical fractures and non-unions of the femoral neck, the osteotomy reorientates the fracture, converting shear forces at the fracture site into compressive forces, which enhances fracture healing [3, 4, 15]. Müller [13] introduced the double-angled 120° plate for internal fixation of the osteotomy. The double-angled blade plate allows the osteotomy to heal with medialisation and verticalisation of the femoral shaft (Fig. 1a). This deformity causes strain of the medial ligament of the knee joint, genu valgum and ultimately knee osteoarthritis (Fig. 1b). It also makes total hip replacement difficult if needed later on.
Fig. 1.
a. Radiograph showing valgus intertrochanteric osteotomy for non-union of neck of the right femur in a boy aged 16 years, fixed by double angled plate. The femoral shaft is medialised in relation to the lateral lip of the acetabulum and is vertically oriented. b. One year later, valgus deformity of right knee is observed
Using a single-angled plate may avoid this problem. The aim of this report is to present our experience in treating displaced vertical fractures and non-unions of the femoral neck by valgus intertrochanteric osteotomy and fixation by the single-angled 130º blade plate.
Patients and methods
This study was carried out in the authors’ institution, a university teaching hospital, between 2000 and 2007. It included 36 patients: 26 men and ten women. Their average age was 37 (18–49) years. Nineteen were recently displaced vertical fractures of the femoral neck, and 17 were un-united fractures after failed internal fixation. All patients were treated by wedge-removing valgus intertrochanteric osteotomy. The fixation device was 130° blade plate in all patients. The study was approved by the ethical committee of our institution, and all patients gave informed consent.
Osteotomy design
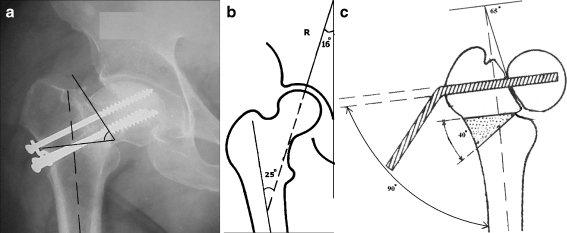
Careful preoperative planning was done in every case (Fig. 2a-c). First, the fracture angle, between the fracture plane and perpendicular to the femoral axis, is measured in a standard anteroposterior radiograph. Second, the osteotomy angle is measured (Fig. 2a). This angle is equal to the fracture angle minus 25°, which is the result of the compressive forces at the hip [13] (Fig. 2b). Third, the seating chisel insertion angle is identified, which is the angle of the blade plate (130º) minus the osteotomy angle. If the osteotomy angle is 40°, the angle between the seating chisel and the femoral shaft will be 90°. Fourth, the entry point of the seating chisel should be at least 2.5 cm above the planned upper cut of the osteotomy. Osteotomy level is at or slightly superior to the lesser trochanter level.
Fig. 2.
a Fracture angle is the angle between fracture line and perpendicular to the femoral axis measured on a standard anteroposterior radiograph. b Compressive forces at the hip (R) subtends an angle of 25º with the anatomical axis of the femur. If the fracture plane is reclined to subtend this angle with the anatomical axis of the femur, it is under pure compression. c If the osteotomy angle is 40°, the angle between the seating chisel and the femoral shaft will be 90°. The blade of the single-angled 130º plate is introduced. The side-plate now stands away from the femoral shaft, making an angle equal to the desired osteotomy angle
Blade insertion
The operation is performed on a radiolucent fracture table for fluoroscopic guidance. The seating chisel is inserted along a guide wire aiming at the inferomedial quadrant of the femoral head at the pre-templated insertion angle. Its position is checked by fluoroscopy, and then the blade of the single-angled 130º plate is introduced. The side plate now stands away from the femoral shaft, making an angle equal to the desired osteotomy angle (Fig. 2c).
Osteotomy cuts
A V-shaped wedge removing osteotomy is performed. The upper cut of the osteotomy is transverse. Correction of any external rotation or flexion deformity, sometimes present in non-union cases, is done at this stage. Then the lower cut is made, subtending the desired angle with the upper cut and meeting it at the medial surface of the femoral shaft. The separated wedge of bone is removed and used as bone graft at the osteotomy site.
Osteotomy reduction
While abducting the hip to close the osteotomy, the femoral shaft is pulled laterally and distally by a bone hook to bring it to the plate, and a clamp is applied to hold them together. The first screw along the shaft is placed obliquely parallel to the osteotomy cut. Tightening this screw helps pull the femoral shaft laterally and distally and compress the osteotomy surfaces.
Post-operative management Hip and knee range of motion and muscle strengthening exercises were instituted for the entire extremity. Touchdown weight bearing was permitted for the first six weeks after surgery, and then increased to full weight bearing according to the progress of fracture and osteotomy healing seen on the radiographs.
Follow-up After hospital discharge, patients were observed periodically every four weeks until fracture healing. Follow-up ranged between one and five (average 3.5) years.
Assessment
Fracture and osteotomy union was assessed radiographically after complete disappearance of the fracture line and the osteotomy site. Clinical union was confirmed when there was painless hip range of movement and painless full weight bearing. Functional assessment was done using subjective and objective information based on pain, limb shortening and walking ability.
Results
Fracture union and osteotomy healing Union was achieved in 35 patients (97%). One recent fracture failed to unite (3%), and also developed avascular necrosis of the femoral head after which the patient was scheduled for total hip arthroplasty. Time to fracture union ranged from two to six (average four) months in recent fractures and from four to 24 (average eight) months in un-united fractures. Healing of the osteotomy site was complete at the three months’ follow-up visit in all patients.
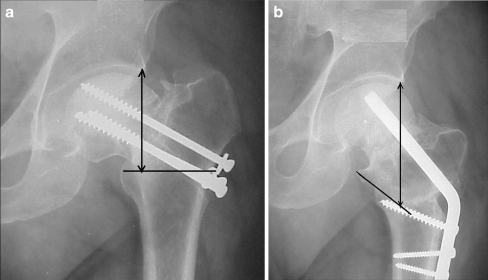
Angle of correction Preoperative fracture angle ranged from 55 to 75º (average 64º). The osteotomy angle varied from 30 to 45º (average 34º). Post-operative neck-shaft angle ranged from 125 to 160º (average 139º). The neck-shaft angle of the normal side ranged from 115 to 140º (average 131º). Patients with united fractures had an almost normal configuration of the upper femur, and the femoral shaft was normally inclined to the sagittal plane (Fig. 3).
Fig. 3.
a A radiograph showing non-union of left femoral neck fracture of a 45-year-old man 4 months after lag screw fixation. b Follow-up radiograph at 24 weeks showing healing of the non-union and osteotomy sites after valgus intertrochanteric osteotomy and single-angled 130° plate fixation. The lengthening effect of the osteotomy is demonstrated. The upper fragment is rotated clockwise, the greater trochanter is lowered and the osteotomy line becomes obliquely situated, running downwards and laterally, resulting in lengthening with restoration of the normal inclination of the femur to the sagittal plane
Complications Avascular necrosis of the femoral head was reported in five cases.
Functional outcome
Pain: Twenty-two patients (61%) were pain free at the last follow-up. Nine (25%) reported occasional hip pain without interference with their daily activities. The remaining five patients (14%), with avascular necrosis of the femoral head, had persistent hip pain.
Lengthening effect: Preoperative limb shortening averaged 2.5 cm, and post-operative shortening averaged 0.5 cm.
Walking ability: At the latest follow-up, 26 patients (72%) could walk any distance without limping. Nine patients (25%) reported limping on long-distance walking, and one patient (3%) with failed fracture union was unable to walk and was scheduled for hip arthroplasty.
Discussion
Non-union of femoral neck fractures in the young has always been challenging [5]. Arthrodesis is not accepted in those who practice squatting and sitting on the floor. Total hip replacement in the young is associated with many problems. Valgus intertrochanteric osteotomy is an alternative line of treatment for those patients [1–3, 8, 11]. Pauwels [15] and Müller [14] advised Y-shaped wedge-closing−wedge-opening osteotomy to treat pseudo-arthrosis of the femoral neck. The Y-shaped osteotomy reduces the area of contact of the osteotomy surfaces. On the other hand, simple V-shaped wedge removing osteotomy provides broad osteotomy surfaces that ensure good bony contact on closure of the osteotomy and lateralisation of the femoral shaft.
Valgus intertrochanteric osteotomy results in rotation of the upper segment of the femur in a clockwise manner for the left hip and counterclockwise for the right hip. The osteotomy line becomes obliquely situated, running downwards and laterally, and its lateral end is displaced distally, resulting in lengthening (Fig. 3). Lengthening is usually desirable to compensate for the shortening that is present in these cases [10]. The femoral shaft is now displaced medially and becomes vertically oriented after the osteotomy. Osteotomy fixation with a double-angled plate will maintain this deformed position (Fig. 1). On the other hand, fixation with a single-angled blade plate will pull the femoral shaft laterally and distally to the plate along the slope of the obliquely situated osteotomy line. This will result in correction of the medialisation of the femoral shaft and also restore the normal inclination of the femur to the sagittal plane. These effects have a positive influence on the knee joint in preventing valgus strain and overloading.
The compressive forces at the hip subtend an angle of 25º with the anatomical axis of the femur (Fig. 2b). If the fracture plane is reclined to subtend this angle with the anatomical axis of the femur, it is under pure compression [13]. Valgus reduction of vertical femoral-neck fractures is a method used to achieve this goal. Valgus over-reduction, however, may result in avascular necrosis of the femoral head due to kinking and obstruction of the postero-superior retinacular vessels. Realignment of the fracture at the intertrochanteric level by a valgus osteotomy and internal fixation provides safe, alternative stabilisation of these fractures and non-unions [1, 3, 6, 9]. In femoral neck non-unions, repositioning the osteotomy will result in union of the pseudarthrosis, even in the presence of avascular necrosis. However, the hip function may deteriorate in these cases later on [14].
The drawback of the valgus intertrochanteric osteotomy is decreasing abductor muscle efficiency and increasing the joint reactive force due to shortening of its lever arm as an effect of rotation and adduction of the upper segment of the femur. This is probably responsible, at least in part, for the persistent limp reported in 25% of our patients following the osteotomy.
In this study, we preferred the fixed single-angled blade plate to the dynamic hip screw (DHS), as it avoids reaming the femoral head and minimises the risk of avascular necrosis. It also provides good purchase when inserted in the inferomedial quadrant of the femoral head, even in the osteopoenic bone, without the risk of cutting through the femoral head. Moreover, the fixed-angle blade plate does not allow medialisation of the femoral shaft, as DHS might do through its gliding effect.
The limitations of this study are the retrospective design and lack of a control group using the double-angled osteotomy plates. However, the results of this study encourage the use of single-angled 130º plate for valgus intertrochanteric osteotomy fixation to realign vertical femoral neck fractures and non-unions in relatively young adult patients.
References
- 1.Anglen JO. Intertrochanteric osteotomy for failed internal fixation of femoral neck fracture. Clin Orthop. 1997;341:175–182. [PubMed] [Google Scholar]
- 2.Ballmer FT, Ballmer PM, Baumgaertel F, Ganz R, Mast JW. Pauwels osteotomy for non-unions of the femoral neck. Orthop Clinics North Am. 1990;21(4):759–767. [PubMed] [Google Scholar]
- 3.Ballmer FT, Ballmer PM, Mast JW, Ganz R. Results of repositioning osteotomies in delayed healing of pseudoarthrosis of the proximal femur. Unfallchirurg. 1992;95(10):511–517. [PubMed] [Google Scholar]
- 4.Brand RA. Hip osteotomies: a biomechanical consideration. J Am Acad Orthop Surg. 1997;5:282–291. doi: 10.5435/00124635-199709000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Comfort TH, Chapman MW. Nonunion and malunion of the hip. In: Chapman MW, Madison M, editors. Operative orthopaedics. 1. Philadelphia: J.B. Lippincott; 1998. pp. 555–565. [Google Scholar]
- 6.Hermichen HG, Thielemann FW, Hofler R, Weller S, Holz U. Primary valgisation osteotomy in femoral neck fractures. Aktuelle Traumatol. 1991;21(3):104–111. [PubMed] [Google Scholar]
- 7.Hernefalk L, Messner K. Rigid osteosynthesis decreases the late complication after femoral neck fracture: the influence of three different devices evaluated in 369 patients. Arch Orthop Trauma Surg. 1996;115:71–74. doi: 10.1007/BF00573444. [DOI] [PubMed] [Google Scholar]
- 8.Kalra M, Anand S. Valgus intertrochanteric osteotomy for neglected femoral neck fractures in young adults. Int Orthop. 2001;25:363–366. doi: 10.1007/s002640100288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Magua NK, Singha R, Mittala R, Garga R, Wokhlub A, Sharmaa AK. Osteosynthesis and primary valgus intertrochanteric osteotomy in displaced intracapsular fracture neck of femur with osteoporosis in adults. Injury. 2005;36:110–122. doi: 10.1016/j.injury.2004.02.017. [DOI] [PubMed] [Google Scholar]
- 10.Marti RK, Holder EJ, Kloen P. Lengthening osteotomy at the intertrochanteric level with simultaneous correction of angular deformities. Int Orthop. 2001;25:355–359. doi: 10.1007/s002640100282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marti RK, Schuller HM, Raaymakers EL. Intertrochanteric osteotomy for non-union of the femoral neck. J Bone Joint Surg Am. 1989;71(5):782–787. doi: 10.1302/0301-620X.71B5.2584247. [DOI] [PubMed] [Google Scholar]
- 12.Müller ME, Allgower M, Schneider R, Willenegger H. Manual of Internal fixation: techniques recommended by AO Group. 2. Berlin: Springer-Verlag; 1979. pp. 360–365. [Google Scholar]
- 13.Müller ME. Intertrochanteric osteotomies: indications, proper planning and technique. In: Schatzker J, editor. The intertrochanteric osteotomy. Berlin: Springer-Verlag; 1984. pp. 25–66. [Google Scholar]
- 14.Müller ME. The intertrochanteric osteotomy and pseudoarthrosis of the femoral head. Clin Orthop. 1999;363:5–8. [PubMed] [Google Scholar]
- 15.Pauwels F. Biomechanics of normal and diseased hip. Translated by Ronald J. Furlong and Paul Maquet (1976) Berlin: Springer-Verlag; 1927. [Google Scholar]