Abstract
Open reduction and internal fixation in distal tibial fractures jeopardises fracture fragment vascularity and often results in soft tissue complications. Minimally invasive osteosynthesis, if possible, offers the best possible option as it permits adequate fixation in a biological manner. Seventy-nine consecutive adult patients with distal tibial fractures, including one patient with a bilateral fracture of the distal tibia, treated with locking plates, were retrospectively reviewed. The 4.5-mm limited-contact locking compression plate (LC-LCP) was used in 33 fractures, the metaphyseal LCP in 27 fractures and the distal medial tibial LCP in the remaining 20 fractures. Fibula fixation was performed in the majority of comminuted fractures (n = 41) to maintain the second column of the ankle so as to achieve indirect reduction and to prevent collapse of the fracture. There were two cases of delayed wound breakdown in fractures fixed with the 4.5-mm LC-LCP. Five patients required primary bone grafting and three patients required secondary bone grafting. All cases of delayed union (n = 7) and nonunion (n = 3) were observed in cases where plates were used in bridge mode. Minimally invasive plate osteosynthesis (MIPO) with LCP was observed to be a reliable method of stabilisation for these fractures. Peri-operative docking of fracture ends may be a good option in severely impacted fractures with gap. The precontoured distal medial tibial LCP was observed to be a better tolerated implant in comparison to the 4.5-mm LC-LCP or metaphyseal LCP with respect to complications of soft tissues, bone healing and functional outcome, though its contour needs to be modified.
Introduction
Distal metaphyseal fractures of the tibia with or without intra-articular fracture extension in adults are among the most problematic injuries to treat. The most important variables that affected the final clinical result are the type of fracture, associated soft tissue injury, the method of treatment and the quality of the reduction [19, 24]. Conservative treatment of these fractures quite often results in a number of complications including malunion, nonunion and ankle stiffness [7, 19, 22]. These fractures are generally not suitable for intramedullary nailing, despite certain reports indicating satisfactory results in some of these fractures [2, 14, 16]. External fixation can be used as either a temporary or definitive method of treatment, especially in fractures with severe soft tissue injury [2, 6, 13, 15, 24], but malunion and delayed union continue to be the main problems with this method of fixation [20, 23]. Conventional plate osteosynthesis with open reduction can further devitalise fragments and lead to higher incidence of nonunion, infection and implant failure [4, 8]. Therefore, minimally invasive osteosynthesis, if possible, offers the best possible option as it permits adequate fixation in a biological manner [3, 13, 21]. However, an inadequate number of screws in a small oblique comminuted distal fragment presents a definite limitation even with this technique. The locking compression plate (LCP) provides enhanced stability in these situations with a minimum number of screws. In addition, it is possible to use these plates in a minimally invasive technique without fear of secondary displacement in the absence of perfect contouring [9]. This retrospective study was undertaken to evaluate the healing rate, complications and functional outcome of distal metaphyseal fracture of the tibia stabilised with three different locking plates from January 2004 to December 2007.
Materials and methods
Eighty-three consecutive adult patients with distal tibial fractures, including one patient with a bilateral metaphyseal fracture of the distal tibia, treated with three types of locking plates between January 2004 and December 2007 were reviewed. Patients with open fractures (Gustilo & Anderson grade IIIB & C), old fractures (>4 weeks), complex pilon fractures (AO 43C3) and pathological fractures were excluded from the study. Four patients not having a minimum follow-up of one year were excluded from the review, leaving 79 patients having 80 fractures (63 men and 16 women) with a median age of 36 years (range: 17–58 years); 68 patients were injured after road traffic accidents and 11 patients had a fall. The average time of five days between injury and surgical procedure (range: three to eight days) was mainly due to delay in reporting to the hospital or time taken to reduce the gross swelling.
Anteroposterior and lateral radiographs of the leg including the ankle joint were obtained to establish the fracture pattern, classification and pre-operative planning. Using the AO classification, 68 fractures were type A (18 type A1, 26 type A2, 24 type A3), eight fractures were type B (2 type B1, 3 type B2, 3 type B3) and four fractures were type C (2 type C1 and 2 type C2). Open fractures were classified according to the Gustilo & Anderson classification. There were 11 cases of grade I, 4 cases of grade II and four cases of grade IIIA open fractures. A 3.5-mm one third tubular plate was used to stabilise the fibula before fixation of the tibia to maintain the alignment of the leg and ankle in the presence of tibial comminution (n = 41), thereby making the stabilisation of the tibia easier. Through a small incision over the medial malleolus, sparing the saphenous vein and nerve, the tibial plate was inserted extraperiosteally. Fracture fragments were reduced using indirect reduction techniques. Precontouring of the plate was performed so as to approximately match the contour of the distal tibia and was followed by stabilisation using proximal and distal locking screws. Closed reduction achieved anatomical alignment in 71 fractures and open reduction was required in the remaining nine fractures. In 33 fractures a 4.5-mm limited-contact locking compression plate (LC-LCP) was used, 27 fractures were fixed with a metaphyseal LCP and in the remaining 20 fractures, a distal medial tibial LCP was used. Choice of implant was primarily dependent on availability of implants. As different plates evolved over time a 4.5-mm LC-LCP was used initially then metaphyseal LCP and distal medial tibial LCP. Primary bone grafting was performed in five cases to fill up the gap at the fracture site caused by compression of cancellous bone. In the event of significant impaction of the cancellous bone resulting in a gap, acute docking of fragments was done (n = 21) to achieve better contact between tibial fragments even if it resulted in mild shortening (average 7 mm). Limb elevation, to achieve gravity-assisted venous drainage along with active toe and ankle movements were carried out for the initial two weeks. Stitches were removed at approximately two weeks in the majority of patients apart from 16 patients with significant pre-operative swelling, where they were left in place for three to four extra days to prevent wound dehiscence.
Non-weight-bearing ambulation was permitted at approximately two weeks, after proper wound healing and appearance of the wrinkle sign. Patients were followed up clinically and radiologically in the fracture clinic at monthly intervals for the first six months and then every two months up to one year to assess progress of union and possible complications. Full weight-bearing was permitted only after clinico-radiological evidence of union. Union was defined as bridging of three of the four cortices and disappearance of the fracture line on the plain radiographs for a patient who was able to bear full weight. Fracture in the process of union but not united at six months was considered as delayed union. Nonunion was defined as a fracture that did not heal within a year. Malunion was defined as the incongruity of the articular surface of more than 2 mm or malalignment greater than 5° in any plane. At the end of one year, final functional outcomes were assessed using the Olerud and Molander scoring system [18].
Statistical analysis
Data were analysed with the chi-square test and Student’s t test. For all tests, probability less than 0.05 was considered significant.
Results
Precontouring was required for all locking plates so as to approximately match the contour of the distal tibia. Even the precontoured distal medial tibial LCP required correction of the contour in all cases as the contour was significantly different from the distal tibial contour in our patients. There was no statistically significant difference in the demographic profile of the patients treated with three different locking plates with respect to age, sex, fracture classification, mode of trauma and associated soft tissue injury (Table 1). Compression plate osteosynthesis plus minimally invasive plate osteosynthesis (MIPO) was used in simple fracture patterns (eight in fractures fixed with the 4.5-mm LC-LCP, six in fractures fixed with the metaphyseal LCP and four in fractures fixed with the distal medial tibial LCP). Bridge plating plus MIPO was used in the rest of the fractures on account of tibial comminution [25 in fractures fixed with the 4.5-mm LC-LCP (Fig. 1a, b), 21 in fractures fixed with the metaphyseal LCP (Fig. 2a, b) and 16 in fractures fixed with the distal medial tibial LCP (Fig. 3a, b)]. There was intra-operative difficulty in closure of the surgical wound in three cases fixed with the 4.5-mm LC-LCP and in two cases fixed with the metaphyseal LCP; hence, the fibular skin incision was left open after stitching the muscle layer and delayed closure was done subsequently (Table 2). Superficial infection was observed in one patient with AO type 43.A1, compound grade IIIA fracture fixed with the 4.5-mm LC-LCP. Stitches of the distal incision were opened for débridement and the wound healed secondarily with topical care. No other patient had wound dehiscence in the post-operative period. The mean time to full weight-bearing was 16 weeks (range: 13–32 weeks). The mean time to union was 19 weeks (range: 16–32 weeks) in 77 fractures. Of these 77 fractures, seven fractures however had delayed union, with union time of less than nine months. One of the cases with delayed union had an anterior gap in the tibia due to cancellous bone impaction and required secondary bone grafting before union could be achieved. The distribution of functional outcome according to the Olerud and Molander score in the three groups is shown in Table 3; the difference between the three groups was not statistically significant.
Table 1.
Demographic profile of the patients
| 4.5-mm LC-LCP (n = 32) | Metaphyseal LCP (n = 27) | Distal medial tibial LCP (n = 20) | P value | |
|---|---|---|---|---|
| Median age (years) | 35 | 36.3 | 38 | NS |
| Male/female | 26/6 | 19/8 | 18/2 | NS |
| AO classification A/B/C | 29/3/1 | 24/2/1 | 15/3/2 | NS |
| Open fracture grade I/II/IIIA | 4/1/1 | 3/2/1 | 4/1/2 | NS |
| RTA | 28 | 23 | 17 | NS |
| Fall from height | 4 | 4 | 3 | |
| Primary bone grafting | 2 | 2 | 1 | NS |
| Fibula fixation | 18 | 13 | 10 | NS |
NS not significant, RTA road traffic accidents
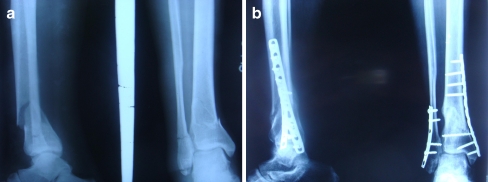
Fig. 1.
a Anteroposterior and lateral radiographs of a 36-year-old male showing the distal tibial metaphyseal fracture type 43A2. b Follow-up radiographs: the tibial fracture was stabilised with the 4.5-mm LC-LCP and united at 6 months
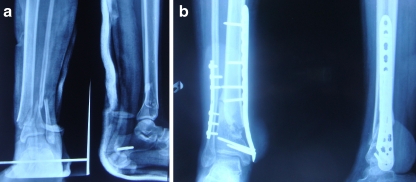
Fig. 2.
a Anteroposterior and lateral radiographs of a 30-year-old male showing the distal tibial metaphyseal fracture type 43A1. b Follow-up radiographs: the tibial fracture was stabilised with the metaphyseal LCP and united at 16 weeks
Fig. 3.
a Anteroposterior and lateral radiographs of a 39-year-old male showing the distal tibial metaphyseal fracture type 43A3. b Follow-up radiographs: the tibial fracture was stabilised with the distal medial tibial LCP and united at 15 weeks
Table 2.
Complications in the three groups
| Complication | 4.5-mm LC-LCP (n = 33) | Metaphyseal LCP (n = 27) | Distal medial tibial LCP (n = 20) | P value |
|---|---|---|---|---|
| Delayed union | 3 | 2 | 2 | NS |
| Nonunion | 2 | 1 | _ | NS |
| Difficult closure | 3 | 2 | _ | NS |
| Malunion | 2 | _ | _ | NS |
| Pain over medial malleolus | 26 (81%) | 16 (60%) | 5 (25%) | < 0.001 |
| Exposed plate | 2 | _ | _ | NS |
| Infection | 1 | _ | _ | NS |
| Wound breakdown | 2 | _ | _ | NS |
| Implant removal | 18 (55%) | 6 (23%) | 3 (15%) | < 0.01 |
NS not significant
Table 3.
Functional outcome in the three groups
| Operative group | Number of patients with Olerud and Molander score | |||
|---|---|---|---|---|
| > 92 (excellent) | 87–92 (good) | 65–86 (fair) | < 65 (poor) | |
| 4.5-mm LC-LCP group | 7 | 17 | 5 | 4 |
| Metaphyseal LCP group | 9 | 12 | 3 | 3 |
| Distal medial tibial LCP group | 9 | 9 | 1 | 1 |
P value: not significant
Nonunion was observed in three of our fractures (two in the 4.5-mm LC-LCP group and one in the metaphyseal LCP group). Of these three fractures, two required secondary bone grafting to fill up the gap before union could be achieved. The third fracture had proximal diaphyseal extension of the fracture with secondary infection and required implant removal. It was subsequently managed by a patellar tendon-bearing (PTB) cast with weight-bearing resulting in union of the fracture. All cases of delayed union or nonunion were observed in cases where plates were used in bridge mode.
There were two cases of delayed scar breakdown resulting in aseptic exposure of the plate, both in the 4.5-mm LC-LCP group. One required a subsequent fasciocutaneous flap. Another patient required only plate removal as the fracture had united. Anatomical alignment (varus or valgus angulations <5°, internal or external rotation <5°, limb length discrepancy <1 cm) was achieved in all but two cases: a 42-year-old female with fracture type 43.A2 which was fixed with the 4.5-mm LC-LCP united in varus malunion of 14° and a 38-year-old male with fracture type 43.A3 which was fixed with the 4.5-mm LC-LCP united in 17° of varus. A total of 65 of our patients (26 patients with fractures fixed with the 4.5-mm LC-LCP, 16 patients with fractures fixed with the metaphyseal LCP and five patients with fractures fixed with the distal medial tibial LCP) reported local pain over the medial malleolus.
Discussion
The treatment of distal metaphyseal fractures of the tibia by closed intramedullary nailing or by open reduction and internal fixation using plates may be associated with complications such as malunion, nonunion, secondary loss of reduction, wound dehiscence, local septic complications and stiffness of adjacent joints [2, 8, 16]. MIPO of these fractures is technically feasible and advantageous in that it minimises soft tissue compromise and devascularisation of the fracture fragments [5, 13, 17, 21]. The procedure includes three important components: closed reduction, minimal soft tissue dissection and stabilisation with a long percutaneously inserted plate fixed with a limited number of widespread screws. Even though early intervention is advantageous, it is desirable to delay surgery in the presence of gross local swelling until subsidence of swelling and appearance of the wrinkle sign (range: three to eight days) to ensure good local skin condition prior to surgery.
In this retrospective study of 79 patients with 80 fractures treated with three different types of locking plates using MIPO techniques, 70 of 80 fractures (88%) healed without malunion or bone healing complications, which is comparable to healing rates reported in other studies incorporating MIPO techniques [5, 13, 15, 17, 21], and supports the biological advantages of MIPO techniques over open reduction techniques especially while dealing with the critical soft tissue conditions. The rate of malunion in our series (2.5%) is comparable to the rates (3.8–5%) reported in the literature [5, 17, 21]. The rate of nonunion in our series (3.7%) is also comparable to the rates (0–6.6%) reported in the literature [10, 12, 15, 17, 21]. No incidence of nonunion or delayed union was observed in cases where plating was done in compression mode, as all the instances of delayed union or nonunion occurred with bridge mode. We agree with Hasenboehler et al. that a bridge plating technique in simple fracture patterns is disadvantageous due to prolonged healing time [12]. However, it should be kept in mind that the patients in the second subset have a higher grade of fractures with comminution and compression of the cancellous bone resulting in some gap at the fracture site. Collinge et al. also reported significant reoperation rate (35%) and prolonged time to union in patients treated by the MIPO technique and recommended extra measures in at-risk patients, including those with highly comminuted fracture patterns, bone loss or type II or III open fractures [5]. In our series we also adopted additional measures in comminuted fractures with bone gap in the form of primary bone grafting in five cases and acute docking of the fracture even at the cost of slight shortening in 21 cases and these measures resulted in union of such difficult fractures. A standard protocol of stitch removal at two weeks was followed apart from 16 cases with preoperative gross swelling when stitch removal was delayed by three to four days to prevent wound dehiscence. The authors are of the opinion that critical soft tissues in the distal tibia require more time to heal and so stitch removal should be delayed in cases of preoperative gross swelling.
Our study included three different types of locking plates (4.5-mm LC-LCP, metaphyseal LCP and distal medial tibial LCP) and we also focused on fracture healing and complications in respect to different plating systems. It is not essential to fix fibular fractures in the presence of a simple fracture pattern of the tibia provided the fibular fracture is proximal to the syndesmosis. However, any fibular fracture at the level of, or distal to the syndesmosis, with comminution of the distal tibia requires stabilisation to maintain the lateral column of the ankle thereby preventing late collapse and secondary loss of reduction. Simple primary closure of the surgical wound was not possible in three cases with the 4.5-mm LC-LCP and in two cases with the metaphyseal LCP, reflecting the bulky nature of these plates; this complication has also been reported by various authors [12, 17]. Two cases had malunion in varus in the 4.5-mm LC-LCP group, as it was not possible to put more than three screws in the distal fragment, resulting in a weak biomechanical construction in comparison to the metaphyseal LCP and distal medial tibial LCP. Delayed wound breakdown was observed in two cases fixed with the 4.5-mm LC-LCP, the plausible explanation being that both cases were open fractures with greater soft tissue insult and bulkiness of the implant.
There were three cases of nonunion, all with high energy open fractures and all of the cases presented with co-morbidities such as peripheral vascular disease with alcohol and tobacco abuse, which are known to be associated with complications of bone healing [1, 11]. Implants with lower profile or variable thickness (distal medial tibial LCP and metaphyseal LCP, respectively) can be strategically used to decrease soft tissue tension. Skin irritation in the distal scar and pain over the medial malleolus was observed in 81% patients where the 4.5-mm LCP was used and 60% where the metaphyseal LCP was used, both attributed to bulkiness of the implant, and this problem was significantly less (P value < 0.001) in patients where the malleolar LCP was used (25%). Gao et al. in their study also observed that 19% of patients had local discomfort over the medial malleolus [10]. Similarly Borg et al. reported tenderness around the plate in 55% of patients [3]. Local soft tissue irritation and pain over the medial malleolus can be avoided using low profile plates such as the distal medial tibial LCP. Implant removal was also required in a lower number of patients treated with the malleolar LCP in comparison to other patients treated with the 4.5-mm LC-LCP and metaphyseal LCP in our series (P value < 0.01). However, an important observation was made that the precontoured distal medial tibial LCP required additional contouring (slight straightening of the plate at the angle, as the plate in the original contour was significantly raised at the level of the medial malleolus in every case), indicating that either the design was faulty or there might be a difference in curvature of the distal tibia between Asian and Western populations. However, this change in contour resulted in change of direction of the locking screws in the subchondral area of the distal tibia.
The limitations of our study include its retrospective nature and potential for user bias because the surgeon could not be blinded with respect to the locking plate used in the treatment, though it was largely guided by the availability of implants. However, on account of long follow-up and a large number of patients in this study, we can conclude that the treatment of distal tibial metaphyseal fractures with an LCP using the minimally invasive locking plate osteosynthesis (MILPO) technique is a reliable alternative method of stabilisation. It decreases the incidence of complications of soft tissue and bone healing associated with the conventional methods of plating or external fixation of these fractures. Intramedullary nailing, though biological, suffers from a limitation of inadequate fixation due to a small distal fragment, even more so in the presence of comminution [14, 16]. A precontoured distal medial tibial LCP is a better tolerated implant in comparison to the 4.5-mm LC-LCP and metaphyseal LCP with respect to complications of soft tissues and bone healing and functional outcome, though its contour needs to be modified. Additional measures in the form of acute docking of the fracture, primary bone grafting and supplementary fibular fixation in comminuted fractures are recommended.
References
- 1.Adams CI, Keating JF, Court-Brown CM. Cigarette smoking and open tibial fractures. Injury. 2001;32(1):61–65. doi: 10.1016/S0020-1383(00)00121-2. [DOI] [PubMed] [Google Scholar]
- 2.Blauth M, Bastian L, Krettek C, Knop C, Evans S. Surgical options for the treatment of severe tibial pilon fractures: a study of three techniques. J Orthop Trauma. 2001;15(3):153–160. doi: 10.1097/00005131-200103000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Borg T, Larsson S, Lindsjö U. Percutaneous plating of distal tibial fractures. Preliminary results in 21 patients. Injury. 2004;35(6):608–614. doi: 10.1016/j.injury.2003.08.015. [DOI] [PubMed] [Google Scholar]
- 4.Borrelli J, Jr, Prickett W, Song E, Becker D, Ricci W. Extraosseous blood supply of the tibia and the effects of different plating techniques: a human cadaveric study. J Orthop Trauma. 2002;16(10):691–695. doi: 10.1097/00005131-200211000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Collinge C, Kuper M, Larson K, Protzman R. Minimally invasive plating of high-energy metaphyseal distal tibia fractures. J Orthop Trauma. 2007;21(6):355–361. doi: 10.1097/BOT.0b013e3180ca83c7. [DOI] [PubMed] [Google Scholar]
- 6.Dickson KF, Montgomery S, Field J. High energy plafond fractures treated by a spanning external fixator initially and followed by a second stage open reduction internal fixation of the articular surface—preliminary report. Injury. 2001;32(Suppl 4):SD92–SD98. doi: 10.1016/s0020-1383(01)00163-2. [DOI] [PubMed] [Google Scholar]
- 7.Digby JM, Holloway GM, Webb JK. A study of function after tibial cast bracing. Injury. 1983;14(5):432–439. doi: 10.1016/0020-1383(83)90094-3. [DOI] [PubMed] [Google Scholar]
- 8.Fisher WD, Hamblen DL. Problems and pitfalls of compression fixation of long bone fractures: a review of results and complications. Injury. 1978;10(2):99–107. doi: 10.1016/S0020-1383(79)80069-8. [DOI] [PubMed] [Google Scholar]
- 9.Frigg R. Development of the Locking Compression Plate. Injury. 2003;34(Suppl 2):B6–B10. doi: 10.1016/j.injury.2003.09.020. [DOI] [PubMed] [Google Scholar]
- 10.Gao H, Zhang CO, Luo CF, Zhou ZB, Zeng BF. Fractures of the distal tibia treated with polyaxial locking plating. Clin Orthop Relat Res. 2009;467:831–837. doi: 10.1007/s11999-008-0459-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gullihorn L, Karpman R, Lippiello L. Differential effect of nicotine and smoke condensate on bone cell metabolic activity. J Orthop Trauma. 2005;19(1):17–22. doi: 10.1097/00005131-200501000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Hasenboehler E, Rikli D, Babst R. Locking compression plate with minimally invasive plate osteosynthesis in diaphyseal and distal tibial fracture: a retrospective study of 32 patients. Injury. 2007;38(3):365–370. doi: 10.1016/j.injury.2006.10.024. [DOI] [PubMed] [Google Scholar]
- 13.Hazarika S, Chakravarthy J, Cooper J. Minimally invasive locking plate osteosynthesis for fractures of the distal tibia—results in 20 patients. Injury. 2006;37(9):877–887. doi: 10.1016/j.injury.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 14.Janssen KW, Biert J, Kampen A. Treatment of distal tibial fractures: plate versus nail: a retrospective outcome analysis of matched pairs of patients. Int Orthop. 2007;31(5):709–714. doi: 10.1007/s00264-006-0237-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Krackhardt T, Dilger J, Flesch I, Höntzsch D, Eingartner C, Weise K. Fractures of the distal tibia treated with closed reduction and minimally invasive plating. Arch Orthop Trauma Surg. 2005;125(2):87–94. doi: 10.1007/s00402-004-0778-y. [DOI] [PubMed] [Google Scholar]
- 16.Moshieff R, Safran O, Segal D, Liebergall M. The unreamed tibial nail in the treatment of distal metaphyseal fractures. Injury. 1999;30(2):83–90. doi: 10.1016/S0020-1383(98)00213-7. [DOI] [PubMed] [Google Scholar]
- 17.Oh CW, Kyung HS, Park IH, Kim PT, Ihn JC. Distal tibial metaphyseal fractures treated by percutaneous plate osteosynthesis. Clin Orthop Relat Res. 2003;408:286–291. doi: 10.1097/00003086-200303000-00038. [DOI] [PubMed] [Google Scholar]
- 18.Olerud C, Molander H. A scoring scaling for symptom evaluation after ankle fracture. Arch Orthop Trauma Surg. 1984;103(3):190–194. doi: 10.1007/BF00435553. [DOI] [PubMed] [Google Scholar]
- 19.Ovadia DN, Beals RK. Fractures of the tibial plafond. J Bone Joint Surg Am. 1986;68(4):543–551. [PubMed] [Google Scholar]
- 20.Pugh KJ, Wolinsky PR, McAndrew MP, Johnson KD. Tibial pilon fractures: a comparison of treatment methods. J Trauma. 1999;47(5):937–941. doi: 10.1097/00005373-199911000-00022. [DOI] [PubMed] [Google Scholar]
- 21.Redfern DJ, Syed SU, Davies SJ. Fractures of the distal tibia: minimally invasive plate osteosynthesis. Injury. 2004;35(6):615–620. doi: 10.1016/j.injury.2003.09.005. [DOI] [PubMed] [Google Scholar]
- 22.Rüedi TP, Allgöwer M. The operative treatment of intra-articular fractures of the lower end of the tibia. Clin Orthop Relat Res. 1979;138:105–110. [PubMed] [Google Scholar]
- 23.Ristiniemi J, Flinkkilä T, Hyvönen P, Lakovaara M, Pakarinen H, Biancari F, Jalovaara P. Two-ring hybrid external fixation of distal tibial fractures: a review of 47 cases. J Trauma. 2007;62(1):174–183. doi: 10.1097/01.ta.0000215424.00039.3b. [DOI] [PubMed] [Google Scholar]
- 24.Streicher G, Reilmann H. Distal tibial fractures (in German) Unfallchirug. 2008;111(11):905–918. doi: 10.1007/s00113-008-1511-z. [DOI] [PubMed] [Google Scholar]