Abstract
Follow-up examinations of 45 patients who received shoulder arthroplasty for osteoarthritis following shoulder instability were conducted after 44 months. The goal of this study was to describe the clinical findings associated with advanced glenohumeral arthritis due to shoulder instability and instability repairs and to present the clinical results and complications of treating this with shoulder arthroplasty. The weighted average Constant score increased significantly from 49.4 to 81.3 points. There was no significant difference in the type of arthroplasty with 35 cases of total shoulder replacements and ten cases of hemiarthoplasty. The rate of complications was 40% (18/45 patients) with 20% (9/45 patients) requiring an operative revision. Patients with arthritis after instability repair showed great improvement in all qualities of the Constant score. Nonetheless, further analyses are required to determine why such a relatively young group of patients showed high complication rates.
Introduction
Epidemiological studies have shown an incidence of shoulder instability between 0.5 and 1.7% [1, 2] following dislocation. Simonet et al. describe an overall adjusted incidence of initial traumatic shoulder dislocation of 8.2/100,000 persons [3]. Owens et al. prospectively captured all traumatic shoulder instability events in the United States Military Academy between September 2004 and May 2005 and found 117 new traumatic shoulder instability events among 4,141 students throughout this time period with a one-year incidence of 2.8% [4]. Approximately 9% of patients with shoulder joint arthroplasty have had shoulder instability [5, 6], while prospective studies have radiologically shown arthritis in over 20% of patients with a history of shoulder dislocation [7, 8]. Marx et al. have demonstrated that the probability of developing shoulder joint arthritis requiring arthroplasty is ten times higher in patients exhibiting a history of shoulder dislocation. Following operative treatment of the instability, this probability increases 20-fold [9]. Although these facts certainly show a statistical correlation, little can be said in terms of causality.
Samilson and Prieto [10] were unable to find a correlation either between the degree of arthritis and the frequency of shoulder dislocation or the extent of initial damage to the joint surfaces in the humeral head or glenoid. Posterior instability appears solely to correlate to a higher degree of instability induced arthritis [10, 11]. Using the Bristow-Latarjet procedure [12], Hovelius et al. were able to demonstrate an arthritis rate of 35% in mild and 14% in moderate and severe cases as defined by Samilson [10].
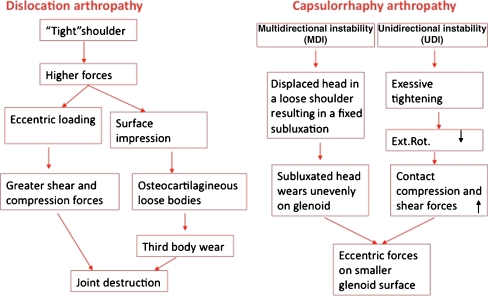
Regarding the aetiology of arthritis following instability repair, two main mechanisms—excluding direct damage resulting from metal implants—are shown schematically in Fig. 1. Both result in eccentric loads and higher compression and shearing forces [13–16]. (Fig. 2)
Fig. 1.
Etiology of arthritis following instability
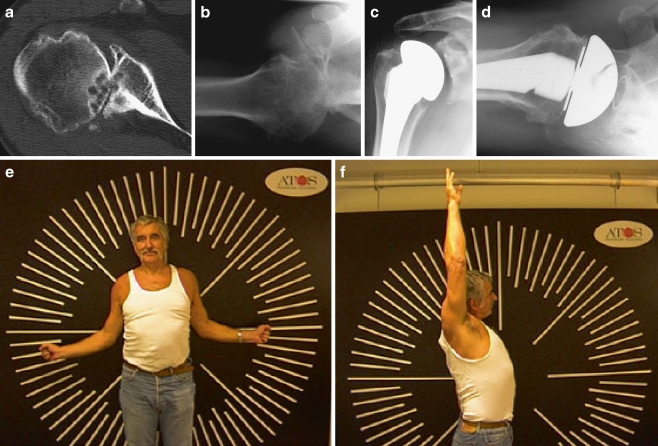
Fig. 2.
Preoperative (a, b) and postoperative (c, d) X-rays with typical posterior bony defect. The same patient two years postoperative demonstrating near normal shoulder range of motion (e, f)
The central aims of this study were to examine the long-term effects of shoulder joint arthroplasty in patients with a history of instability induced arthritis with regard to the clinical, functional and radiological results, and to evaluate the type, reasons and treatment of complications associated with this sequela of instability.
Materials and methods
We retrospectively reviewed 45 of 51 patients with osteoarthritis of the glenohumeral joint and a history of shoulder instability who underwent prosthetic replacement of the shoulder between 1999 and 2006. Six patients (11.8%) were lost to follow-up, two patients died, and four were not available for follow-up examination. Prior surgical shoulder stabilisation was performed in 21 of 45 cases including three arthroscopic stabilisation procedures, nine Eden-Hybbinette and nine open Bankart repair procedures. All patients had a single instability procedure. The mean age at the time of surgery was 55.8 years (n = 45; range 32–76 years, SD 10.553). There were 30 males and 15 females. The aetiology of the instability was traumatic in 14 and atraumatic in 29 cases, with two shoulder dislocations due to seizure. We detected seven bony Bankart lesions in these 45 cases. All fracture dislocations and cases of posterior dislocation were excluded from the study.
The diagnosis was based on clinical examination with evaluation of active ranges of motion. A radiological investigation of X-ray examinations in three planes was carried out. The radiological evaluation was performed by one reviewer (orthopaedic surgeon).
Prior to surgery, all patients underwent unsuccessful conservative treatment of physiotherapy for a minimum of six months and pain medication with non steroidal anti inflammatory drugs.
The mean time interval between last surgery and shoulder arthroplasty was 63.02 months (n = 45; range 0–288 month; SD 94.04 month). MR imaging showed an articular side, partial tear of the supraspinatus tendon in ten cases. In 35 cases there was an intact rotator cuff.
Preoperative CT scan was performed in 36 cases in order to determine the glenoid type according to Walch et al. [17], revealing seven A1 types, seven A2 types, eight B1 types, and ten B2 types. Four type C cases had a dysplastic glenoid.
Prior to the operation all patients had a severe functional disability caused by pain and limited range of motion. Thirty-five patients (77.8%) underwent total shoulder replacement, and ten patients (22.2%) underwent humeral head replacement. Among these prostheses, there were seven cemented (15.6%) and 38 uncemented stems (84.4%) as well as four cemented glenoids (8.9%) and 31 uncemented glenoids (91.1%).
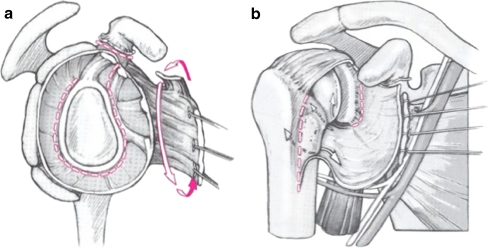
Following general anaesthesia we used the deltopecoral approach. The deltoid and pectoralis major muscles were retracted. In an external rotation position the lateral border of the subscapularis tendon was identified just medial to the bicipital groove. The subscapularis muscle was entirely released from the rotator interval below the level of the anterior circumflex vessels continuing along the humeral shaft in order to perform a complete capsular release on the humeral side anterior and inferiorly (Fig. 3). This step is necessary in order to create a sufficient visualisation and for the preparation of the glenoid bone.
Fig. 3.
Bifocale capsulotomy according to Habermeyer
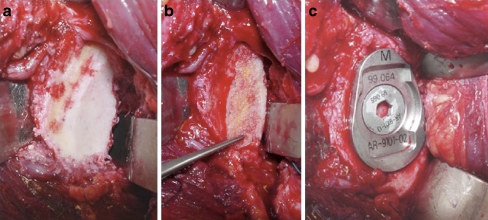
Glenoid preparation was performed to alter the posterior wear in one case with a posterior bone graft (Fig. 4) or with anterior shaping of the glenoid. In one case an additional coracoid transfer was performed to restore stability.
Fig. 4.
Bone grafting in a case with posterior bony defect. The hollow screw of the cementless glenoid component fixes the bone graft
Contraction of the anterior capsule and the subscapularis was addressed by bifocal capsulotomy, according to circumstances, and by the preoperative mobility by appropriate lengthening of the subscapularis tendon (Fig. 3).
All index arthroplasty procedures and revision procedures were performed by the same surgeon (H.P.).
Postoperative rehabilitation Immediately following surgery, the joint was immobilised for three weeks by means of an abduction pillow. During the first three weeks, passive mobilisation was restricted to 30° abduction, 30° flexion, 60° internal and 0° external rotation. By the end of the sixth week, the range of motion was increased to 60° abduction, 90° flexion and 60° internal rotation. Following the seventh week, the patients were allowed to freely move their shoulders following careful strengthening if the pain was tolerable.
Follow-up evaluation The follow-up was performed after a mean of 44 months (range 12–101 months, n = 45). All patients with complications came back for follow-up. The patients were clinically evaluated using the Constant score (CS) and the age and gender adjusted Constant score system according to Katolik et al. [18, 19]. Standard radiography including a true anterioposterior (AP), an outlet, and an axillary view in order to detect radiolucent lines around the stem and the glenoid and to detect concentric or eccentric glenoid abrasion was attempted.Complications occurred in 40% of the patients (n = 18/45). Nine patients were treated conservatively. Among those, five patients (11.1%) displayed clinically asymptomatic radiolucency lines. One patient (1/45; 2.2%) showed clinical signs of instability without dislocation of the shoulder arthroplasty; hence, he could be treated conservatively. Three patients (3/45; 6.67%) had a subsequent rotator cuff tear but did not require surgical revision after successful conservative treatment with physiotherapy and muscle strengthening. In a total of nine cases (n = 9/45; 20%) a second operation was required, and in three of these nine cases a second revision. One patient developed a postoperative frozen shoulder after three months and a posterior PE abrasion of the glenoid component with subsequent loosening of the stem that required a complete revision arthroplasty after 38 months. The same patient suffered from a further glenoid loosening that required a second revision of the uncemented glenoid component to a cemented glenoid.There were six cases (n = 6/45, 13.3%) of abrasive wear of the posterior glenoid. In three of those cases (n = 3/45; 6.67%), due to posterior instability, exchange of the glenoid component was required with a posterior capsular shift after 14, 42 and 62 months, respectively. One of these patients sustained a breakout of the uncemented glenoid after 84 months that required a further revision of the glenoid component to a cemented glenoid component.One patient showed an exostosis on the anterior glenoid that required removal of this exostosis after 24 months. Sixty-nine months after the index arthroplasty procedure a glenoid component was implanted due to painful glenoid erosion.One patient with anterior bone loss of the glenoid and shoulder instability was treated with a shoulder arthroplasty and coracoid transfer. After 16 months a breakout of the anterior screw occurred, which was treated by a “ream and run” [20] technique of the glenoid in order to create stability of the shoulder arthroplasty.Fifty months after the index arthroplasty procedure one patient showed an anterior inferior dislocation with rotator cuff tear and dislocation of the PE component of the uncemented glenoid. A revision procedure was performed to exchange the PE insert and a rotator cuff repair (Table 1).
Table 1.
Complications after arthroplasty due to shoulder instability
| Complications | Treated conservatively | Treated operatively | Asymptomatic |
|---|---|---|---|
| Radiolucency | 5 | ||
| Rotator cuff tear | 3 | ||
| Instability without dislocation | 1 | ||
| Glenoid PE wear | 6 | ||
| Exostosis | 1 (with second revision) | ||
| Anterior bone loss | 1 (with second revision) | ||
| Stem loosening | 1 (with second revision) |
Statistical analysis We used SPSS version 13.0 (SPSS Inc., Chicago, Illinois). The level of significance was set at p < 0.05. Pre- and postoperative nonparametric data (Constant score, Range of motion) were compared using the Wilcoxon signed-rank test. Differences in the Constant scores were analysed for the groups with and without complications and between patients that were treated conservatively before and those that were stabilised before prosthetic replacement.
Results
Clinical
The mean Constant score increased significantly (p < 0.0001) from 40.9 points (range 12.6–75 points; adjusted CS 49.4) to 65.7 points (range 36.2–95.5 points; adjusted CS 81.3 ± 36 ) 44 months postoperatively. The patients showed a significant improvement in the level of pain (p < 0.0001), activities of daily living (p < 0.0001), and active range of motion (p < 0.006), but not in strength of abduction. The abduction strength averages increased—but not statistically significantly—from 6.1–7.8 points (p = 0.221).
Evaluation of the range of motion showed a significant increase in active flexion from 114° (range 20–170°) to 140° (range 40–180° ; p = 0.023) and in abduction from 88° (range 20–170°) to 125° (range 40–170°; p < 0.0001). A significant gain in active external rotation (p < 0.0001) was seen from 31° (range −10° to 75°) to 44° (range 10–80°; p = 0.016).
There were no differences in outcome between patients that were treated conservatively and those that were stabilised before prosthetic replacement (p > 0.05).
Analysis of the postoperative radiographs in 35 cases showed concentric glenoid wear in 17 and eccentric glenoid wear in 18 cases.
A statistical comparison of the groups with and without complications showed better results for the group without complications in respect of the Constant score (71.4 vs 84.7; p = 0.059), postop range of motion (23.8 points vs 29.4 points; p = 0.062) and postop external rotation (33.9° vs 47.3°; p = 0.048).
Discussion
Several factors have been described as related to inferior functional outcome after shoulder arthroplasty [21]. Scarring of the normally mobile soft tissue limits motion and can lead to nerve injuries, muscle dehiscence and wound infection. Hardware complications, such as those from metal anchor systems, can badly damage the cartilage surface of the humeral head [13].
Non anatomical surgical procedures that cause internal rotation contracture have a poor effect on humeral biomechanics [14, 15]. Therefore, Lusardi et al. consider an anterior release in patients who have a major loss of external rotation following anterior capsulorhaphy [16].
Young et al. described the complications of the Bristow procedure including recurrent painful anterior instability, injury to the articular cartilage, failure of the coracoid bone-block to unite with the glenoid, loosening of the screw, neurovascular injury, and posterior instability [22].
This mechanically-changed biomechanics can furthermore affect the outcome of shoulder arthroplasty. Probably the effects of previous operations were the major factors in this regard.
Shoulder arthroplasty in cases of instability-induced arthritis shows significantly more complications such as instability, loosening, and decreased range of motion than in cases of idiopathic osteoarthritis [21, 23–26]. According to Neer et al. [6, 27], approximately 7% of all shoulder arthroplasties are based on arthritis after instability repair. Norris has shown similar figures with an additional 5% of patients displaying previous anterior instability. This study reveals the largest number of cases to date and similar clinical results to other studies. For example, Matsoukis et al. found an increase of the CS from 30.8 to 65.8 points in follow-up examinations after 45 months [24]. Our examination also revealed an improvement in the unweighted CS [18] from the albeit higher initial level of 40.9 to a similar level of 65.7 points postoperatively.
Osteoarthritis of the shoulder resulting from instability is relatively rare and not frequently published, nevertheless one has to approach this problem carefully due to the young age of affected patients. While the average age in this study was 56 years, Sperling et al. [23] reported an average of 46 years, Green and Norris [21] an average of 45 years, and Bigliani et al. [25]] an average age of 43 years. As a comparison, in a large, French, multicentre study of 689 shoulder arthroplasties, Edwards et al. [28] reported an average age of 67 years. Consequently, if one considers the Kaplan Meyer curves in shoulder arthroplasties, it becomes evident that these special problems require other procedures and solutions [28–30].
One such example is soft tissue balancing in cases of internal rotation contractures, and another is the necessity for bone restoration in the common case of glenoid defects resulting from the posterior subluxation of the humeral head. However, anterior defects resulting from chronic dislocations—especially in elderly patients—have also been described [31]. We believe that an improvement in external rotation is of critical importance in order to avoid a postoperative posterior subluxation with eccentric abrasion. Generally this requires an elongation of the subscapularis using either Matsen′s 360° method, a Z-plasty, or Habermeyer′s bifocal capsule splitting (Fig. 3). Although the first method can cause a postoperative weakness in internal rotation, we share the opinion of Green and Norris that regaining active external rotation and active abduction is more important, especially, long term [21].
Subscapularis tendon plication or incision techniques may impair subscapularis recovery and can negatively influence the final clinical outcome [32], Z-plasty or intraarticular lengthening can weaken the tendon and lead to subsequent postoperative subscapularis tear.
The bone defects in the glenoid generally require glenoid replacement. A survey of available literature has shown a ratio of 1 to 3 for hemi and total arthroplasty, which is comparable to the ratio in this study (1 to 3.5).
This is commonly accompanied by a posterior bone graft (Fig. 4) or anterior shaping of the edge of the glenoid. The altered glenoid anatomy can potentially lead to a lateralisation, resulting in further reduction of external rotation. Although technically difficult and laborious, bone grafting has shown positive long-term results. For example, using a follow-up period of 70 months, Hill and Norris were able to demonstrate a reliable correction of the glenoid version of an average of 33° in 17 cases [33]. As a result, we consider a CT scan imperative for preoperative planning.
The importance of the glenoid becomes evident when one examines the subset of patients with idiopathic osteoarthritis and a concentric glenoid, which displayed better clinical outcomes [17, 34].
Significantly higher complication rates were shown than in the cases of idiopathic osteoarthritis. The revision rate found in available literature ranged from 20–33%. This study had an overall rate of complication of 40%, with a revision rate of 20%.
Advanced glenohumeral osteoarthritis can be a result of shoulder instability. The probability of clinical manifestation increases following stabilising operations, with extra anatomical methods posing an additional risk [4, 14, 15, 22]. However, even this aetiology can lead to excellent clinical results, especially in terms of pain reduction [21, 24].
Acknowledgments
Conflict of interest statement The authors have no conflicts of interest.
Footnotes
Level of evidence: IV
References
- 1.Hovelius L (1982) Incidence of shoulder dislocation in Sweden. Clin Orthop Relat Res 127–131 [PubMed]
- 2.Hovelius L. The natural history of primary anterior dislocation of the shoulder in the young. J Orthop Sci. 1999;4:307–317. doi: 10.1007/s007760050109. [DOI] [PubMed] [Google Scholar]
- 3.Simonet WT, Melton LJ 3rd, Cofield RH, Ilstrup DM (1984) Incidence of anterior shoulder dislocation in Olmsted County, Minnesota. Clin Orthop Relat Res 186–191 [PubMed]
- 4.Owens BD, Duffey ML, Nelson BJ, DeBerardino TM, Taylor DC, Mountcastle SB. The incidence and characteristics of shoulder instability at the United States Military Academy. Am J Sports Med. 2007;35:1168–1173. doi: 10.1177/0363546506295179. [DOI] [PubMed] [Google Scholar]
- 5.Gartsman GM, Roddey TS, Hammerman SM. Shoulder arthroplasty with or without resurfacing of the glenoid in patients who have osteoarthritis. J Bone Joint Surg Am. 2000;82:26–34. doi: 10.2106/00004623-200001000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Neer CS, 2nd, Watson KC, Stanton FJ. Recent experience in total shoulder replacement. J Bone Joint Surg Am. 1982;64:319–337. [PubMed] [Google Scholar]
- 7.Hindmarsh J, Lindberg A. Eden-Hybbinette′s operation for recurrent dislocation of the humero-scapular joint. Acta Orthop Scand. 1967;38:459–478. doi: 10.3109/17453676708989654. [DOI] [PubMed] [Google Scholar]
- 8.Hovelius L, Augustini BG, Fredin H, Johansson O, Norlin R, Thorling J. Primary anterior dislocation of the shoulder in young patients A ten-year prospective study. J Bone Joint Surg Am. 1996;78:1677–1684. doi: 10.2106/00004623-199611000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Marx RG, McCarty EC, Montemurno TD, Altchek DW, Craig EV, Warren RF. Development of arthrosis following dislocation of the shoulder: a case-control study. J Shoulder Elbow Surg. 2002;11:1–5. doi: 10.1067/mse.2002.119388. [DOI] [PubMed] [Google Scholar]
- 10.Samilson RL, Prieto V. Dislocation arthropathy of the shoulder. J Bone Joint Surg Am. 1983;65:456–460. [PubMed] [Google Scholar]
- 11.Gavriilidis I, Magosch P, Lichtenberg S, Habermeyer P, Kircher J. Chronic locked posterior shoulder dislocation with severe head involvement. Int Orthop. 2009 doi: 10.1007/s00264-009-0762-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hovelius L, Akermark C, Albrektsson B, Berg E, Korner L, Lundberg B, Wredmark T. Bristow-Latarjet procedure for recurrent anterior dislocation of the shoulder. A 2–5 year follow–up study on the results of 112 cases. Acta Orthop Scand. 1983;54:284–290. doi: 10.3109/17453678308996571. [DOI] [PubMed] [Google Scholar]
- 13.Zuckerman JD, Matsen FA., 3rd Complications about the glenohumeral joint related to the use of screws and staples. J Bone Joint Surg Am. 1984;66:175–180. [PubMed] [Google Scholar]
- 14.Hawkins RJ, Angelo RL. Glenohumeral osteoarthrosis. A late complication of the Putti-Platt repair. J Bone Joint Surg Am. 1990;72:1193–1197. [PubMed] [Google Scholar]
- 15.MacDonald PB, Hawkins RJ, Fowler PJ, Miniaci A. Release of the subscapularis for internal rotation contracture and pain after anterior repair for recurrent anterior dislocation of the shoulder. J Bone Joint Surg Am. 1992;74:734–737. [PubMed] [Google Scholar]
- 16.Lusardi DA, Wirth MA, Wurtz D, Rockwood CA., Jr Loss of external rotation following anterior capsulorrhaphy of the shoulder. J Bone Joint Surg Am. 1993;75:1185–1192. doi: 10.2106/00004623-199308000-00008. [DOI] [PubMed] [Google Scholar]
- 17.Walch G, Badet R, Boulahia A, Khoury A. Morphologic study of the glenoid in primary glenohumeral osteoarthritis. J Arthroplast. 1999;14:756–760. doi: 10.1016/S0883-5403(99)90232-2. [DOI] [PubMed] [Google Scholar]
- 18.Constant CR. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214(160–4):160–164. [PubMed] [Google Scholar]
- 19.Katolik LI, Romeo AA, Cole BJ, Verma NN, Hayden JK, Bach BR. Normalization of the Constant score. J Shoulder Elbow Surg. 2005;14:279–285. doi: 10.1016/j.jse.2004.10.009. [DOI] [PubMed] [Google Scholar]
- 20.Matsen FA 3rd, Bicknell RT, Lippitt SB (2007) Shoulder arthroplasty: the socket perspective. J Shoulder Elboow Surg 16(5 Suppl):S241–S247 [DOI] [PubMed]
- 21.Green A, Norris TR. Shoulder arthroplasty for advanced glenohumeral arthritis after anterior instability repair. J Shoulder Elbow Surg. 2001;10:539–545. doi: 10.1067/mse.2001.118007. [DOI] [PubMed] [Google Scholar]
- 22.Young DC, Rockwood CA., Jr Complications of a failed Bristow procedure and their management. J Bone Joint Surg Am. 1991;73:969–981. [PubMed] [Google Scholar]
- 23.Sperling JW, Antuna SA, Sanchez-Sotelo J, Schleck C, Cofield RH. Shoulder arthroplasty for arthritis after instability surgery. J Bone Joint Surg Am. 2002;84-A:1775–1781. doi: 10.2106/00004623-200210000-00006. [DOI] [PubMed] [Google Scholar]
- 24.Matsoukis J, Tabib W, Guiffault P, Mandelbaum A, Walch G, Nemoz C, Edwards TB. Shoulder arthroplasty in patients with a prior anterior shoulder dislocation. Results of a multicenter study. J Bone Joint Surg Am. 2003;85-A:1417–1424. doi: 10.2106/00004623-200308000-00001. [DOI] [PubMed] [Google Scholar]
- 25.Bigliani LU, Weinstein DM, Glasgow MT, Pollock RG, Flatow EL. Glenohumeral arthroplasty for arthritis after instability surgery. J Shoulder Elbow Surg. 1995;4:87–94. doi: 10.1016/S1058-2746(05)80060-6. [DOI] [PubMed] [Google Scholar]
- 26.Aldinger PR, Raiss P, Rickert M, Loew M. Complications in shoulder arthroplasty: an analysis of 485 cases. Int Orthop. 2009 doi: 10.1007/s00264-009-0780-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Neer CS, 2nd, Morrison DS. Glenoid bone-grafting in total shoulder arthroplasty. J Bone Joint Surg Am. 1988;70:1154–1162. [PubMed] [Google Scholar]
- 28.Edwards TB, Kadakia NR, Boulahia A, Kempf JF, Boileau P, Nemoz C, Walch G. A comparison of hemiarthroplasty and total shoulder arthroplasty in the treatment of primary glenohumeral osteoarthritis: results of a multicenter study. J Shoulder Elbow Surg. 2003;12:207–213. doi: 10.1016/S1058-2746(02)86804-5. [DOI] [PubMed] [Google Scholar]
- 29.Deshmukh AV, Koris M, Zurakowski D, Thornhill TS. Total shoulder arthroplasty: long-term survivorship, functional outcome, and quality of life. J Shoulder Elbow Surg. 2005;14:471–479. doi: 10.1016/j.jse.2005.02.009. [DOI] [PubMed] [Google Scholar]
- 30.Torchia ME, Cofield RH, Settergren CR. Total shoulder arthroplasty with the Neer prosthesis: long-term results. J Shoulder Elbow Surg. 1997;6:495–505. doi: 10.1016/S1058-2746(97)90081-1. [DOI] [PubMed] [Google Scholar]
- 31.Raiss P, Aldinger PR, Kasten P, Rickert M, Loew M. Humeral head resurfacing for fixed anterior glenohumeral dislocation. Int Orthop. 2009;33:451–456. doi: 10.1007/s00264-007-0487-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Scheibel M, Habermeyer P. Subscapularis dysfunction following anterior surgical approaches to the shoulder. J Shoulder Elbow Surg. 2008;17:671–683. doi: 10.1016/j.jse.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 33.Hill JM, Norris TR. Long-term results of total shoulder arthroplasty following bone-grafting of the glenoid. J Bone Joint Surg Am. 2001;83-A:877–883. [PubMed] [Google Scholar]
- 34.Edwards TB, Boulahia A, Kempf JF, Boileau P, Nemoz C, Walch G. Shoulder arthroplasty in patients with osteoarthritis and dysplastic glenoid morphology. J Shoulder Elbow Surg. 2004;13:1–4. doi: 10.1016/j.jse.2003.09.011. [DOI] [PubMed] [Google Scholar]