Abstract
The purpose of this study was to report the management and outcome of 11 patients presenting with chronic Achilles tendon (AT) rupture treated by a modified flexor hallucis longus (FHL) transfer. Seven patients presented with a neglected AT rupture, one with a chronic AT rupture associated with Achilles tendinosis and three with an AT re-rupture. AT defect after fibrosis debridement averaged 7.4 cm. In addition to FHL transfer, we performed an augmentation using the two remaining fibrous scar stumps of the ruptured AT. Functional assessment was performed using the AOFAS score and isokinetic evaluation was performed to assess ankle plantarflexion torque deficit. Follow-up averaged 79 months. Functional outcome was excellent with a significant improvement of the AOFAS score at latest follow-up. No re-rupture nor major complication, particularly of wound healing, was observed. All patients presented with a loss of active range of motion of the hallux interphalangeal joint without functional weakness during athletic or daily life activities. Isokinetic testing at 30 degrees/second and 120 degrees/second revealed a significant average decrease of 28 ± 11% and 36 ± 4.1%, respectively, in plantarflexion peak torque. Although strength deficit persisted at latest follow-up, functional improvement was significant without morbidity due to FHL harvesting. For patients with chronic AT rupture with a rupture gap of at least 5 cm, surgical repair using FHL transfer with fibrous AT stump reinforcement achieved excellent outcomes.
Introduction
Achilles tendon (AT) rupture is a common sports injury with an increasing incidence, predominantly in middle-aged patients (75% in the range of 30–40 years) [16]. Although clinical examination is sufficient to diagnose AT rupture after injury, about 10–25% of acute ruptures remain initially undiagnosed [3, 23]. The management of chronic AT ruptures is usually different from that of acute ruptures as tendon ends are retracted and atrophied with short fibrous distal stumps. Moreover, expected outcome after chronic AT rupture treatment could not match the results had the repair been performed at the acute stage and depended on the extent of the gap between tendon ends and potential for muscle recovery [19].
Many procedures have been described in the literature for chronic AT rupture reconstruction with different local autologous material such as the gastrocnemius soleus complex with V-Y myotendinous advancement [1] or a “turn-down” of proximal AT tissue described by Bosworth [2]. Other surgical techniques used tendon transfer of peroneus brevis (PB) [22], flexor digitorum longus (FDL) [17] or flexor hallucis longus (FHL) [10] tendon. All these surgical procedures have been shown to yield satisfactory clinical results, although ankle plantar flexion strength and peak torque deficits persisted [1, 2, 10, 17, 21, 24].
The purpose of this series was to report the management of 11 patients presenting with chronic AT rupture and treated by a modified FHL transfer performed with transfer augmentation using the two remaining fibrous scar Achilles’ stumps and to report their midterm outcome with particular attention on the ankle plantar flexion torque deficit assessed using isokinetic evaluation.
Materials and methods
Patients
A series of 11 patients (seven men, four women) treated by a modified FHL transfer for chronic AT rupture by a single senior surgeon at our institution from April 2002 to January 2005 was reviewed. Each patient had a chronic AT rupture, whereby all Achilles tears were diagnosed and/or treated more than three months after the index lesion. The average age of patients at surgery was 44 years (range, 27–70). The average body mass index (BMI) was 25.8 kg/m² (range, 21–38). The average pre-operative American Orthopedic Foot and Ankle Society (AOFAS) score was 64/100 (range, 58–80) [14].
Nine patients practised sports requiring push-off strength: jogging, handball, tennis, judo, soccer, gymnastics or mountaineering. There were six left and five right tendons involved, and no bilateral cases. Seven patients were treated operatively for chronic AT rupture: in five cases, the initial diagnosis of acute rupture was missed, and in two cases brace treatment had been inadequate. For one patient, chronic rupture was associated with Achilles tendinosis. In this case, there was a partial rupture followed by complete AT insertion avulsion. Three cases were re-ruptures: two patients had been treated by classical end-to-end tendon surgical suture and one patient by percutaneous surgery with the Tenolig system (FH Orthopedics S.A.S., Heimsbrunn, France.).
Surgical procedure
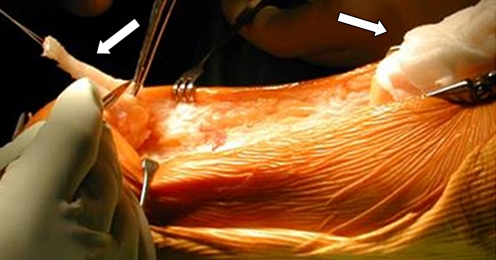
All patients underwent the same surgical procedure by a single senior surgeon (JLB). The surgical procedure was similar to one described previously by Hansen et al. [10] and modified by Wapner et al. [26]. Surgery was performed under general anaesthesia, in a prone position. A tourniquet was applied to the thigh rather than to the calf to avoid tethering the gastrocnemius-soleus complex which would prevent the proximal stump from being pulled distally. After usual antiseptic preparation, the limb was draped in a sterile field. A strict posterior approach was made with a longitudinal skin incision. After sural nerve location, the paratenon was incised. Tenolysis was performed and the AT was inspected. Debridement of tendon fibrosis was then performed with conservation of a distal and a proximal fibrous flap (Fig. 1). The average AT defect after fibrosis debridement was 7.4 cm (range, 2.5–10).
Fig. 1.
Chronic ruptured Achilles tendon after tenolysis and debridement of tendon fibrosis with conservation of distal and proximal fibrous flaps (arrows)
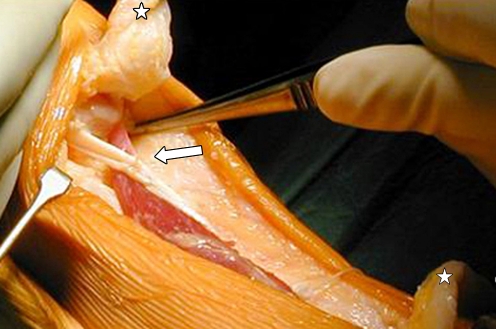
After incision of the deep fascia of the leg and having located and retracted the posterior tibial bundle, the FHL muscle belly and tendon were identified and isolated. To harvest the distal portion of the FHL, a second short medial arch incision was performed. The flexor digitorum longus (FDL) tendons were identified and connections between FHL and FDL were freed. Occasional adherences with quadratus plantae were discovered and freed if necessary. FHL tendon was sectioned distally at the Henry’s knot and was pulled out using the posterior approach. A transverse 4.5-mm drill tunnel was made in the posterior calcaneal cortex. The FHL tendon was pulled mediolaterally through the tunnel. Next, the FHL tendon was tenodesed to itself with a tension fixed at 40° of plantar flexion (Fig. 2). Augmentation with suture of two remaining Achilles fibrous flaps and fixation on FHL transfer was made (Fig. 3). The paratenon was repaired to help maintain the blood supply to the tendon. Wound closure was performed carefully to avoid subsequent skin necrosis. Patients were placed in a non-weight bearing below-knee cast in plantar flexion for three weeks and in a neutral position for three weeks. Six weeks postoperatively, a rehabilitation program for weight bearing, strengthening and range of motion was begun. Athletic activities were restricted for six months after surgery.
Fig. 2.
The flexor hallucis longus (FHL) tendon was pulled mediolaterally through a calcaneal transverse 4.5-mm drill tunnel and sutured to itself at 40° of plantar flexion (arrow indicates FHL tendon transfer; stars show the AT fibrous flaps)
Fig. 3.
Augmentation with suture of the two remaining Achilles fibrosis flaps and fixation on flexor hallucis longus (FHL) transfer
Outcome assessment at latest follow-up
Postoperative complications were recorded. The intervals to work and sports recovery were assessed.
All patients underwent clinical examination to assess gait, surgical wound, pain, ankle range of motion, tip-toe stance, calf atrophy, first metatarsophalangeal joint and hallux interphalangeal join active plantar flexion and ankle plantar flexion strength. Clinical examination was performed by an independent surgeon (JW). Functional outcome was evaluated using AOFAS score [14].
An isokinetic assessment was performed using a Con-Trex dynamometer (Con-Trex MJ; CMV AG, Dübendorf, Switzerland) with standardised procedure by a single independent operator (JFL). Ankle plantar- and dorsi-flexion isokinetic assessment was shown to be valid and reliable in previous studies [5, 28]. A ten-minute warm-up on a stationary exercise bike was performed with low resistance (60 cycles per minute at 50 W). Next, patients were tested in a prone position, with the legs in extension. The foot was placed on the ankle plantar flexion–dorsiflexion footplate. The midpoint of the lateral malleolus was taken as the best-fit axis of the ankle and was aligned with the mechanical axis of the dynamometer. The range of motion was based on a reference position with the foot in neutral position at 90° from a maximal plantar flexion to a maximal dorsiflexion position without pain. Data were obtained at two testing angular velocities, 30 and 120 degree per second (deg/sec) concentrically, with five and 15 repetitions respectively [11, 26]. Tests were conducted on both ankles and began with the noninvolved ankle. Peak torque (N-m) was recorded for each angular velocity without gravity correction.
Statistical analysis
Analysis of the results was carried out using SPSS 16.0 program for Windows (SPSS Inc., Chicago, Il, USA). Descriptive statistics were used for the single parameters. Student’s t-test for paired variables and Wilcoxon test for intragroup comparison between peak torque of uninvolved and involved ankle were performed (level of significance, p < 0.05).
Results
Clinical outcome
The average follow-up of the series was 79 months (range, 48–81). No major complications or concerns with regards to wound healing were noted. In one ankle reflex sympathetic dystrophy was observed at two months after surgery with good outcome at latest follow-up. The average interval to work and sports recovery was five months (range, 2–12) and ten months (range, 6–18), respectively. However, all patients returned to a sports activity at a lower level compared to pre-injury level. No re-rupture has been recorded at latest follow-up.
Mean pre-operative AOFAS score improved from 64 points to 98 points (range, 90–100) at latest follow-up (p < 0.0001). Ankle range of motion was close to the non-involved ankle with an average of 12° of dorsiflexion (range, 5–15°) and 45.5° of plantar flexion (range, 40–50°) (the p value was not significant). Average calf atrophy was 1.7 cm (range, 0.5–3 cm) (p = 0.045). Tip-toe stance was possible for all patients without limitation. All patients presented with a loss of active range of motion of the hallux interphalangeal joint without subsequent hyperextension. However, none of the patients noticed functional weakness of the hallux during athletic or daily life activity.
Isokinetic assessment
Isokinetic testing at 30 deg/sec and 120 deg/sec revealed an average decrease of 28 ± 11% and 36 ± 4%, respectively, in the plantar flexion peak torque of the involved ankle compared with the non-involved ankle (p = 0.0027 and p = 0.001, respectively) (Table 1).
Table 1.
Descriptive statistics (mean values ± standard deviation) for ankle plantar- and dorsi-flexion peak torque (N-m)
| Angular velocity | Plantar flexion | Dorsiflexion | ||
|---|---|---|---|---|
| Involved ankle | Noninvolved ankle | Involved ankle | Noninvolved ankle | |
| 30 deg/sec | 71.1 ± 23.3* | 93.4 ± 39.2* | 35.4 ± 8.1 | 35.6 ± 13.4 |
| 120 deg/sec | 43.7 ± 7.5* | 66.0 ± 24.0* | 21.1 ± 4.8 | 22.8 ± 10.3 |
* p < 0.05
Discussion
This study reports our experience and outcome of a modified FHL transfer performed in 11 cases of AT chronic rupture with a 6.6-year average follow-up. Functional outcome improved significantly as assessed by the mean AOFAS score increment of 34 points at latest follow-up. In our series, all patients presented with a loss of active range of motion of the hallux interphalangeal joint. Despite this, none of the patients reported functional weakness of the hallux during athletic or daily life activity. No hyperextension of the hallux interphalangeal joint occurred. For functional outcome, our results were close to those reported by other authors [8, 12, 21, 24, 26, 27].
Previous studies have shown high reliability for isokinetic assessment, particularly for plantar flexion peak torque with slower speeds (30–60 deg/sec) [5, 28]. In our series, the decrease in plantar flexion peak torque value at 30 deg/sec between the involved and non-involved ankle was significant and averaged 28%. Using the same protocol, Wapner et al. found a 41.8% average decrease in plantar flexion peak torque [26]. In a recent study, Hahn et al. found a plantar flexion peak torque deficit of 35% at 60 deg/sec in a cohort of 13 patients including ten chronic AT ruptures and three tendinopathies at an average follow-up of 46.5 months [9]. Two other studies in the literature included both chronic rupture and Achilles tendinosis and had some limitations [18, 27]. Monroe et al. also recorded a 28% peak torque deficit at 30 deg/sec [18]. However, this series included a small cohort of seven patients who presented with chronic AT rupture, and isokinetic evaluation was performed at 19 months post-operatively [18]. Wilcox et al. showed a 7% plantar flexion strength deficit in a series of 20 patients including three chronic AT ruptures and 17 tendinopathies at a 14-month average follow-up [27]. However, in this study, isokinetic evaluation was performed at high speed (120 deg/sec) without assessment of the peak torque [27]. We believe that the differences in our results are due to FHL transfer augmentation using the remaining fibrous scar stumps of the ruptured AT.
Compared to PB or FDL, the FHL is a stronger plantar flexor; its axis of contractile force more closely reproduces that of the AT, it fires in phase with the gastrocnemius-soleus complex, and its anatomical proximity avoids the neurovascular bundle. Another benefit of FHL transfer is the plantar flexion strength reinforcement which is almost always compromised with fascial advancement alone [7]. With regards to vascularisation of AT, the FHL muscle belly extends distally into the avascular zone of AT and allows recruitment of an increased blood supply to the repaired AT. Furthermore, FHL transfer maintains the normal muscle balance of the ankle by transferring a muscle with the same function. In a recent study using MRI evaluation, Hahn et al. showed a complete integration of the FHL tendon in 60% of the patients (Fig. 4) [9]. The FHL was free of degeneration in all patients, and hypertrophy of the FHL of more than 15% was observed in 80% of the patients [9]. This hypertrophy of the FHL muscle suggests functional incorporation into plantar flexion after the transfer [9].
Fig. 4.
Complete integration of the flexor hallucis longus (FHL) tendon at 5.25 years after FHL transfer for a chronic Achilles tendon (AT) rupture on MRI evaluation. Preoperative MRI (left) showing the chronic AT rupture (arrow). Postoperative MRI (right)
Initially, for Wapner et al., augmentation of the reconstruction provided no additional benefit and, in fact, increased the amount of scar tissue formed, which only compromised functional outcome [26]. Excision of the AT segment with degenerative changes due to chronic rupture was complete to improve pain relief [26]. However, for other authors, FHL transfer alone was insufficient for reconstruction of defects greater than 5 cm, and a V-Y myotendinous advancement or a fascial turn-down flap was required [7, 8, 12, 13]. In a recent series, some authors proposed preservation of fibrous scar tissue at the stumps of the ruptured AT to keep its original length, make length adjustment easier and to use it as a scaffold for the FHL transfer [7–9, 15, 30]. In our series, fibrous scar tissue of AT stumps was preserved to restore some thickness with suture on the FHL transfer. Preserving this interposition scar tissue between tendon stumps has been shown to have the capacity to form tendon-like repair tissue, and previous studies concluded that it is suitable for repairing chronic AT ruptures [20, 29]. Similarly, in a recent study, Lee et al. showed on histological examination of fibrous scar stump biopsies that this tissue was composed of thick collagen fibers running parallel to the tendon axis with highly cellular fibrovascular tissue, altogether improving tendon healing [15].
The potential morbidity of FHL harvesting is essentially the loss of hallux interphalangeal plantar flexion strength. According to our results and those of other studies, FHL transfer morbidity is clinically insignificant, even for good push-off or balance in running sports [6, 26]. Therefore, alternatives to FHL such as FDL or PB appear less advantageous in these respects. Taking into account all surgical procedures, the incidence of AT re-rupture following acute or chronic rupture reconstruction has been reported to be 1.4–3.7% [4, 25]. However, in our study and other previous series, when using FHL tendon transfer for AT chronic rupture reconstruction, no case of re-rupture has been reported at latest follow-up [8, 12, 21, 24, 26, 27].
The main limitation of our series is the small number of patients included. However, this series of 11 patients was one of the largest on FHL transfer in this specific indication of chronic AT rupture and the average follow-up at 79 months was the longest in the literature.
In conclusion, for chronic or neglected AT rupture with a gap of at least 5 cm, surgical repair using a modified FHL transfer with fibrous AT stump reinforcement achieved excellent outcome at our latest follow-up.
References
- 1.Abraham E, Pankovich AM. Neglected rupture of the Achilles tendon: treatment by V-Y tendinous flap. J Bone Joint Surg Am. 1975;57-A:253–255. [PubMed] [Google Scholar]
- 2.Bosworth DM. Repair of defects in the tendo Achillis. J Bone Joint Surg Am. 1956;38-A:111–114. [PubMed] [Google Scholar]
- 3.Boyden EM, Kitaoka HB, Cahalan TD, An K. Late versus early repair of Achilles tendon rupture. Clin Orthop Relat Res. 1995;317:150–158. [PubMed] [Google Scholar]
- 4.Cetti R, Christensen SE, Ejsted R, Jensen NM, Jorgensen U. Operative vs. nonoperative treatment of Achilles tendon rupture. A prospective randomized study and review of the literature. Am J Sports Med. 1993;21:791–799. doi: 10.1177/036354659302100606. [DOI] [PubMed] [Google Scholar]
- 5.Chester R, Costa ML, Shepstone L, Donell ST. Reliability of isokinetic dynamometry in assessing plantar flexion torque following Achilles tendon rupture. Foot Ankle Int. 2003;24:909–915. doi: 10.1177/107110070302401207. [DOI] [PubMed] [Google Scholar]
- 6.Coull R, Flavin R, Stephens MM. Flexor hallucis longus tendon transfer: evaluation of postoperative morbidity. Foot Ankle Int. 2003;24:931–934. doi: 10.1177/107110070302401211. [DOI] [PubMed] [Google Scholar]
- 7.Hartog BD. Surgical strategies: delayed diagnosis or neglected Achilles’ tendon ruptures. Foot Ankle Int. 2008;29:456–463. doi: 10.3113/FAI.2008.0456. [DOI] [PubMed] [Google Scholar]
- 8.Elias I, Besser M, Nazarian LN, Raikin SM. Reconstruction for missed or neglected Achilles tendon rupture with V-Y lengthening and flexor hallucis longus tendon transfer through one incision. Foot Ankle Int. 2007;28:1238–1248. doi: 10.3113/FAI.2007.1238. [DOI] [PubMed] [Google Scholar]
- 9.Hahn F, Meyer P, Maiwald C, Zanetti M, Vienne P. Treatment of chronic Achilles tendinopathy and ruptures with flexor hallucis tendon transfer: clinical outcome and MRI findings. Foot Ankle Int. 2008;29:794–802. doi: 10.3113/FAI.2008.0794. [DOI] [PubMed] [Google Scholar]
- 10.Hansen ST. Trauma to the heel cord. In: Jahss MH, editor. Disorders of the foot and ankle. 2. Philadelphia: W.B. Saunders; 1991. p. 2357. [Google Scholar]
- 11.Kangas J, Pajala A, Ohtonen P, Leppilahti J. Achilles tendon elongation after rupture repair: a randomized comparison of 2 postoperative regimens. Am J Sports Med. 2007;35:59–64. doi: 10.1177/0363546506293255. [DOI] [PubMed] [Google Scholar]
- 12.Kann JN, Myerson MS. Surgical management of chronic ruptures of the Achilles tendon. Foot Ankle Clin. 1997;2:535–545. [Google Scholar]
- 13.Kissel CG, Blacklidge DK, Crowley DL. Repair of neglected Achilles tendon rupture: procedure and functional results. J Foot Ankle Surg. 1994;33:46–52. [PubMed] [Google Scholar]
- 14.Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle, hindfoot, midfoot, hallux and lesser toes. Foot Ankle. 1994;15:349–353. doi: 10.1177/107110079401500701. [DOI] [PubMed] [Google Scholar]
- 15.Lee KB, Park YH, Yoon TR, Chung JY. Reconstruction of neglected Achilles tendon rupture using the flexor hallucis longus tendon. Knee Surg Traumatol Arthrosc. 2008;17:316–320. doi: 10.1007/s00167-008-0693-9. [DOI] [PubMed] [Google Scholar]
- 16.Maffulli N, Waterston SW, Squair J, Reaper J, Douglas AS Changing incidence of Achilles tendon rupture in Scotland: a 15-year study. Clin J Sport Med. 1999;9:157–160. doi: 10.1097/00042752-199907000-00007. [DOI] [PubMed] [Google Scholar]
- 17.Mann RA, Holmes GB, Seale KS, Collins DN. Chronic rupture of the Achilles tendon: a new technique of repair. J Bone Joint Surg Am. 1991;73-A:214–219. [PubMed] [Google Scholar]
- 18.Monroe MT, Dixon DJ, Beals TC, Pomeroy G, Crowley DL, Manoli A. Plantar flexion torque following reconstruction of Achilles tendinosis or rupture with flexor hallucis longus augmentation. Foot Ankle Int. 2000;21:324–329. doi: 10.1177/107110070002100409. [DOI] [PubMed] [Google Scholar]
- 19.Myerson MS. Achilles tendon ruptures. Instr Course Lect. 1999;48:219–230. [PubMed] [Google Scholar]
- 20.Porter DA, Mannarino FP, Snead D, Gabel SJ, Ostrowski M. Primary repair without augmentation for early neglected Achilles tendon ruptures in the recreational athlete. Foot Ankle Int. 1997;18:557–564. doi: 10.1177/107110079701800905. [DOI] [PubMed] [Google Scholar]
- 21.Sebastian H, Datta B, Maffulli N, Neil M, Walsh WR. Mechanical properties of reconstructed Achilles tendon with transfer of peroneus brevis or flexor hallucis longus tendon. Foot Ankle Surg. 2007;46:424–428. doi: 10.1053/j.jfas.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 22.Teuffer AP. Traumatic rupture of the Achilles tendon: reconstruction by transplant and graft using the lateral peroneus brevis. Orthop Clin North Am. 1974;5:89–93. [PubMed] [Google Scholar]
- 23.Thermann H, Hufner T, Tscherne H. Achilles tendon rupture. Orthopade. 2000;29:235–250. doi: 10.1007/s001320050442. [DOI] [PubMed] [Google Scholar]
- 24.Us AK, Bilgin SS, Aydin T, Mergen E. Repair of neglected Achilles tendon ruptures: procedures and functional results. Arch Orthop Trauma Surg. 1997;116:408–411. doi: 10.1007/BF00434001. [DOI] [PubMed] [Google Scholar]
- 25.van der Linden-van der Zwang HMJ, Nelissen RGHH, Sintenie JB. Results of surgical versus non-surgical treatment of Achilles tendon rupture. Int Orthop. 2004;28:370–373. doi: 10.1007/s00264-004-0575-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wapner KL, Pavlock GS, Hecht PJ, Naselli F, Walther R. Repair of chronic Achilles tendon rupture with flexor hallucis longus tendon transfer. Foot Ankle. 1993;14:443–449. doi: 10.1177/107110079301400803. [DOI] [PubMed] [Google Scholar]
- 27.Wilcox DK, Bohay DR, Anderson JG. Treatment of chronic Achilles tendon disorders with flexor hallucis longus tendon transfer/augmentation. Foot Ankle Int. 2000;21:1004–1010. doi: 10.1177/107110070002101204. [DOI] [PubMed] [Google Scholar]
- 28.Woodson C, Bandy WD, Curis D, Baldwin D. Relationship of isokinetic peak torque with work and power for ankle plantar flexion and dorsiflexion. J Orthop Sports Phys Ther. 1995;22:113–115. doi: 10.2519/jospt.1995.22.3.113. [DOI] [PubMed] [Google Scholar]
- 29.Yasuda T, Kinoshita M, Okuda R. Reconstruction of chronic Achilles tendon rupture with the use of interposed tissue between the stumps. Am J Sports Med. 2007;35:582–588. doi: 10.1177/0363546506295939. [DOI] [PubMed] [Google Scholar]
- 30.Young A, Redfern DJ. Simple method of local harvest and fixation of FHL in Achilles tendon reconstruction: technique tip. Foot Ankle Int. 2008;29:1148–1150. doi: 10.3113/FAI.2008.1148. [DOI] [PubMed] [Google Scholar]