Abstract
The purpose of this study was to evaluate the medium-term follow-up results of a series of ten perilunate dislocations treated operatively at least three weeks following injury. The intervals from injury to treatment of the delayed and the chronic groups were four weeks (range, three to six weeks) and 17 weeks (range, 11–25 weeks), respectively. The average follow-up time was 90 months. Surgical procedures included open reduction, internal fixation, grafting, ligament repair, and external fixation. Clinical function was evaluated by the Cooney clinical scoring system. The radiological assessment included the radiolunate angle, scapholunate angle, the revised carpal height ratio, and presence or absence of midcarpal arthritis. In the delayed group, there were two excellent, one good and one poor results. The average postoperative clinical score was 81 (good). In the chronic group, there were four good, one fair, and one poor results. At the last follow-up, the average postoperative clinical score was 76.7 (good). Our results indicate that open reduction and internal fixation can be applied in the treatment of delayed and some of the chronic perilunate dislocations and achieve satisfactory results.
Introduction
Perilunate dislocations represent approximately 10% of all wrist injuries and are diagnosed late in up to 25% of cases. These dislocations can be classified into three phases [1]. The acute phase is defined as within the first week after injury, the delayed phase is the period between the seventh and the 45th day, and after 45 days the injury is considered to be in the chronic phase [1]. Most authors agree that early open reduction and internal fixation are necessary to obtain satisfactory results [2]. However, late treatment of unreduced perilunate dislocations is difficult and controversial [3]. Wrist fusion was recommended by Wagner [4] and proximal row carpectomy was advised by Campbell et al. [5] for old dislocations. The time limit for open reduction was recommended to be six weeks by MacAusland [6] and two months by Inoue and Shionoya [7], while Green and O’Brien [3] and Fisk [8] recommended open reduction should be attempted regardless of time delay.
The purpose of this study was to assess the results of open reduction of delayed and chronic perilunate dislocations and to compare these results with previous reports; some comments on their treatment are also proffered.
Patients and methods
Between 1998 and 2004, 12 patients with delayed and chronic perilunate dislocations (isolated scaphoid-lunate dissociations were excluded from this study) that had been left untreated for a minimum of three weeks after the initial injury were treated at our hospital. Misdiagnosis and failed conservative treatment at the local hospital were the main reasons for the late presentation. Two patients were lost to follow-up, leaving ten patients available for review. The patients were divided into two groups based on the time from injury to treatment. The delayed group consisted of four patients who were treated between three and six weeks (average, four weeks). The chronic group included six patients who were treated between 11 and 25 weeks (average, 17 weeks). The time from injury to treatment for all cases ranged from three weeks to 25 weeks.
At presentation, these patients had significant limitation of wrist motion and moderate or severely incapacitating wrist pain. The patient diagnosed with volar lunate dislocations had the syndrome of chronic median nerve compression. Standard posteroanterior and lateral views of the wrist were used for preoperative and postoperative radiological evaluation. The injuries included nine great arc injuries (eight trans-scaphoid perilunate dislocations, one trans-scaphoid trans-radial styloid perilunate dislocation) and one lesser arc injury (volar lunate dislocation).
Open reduction was performed through the dorsal approach in nine cases; a combined volar and dorsal approach was performed in the lunate dislocation case. In chronic injuries, reduction was not easy to achieve. The following procedures can help to solve this problem. The first step was to thoroughly remove the scar tissue in the carpal joint space and the fracture sites; then, longitudinal manual distraction to the hand was applied. Under manual distraction, a leverage technique was used to reduce the dislocated lunocapitate joint and scaphoid fracture. During leverage reduction, the cartilage of the carpal bones should be carefully protected. The condition of the articular cartilage of the midcarpal joints was carefully inspected during the surgery. Scaphoid fractures were fixed with cannulated screws (3.5 mm) in four cases and Herbert screws (2.7 mm) in five cases. Iliac bone graft (in four cases) or vascularised distal radius bone graft (in two cases) was used in cases with massive comminution or bone resorption. Nonabsorbable suture materials were used to repair the scapho-lunate interosseous ligament and luno-triquetral interosseous ligament. After repairing the ligaments, the luno-triquetral or the scapho-lunate intervals were stabilised with Kirschner wires. Reasorbable sutures were used to repair the capsule rents. After completing the reduction and internal fixation, the wrist external fixator (Pennig wrist fixator, Orthofix Srl, Italy) was applied in a slight distraction mode with the wrist in the neutralising position (Fig. 1). The fixator was mounted on two predrilled pins in the distal radial diaphysis and near the base into the second metacarpal from the radial side via limited approaches. The proximal ball joint was adjusted to the radiocarpal joint space and the distal ball joint was set to the so-called centre of rotation of the wrist joint (between capitate and lunate).The patients were started on a range of motion exercises on the third postoperative day. The external fixation was continued for six to eight weeks.
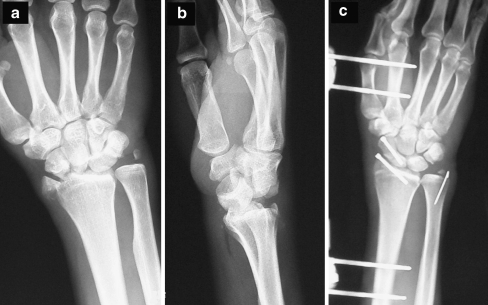
Fig. 1.
Posteroanterior (PA) (a) and lateral (b) views of a dorsal trans-radial styloid perilunate dislocation. c PA postoperative view (case 2)
Results
The patients included nine men and one woman. Right wrists were injured in seven and left wrists in three cases. The dominant side was affected in eight and the nondominant side in two patients. The age ranged from 21 to 58 years (average, 35 years) at the time of injury. The average follow-up period was 90 months (range, 55–121). At follow-up, the patients were evaluated according to the clinical scoring system described by Cooney et al. [9] (Table 1). The radiological outcome included the revised carpal height ratio, radiolunate angle (RL), scapholunate angle (SL), and presence or absence of midcarpal arthritis. In cases 1, 6, 7, 8 and 10, loaded clenched-fist radiographs were performed to evaluate the scapho-lunate and luno-triquetral interval. The results of treatment are summarised in Table 2.
Table 1.
Clinical scoring chart
| Category and description | Number of patients |
|---|---|
| Pain (25 points) | |
| None | 25 |
| Mild occasional (climatic or with heavy use) | 20 |
| Moderate (with normal use, not at rest) | 10 |
| Severe, constant | 0 |
| Range of motion (25 points): Flexion+Extention (degrees) | |
| >140 | 25 |
| 100–140 | 20 |
| 70–99 | 15 |
| 40–69 | 10 |
| <40 | 0 |
| Grip strength (25 points) | |
| Normala | 25 |
| Diminished but >50% of normal | 15 |
| Less than 50% of normal | 0 |
| Activities (25 points) | |
| Same activities | 25 |
| Restricted activities caused by injured wrist | 15 |
| Change of work or sports caused by injured wrist | 0 |
Excellent ≥95 points; good ≥75 points; fair ≥60 points; poor <60 points
aNormal is the contralateral side (minus or plus 10% depending on dominance) if not disabled. If disabled, then reference is made to normal estimated values with respect to age
Table 2.
Results of the treatment
| Parameter | Case | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
| Age (years) | 33 | 37 | 21 | 27 | 33 | 29 | 27 | 30 | 44 | 58 |
| Diagnosis | TSPL | TSTR | TSPL | TSPL | TSPL | TSPL | TSPL | TSPL | TSPL | MNC LD |
| Interval | 4 | 3 | 4 | 5 | 25 | 14 | 15 | 11 | 18 | 16 |
| Treatment | EF ORIF LTLR | ORIF EF | EF OR BG | EF ORIF BG | EF ORIF VBG |
ORIF LTLR BG EF | ORIF LTLR BG EF | EF ORIF LTLR |
EF ORIF VBG | OR SLLR LTLR EF |
| Follow-up | 55 | 108 | 79 | 83 | 102 | 96 | 92 | 98 | 121 | 65 |
| Pain | 20 | 20 | 25 | 10 | 20 | 20 | 20 | 10 | 20 | 20 |
| ROM | 15 | 20 | 20 | 15 | 15 | 15 | 20 | 10 | 20 | 20 |
| GS | 25 | 25 | 25 | 15 | 15 | 25 | 25 | 15 | 15 | 25 |
| Activity | 25 | 25 | 25 | 15 | 25 | 25 | 25 | 15 | 15 | 25 |
| Total | 85 | 90 | 95 | 55 | 75 | 85 | 90 | 50 | 70 | 90 |
| SL/RL angles | 46/−9 | 48/5 | 50/8 | 65/15 | 55/8 | 57/−6 | 50/4 | 74/20 | 56/7 | 48/−5 |
TSPL trans-scaphoid perilunate fracture-dislocation, TSTR trans-scaphoid trans-radial styloid perilunate fracture-dislocation, MNC median nerve compression, LD lunate dislocation, interval interval between injury and surgery, EF external fixation, ORIF open reduction and internal fixation, LTLR luno-triquetral ligament repair, BG bone grafting, VBG vascularised bone grafting, OR open reduction, SLLR scapho-lunate ligament repair, ROM range of motion, GS grip strength, SL scapho-lunate, RL radio-lunate
The delayed group
There were two excellent results, as well as one good and one poor. The average postoperative clinical score was 81 (good). Three patients were free of pain, while one patient reported moderate pain. Mean range of motion (flexion and extension) was 112 ± 23 degrees. The mean grip strength was 35 ± 15 kg (grip strength was evaluated with the Jamar dynamometer) and was 90% of the grip strength of normal hands of all patients (39 ± 7 kg). All patients (two farmers, one bus driver, one office worker) returned to their previous work. The average time away from work was 17 weeks (range, 12–23).
One of the four cases developed post-traumatic midcarpal arthritis. None of the patients demonstrated any sign of avascular necrosis of the proximal pole of the scaphoid and the lunate. In case 1, the luno-triquetral interval in the loaded clenched views were in the normal range (less than 3 mm). The average SL and RL angles in the early postoperative period (after the removal of the external fixator) were 48.5 and −5.0 degrees, respectively. At the last follow-up, average SL and RL angles were 52.3 and 4.8 degrees, respectively. Revised carpal height ratio was 1.56 in the early postoperative period (without external fixation) and decreased to 1.54 at the last follow-up.
The chronic group
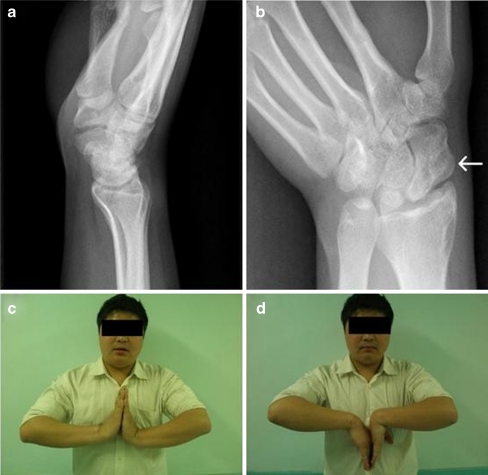
There were four good results, one fair, and one poor. At the last follow-up, the average postoperative clinical score was 76.7 (good). One patient reported moderate pain, one patient reported mild pain, and four patients were free of pain. Mean range of motion was 93 ± 28 degrees (Fig. 2). The mean grip strength was 29 ± 16 kg and was 72% of the grip strength of the normal hand. Five patients (two farmers, one construction worker, one office worker, and one manual worker) returned to their previous work and one patient retired (case 13, manual worker). The average time away from work was 28 weeks (range, 25–35).
Fig. 2.
Lateral (a) and scaphoid axial (b) views of case 7 at 92 months follow-up (the screw had been removed two years after the initial surgery). The arrow points at the iliac bone graft. The range of motion of the injured right wrist was satisfactory (c, d)
Postoperative midcarpal arthritis developed in three cases. In case 6, 7, 8 and 10, the scapho-lunate and luno-triquetral in loaded clenched views were in the normal range. The average SL and RL angles in the early postoperative period were 55.1 and 6.7 degrees, respectively. At the last follow-up, average SL and RL angles were 56.7 and 4.7 degrees, respectively. Revised carpal height ratio was 1.52 in the early postoperative period (after the removal of the external fixator) and decreased to 1.49 at the last follow-up.
Discussion
A delay in diagnosis and treatment has adverse effects on the prognosis of perilunate dislocations [10]. The treatment options for delayed and chronic cases included proactive procedures such as open reduction and internal fixation, or such salvage procedures as proximal row corpectomy and primary wrist arthrodesis. Mahmut et al. reported six cases of delayed dorsal transscaphoid perilunate fracture-dislocations (average interval between injury and surgery, 3.7 weeks) which were treated by open reduction and internal fixation and achieved one excellent, one good and four fair results [11]. Takami et al. reported four good results in four cases of chronic perilunate dislocations (average interval between injury and surgery, 12 weeks) treated by open reduction [12]. In the study reported by Inoue et al. [7], there were three good, one fair, and two poor results in the six chronic cases (average interval between injury and surgery, 16 weeks) treated by open reduction and internal fixation. In the other 16 cases (average interval between injury and surgery, 14 months) treated by proximal row carpectomy, there were no good results. The authors stated that open reduction should be attempted in cases with perilunate dislocations delayed up to two months and that proximal carpectomy should be considered in cases seen later than two months. In this study, open reduction, screw internal fixation for scaphoid fractures, bone grafting, ligament repair, and external fixation using a wrist external fixator were employed to treat delayed and chronic cases untreated up to 25 weeks and achieved good results in both of the two groups. In the delayed group, both of the average wrist scores (81) and the mean wrist flexion-extension arc (112 ± 23 degrees) were better than the results reported by the previous study [11]. In the chronic group, the average wrist score (76.7) was similar to the value reported by Takami et al. [12]. There was no incapacitating pain in our series. Grip strength in our study averaged 72% of the contralateral side, which is similar to findings reported by others [7, 11–13]. We believe that pain relieving, restoration of the normal anatomy of the carpal bones and intercarpal stability were the main factors that helped to restore the grip strength.
However, there is no consensus for the upper time limit at which an initially unrecognised perilunate dislocation could be treated by open reduction with a satisfactory result [6–9]. In this study, we achieved satisfactory results in cases delayed up to 25 weeks. In that case, the condition of the cartilage of the lunate, the scaphoid and the capitate were found to be good. In another two cases (cases 4 and 8) which were treated five and 11 weeks after the initial injury, the results turned out to be poor. During the surgery, it was found that there was severe contusion on the cartilage of the scaphoid and the lunate. At the last follow-up, advanced post-traumatic arthritis of the midcarpal joints developed and the patients were in constant pain. With no exception, cases with excellent or good results in this study had satisfactory cartilage condition of the midcarpal joints when evaluated during the operation. These results indicate that the time delay was not the only factor determining the final result, the status of the cartilage of the midcarpal joints could play a more important role and should be considered as a prerequisite for a proactive procedure such as open reduction and internal fixation. Therefore, several surgical alternatives should be prepared preoperatively, and the final procedure should be determined based on the cartilage condition of the midcarpal joints at operation. The international cartilage repair society grading systems (ICRS) could be used to grade the severity of the cartilage damage (grade 0, normal; grade I, nearly normal: superficial lesions, softening, fissures; grade II, abnormal: lesions extending to <50% of cartilage depth; grade III, severely abnormal: lesions extending to >50% of cartilage depth; grade IV, severely abnormal: complete defect) [14]. We believe that in low-grade cartilage damage (grade 0, grade I and grade II), a proactive procedure should be attempted. While in high-grade damage (grade III and grade IV), a salvage procedure such as proximal row carpectomy or wrist arthrodesis should be considered.
Intercarpal instability can be assessed by measurement of the SL and RL angles. In this study, at the early postoperative and last follow-ups, the values of the SL and RL angles in all of the cases remained in the range of the normal population. Gradual loss of intercarpal reduction over time results in intercarpal instability and the increase of these angles [15]. Fracture reduction and union, interosseous ligament repair or reconstruction play critical roles in the restoration of the intercarpal stability. In this study, scaphoid fractures were treated by open reduction and internal fixation. If the fracture was severely comminuted or signs of bone resorption were present, a compression resistant anterior iliac wedge graft was inserted to restore the scaphoid length and to prevent hump back deformity. In three cases where the fractures were located in the proximal pole and the time from injury was comparatively long, vascularised distal radius bone grafts based on 1,2 intercompartmental supraretinacular artery were inserted to promote bone union. There was no fracture nonunion in this study. The severity of ligamentous injury was evaluated in the surgery and classified according to the Geissler classification system [16]. In the grade 3 and 4 injuries (entire rupture of the ligaments), ligamentous repair was performed with transosseous suture techniques using non-absorbable material. The follow-up radiographic evaluation (loaded clenched-fist views) showed that the values of the scapho-lunate and luno-triquetral interval were in the normal range (less than 3 mm).
In the delayed group, the revised carpal height ratio was 1.56 in the early postoperative period, 1.54 at the last follow-up and remained in the range of the general population (1.57 ± 0.06) [17]. In the chronic group, during the early postoperative period the value was 1.52 and at the last follow-up the value was 1.49, which was slightly less than the normal value. These results were comparatively better than the previous reported results [11]. The loss of articular cartilage at the midcarpal joints leads to the decrease of this carpal ratio and has adverse effects on the wrist function [17]. Therefore, it is important to protect the articular cartilage postoperatively, especially in delayed and chronic cases in which the joint capsule around the wrist is contracted and the articular cartilage is inevitably under compression after reduction. In this study, after open reduction and ligamentous repair, we used a wrist external fixator in a neutralising mode to block the axial load on the cartilage of the injured proximal carpal row and to maintain normal carpal alignment during the initial stages of ligament healing.
Under the protection of the external fixation, functional rehabilitation of the hand, wrist, forearm, and elbow could be started on the third day postoperatively. The patients could actively flex and extend the wrist around the ball joints of the fixator. This is important for recovery of wrist motion. In this study, the range of motion of the wrist was satisfactory. We believe that this it was at least partially related to the early postoperative functional rehabilitation which is an advantage of the application of the wrist external fixator over plaster.
In conclusion, proactive procedures such as open reduction and internal fixation can be employed to achieve satisfactory results in cases with delayed and chronic perilunate dislocations. Both proactive and salvage procedures should be prepared preoperatively, and proactive procedures should be attempted if the cartilage condition of the midcarpal joints is found to be good during operation; otherwise, salvage procedures such as proximal row carpectomy or wrist arthrodesis should be considered. Bone grafting should be performed in cases with severe comminution and signs of bone resorption. Vascularised bone grafting should be considered when the scaphoid fracture is located at the proximal pole or the interval between the initial injury and the treatment is long. Ligamentous repair is important to restore the normal relationship between the midcarpal bones and to prevent late intercarpal instability. A wrist external fixator should be routinely employed to provide protection for the wrist cartilage postoperatively, and functional rehabilitation should be started as early as possible under the protection of the external fixation.
Contributor Information
Liang Kailu, Email: liang-kai-lu@163.com.
Xiang Zhou, Email: xiangzhou15@hotmail.com.
Huang Fuguo, Phone: +86-28-85422430, FAX: +86-28-85423438, Email: huangfuguo2009@hotmail.com.
References
- 1.Herzberg G, Comtet JJ, Linscheid RL, Amadio PC, Cooney WP, Stalder Perilunate dislocations and fracture dislocations: a multicenter study. J Hand Surg Am. 1993;18(5):768–779. doi: 10.1016/0363-5023(93)90041-Z. [DOI] [PubMed] [Google Scholar]
- 2.Inoue G, Imaeda T. Management of trans-scaphoid perilunate dislocations. Herbert screw fixation, ligamentous repair and early wrist mobilization. Arch Orthop Trauma Surg. 1997;116(6–7):338–340. doi: 10.1007/BF00433985. [DOI] [PubMed] [Google Scholar]
- 3.Green DP, O’Brien ET. Open reduction of carpal dislocations: indications and operative techniques. J Hand Surg Am. 1978;3(3):250–265. doi: 10.1016/s0363-5023(78)80089-6. [DOI] [PubMed] [Google Scholar]
- 4.Wagner CJ. Perilunar dislocations. J Bone Joint Surg Am. 1956;38-A(6):1198–1207. [PubMed] [Google Scholar]
- 5.Campbell RD, Jr, Lance EM, Yeoh CB. Lunate and perilunar dislocations. J Bone Joint Surg Br. 1964;46:55–72. [PubMed] [Google Scholar]
- 6.MacAusland WR. Perilunar dislocation of the carpal bones and dislocation of the lunate bone. Surg Gynecol Obstet. 1944;79:256–259. [Google Scholar]
- 7.Inoue G, Shionoya K. Late treatment of unreduced perilunate dislocations. J Hand Surg Br. 1999;24(2):221–225. doi: 10.1054/jhsb.1998.0003. [DOI] [PubMed] [Google Scholar]
- 8.Fisk GR. The wrist. J Bone Joint Surg Br. 1984;66(3):396–407. doi: 10.1302/0301-620X.66B3.6373778. [DOI] [PubMed] [Google Scholar]
- 9.Cooney WP, Bussey R, Dobyns JH, Linscheid RL. Difficult wrist fractures. Perilunate fracture-dislocations of the wrist. Clin Orthop Relat Res. 1987;214:136–147. [PubMed] [Google Scholar]
- 10.Siegert JJ, Frassica FJ, Amadio PC. Treatment of chronic perilunate dislocations. J Hand Surg Am. 1988;13(2):206–212. doi: 10.1016/S0363-5023(88)80049-2. [DOI] [PubMed] [Google Scholar]
- 11.Komurcu M, Kürklü M, Ozturan KE, Mahirogullari M, Basbozkurt M. Early and delayed treatment of dorsal transscaphoid perilunate fracture–dislocations. J Orthop Trauma. 2008;22(8):535–540. doi: 10.1097/BOT.0b013e318183eb23. [DOI] [PubMed] [Google Scholar]
- 12.Takami H, Takahashi S, Ando M, Masuda A. Open reduction of chronic lunate and perilunate dislocations. Arch Orthop Trauma Surg. 1996;115(2):104–107. doi: 10.1007/BF00573451. [DOI] [PubMed] [Google Scholar]
- 13.Weir IG. The late reduction of carpal dislocations. J Hand Surg Br. 1992;17(2):137–139. doi: 10.1016/0266-7681(92)90073-B. [DOI] [PubMed] [Google Scholar]
- 14.Brittberg M, Winalski CS. Evaluation of cartilage injuries and repair. J Bone Jt Surg Am. 2003;85-A(Suppl 2):58–69. doi: 10.2106/00004623-200300002-00008. [DOI] [PubMed] [Google Scholar]
- 15.Hildebrand KA, Ross DC, Patterson SD, Roth JH, MacDermid JC, King GJ. Dorsal perilunate dislocations and fracture-dislocations: questionnaire, clinical, and radiographic evaluation. J Hand Surg Am. 2000;5:1069–1079. doi: 10.1053/jhsu.2000.17868. [DOI] [PubMed] [Google Scholar]
- 16.Geissler WB, Freeland AE, Savoie FH, McIntyre LW, Whipple TL. Intracarpal soft-tissue lesions associated with an intra-articular fracture of the distal end of the radius. J Bone Joint Surg Am. 1996;78:357–365. doi: 10.2106/00004623-199603000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Nattrass GR, King GJ, McMurtry RY, Brant RF. An alternative method for determination of the carpal height ratio. J Bone Joint Surg Am. 1994;76(1):88–94. doi: 10.2106/00004623-199401000-00011. [DOI] [PubMed] [Google Scholar]