Abstract
The purposes of this study were to investigate the mode of failure and survivorship of an independently performed series of medial Oxford unicompartmental knee arthroplasties. The study included 43 knees in 40 patients with a mean follow-up of 14.88 years: 13 knees (11 patients) had revision surgery (30%), and ten patients required conversion to total knee prosthesis. The mean International Knee Society (IKS) scores at the time of the revision were 145.52 [standard deviation (SD): 39.90, range: 167–200]. The overall alignment of the knee was restored to neutral, with a hip-knee-ankle (HKA) angle average of 178° (SD: 3.21°, range: 170–186°). Survivorship, as defined by an endpoint of failure for any reason, showed that the survival rate at five years was 90%, at ten years 74.7% and at 15 years 70%. Excluding inappropriate patient selection and surgeon-associated failures, our survival analysis plot is much improved: survivorship at five years is 94.5%, at ten years 85.7% and at 15 years 80.4%. The Oxford meniscal bearing arthroplasty offers long-term pain relief with good knee function. Unfortunately, we demonstrated a high complication rate, with some of the failures encountered indicating that the surgical technique is very demanding.
Introduction
Unicompartmental knee arthroplasty (UKA) is one of the main treatment options for isolated medial tibiofemoral osteoarthritis. The advantages of this implant include a faster and better functional recovery than total knee arthroplasty [10, 21] and less morbidity due to minimal postoperative blood loss, smaller incision and less soft tissue damage. In addition, it seems logical to replace only the damaged compartment of the knee. Nowadays, the indications, contraindications and surgical techniques for UKA are well defined.
The Oxford implant uses a fully congruent mobile bearing tibial implant in an attempt to achieve congruency between the articulating surfaces throughout the range of motion.
The designers reported a 98% survival rate at ten years and encouraging clinical outcome scores for a small series of prostheses beyond ten years [15, 25]. However, some independent studies have shown less favourable implant survival, casting doubts as to the efficacy and reliability of the device [11, 14].
The purpose of this study was to present the clinical and radiological results of 43 Oxford UKA (Phase II implants, Biomet, Warsaw, IN, USA) and compare them with those in the literature. We also analysed the survivorship and modes of failure.
Materials and methods
From 1988 to 1994, 59 consecutive medial compartment Oxford Phase II implants (Biomet, Warsaw, IN, USA) were placed in 55 patients by the senior author (DS). We excluded five patients (six knees) because they were lost to follow-up and nine patients who were deceased (nine knees) with follow-up less than two years. At final follow-up, 40 patients (43 knees) remained and thus were included. There were 23 right (65%) and 20 left (45%) knees on 16 (40%) female and 24 (60%) male patients. The average age at the time of surgery was 68.83 years (SD: 7.54 years, range: 47–86 years) and the mean body mass index (BMI) was 28.28 (SD: 4.03, range: 25–35). There were 37 unilateral procedures and three staged bilateral procedures. Four patients (10%) had had previous knee surgery: three had a meniscectomy and one a high tibial osteotomy.
Indications for the initial UKA were medial compartment osteoarthritis in 39 knees (91%), medial femoral condyle osteonecrosis in three cases (7%) and arthritis in one knee (2%). Fibrillation or marginal erosions of the lateral compartment and patellofemoral osteoarthritis of any severity did not constitute a contraindication.
For the 43 knees, the mean preoperative alignment was 171.25° (SD: 3.21°, range: 166–180°), and the mean preoperative International Knee Society (IKS) score was 52.79 points (SD: 18.16, range: 5–85) for function score, 54.67 points (SD: 10.55, range: 34–75) for knee score and 106.72 points (SD: 25.19, range: 30–155) for global score.
Of the 40 patients (43 knees), 14 died and five were too ill to attend for follow-up. In these cases we used hospital and local doctors’ records to establish the status of every implant at the time of the patient’s death. All remaining patients were reviewed clinically and radiologically by an independent observer. We used the IKS score to evaluate the functional results [6].
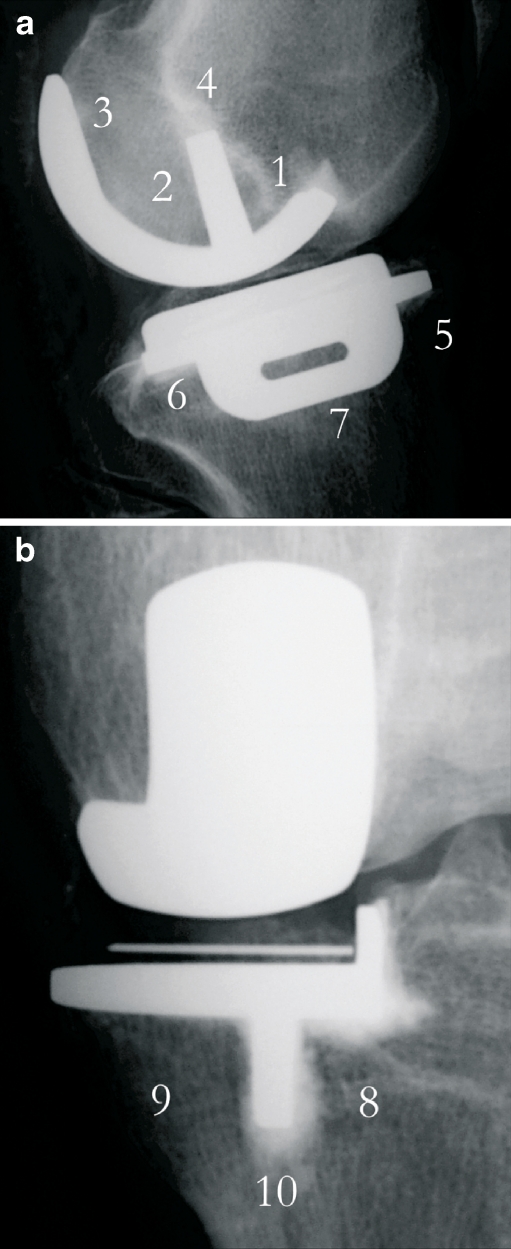
The radiological results were evaluated using weight-bearing anteroposterior (AP) and lateral views as well as skyline views. All radiographs were assessed by one of the authors (NM) for the presence of arthritis in the retained compartments, evidence of component subsidence or loosening, evidence of osteolysis, polyethylene (PE) wear and the presence of any radiolucency around the metal components. Arthritis in the lateral and patellofemoral compartments was graded using the Ahlbäck system [1]. Radiolucency around the tibial or femoral component was evaluated in terms of thickness and positioning. Thickness of radiolucency was graded as follows: grade 1 was radiolucency less than 2 mm, grade 2 was over 2 mm and grade 3 was radiolucency plus change of component positioning. The anatomical area of radiolucency was also noted for each component (Fig. 1a, b). Alignment was evaluated on weight-bearing X-rays taken three months postoperatively. These long-leg films were not repeated prior to revision surgery.
Fig. 1.
a, b Zones of radiolucency around components (AP and lateral)
All revisions and reoperations are reported in this study. Revision was defined as any surgical procedure that resulted in the removal or exchange of any of the prosthetic components. The indications for revision or reoperation, the findings at surgery and the eventual outcome also are reported.
All clinical and radiographic data were collected retrospectively. Preoperative and postoperative alignment was analysed statistically using Student’s t test. For all tests a p value of <0.05 was considered significant. Survivorship analysis was calculated using the Kaplan-Meier method. Using revision of the prosthesis for any cause as the endpoint (including any patients who were on the waiting list for revision), a life table was constructed and the one- to 15-year survival rates were determined.
Results
At the time of the final follow-up of the original series, 40 patients (43 knees) were included. Fourteen patients (15 knees) had died with the prosthesis intact. These 14 patients had been followed for an average of 10.53 years (SD: 4.16 years, range: 1–18 years) prior to death. Eleven patients (11 knees) had revision surgery (30%) and ten of them required conversion to total knee replacement (TKR) at an average of 6.28 years (SD: 3.71 years, range: 0.8–13.9 years). The remaining 15 patients (17 knees) continued to function at the time of the latest follow-up. This final group of living patients had an average duration of follow-up of 14.88 years (SD: 1.16 years, range: 13–17 years). Of these patients, five had no recent follow-up radiograph and they were contacted by telephone. None of the contacted patients reported any changes in implant function.
Failures
There had been 13 revision operations (11 patients) in the total group of 43 knees (30%) (Table 1). Ten patients that had undergone revision arthroplasty underwent conversion to total knee prosthesis. One patient only required change of the UKA polyethylene bearing. The mean time until revision was 6.28 years (range: 0.8–13.9 years). Early failures (less than five years) included four patients (six failures): two tibial loosenings, one recurrent dislocation of the meniscal bearing (twice in the same patient) and one anterior impingement between the bony femoral condyle and the meniscal bearing (twice in the same patient). Intermediate failures (five to ten years) included six patients (six failures): one tibial loosening, one radiolucency (grade 2) on the femoral component, one implant fracture and three cases of osteoarthritis progression. Late failures (over ten years) included one patient (one failure): a case of femoral component fracture with polyethylene wear. At the time of study completion, no patients were awaiting revision surgery.
Table 1.
Details of the 13 revision procedures
| Cases | Time to revision (years) | Indication for revision | Operative findings | Procedure |
|---|---|---|---|---|
| 1 | 1 | Chronic pain | Anterior impingement | First: open bearing exchange |
| 2 | Second: change of bearing (10 years later) | |||
| 3 | 1 | Tibia loosening | Tibia loosening + dislocation of PE | TKA |
| 4 | 1 | Dislocation of meniscal bearing + ACL rupture | Dislocation of meniscal bearing | First: change of PE T7 by T8 |
| 5 | Second: TKA (PCL retaining + metallic wedge 1 month later) | |||
| 6 | 5 | Tibia loosening + ACL rupture (HKA = 174°) | Tibia loosening + PE wear | TKA |
| 7 | 6 | Arthritis in lateral compartment (HKA = 186°) | Arthritis + tibia loosening | TKA |
| 8 | 6 | Fracture of femoral component + PE wear (HKA = 180°) | Fracture of femoral component + PE wear | TKA |
| 9 | 6 | Arthritis in lateral compartment (HKA = 184°) | Arthritis | TKA |
| 10 | 7 | Loose tibial component (HKA = 177°) | Loose tibial component | TKA |
| 11 | 8 | Radiolucencies on femoral component (HKA = 171°) | Loose femoral component + PE wear | TKA |
| 12 | 9 | Arthritis in lateral compartment (HKA = 184°) | Arthritis | TKA |
| 13 | 14 | Fracture of femoral implant + PE wear | Fracture of femoral implant + PE wear | TKA |
PE polyethylene, TKA total knee arthroplasty, ACL anterior cruciate ligament, HKA hip-knee-ankle
Functional results
The mean preoperative IKS score was 106.72 points (SD: 25.19, range: 30–155). The mean immediate postoperative IKS score was 189.67 points (SD: 14.43, range: 115–120). The improvement was statistically significant (p < 0.0001).
The mean IKS scores at the time of the latest follow-up were 145.52 points (SD: 39.90, range: 167–200) for global score, 61.17 points (SD: 34.43, range: 0–100) for function score and 89.05 points (SD: 15.85, range: 49–100) for knee score. Of the 15 patients (17 knees) that were reviewed, four patients were rated excellent by the IKS score groupings (IKS > 170 points), four patients were rated as having a good result (IKS between 140 and 170 points), two patients a medium result (IKS between 120 and 140 points) and five patients had a poor result (IKS < 120 points).
Pain was improved (p < 0.01) after surgery and this was maintained at revision surgery. At 14 years follow-up, 56% (nine patients) of patients were pain free and 19% (three patients) reported only mild pain. Three patients (three knees, 19%) reported moderate pain.
The mean flexion at the time of revision was 113.21° (SD: 14.59°, range: 90–140°). No significant extension lag was noted.
We then analysed the patients’ subjective evaluation of the prosthesis: at the time of the revision one patient was very satisfied, ten satisfied, three moderately satisfied and one dissatisfied.
Radiological assessment
To assess varus/valgus deformity, the hip-knee-ankle (HKA) was measured. All knees were in varus before the operation: 171.25° (SD: 3.21°, range: 166–180°). Postoperatively, the mean HKA was 178.03° (SD: 3.21°, range: 170–186°). The radiographs showed that 27 knees (65%) were in varus of between 176 and 180°, eight knees (19%) a varus angulation between 171 and 175° and one knee (2%) a varus angulation of 170°. Lastly, seven knees (14%) had a valgus deformity (greater than 180°). There was a correlation between the postoperative valgus angle and the extension of osteoarthritis in the lateral compartment (p = 0.005).
We then studied the progression of the osteoarthritis. The radiographic review at the time of final follow-up showed that nine knees had evidence of arthritis in the retained compartments. Most lesions (six knees) in retained compartments were Ahlbäck grade I. Of the three patients (six knees) who had Ahlbäck grade II or grade III changes, all had reported knee pain, and their results were considered as a failure (revision to TKR). Thirteen knees had arthritic changes in the patellofemoral joint and were not considered as a failure.
Twelve knees (28%) had radiolucencies around one or both components (Table 2). On the femoral side, with four zones for analysis, only two components had a radiolucent line (5%). One component had a grade 1 (zone 3) radiolucent line in one zone and the other a grade 2 (zones 2 and 3). Around the tibial component, with six zones for analysis, ten components had a radiolucent line (23%). Four were grade 1, three grade 2 and three complete loosening (with evidence of implant position change) (Fig. 2). The most common location for lucencies was zone 10.
Table 2.
Details of radiolucencies and loosening
| Cases | Location | Grade | Zone | Time (years) | Outcome |
|---|---|---|---|---|---|
| 1 | Tibia | Loosening | 5 | TKA | |
| 2 | Tibia | 1 | 9 | 9 | Dead |
| 3 | Tibia | 1 | 8, 10 | 9 | Dead |
| 4 | Tibia | 2 | 8, 9 | 6 | Dead |
| 5 | Tibia | 1 | 8, 10 | 8 | Dead |
| 6 | Tibia | 2 | 10 | 14 | TKA |
| 7 | Tibia | Loosening | 7 | TKA | |
| 8 | Tibia | Loosening | 1 | TKA | |
| 9 | Tibia | 2 | 9, 10 | 6 | TKA |
| 10 | Femur | 2 | 2, 3 | 8 | TKA |
| 11 | Femur | 1 | 3 | 8 | Stationary |
| 12 | Tibia | 1 | 9 | 13 | Stationary |
TKA total knee arthroplasty
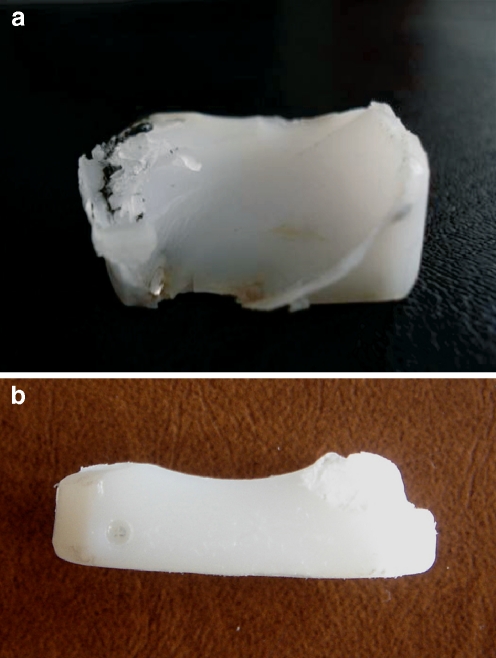
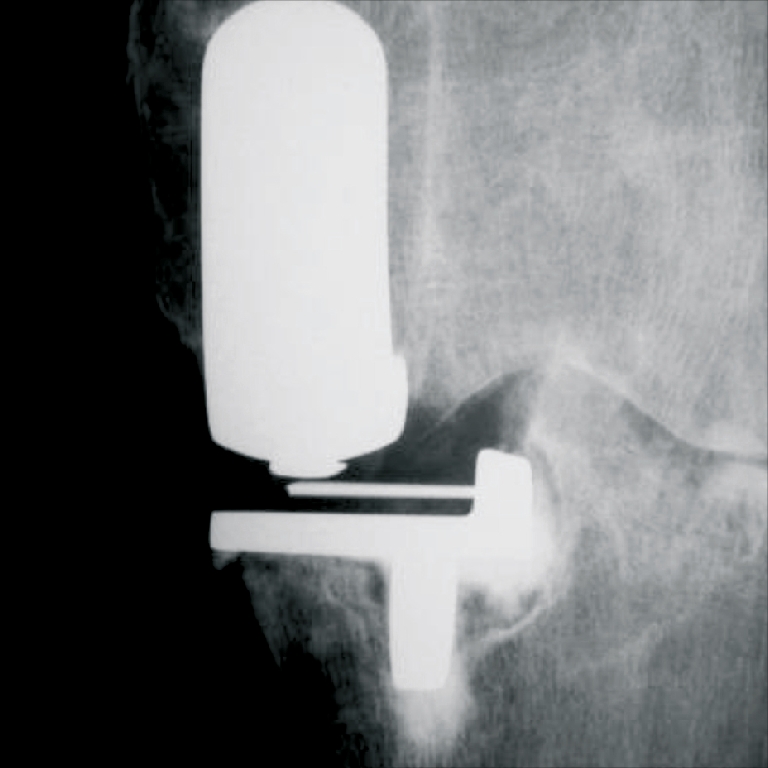
Fig. 2.
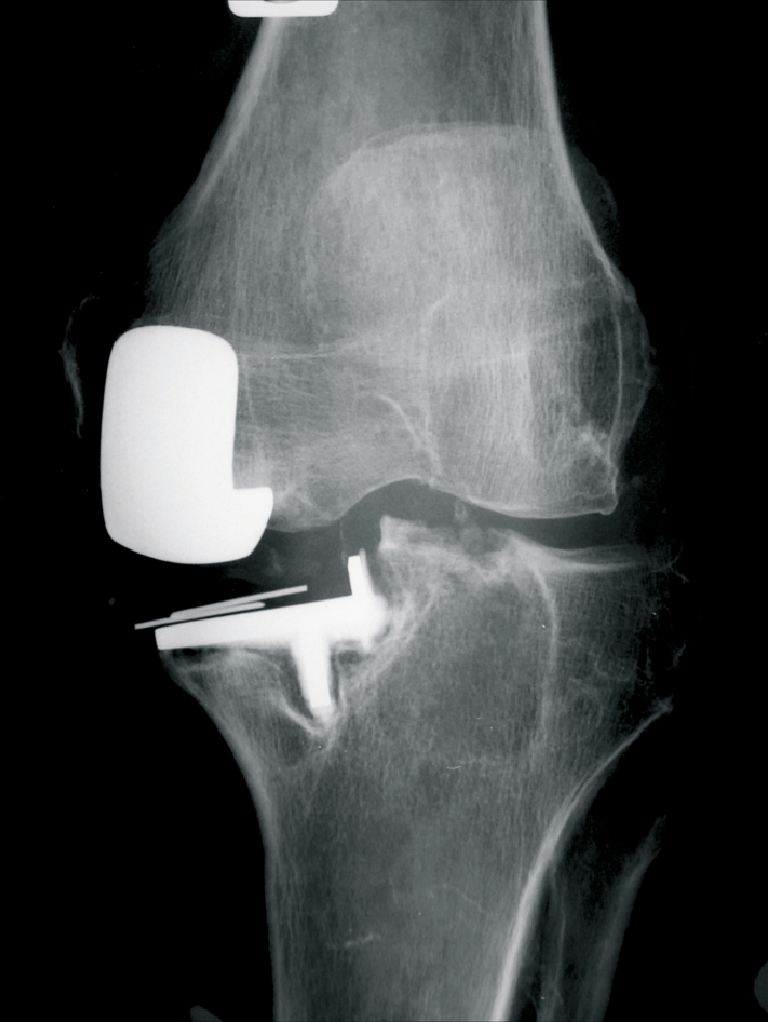
Loosening of tibial component with migration
We also found evidence of polyethylene wear in eight knees. The global wear was 3.25 mm (range: 1–3 mm). Six knees with polyethylene wear had been revised to TKR. Of the eight knees, we noted that most of them had significant wear (Fig. 3a, b) and that there was only one case of dislocation and two cases of osteoarthritis progression.
Fig. 3.
a Wear of meniscal bearing. b Wear of the anterior and posterior edge of meniscal bearing (anterior and posterior impingement)
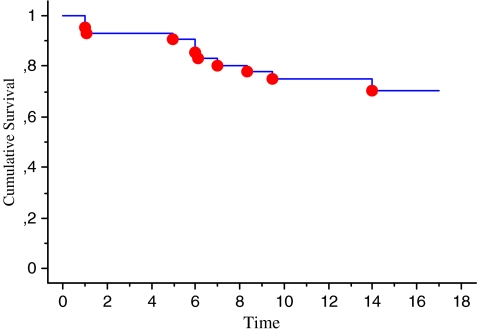
Survival analysis
With use of the Kaplan-Meier method, survivorship at one year was 93%, at five years 90.5%, at ten years 74.7% (number at risk at ten years was 24) and at 15 years was 70.1% (number at risk at 15 years was eight) with revision surgery for any reason as the endpoint (Fig. 4).
Fig. 4.
Survivorship curve with failure for any reason. The calculation includes 36 knees, 24 at 10 years and 8 patients at 15 years
Discussion
The Oxford knee arthroplasty for the treatment of medial osteoarthritis of the knee remains controversial due to excellent results reported by the designers and poor results by surgeons (Table 3). Appropriate patient selection and good surgical technique are the key factors in producing good results, according to the designers.
Table 3.
Outcome studies for Oxford unicompartmental knee arthroplasty
| Year | Authors | Compartment | Number | Survival at 10 years (%) (95% CI) | Survival at 15 years (%) (95% CI) |
|---|---|---|---|---|---|
| 1995 | Lewold et al. (Swedish) [13] | Medial/lateral | 699 | ? | |
| 1998 | Murray et al. [15] | Medial | 144 | 98 (93–100) | |
| 1999 | Kumar [11] | Medial | 100 | 85 (77–92) | |
| 2001 | Svärd and Price [23] | Medial | 124 | 95 | |
| 2003 | Lidgren [14] | Medial | 749 | 86 (76–89) | |
| 2004 | Keys et al. [8] | Medial | 40 | 95 | |
| 2004 | Rajasekhar et al. [19] | Medial | 135 | 94 (84–97.8) | |
| 2005 | Price et al. [18] | Medial | 439 | 93 (89–89) | 93 (84–100) |
| 2005 | Skowronski et al. [22] | Medial | 42 | 86 | |
| 2006 | Vorlat et al. [24] | Medial | 149 | 82 | |
| 2007 | Koskinen et al. (Finnish) [9] | Medial/lateral | 1,145 | 81 (72–89) | |
| 2008 | Emerson and Higgins [4] | Medial | 55 | 85 | |
| 2008 | Robertsson and Lidgren (Sweden) [20] | Medial/lateral | 1,758 | ? |
CI confidence interval
We analysed all of our failures in this study in order to determine if the unicompartmental knee replacement (UKR) is subject to a long learning curve, if inappropriate implants or patients were selected or if the prosthesis is flawed when not being implanted by the surgeons involved in its design. We decided to divide the failures into three categories: aseptic loosening, surgeon-associated failures and implant-associated failures.
Aseptic loosening or radiolucencies grade 2 represented 31% of the indications for revision. Three cases were on the tibial side (three loosenings) and one on the femoral side (grade 2). The mean time to revision was 5.25 years (range: one to eight years). The causes were as follows: bone dystrophy (one case), knee instability because of anterior cruciate ligament (ACL) deficiency (one case) and too much undercorrection (174°) of HKA (one case). In one case, no cause was diagnosed and the prosthesis was well positioned. The prosthetic loosening, in our series, therefore was due to inappropriate case selection in three cases.
The experience of the surgeon plays an important role in the survival of the prosthesis. Indeed, the low experience of the surgeon is a factor for failures with a high revision rate if less than 23 UKRs are implanted per year [13]. The most obvious surgeon-associated failure is progression of arthritis in the lateral compartment. This failure, which is commonly due to the overcorrection, should never occur as a direct result of the operation. The mean time to revision was seven years. In all cases, the knees were overcorrected. None of them occurred within five years, whereas relatively rapid deterioration leading to revision has been seen in other series and has been attributed to overcorrection of the varus deformity [5, 12, 25]. Kennedy and White [7] have shown that the best results occur when alignment is slightly undercorrected. The reason why knees are overcorrected is to achieve stability of the mobile bearing. There is a tendency to use the largest possible bearing, with the potential unintentional consequence of overcorrecting the knee into valgus alignment. The worst situation is represented when the varus is low with an over-reducibility of the deformity. Another failure identified in our study was a case of polyethylene liner impingement upon the femoral bearing, which occurred in full extension. This diagnosis was not made radiologically, but clinically in a patient who at revision surgery was found to have the liner impinging on the anterior femoral cortex in full extension. We postulate that this was due to bilateral genu recurvatum. Similarly, we also report a recurrent dislocation of the mobile bearing in a patient with an ACL-deficient knee. We acknowledge that this failure is likely to be due to inappropriate patient selection (ACL-deficient knee), particularly as the time to failure was only one year. Lewold et al. [13] documented, in the Swedish Register, 16 dislocations attributed to malposition of the components and soft tissue imbalance with subsequent maltracking of the meniscal bearing. The consequence of the study by Lewold et al. was the recommendation that all surgeons undergo specific training on the Oxford knee surgical technique. In a separate study from Sweden, Svärd and Price [23] reported only three dislocated bearings in 124 knees with a ten-year survivorship of 95%.
Sometimes, failure may be due to the implant (design, materials or manufacture). Failure of the implant was a rare cause of revision. It occurred twice. The first case was perforation of the femoral component articular surface by the peg six years after surgery (Fig. 5). In this case, we hypothesise that this was as a result of a manufacturing defect. The second case was a transverse fracture through the central section of the femoral implant 13 years after surgery. Once again, this was likely to be due to a manufacturing defect. No such implant failures were reported by the Oxford team. Price et al. [17] reported a failure of the meniscal bearing and Kumar [11] a fracture of the tibial component.
Fig. 5.
Femoral implant fracture (peg failure)
We would like to mention the incidence of radiolucent lines under the tibial tray. The designers demonstrated recently [16] that their incidence of radiolucent zones at one year was as high as 75%. In contrast, only 23% of the tibial implants in our study showed up a lucent line. One of the reasons for this discrepancy, however, may be that the Oxford group used extremely precise fluoroscopically assisted radiography to look for zones of lucency, whereas our images were standard AP and lateral views. The other reason may be that we used a different technique for cementing [3]. Despite the potentially significant finding of frequent lucencies, more than three quarters of our cases did not have visible lucent zones at either short- or long-term follow-up, and even in those cases which did show up lucent zones, these did not progress so long as the implant was not malpositioned.
Our survivorship at five years was 90.5%, at ten years 74.7% and at 15 years 70.1%. These are much less than that reported by the designers and the difference was statistically significant (log rank test, p = 0.1). Our survivorship at five years is included in the result range: 85% [2] to 97.7% [15]. Unfortunately, at ten years our results are inferior to those of other studies: 81% [9] to 97.7% [15]. Our relatively poor results are explained by inappropriate patient selection in three cases (one inflammatory arthropathy and two ACL-deficient knees). The other reason was possibly due to the difficulty in recreating the desired HKA angle, resulting in overcorrection and accelerating progression of arthritis in the lateral compartment in three cases. Excluding inappropriate patient selection and surgeon-associated failures, our survival analysis plot is much improved: survivorship at five years is 94.5%, at 10 years 85.7% and at 15 years 80.4%. This greatly reinforces the current evidence that patient selection and good surgical technique are fundamental for prosthesis survival.
In conclusion, the Oxford meniscal bearing arthroplasty offers long-term relief from pain with good knee function in the treatment of medial osteoarthritis of the knee. In our series, however, we report a high failure rate. Had we applied strict exclusion criteria, the results may have been better (ACL-deficient knee and a case of bone dystrophy). Nonetheless, some of our failures indicate that the surgical procedure is technically challenging, in particular the overcorrection of the knee axis; it was very hard to control the undercorrection, ligamentous tension and the stability of the meniscal bearing. We conclude that a learning curve is needed (all the overcorrections were at the beginning of the study) and particular attention must be directed to the technical aspects of the surgery, and in particular to patient selection, both of which are vital for implant longevity.
Footnotes
Reprints: Dominique Saragaglia, address above.
References
- 1.Ahlbäck S. Osteoarthrosis of the knee. A radiographic investigation. Acta Radiol Diagn (Stockh) 1968;Suppl 277:7–72. [PubMed] [Google Scholar]
- 2.Argenson JN. Biomechanical study of the Oxford knee prosthesis with mobile meniscus (in French) Chirurgie. 1993;119:268–272. [PubMed] [Google Scholar]
- 3.Clarius M, Hauck C, Seeger JB, James A, Murray DW, Aldinger PR (2009) Pulsed lavage reduces the incidence of radiolucent lines under the tibial tray of Oxford unicompartmental knee arthroplasty: pulsed lavage versus syringe lavage. Int Orthop published online 14 Feb 2009 [DOI] [PMC free article] [PubMed]
- 4.Emerson RH, Jr, Higgins LL. Unicompartmental knee arthroplasty with the oxford prosthesis in patients with medial compartment arthritis. J Bone Joint Surg Am. 2008;90:118–122. doi: 10.2106/JBJS.F.00739. [DOI] [PubMed] [Google Scholar]
- 5.Insall J, Aglietti P. A five to seven-year follow-up of unicondylar arthroplasty. J Bone Joint Surg Am. 1980;62:1329–1337. [PubMed] [Google Scholar]
- 6.Insall J, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13–14. [PubMed] [Google Scholar]
- 7.Kennedy WR, White RP. Unicompartmental arthroplasty of the knee. Postoperative alignment and its influence on overall results. Clin Orthop Relat Res. 1987;221:278–285. [PubMed] [Google Scholar]
- 8.Keys GW, Ul-Abiddin Z, Toh EM. Analysis of first forty Oxford medial unicompartmental knee replacement from a small district hospital in UK. Knee. 2004;11:375–377. doi: 10.1016/j.knee.2004.03.007. [DOI] [PubMed] [Google Scholar]
- 9.Koskinen E, Paavolainen P, Eskelinen A, Pulkkinen P, Remes V. Unicondylar knee replacement for primary osteoarthritis: a prospective follow-up study of 1,819 patients from the Finnish Arthroplasty Register. Acta Orthop. 2007;78:128–135. doi: 10.1080/17453670610013538. [DOI] [PubMed] [Google Scholar]
- 10.Kozinn SC, Scott RD. Surgical treatment of unicompartmental degenerative arthritis of the knee. Rheum Dis Clin North Am. 1988;14:545–564. [PubMed] [Google Scholar]
- 11.Kumar M. Medial unicompartmental arthroplasty of the knee. Knee. 1999;6:21–23. doi: 10.1016/S0968-0160(98)00006-4. [DOI] [Google Scholar]
- 12.Laskin RS. Unicompartmental tibiofemoral resurfacing arthroplasty. J Bone Joint Surg Am. 1978;60:182–185. [PubMed] [Google Scholar]
- 13.Lewold S, Goodman S, Knutson K, Robertsson O, Lidgren L. Oxford meniscal bearing knee versus the Marmor knee in unicompartmental arthroplasty for arthrosis. A Swedish multicenter survival study. J Arthroplasty. 1995;10:722–731. doi: 10.1016/S0883-5403(05)80066-X. [DOI] [PubMed] [Google Scholar]
- 14.Lidgren L (2003) Swedish Knee Arthroplasty Register: 2002 annual report. www.ort.lu.se/knee
- 15.Murray DW, Goodfellow JW, O’Connor JJ. The Oxford medial unicompartmental arthroplasty: a ten-year survival study. J Bone Joint Surg Br. 1998;80:983–989. doi: 10.1302/0301-620X.80B6.8177. [DOI] [PubMed] [Google Scholar]
- 16.Pandit H, Jenkins C, Beard DJ, Gallagher J, Price AJ, Dodd CAF, Goodfellow JW, Murray DW. Cementless Oxford unicompartmental knee replacement shows reduced radiolucency at one year. J Bone Joint Surg Br. 2009;91:185–189. doi: 10.1302/0301-620X.91B2.21413. [DOI] [PubMed] [Google Scholar]
- 17.Price AJ, Dodd CA, Svard UG, Murray DW. Oxford medial unicompartmental knee arthroplasty in patients younger and older than 60 years of age. J Bone Joint Surg Br. 2005;87:1488–1492. doi: 10.1302/0301-620X.87B11.16324. [DOI] [PubMed] [Google Scholar]
- 18.Price AJ, Waite JC, Svard U. Long-term clinical results of the medial Oxford unicompartmental knee arthroplasty. Clin Orthop Relat Res. 2005;435:171–180. doi: 10.1097/00003086-200506000-00024. [DOI] [PubMed] [Google Scholar]
- 19.Rajasekhar C, Das S, Smith A. Unicompartmental knee arthroplasty. 2- to 12-year results in a community hospital. J Bone Joint Surg Br. 2004;86:983–985. doi: 10.1302/0301-620X.86B7.15157. [DOI] [PubMed] [Google Scholar]
- 20.Robertsson O, Lidgren L. The short-term results of 3 common UKA implants during different periods in Sweden. J Arthroplasty. 2008;23:801–807. doi: 10.1016/j.arth.2007.07.011. [DOI] [PubMed] [Google Scholar]
- 21.Rougraff BT, Heck DA, Gibson AE. A comparison of tricompartmental and unicompartmental arthroplasty for the treatment of gonarthrosis. Clin Orthop Relat Res. 1991;273:157–164. [PubMed] [Google Scholar]
- 22.Skowronski J, Jatskewych J, Dlugosz J, Skowronski R, Bielecki M. The Oxford II medial unicompartmental knee replacement. A minimum 10-year follow-up study. Ortop Traumatol Rehabil. 2005;7:620–625. [PubMed] [Google Scholar]
- 23.Svärd UC, Price AJ. Oxford medial unicompartmental knee arthroplasty. A survival analysis of an independent series. J Bone Joint Surg Br. 2001;83:191–194. doi: 10.1302/0301-620X.83B2.10966. [DOI] [PubMed] [Google Scholar]
- 24.Vorlat P, Verdonk R, Schauvlieghe H. The Oxford unicompartmental knee prosthesis: a 5-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2000;8:154–158. doi: 10.1007/s001670050206. [DOI] [PubMed] [Google Scholar]
- 25.Weale AE, Murray DW, Crawford R, Psychoyios V, Bonomo A, Howell G, O’Connor J, Goodfellow JW. Does arthritis progress in the retained compartments after ‘Oxford’ medial unicompartmental arthroplasty? A clinical and radiological study with a minimum ten-year follow-up. J Bone Joint Surg Br. 1999;81:783–789. doi: 10.1302/0301-620X.81B5.9197. [DOI] [PubMed] [Google Scholar]