Abstract
A cross-sectional epidemiological study via personal interviews was performed regarding low back pain and its related clinical aspects in a Hungarian sample of 10,000 people. Joining the international campaign of the “Bone and Joint Decade”, our aim was to give data on low back pain prevalence and to explore the underlying possible clinical conditions in a Central European adult and adolescent population. Ten thousand people aged 14–65, selected randomly by the Hungarian central office of statistics from three counties of the south-western Hungarian region, were surveyed using a special questionnaire focusing on low back pain and other degenerative spinal symptoms. People with low back pain complaints and written consent were asked to participate in a further clinical investigation, where radiological and clinical assessment was performed. A total of 4,389 persons (44.1%) reported low back pain in the last month at the time of the survey. Work absenteeism due to low back pain affected 2,140 persons (21.5%). A total of 292 people (2.9%) had already undergone spinal surgery. Upon request 682 people came for a clinical follow-up, where thorough physical examination and radiological analysis was performed and results were statistically interpreted. The Oswestry disability index (ODI) in the examined group of patients averaged 35.1%; radiological degenerative signs were observed in 392/682 (57.5%). Individuals with signs of radiological degeneration had a statistically significant higher ODI value, age, and a higher, yet not significantly increased BMI value than radiographically negative patients (p < 0.05). Co-existence of hip and knee osteoarthritis was also investigated. Higher osteoarthritis prevalence was found in individuals with radiographic signs of spinal degeneration. Details of the survey and clinical investigations are discussed.
Introduction
In most countries low back pain is a major cause of disability, leading to work absenteeism and use of health services, particularly in adults of working age. Depending on the method of sampling, questionnaire type of a survey and the examined population, the estimated prevalence varies widely. In a recent review article authors analysed epidemiological literature from 1981 to 1998 and found that the number of methodologically acceptable articles defining prevalence rates of low back pain is limited. It was estimated that the point prevalence rate in North America was 5.1% [1]. In a British study conducted in 1997–1998, the authors found that in a ten-year period the prevalence of low back pain increased by 12.7% from 36.4% to 49.1% in the same population [2]. According to another European review article the point prevalence of back pain ranged between 14% and 42%, whereas lifetime prevalence was between 51% and 84%. According to their observations the highest prevalence is found between the ages of 50 and 64 [3]. Other studies also report 50% annual prevalence rates of low back pain [4, 5].
Most of these epidemiological studies were carried out in high-income (Western European and North American) countries, whereas little is known about low back pain in low- to middle-income countries [6]. According to Volinn [6], the hypothesis of having a higher percentage of low back pain prevalence in the low income countries due to the higher percentage of physical workers and people forced to work for prolonged periods of time could not be proven, since he found a two to four times lower prevalence amongst these populations than in the Swedish, German or Belgian general population.
Hungary, as a recent member of the EU, is considered to be a country of economic transition with a GDP of approximately $14,000 at the time of the survey. According to our knowledge no previous study has been carried out in Central and Eastern European countries to determine low back pain prevalence and its related aspects. Most of the reviewed epidemiological studies were carried out using postal questionnaires, phone surveys and only a few have been performed via personal interviews. In order to obtain a high response rate and to diminish the number of incorrect answers, we believe that the best way to obtain data is through personal interviewing. The aim of our study was to investigate low back pain prevalence in a representative sample of 10,000 people aging from 14 to 65 years and to explore the possible socioeconomic factors that could influence its frequency and severity.
In a second phase of the project, people complaining of low back pain and giving prior consent were invited for a clinical follow-up in order to explore possible underlying degenerative conditions. According to literature there is no consensus as to whether functional spinal scores representing the patient’s complaints have any close correlation to degenerative conditions diagnosed on the radiographs. Nor is there any universally accepted radiological score to categorise degenerative spinal conditions by severity as there are existing radiological scores for hip or knee degenerative pathology.
Even the most thorough review articles state that body weight and increased BMI should be considered a possible, yet weak risk factor for low back pain [7]. With the aim of contributing to this issue, the possible effect of obesity on complaints and radiological conditions was also investigated.
The hip spine syndrome was first described by Offierski and Macnab [8]. In their article they emphasise the need to investigate the source of the disability, because co-existing hip and spine pathology can give a very confusing clinical picture and can lead to faulty diagnosis and false treatment. In a recent article substantial improvement was noticed in low back pain and spinal functional outcome following total hip replacement in a group of patients with co-existing severe hip osteoarthritis and lumbar spine degeneration [9].
In a recent article Murata et al. defined the knee–spine syndrome. According to their observations advanced knee osteoarthritis with flexion contracture affects posture by increasing lumbar lordosis and thereby increasing low back pain [10]. In our study, physical examination and radiological screening helped us find those affected by spinal, hip and knee degeneration.
Patients and methods
Ten thousand individuals aged between 14 and 65 years living in three counties of the south-western region of Hungary were involved in the study. According to Hungarian census data carried out in 2001, this region had approximately 995,000 inhabitants, approximately 9.8% of the Hungarian population. More than half (56%) of them were living in 34 cities of the area, while the remaining 44% were living in 619 villages. The average population density was 70.2 inhabitants/km2.
The sample was selected by multistage sampling, and thus the address list was provided by the Baranya County Division of the Hungarian Central Office of Statistics. The sample quotas were representative concerning age, employment and municipal structure. Using the address list, data were obtained in May and June 2002 via personal interviews conducted by approximately 300 trained pollsters.
In the examined population, 55.1% were female and 44.9% male with an average age of 42.1 years. Of those surveyed, 51% were employed, 28.4% retired, and 19.4% were unemployed for various reasons (students, pregnant women, etc.). Among the employed people the percentage of physical workers was higher (32% of the total surveyed) than that of the white-collar workers (19% of the total).
Due to the lack of a universally accepted questionnaire for low back pain symptoms, our own questionnaire was used to explore lower back complaints. This incorporated questions of standardised, internationally used scores used by the literature, and pain drawing schemes as well.
From the 4,389 patients who reported low back pain at the time of the questionnaire survey, 2,241 had given consent for a later clinical investigation. Following repeated written request, 682 people came for a clinical follow-up, of which 249 had low back pain only and 433 had hip or knee pain, or both, as well. Based on patient history and physical examinations, the Oswetry disability index was calculated, BMI was recorded, and standard AP and lateral view radiographs were taken of the lumbar spine. In order to explore co-existing hip or knee pathology, AP pelvis and bilateral AP and lateral view X-rays were taken. The diagnosis of hip and knee osteoarthritis was established at a cut-off value of 2 points or above according to the Kellgren-Lawrence classification system [11].
Lumbar spine degenerative conditions were categorised into four groups: discopathy, degenerative scoliosis, spondylolisthesis and spondylosis. Negative cases and other pathologies, e.g. compression fractures and spina bifida, were also recorded. Our results were statistically analysed. Continuous variables were analysed in terms of mean ± standard deviation. Chi square test was used to establish data correlation. Standard Student’s t-test for paired samples or one-way ANOVA was performed for comparing data, as needed. A p-value < 0.05 was considered significant. All analyses were carried out with SPSS software for Windows version 13.0 (SPSS Inc., Chicago, IL, USA).
Results
Of the people surveyed, 9,957 out of the 10,000 answered our questionnaire completely, making further data processing possible. To the question: "Have you experienced low back pain recently?”, 4,389 people (44.1%) gave a positive answer. Upon examining the gender specific prevalence we found that almost half of surveyed women were affected by low back pain (48.1%), whereas only 39.1% of men reported pain at the time of the survey.
Age specific investigations showed that the average age of the affected population was 46.71 years, and in those without pain was 38.5 years. Age specific distribution is shown in Table 1.
Table 1.
Age specific prevalence of low back pain
| Age group | Low back pain | Total number | |
|---|---|---|---|
| Yes | No | ||
| 14–19 years | 82 (12.5%) | 575 (87.5%) | 657 |
| 20–29 years | 450 (26.3%) | 1,264 (73.7%) | 1,714 |
| 30–39 years | 742 (39%) | 1,163 (62%) | 1,905 |
| 40–49 years | 1,043 (50%) | 1,041 (50%) | 2,084 |
| 50–59 years | 1,222 (56.7%) | 934 (43.3%) | 2,156 |
| 60–65 years | 850 (59.1%) | 588 (40.9%) | 1,438 |
Did not know/did not answer: 46
The onset and the duration of the pain at the time of the survey was over a year in most cases (81.5%). Nine hundred twenty (9.2%) persons complained of limping. Irradiating pain into the groin, gluteal region or the lower extremities was experienced by 2,945 (29.6%) individuals. Nine hundred ninety two (9.9%) could not tiptoe or heel-walk because of low back pain. At the time of the survey, 883 (8.9%) individuals were under continuous medical treatment for low back pain. Most of those with current low back pain had already experienced painful episodes, whereas there was a considerable number who were currently free of pain, but had experienced earlier attacks. Low back pain was given as the reason by 2,140 persons (21.5%) for absenteeism from work. Absenteeism was divided into weekly, then monthly periods. Most of those surveyed were absent for a period of two to four weeks (789), followed by the group of one to three months (494), and then those who were absent for less than two weeks (411) (Table 2). Two hundred ninety two (2.9%) individuals were operated upon because of back problems; 43% of this group did not go back to work after the operation. In the 12 preceding months prior to the survey 1,883 (18.9%) people asked for medical help from one or more doctors because of low back pain. Of these, 1,695 (17%) visited the GP, 1,033 (10.3%) were seen by a specialist, 653 (6.5%) went to an outpatient department of a hospital/clinic, and 182 (1.8%) were admitted to hospital.
Table 2.
Duration of absenteeism because of low back pain
| Absenteeism | Number | Percent |
|---|---|---|
| Less than two weeks | 411 | 19.5% |
| 2–4 weeks | 789 | 37.4% |
| 1–3 months | 494 | 23.4% |
| 3–6 months | 141 | 6.7% |
| Over 6 months | 275 | 13.0% |
| Total | 2,110 | 100.0% |
Did not know/ did not answer: 30
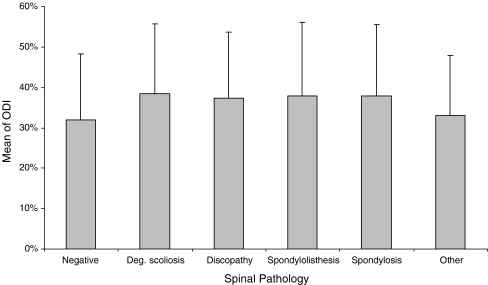
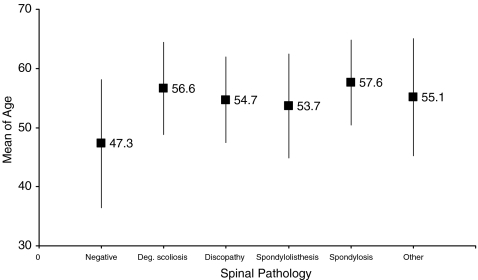
In total, 682 (241 male, 441 female) people came for clinical assessment. The average age at the time of the investigation was 52.3 years (range 16–67). The average Oswestry disability index (ODI) was 35.1%. Following radiological analysis patients were categorised into groups: 290 had no sign of spinal degeneration, 160 showed discopathy, 158 spondylosis, 35 degenerative scoliosis, 12 degenerative spondylolisthesis, and in 27 other alterations were recorded. Functional scores (ODI) of the different radiological groups are compared in Fig. 1. A statistically significant difference was detected only in the radiological negative group vs. all other groups with spinal pathology (p < 0.05). There was also a significant difference (p < 0.05) regarding patient age between individuals having no alteration on the X-rays and those having spinal pathology as shown in Fig. 2.
Fig. 1.
Oswestry disability index in various degenerative radiological conditions. Oswestry disability index is significantly worse in individuals with signs of radiographic degeneration (p < 0.05). All of the examined patients in the cohort reported episodes of prior low back pain symptoms
Fig. 2.
Age distribution of various degenerative spinal conditions. The mean age of radiographically negative patients is significantly lower (an average 8 years) than individuals with spinal degeneration (p < 0.05)
Due to the low number of cases, degenerative scoliosis, spondylolisthesis and other pathologies were excluded from further statistical analysis.
Regarding BMI, radiologically negative patients were slightly overweight (average BMI 27.8), whereas average values of 29.9 and 30.2 were recorded in patients with discopathy and spondylosis, respectively. This difference was not significant.
Spinal degenerative conditions were cross-matched with hip and knee X-rays, where patients having ≥2 points according to the Kellgren-Lawrence classification were defined as having osteoarthritis of the hip and knee joints. We found that the number of patients affected by hip and knee osteoarthritis is significantly higher in those having spinal degeneration (p < 0.05). The associations are shown in Tables 3 and 4.
Table 3.
Co-existence of spinal degeneration and knee osteoarthritis
| Spinal pathology | Knee pathology | ||
|---|---|---|---|
| Negative | Osteoarthritis | Total | |
| Negative | 266 | 26 | 290 |
| Discopathy | 126 | 34 | 160 |
| Spondylosis | 115 | 43 | 158 |
| Total | 505 | 103 | 608 |
Table 4.
Co-existence of spine degeneration and hip pathology
| Spinal pathology | Hip pathology | |||
|---|---|---|---|---|
| Negative | Osteoarthritis | THR | Total | |
| Negative | 268 | 21 | 1 | 290 |
| Discopathy | 128 | 27 | 5 | 160 |
| Spondylosis | 109 | 43 | 6 | 158 |
| Total | 501 | 91 | 16 | 608 |
THR total hip replacement
Discussion
In this study prevalence of low back pain and its related aspects were examined in a representative Hungarian sample of 10,000 individuals. The response rate was over 99%, which may have been a result of personal interviews by trained pollsters instead of using a postal survey. More than 44% of those interviewed reported low back pain for the preceding month of the survey. This prevalence rate seems to be relatively high in comparison with other general population surveys [4–6, 12]. This difference may arise from several factors: high response rate, differences in methodology, sampling, and definition of low back pain, self-reported pain, and pain perception. Palmer et al. pointed out in their comparative surveys that due to cultural changes people also show more willingness to report even minor back symptoms as a reason for absence attributed to sickness [2]. In our study though, the higher prevalence is possibly due to the fact that the number of people employed as physical workers is higher than in other examined populations (32% in our survey).
Most of the surveys performed aimed to screen the adult population only, whereas according to Leboeuf-Yde and Kyvik, investigation of the causes and prevention should be focussed on at a much younger age. In their twin study of 29,424 individuals they found that the one-year prevalence of low back pain amongst the 12-year-olds was 7%, rising to 56% in the 41-year-old age group [13]. In another British study, a much higher one-month prevalence (24%) was found in schoolchildren aged 11–14 years, with girls having higher prevalence than boys [14]. In full accordance with their opinion of focussing on the adolescents as well, the age profile of our survey incorporated individuals from 14–65 years. In the lowest age group we found that the one-month prevalence was 12.5%, whereas in the age group 40–49 it reached 50%.
Upon examining the gender we found that the number of women affected was 9% higher than men. This observation corresponds to the results of similar studies, which suggested that lifting children and pregnancies are the possible factors that contribute to this difference [4, 15]. The difference of LBP prevalence between genders was not due to BMI difference, as the number of overweight and obese individuals was higher amongst male participants.
In the clinical follow-up, 57.5% of the patients had spinal degeneration on the radiographs. In the lack of a universally accepted radiological score for spinal degeneration, comparison is difficult. This relatively high number is not surprising considering that all these patients reported previous LBP, and the average age is higher than that at the time of the questionnaire survey. Average ODI was 35.1% in the overall sample.
Regarding the relationship between BMI and low back pain in our study, lower prevalence rates were detected than in the survey of Fanuele et al., where ODI scores of 39.0, 41.6, 46.6, and 52.2 were measured in the four BMI groups, respectively [16].
Upon examining the presence of hip and knee osteoarthritis, we found that individuals with spinal degenerative disorders have higher hip and knee osteoarthritis prevalence. According to Hassett et al., the progression of knee osteoarthritis is associated with the progression of hip and lumbar spine degeneration [17]. Whether this observation or the higher age or other factors are responsible for co-existing spine, hip and knee pathology needs further investigation. The screening of this coexistence in our view is very important, as candidates for major joint replacement will possibly have inferior functional results and satisfaction rates following surgery with prior lumbar spine pathology.
In this study our aim was to support data on low back pain prevalence and related aspects in a formerly unexamined Central European country. With the presented data we aimed to contribute to low back pain epidemiology within the “Bone and Joint Decade”. Regarding lumbar spine degenerative conditions, further investigations and development of radiological scoring systems are required to make radiological comparison possible.
Acknowledgments
Conflict of interest statement The authors declare that they have no conflicts of interest.
References
- 1.Loney PL, Stratford PW. The prevalence of low back pain in adults: a methodological review of the literature. Phys Ther. 1999;79:384–396. [PubMed] [Google Scholar]
- 2.Palmer KT, Walsh K, Bendall H, Cooper C, Coggon D. Back pain in Britain: comparison of two prevalence surveys at an interval of 10 years. BMJ. 2000;320:1577–1578. doi: 10.1136/bmj.320.7249.1577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schochat T, Jackel WH. Prevalence of low back pain in the population. Rehabilitation. 1998;37:216–223. [PubMed] [Google Scholar]
- 4.Stranjalis G, Tsamadouraki K, Sakas DE, Alamanos Y. Low back pain in a representative sample of Greek population. Spine. 2004;29:1355–1361. doi: 10.1097/01.BRS.0000127181.59012.1C. [DOI] [PubMed] [Google Scholar]
- 5.Waxman R, Tennat A, Helliwell P. A prospective follow-up study of low back pain in the community. Spine. 2000;25:2085–2090. doi: 10.1097/00007632-200008150-00013. [DOI] [PubMed] [Google Scholar]
- 6.Volinn E. The epidemiology of low back pain in the rest of the world: a review of surveys in low and middle-income countries. Spine. 1997;22:1747–1754. doi: 10.1097/00007632-199708010-00013. [DOI] [PubMed] [Google Scholar]
- 7.Leboeuf-Yde C. Body weight and low back pain. A systematic literature review of 56 journal articles reporting on 65 epidemiologic studies. Spine. 2000;25:226–237. doi: 10.1097/00007632-200001150-00015. [DOI] [PubMed] [Google Scholar]
- 8.Offierski CM, MacNab I. Hip-spine syndrome. Spine. 1983;8:316–321. doi: 10.1097/00007632-198304000-00014. [DOI] [PubMed] [Google Scholar]
- 9.Ben-Galim P, Ben-Galim T, Rand N, Haim A, Hipp J, Dekel S, Floman Y. Hip-spine syndrome: the effect of total hip replacement surgery on low back pain in severe osteoarthritis of the hip. Spine. 2007;32:2099–2110. doi: 10.1097/BRS.0b013e318145a3c5. [DOI] [PubMed] [Google Scholar]
- 10.Murata Y, Takahashi K, Yamagata M, Hanaoka E, Moriya H. The knee-spine syndrome. J Bone Joint Surg Br. 2003;85:95–99. doi: 10.1302/0301-620X.85B1.13389. [DOI] [PubMed] [Google Scholar]
- 11.Kellgren J, Lawrence JS. Radiological assessment of osteoarthritis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Leboeuf-Yde C, Klougart N, Lauritzen T. How common is low back pain in the Nordic population? Data from a recent study on a middle-aged general Danish population and four surveys previously conducted in the Nordic countries. Spine. 1996;21:1518–1525. doi: 10.1097/00007632-199607010-00005. [DOI] [PubMed] [Google Scholar]
- 13.Leboeuf-Yde C, Kyvik KO. At what age does low back pain become a common problem? A study of 29424 individuals aged 12–41 years. Spine. 1998;23:228–234. doi: 10.1097/00007632-199801150-00015. [DOI] [PubMed] [Google Scholar]
- 14.Watson KD, Papageorgiou AC, Jones GT, et al. Low back pain in schoolchildren: occurrence and characteristics. Pain. 2002;97:87–92. doi: 10.1016/S0304-3959(02)00008-8. [DOI] [PubMed] [Google Scholar]
- 15.Morgen IM, Pohjanen AI. Low back pain and pelvic pain during pregnancy: prevalence and risk factors. Spine. 2005;30:983–991. doi: 10.1097/01.brs.0000158957.42198.8e. [DOI] [PubMed] [Google Scholar]
- 16.Fanuele JC, Abdu WA, Hanscom B, Weinstein JN. Association between obesity and functional status in patients with spine disease. Spine. 2002;27:306–312. doi: 10.1097/00007632-200202010-00021. [DOI] [PubMed] [Google Scholar]
- 17.Hassett G, Hart DJ, Doyle DY, March L, Spector TD. The relation between progressive osteoarthritis of the knee and long term progression of osteoarthritis of the hand, hip, and lumbar spine. Ann Rheum Dis. 2006;65:623–628. doi: 10.1136/ard.2005.038414. [DOI] [PMC free article] [PubMed] [Google Scholar]