Abstract
Minimally invasive plate osteosynthesis (MIPO) has been advocated as a safe approach to humeral shaft fracture management. We evaluated the reproducibility of this technique in a regional hospital. Thirty-five patients underwent MIPO of humerus shaft fractures. Fifteen patients had an open fracture, six a preoperative radial nerve palsy, and nine a concomitant thoracic, musculoskeletal or vascular injury. At an average 12-month follow-up, 91% of fractures healed after a mean of 12 weeks (range, 8–16). Two infections occurred. Final alignment averaged 4° of varus (range, 5° of valgus to 20° of varus). Active elbow ROM averaged 114° (range, 60–135°) and was less than 100° in nine elbows. Five of six preoperative radial nerve injuries recovered spontaneously. Healing and infection rates in this study are consistent with those reported in the literature. Lower elbow ROM and higher fracture angulation at healing were nevertheless found. MIPO is technically demanding and requires adequate intraoperative imaging and surgical experience in order to obtain adequate fracture alignment. Brachialis muscle scarring and inadequate postoperative rehabilitation may be involved in limited elbow range of motion.
Background
Even though the majority of humeral shaft fractures heal after nonoperative treatment [1], surgical management is required in special circumstances such as polytrauma, open or bilateral fractures, floating elbow, and obesity [2].
Open reduction and internal fixation (ORIF) with plates and screws continues to be considered the gold standard for surgical treatment given its lower complication rate [3, 4] and shorter time to union [5] over intramedullary nailing. Due to concerns about soft tissue dissection required for ORIF, a less invasive technique that allows indirect reduction and percutaneous plating of the anterior humerus has been developed. Early reports have shown excellent healing rates and alignment, and infrequent complications [6–13].
The purpose of this study was to establish the reproducibility of minimally invasive plate osteosynthesis (MIPO) of humeral shaft fractures in a regional hospital in Popayán, Colombia.
Methods
Between June 2004 and January 2007, 35 patients with a fracture of the humeral diaphysis were treated using the MIPO technique at the senior author’s (JMC) institution, a regional hospital in Colombia. Mean age of the 26 males and nine females was 33 years (range, 19–54). Eighteen patients had AO type 12C fractures, and 15 sustained an open fracture of which 13 were associated with gunshot injuries. Nine patients had a concomitant thoracic, musculoskeletal or vascular injury; a radial nerve palsy was present upon admission in six patients (Table 1).
Table 1.
Patient demographics and injury-related data at baseline
| Factors | n | % | Mean | Range | |
|---|---|---|---|---|---|
| Age (years) | 33 | 19–54 | |||
| Gender | Male | 26 | 74 | ||
| Female | 9 | 26 | |||
| Mechanism of injury | GSW | 13 | 37 | ||
| MCC | 7 | 20 | |||
| Fall | 6 | 17 | |||
| MVC | 5 | 14 | |||
| Work | 1 | 3 | |||
| Blunt trauma | 3 | 9 | |||
| Fracture type | Closed | 20 | 57 | ||
| Open type I | 13 | 37 | |||
| Open type III | 2 | 6 | |||
| AO classification | 12A | 7 | 20 | ||
| 12B | 10 | 29 | |||
| 12C | 18 | 51 | |||
| Radial nerve palsy on admission | 6 | 17 | |||
| Additional injuries | Other fracture | 6 | 17 | ||
| Thoracic injury | 2 | 6 | |||
| Vascular injury | 1 | 3 | |||
GSW gunshot wound, MCC motorcycle collision, MVC motor vehicle collision
Surgical technique
Patients are routinely operated upon under general anaesthesia and placed on a conventional table in the supine position. Surgical approach is that described by Livani et al. [9]. Briefly, a limited anterolateral approach is performed over the proximal humerus entering between the deltoid and cephalic vein laterally and the biceps medially. In very proximal fractures, the humerus can be approached via a deltoid split through the anterior fibrous raphé [14]. Distal access to the humerus is obtained through an anterior approach between the biceps and brachioradialis muscles. After the lateral antebrachial cutaneous nerve is identified and medially retracted, the brachialis muscle is longitudinally split and the anterior surface of the humerus exposed. The radial nerve is hereby protected as it courses laterally between the brachialis and brachioradialis. The submuscular tunnel connecting the proximal and distal incisions is created by blunt dissection using either a Cobb retractor or the edge of the plate. In distal fractures that require access to the anterior aspect of the lateral column of the humerus, the brachioradialis and extensor carpi radialis longus origins are subperiosteally reflected anteriorly by using the proximal extension of Kocher’s interval. The radial nerve and posterior interosseous nerve are thereby protected and do not require exposure. Alternatively, four smaller incisions can be performed for plate introduction and percutaneous screw fixation. In the setting of preoperative radial nerve palsy an exploration is performed at the surgeons discretion through an oblique incision on the lateral aspect of the mid-distal humerus as described by Livani et al. [10]. The radial nerve is identified in the anterior muscle compartment between the brachialis and brachioradialis muscles and followed proximal through the intermuscular septum, which is released.
Based on availability, fracture fixation was performed in 26 patients using a 4.5-mm dynamic compression plate (DCP) and in nine patients using a 4.5-mm locking compression plate (LCP) (Synthes, Paoli, Pennsylvania). Previous studies on MIPO of humerus shaft fractures have shown no advantage of broad over narrow plates with respect to rotational stability and hardware failure [9, 10]. Since narrow plates allow a more accurate and less traumatic introduction of hardware they are routinely used in the author’s institution. The plate is pre-bent according to fracture location in order to avoid soft tissue impingement, and is introduced either in a proximal to distal or distal to proximal fashion.
Median plate length was 12 holes for both DCP and LCP plates (range 10–14 for both plates). Fixation was most frequently obtained through the two most proximal and two most distal plate holes. Average working length (length between the most distal screw in the proximal segment and most proximal screw in the distal segment) was 7.6 holes (range 6–8) and average screw density (screw count divided by holes between most distal and most proximal screw of the fracture segment) 0.94 (range 0.67–1) proximally and 0.85 (range 0.67–1) distally. Screws located at the humerus diaphysis were introduced with bicortical purchase in all cases. As screws located at the proximal epiphysis only gained unicortical purchase, locked screws were used at this location in all locked plates when available. The remaining fixation for both locked and conventional plates was obtained with conventional screws in a divergent fashion attempting to increase screw pullout strength (Figs. 1a, b, c, d and e, 2a, b, c, d and e). Locked screws were used for the whole construction in only one 54 year old patient as bone stock was of concern.
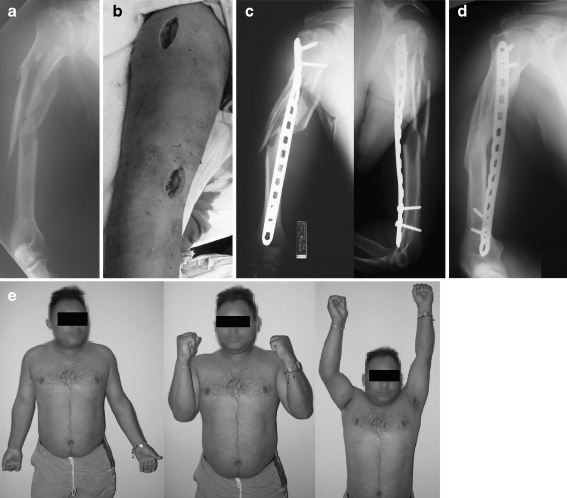
Fig. 1.
(a) Preoperative radiograph of a 30-year-old patient who sustained a closed type AO 12C3 fracture of the proximal third, (b) A proximal anterolateral deltoid split was required due to the proximity of the fracture. An anterior window was used for distal fixation, (c) Immediate postoperative radiographs show fracture fixation using a pre-bent 4.5 LCP with 15° of varus angulation, (d) Healed fracture at eight weeks of follow-up. No change in angulation is observed, (e) Clinical function at eight weeks after surgery. Despite radiographic angulation, clinical alignment is satisfactory
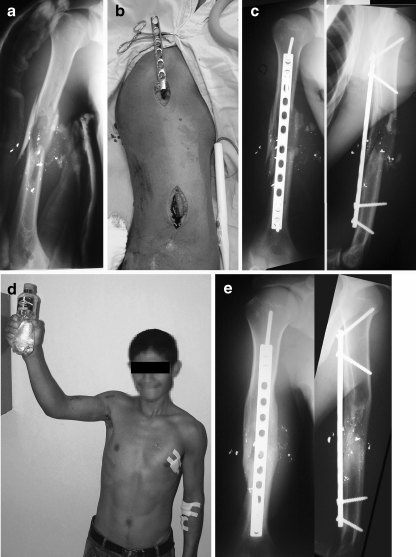
Fig. 2.
(a) Preoperative radiograph of a 28-year-old patient who sustained a gunshot fracture type AO 12C3, (b) Intraoperative photograph showing anterograde sliding of a 12-hole narrow 4.5-mm DC plate, (c) Immediate postoperative radiographs showing adequate alignment and fixation with two proximal and two distal screws, (d) Clinical function one week after surgery, (e) Healed fracture at eight weeks after surgery with adequate alignment and no hardware failure
Antibiotics were routinely used for all patients following the guidelines of the Centre of Disease Control [15]. In essence oxacillin, a first generation cephalosporin or clindamycin was administered in closed fractures at induction of anesthesia, depending on the patient’s allergy history. Antibiotics are continued for 24 hours. In open fractures the above-mentioned scheme was started at patient admission and combined with an aminoglycoside for type II and III fractures and penicillin in the event of major contamination or soft tissue injury. Antibiotics were continued until 72 hours after fracture fixation. Antithrombotic prophylaxis was not used.
Postoperative evaluations
After surgery, patients were immobilised in a sling, while active and active-assisted range of motion began as soon as tolerated. A formal rehabilitation program was not routinely started.
Patients were followed-up at two weekly intervals during the first month and monthly thereafter until bony union occurred. Anterior–posterior and lateral radiographs were taken at monthly intervals. Elbow range of motion was assessed by one of the authors (JMC) at each follow-up visit using a standard goniometer. Arm and forearm longitudinal axes were used for angular measurement and flexion–extension performed with the forearm in neutral pronation–supination.
Fracture union was defined as the presence of bridging callus radiographically visible on at least three cortices. Malunion was defined as healing occurring at more than 15° of angulation. A non-union was diagnosed when healing had not occurred after six months.
Results
Surgery was performed on average 4.8 days (range, 0–8) after injury. All open fractures underwent debridement and irrigation within six hours of admission. Two open fractures underwent fixation within 24 hours of admission, including one open grade IIIC fracture that required revascularisation and one open type I fracture in a patient with minimal soft tissue damage and no concomitant injuries. The remaining open fractures underwent fixation at an average of 6.7 days (range, 3–7) after injury. Fractures were fixed using conventional plating in 26 cases and locked plating in nine cases. Locked plating was used in six of 13 open gunshot fractures. After an average follow-up of 12 months (range, 6–24), 32 fractures (91%) had healed. Average time to healing was 12 weeks (range, 8–16). Three non-unions occurred, two of them in gunshot fractures, which healed after revision with hardware exchange using standard open reduction and internal fixation with autogenous iliac crest bone grafting. One superficial infection occurred which resolved with antibiotic treatment. One patient developed a deep infection that responded to serial debridement and irrigation with culture specific antibiotics. Removal of hardware was not deemed necessary as no signs of loosening were present and progressive bone healing was visible on radiographs. Adequate healing with complete remission of infection was achieved.
Six patients had preoperative radial nerve injuries, five of them after a low velocity and one due to a high velocity gunshot injury. In the latter, the nerve had been transected in a complex injury that involved the brachial artery. Vascular repair was performed, while the nerve injury could not be reconstructed. All nerves associated to low velocity gunshot injuries recovered during the first 12 weeks after surgery. Tendon transfers were required for the non-repairable nerve injury.
Average alignment at final follow-up was 4° of varus, ranging from 5° of valgus to 20° of varus. Thirteen fractures healed with an angulation greater than 5°, all of them in varus alignment. Of these, five, five and two fractures had a final angulation of 7°, 10° and 15°, respectively. Finally, one fracture was defined as a malunion, which healed with 20° of varus angulation. This fracture occurred as a floating elbow injury with a concomitant radius and ulna fracture of the forearm, with no additional complications. Of the two fractures that healed with 15° of varus one occurred as a gunshot fracture and the other during a motorcycle accident (Figs. 1a, b, c, d and e). None of these were associated with complications or concomitant injuries. Despite radiographic deformity, none of the patients with an angulation of 15° or more were willing to undergo corrective surgery due to absence of functional limitation and almost absent clinical deformity.
Active elbow range of motion (ROM) at final follow-up averaged 114° (range, 60–135). Twenty patients obtained full extension, while two, 11 and two patients had an extension lag of 15°, 20° and 30°, respectively. Flexion of at least 130° was obtained in 20 patients. Five, seven, one and two patients had maximal elbow flexion of 120°, 115°, 110° and 90°, respectively. In nine elbows ROM was less than 100°. This loss of ROM occurred after nonunion in two cases, infection in two cases (one of them a high velocity projectile with multiple nerve and vascular injuries), a type I open fracture in one case, and closed fractures in four cases. Seven patients with ROM of less than 100° had an extension lag of 20° and two of 30°; seven patients had maximal flexion of 110° and two of 90°. Postoperative results are summarised in Table 2.
Table 2.
Description of surgical factors, functional outcomes and complications
| Factors | n | % | Mean | Range | |
|---|---|---|---|---|---|
| Time to surgery (days) | 4.83 | 0–8 | |||
| Implant type | 4.5 mm DCP | 26 | 74 | ||
| 4.5 mm LCP | 9 | 26 | |||
| Time to healing (weeks) | 12 | 8–16 | |||
| Alignmenta (frontal plane; in degrees) | 4 | −5 to 20 | |||
| Elbow functiona (degrees) | Active ROM | 114 | 60–135 | ||
| Extension | −9 | −30 to 0 | |||
| Flexion | 123 | 90–135 | |||
| Spontaneous radial nerve recovery | 5 | 83 | |||
| Complications | Nonunion | 3 | 9 | ||
| Infection | 2 | 6 | |||
| Malunion | 1 | 3 | |||
| Additional procedures | Revision and bone grafting | 3 | 9 | ||
| Debridement and irrigation | 1 | 3 | |||
a Negative numbers express valgus and flexion deformity
Discussion
Open reduction internal fixation of humerus shaft fractures is considered the standard for operative treatment of humeral shaft fractures. A large body of literature on this treatment modality reports healing rates that range between 88 and 100% [4, 5, 7, 16–25] (Table 3). Furthermore, adequate fracture reduction is consistently reported, with malunion occurring in less than 5% of cases [4, 5, 7, 16, 20, 23]. Iatrogenic radial nerve injuries have nevertheless been reported to occur in up to 31% of cases [5, 7, 16–19, 21–23] and infections in around 3–7% [5, 7, 16, 17, 19, 20, 22, 23, 25] with one prospective study reporting infections in five (two superficial and three deep) out of 21 fractures (21%) [18]. Extensive soft tissue dissection and radial nerve exposure associated with ORIF may have been possible risk factors for these complications. Additionally, bone grafting is frequently required as an adjunct measure to obtain the high reported union rates, with frequency of between 0 and 49% [4, 5, 16, 18, 20, 21, 23, 24]. Minimally invasive plate osteosynthesis of the humeral shaft has been developed to allow anterior plate and screw stabilisation involving less soft tissue disruption, thereby theoretically improving healing rates and reducing complications like infection and iatrogenic radial nerve palsy [9]. As summarised in Table 3, MIPO has consistently shown healing rates of more than 90%, even in the setting of open fractures. Even though these results are similar to those of ORIF, bone grafting was not used in any of the studies on MIPO. Furthermore, from the pool of 114 fractures treated with MIPO and reported in the literature, iatrogenic radial nerve injury has only been reported in a single case [12] (Table 4).
Table 3.
Summary of minimally invasive plate osteosynthesis (MIPO) and open reduction internal fixation (ORIF) for humerus shaft fractures published in the literature in the last 20 years. Results are grouped into studies with and without open fractures
| References | Technique | n | Age (y)a | Open fracturea | Grafta | Healinga | Maluniona | Infectiona | IRNIa | Elbow ROMb,c |
|---|---|---|---|---|---|---|---|---|---|---|
| [6, 7, 10, 13] | MIPO | Total 36 Rangea 5–13 | 14–64 | 0% | 0% | 100% | 0% (most n.r.) | 0–17% | 0% | 128°–133° |
| [8, 9, 11]; our study | MIPO | Total 78 Rangea 7–35 | 18–75 | 19–43% | 0% | 90–100% | 0–3% | 0–7% | 0% | 114°–133° |
| [7, 18, 20, 21, 26] | ORIF | Total 147 Rangea 16–59 | 19–85 | 0% | 0–49% (most n.r.) | 89–100% | 0% (most n.r.) | 3–5% | 0–31% | 137° (most n.r.) |
| [4, 5, 17, 19, 22–25] | ORIF | Total 494 Rangea 3–156 | 14–93 | 7–36% | 0–29% | 88–97% | 0–5% | 0–21% | 0–5% | 16% minimally impaired; 100% >100°; mean 141°; 13% loss >10° |
IRNI iatrogenic radial nerve injury, ROM range of motion, n.r. not reported
a Range of values reported per study
b Range of mean values reported per study
c Information for ORIF in studies that include open fractures reflects available results from studies in which data could be obtained
Table 4.
Results for minimally invasive plate osteosynthesis (MIPO) for humerus shaft fractures published in the literature
| Description | Reference | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Livani et al. [9] | Apivatthakakul et al. [6] | Pospula et al. [12] | Livani et al. [10] | Jiang et al. [8] | Ziran et al. [13] | Numbela et al. [11] | An et al. [7] | Our study | |
| Year of publication | 2004 | 2005 | 2006 | 2006 | 2007 | 2007 | 2007 | 2009 | 2009 |
| Fractures (n) | 15 | 5 | 12 | 6 | 21 | 8 | 7 | 17 | 35 |
| Female:male ratio (n) | 1:2.8 | n.r. | 1:11 | 1:2 | 1:2 | 1:2.5 | n.r. | 1:2.4 | 1:2.9 |
| Age (years)a | 36 (14–66) | n.r. | 30 (17–46) | 26 (14–42) | 42 (18–75) | 32 (21–64) | >18 | 38 (19–60) | 33 (19–54) |
| AO type (n)b | |||||||||
| 12A | 5 (33) | 2 (40) | n.r. | n.r. | 0 (0) | 3 (36) | 0 (0) | n.r. | 7 (20) |
| 12B | 7 (47) | 0 (0) | 0 (0) | 3 (36) | 5 (71) | 10 (29) | |||
| 12C | 4 (20) | 3 (60) | 21 (100) | 1 | 2 (29) | 18 (51) | |||
| Fracture type (n)b | |||||||||
| Closed | 12 (80) | 5 (100) | n.r. | 6 (100) | 17 (81) | 8 (100) | 5 (71) | 17 (100) | 20 (57) |
| Open | 3 (20) | 0 (0) | 0 (0) | 4 (19) | 0 (0) | 2 (29) | 0 (0) | 15 (43) | |
| Follow-up (months)a | 24 (21–28) | 10 (8–11) | n.r. | 16 (8–22) | 29 (19–37) | 8 (4–14) | 12 (n.r.) | 26 (14–44) | 12 (6–24) |
| Implant DCP:LCP:Recon (n) |
15:0:0 | 4:1:0 | 12:0:0 | 6:0:0 | 0:21:0 | 0:8:0 | 3:0:4 | 17:0:0 | 26:9:0 |
| Time to healing (weeks)a | 10.4 (9–13) | 9.6 (6–18) | 13.6 (12–16) | 11.7 (9–13) | 14.3 (11–20) | n.r. | n.r. | 15.3 (8–24) | 12 (8–16) |
| Nonunion (n)b | 1 (7) | 0 (0) | 0 (0) | 0 (0) | 2 (10) | 0 (0) | 0 (0) | 0 (0) | 3 (9) |
| Infection (n)b | 1 (7) | 0 (0) | 0 (0) | 1 (17) | 1 (5) | 0 (0) | 0 (0) | 0 (0) | 2 (6) |
| PRNI (n)b | 0 (0) | 0 (0) | 0 (0) | 6 (100) | 2 (10) | 1 (13) | 1 (14) | 0 (0) | 6 (17) |
| PRNI recovery (n)b | N/A | N/A | N/A | 6 (100) | 2 (100) | 1 (100) | 0 (0) | N/A | 5 (83) |
| IRNI (n)b | 0 (0) | 0 (0) | 1 (8) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Reoperation due to failure (n)b | 0 (0) | 0 (0) | 0 (0) | 1 (17) | 2 (10) | 0 (0) | 0 (0) | 0 (0) | 2 (6) |
| Coronal angulationb | n.r. | n.r. | 12 (100): <15° | n.r. | 20 (95): <5° | n.r. | 5 (72): <5° | n.r. | 22 (63): <5° |
| Elbow flexion–extension ROMa | 133° (110–135) | n.r. | 119° (100–145) | 128° (120–130) | 117° (n.r.) | 129° (120–135) | n.r. | 133° (100–140) | 114° (60–135) |
n.r. not reported, N/A not applicable, DCP dynamic compression plate, LCP locking compression plate, Recon reconstruction plate, PRNI preoperative radial nerve injury, IRNI iatrogenic radial nerve injury, ROM range of motion
a Numbers in means, range in parenthesis
b Number of cases, percentages in parenthesis
c Positive values represent varus, negative valgus
d Numbers in median, range in parenthesis
One of the major difficulties of MIPO is obtaining adequate fracture reduction. During conventional ORIF fracture reduction is achieved by direct visualisation of the fracture and temporary stabilisation with bone clamps. MIPO on the other hand requires indirect reduction techniques and closed fracture manipulation while plate fixation is obtained. Despite these challenges, malunion rates for MIPO range between 0 and 3%, similar to those reported for ORIF [7, 8, 11, 12] (Table 3).
As mentioned above, most articles on MIPO of humerus shaft fractures report healing rates of 100% for closed fractures [6, 7, 10, 12, 13] and between 90% and 100% for open fractures [8, 9, 11]. Infection rates after MIPO of the humerus range from 0% to 17% in closed fractures and from 0% to 7% in studies that include open fractures [6–13]. With a healing rate of 91% and a prevalence of open fractures of 43%, our study supports MIPO as an effective surgical option for humeral shaft fractures. Furthermore, only one deep and one superficial infection occurred, which represents a 6% infection rate that is consistent with that reported in the literature (Table 4).
An average elbow range of motion of 114° was found in our study, which is similar to the results of Jiang et al. and Pospula et al. who obtained an average 117° and 119°, respectively, after MIPO of humerus shaft fractures [8]. Most studies on MIPO have, however, found average elbow ROM to range from 128° to 134° [7, 9, 10, 13]. Furthermore, elbow ROM after MIPO is consistently reported to be above 100° [7, 9, 10, 12, 13], a minimum value that has been shown to be required for normal elbow function [26]. In our study, nine patients had final elbow range of motion of less than 100°. While four of these nine patients had presented with postoperative complications, including infection in one case, nonunion in two cases and multiple nerve injuries in one case, five patients had non-complicated fracture healing. Therefore, 16% of cases were found to have a significant restriction in elbow range of motion after uncomplicated healing of humerus shaft fractures. Since a flexion contracture of at least 20° was present in these cases, we hypothesise that anterior scaring of the brachialis muscle may be involved, since this muscle is invariably incised during the MIPO technique.
An average alignment of 4° degrees of varus was found in our study, with only 22 fractures (66%) achieving a final coronal alignment within 5° of neutral. More accurate reductions have been reported for MIPO. In a series from Numbela et al., healing was found with less than 5° of angulation in 72% of cases [11], while Jiang et al. obtained a coronal angulation of less than 5° in 95% of cases [8] (Table 4). In our series seven patients had a final coronal angulation of at least 10°. While the humerus is considered to be able to tolerate coronal angulations of up to 20° before becoming functionally limiting [27], our results reflect the technical complexity of obtaining anatomical alignment using a minimally invasive approach. In order to obtain adequate alignment we have paid special attention to three aspects: (1) intraoperatively obtaining adequate abduction of the upper extremity in order to avoid varus malalignment, (2) maintaining 30 degrees of elbow flexion with longitudinal traction of the arm in order to avoid flexion–extension malalignment, and (3) assuring adequate intraoperative images in AP, lateral and oblique views. Furthermore, after obtaining initial fixation with the distal and proximal most screws, absolute certainty about alignment must exist before introducing the middle screws. Correction of angulation is not possible thereafter.
Only one radial nerve injury did not recover after fracture fixation in our study. This injury was secondary to a gunshot fracture graded as open type III C and caused by a high velocity projectile. Despite this particular case, our results further support the findings of Liviani et al. [10] for the use of MIPO in humeral fracture management with the presence of radial nerve injury. In their series of six humerus shaft fractures with radial nerve injury, nerve function recovered in all cases. Interestingly in our series, all radial nerve palsies caused by low velocity gunshot wounds were intact and recovered within 12 weeks of injury. No iatrogenic radial nerve injury occurred in our series, which is consistent with most studies on MIPO. Only one case of an iatrogenic radial nerve palsy following the MIPO technique has been reported in a series of 12 humerus shaft fractures [12] (Table 4).
Conclusions
Our study supports MIPO as a safe and efficient procedure for humeral shaft fracture treatment. Adequate healing and low infection rates can be obtained. Risk of iatrogenic radial nerve injury is low if the appropriate surgical technique is used. Furthermore, fractures accompanied by radial nerve injuries may be adequately fixed using this approach. The high rates of postoperative angulation found in our study reflect the fact that MIPO is a demanding surgical technique that requires adequate imaging and surgical experience. Elbow flexion contracture should also be regarded as a possible complication using this approach and may indicate the need for a formal elbow rehabilitation protocol.
Acknowledgements
We would like to thank Melissa Wilhelmi for reviewing this manuscript.
Conflict of interest The authors declare that they have no conflict of interest.
Contributor Information
Juan M. Concha, Phone: +57-28-399797, FAX: +57-28-234712, Email: jmconcha40@hotmail.com
Alejandro Sandoval, Email: alejo_sandoval@hotmail.com.
Philipp N. Streubel, Phone: +1-314-6230209, FAX: +57-1-6030303, Email: philipp.streubel@aofoundation.org
References
- 1.Sarmiento A, Zagorski JB, Zych GA, Latta LL, Capps CA. Functional bracing for the treatment of fractures of the humeral diaphysis. J Bone Joint Surg Am. 2000;82:478–486. doi: 10.1302/0301-620X.82B7.11561. [DOI] [PubMed] [Google Scholar]
- 2.Green A, Reid JP, DuWayne AC. Fractures of the humerus. In: Baumgaertner MR, Tornetta P, editors. Orthopeadic knowledge update: trauma 3. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2005. pp. 163–180. [Google Scholar]
- 3.Bhandari M, Devereaux PJ, McKee MD, Schemitsch EH. Compression plating versus intramedullary nailing of humeral shaft fractures—a meta-analysis. Acta Orthop. 2006;77:279–284. doi: 10.1080/17453670610046037. [DOI] [PubMed] [Google Scholar]
- 4.McCormack RG, Brien D, Buckley RE, McKee MD, Powell J, Schemitsch EH. Fixation of fractures of the shaft of the humerus by dynamic compression plate or intramedullary nail. A prospective, randomised trial. J Bone Joint Surg Br. 2000;82:336–339. doi: 10.1302/0301-620X.82B3.9675. [DOI] [PubMed] [Google Scholar]
- 5.Chapman JR, Henley MB, Agel J, Benca PJ. Randomized prospective study of humeral shaft fracture fixation: intramedullary nails versus plates. J Orthop Trauma. 2000;14:162–166. doi: 10.1097/00005131-200003000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Apivatthakakul T, Arpornchayanon O, Bavornratanavech S. Minimally invasive plate osteosynthesis (MIPO) of the humeral shaft fracture. Is it possible? A cadaveric study and preliminary report. Injury. 2005;36:530–538. doi: 10.1016/j.injury.2004.05.036. [DOI] [PubMed] [Google Scholar]
- 7.An Z, Zeng B, He X, Chen Q, Hu S. Plating osteosynthesis of mid-distal humeral shaft fractures: minimally invasive versus conventional open reduction technique. Int Orthop. 2009 doi: 10.1007/s00264-009-0753-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jiang R, Luo CF, Zeng BF, Mei GH. Minimally invasive plating for complex humeral shaft fractures. Arch Orthop Trauma Surg. 2007;127:531–535. doi: 10.1007/s00402-007-0313-z. [DOI] [PubMed] [Google Scholar]
- 9.Livani B, Belangero WD. Bridging plate osteosynthesis of humeral shaft fractures. Injury. 2004;35:587–595. doi: 10.1016/j.injury.2003.12.003. [DOI] [PubMed] [Google Scholar]
- 10.Livani B, Belangero WD, Castro de Medeiros R. Fractures of the distal third of the humerus with palsy of the radial nerve: management using minimally-invasive percutaneous plate osteosynthesis. J Bone Joint Surg Br. 2006;88:1625–1628. doi: 10.1302/0301-620X.88B12.17924. [DOI] [PubMed] [Google Scholar]
- 11.Numbela BX, Aceves LH, Gonzalez AB, Castro CT. Minimally invasive surgery in diaphyseal humeral fractures with helicoidal plate. One year result in seven patients. Acta Ortop Mex. 2007;21:239–246. [PubMed] [Google Scholar]
- 12.Pospula W, Abu Noor T. Percutaneous fixation of comminuted fractures of the humerus: initial experience at Al Razi hospital, Kuwait. Med Princ Pract. 2006;15:423–426. doi: 10.1159/000095487. [DOI] [PubMed] [Google Scholar]
- 13.Ziran BH, Belangero W, Livani B, Pesantez R. Percutaneous plating of the humerus with locked plating: technique and case report. J Trauma. 2007;63:205–210. doi: 10.1097/01.ta.0000231870.11908.3e. [DOI] [PubMed] [Google Scholar]
- 14.Gardner MJ, Griffith MH, Dines JS, Briggs SM, Weiland AJ, Lorich DG. The extended anterolateral acromial approach allows minimally invasive access to the proximal humerus. Clin Orthop Relat Res. 2005;434:123–129. doi: 10.1097/01.blo.0000152872.95806.09. [DOI] [PubMed] [Google Scholar]
- 15.Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol. 1999;20:250–278. doi: 10.1086/501620. [DOI] [PubMed] [Google Scholar]
- 16.Paris H, Tropiano P, Clouet D'orval B, Chaudet H, Poitout DG. Fractures of the shaft of the humerus: systematic plate fixation. Anatomic and functional results in 156 cases and a review of the literature. Rev Chir Orthop Reparatrice Appar Mot. 2000;86:346–359. [PubMed] [Google Scholar]
- 17.Singisetti K, Ambedkar M. Nailing versus plating in humerus shaft fractures: a prospective comparative study. Int Orthop. 2009 doi: 10.1007/s00264-009-0813-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Changulani M, Jain UK, Keswani T. Comparison of the use of the humerus intramedullary nail and dynamic compression plate for the management of diaphyseal fractures of the humerus. A randomised controlled study. Int Orthop. 2007;31:391–395. doi: 10.1007/s00264-006-0200-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chao TC, Chou WY, Chung JC, Hsu CJ. Humeral shaft fractures treated by dynamic compression plates, Ender nails and interlocking nails. Int Orthop. 2005;29:88–91. doi: 10.1007/s00264-004-0620-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chiu FY, Chen CM, Lin CF, Lo WH, Huang YL, Chen TH. Closed humeral shaft fractures: a prospective evaluation of surgical treatment. J Trauma. 1997;43:947–951. doi: 10.1097/00005373-199712000-00014. [DOI] [PubMed] [Google Scholar]
- 21.Dabezies EJ, Banta CJ, 2nd, Murphy CP, d'Ambrosia RD. Plate fixation of the humeral shaft for acute fractures, with and without radial nerve injuries. J Orthop Trauma. 1992;6:10–13. [PubMed] [Google Scholar]
- 22.Heim D, Herkert F, Hess P, Regazzoni P. Surgical treatment of humeral shaft fractures—the Basel experience. J Trauma. 1993;35:226–232. doi: 10.1097/00005373-199308000-00009. [DOI] [PubMed] [Google Scholar]
- 23.Lin J. Treatment of humeral shaft fractures with humeral locked nail and comparison with plate fixation. J Trauma. 1998;44:859–864. doi: 10.1097/00005373-199805000-00019. [DOI] [PubMed] [Google Scholar]
- 24.Niall DM, O'Mahony J, McElwain JP. Plating of humeral shaft fractures—has the pendulum swung back? Injury. 2004;35:580–586. doi: 10.1016/j.injury.2003.10.021. [DOI] [PubMed] [Google Scholar]
- 25.Rodriguez-Merchan EC. Compression plating versus Hackethal nailing in closed humeral shaft fractures failing nonoperative reduction. J Orthop Trauma. 1995;9:194–197. doi: 10.1097/00005131-199506000-00003. [DOI] [PubMed] [Google Scholar]
- 26.Morrey BF, Askew LJ, Chao EY. A biomechanical study of normal functional elbow motion. J Bone Joint Surg Am. 1981;63:872–877. [PubMed] [Google Scholar]
- 27.Klenerman L. Fractures of the shaft of the humerus. J Bone Joint Surg Br. 1966;48:105–111. [PubMed] [Google Scholar]