Abstract
The choice between reamed and unreamed intramedullary nailing for the treatment of open and closed tibial fractures is an ongoing controversy. We carried out a comprehensive search strategy. Six eligible randomised controlled trials were included. Three reviewers independently assessed methodological quality and extracted outcome data. Analyses were performed using Review Manager 5.0. The results showed lower risks of tibial fracture nonunion and implant failures with reamed nails compared to unreamed nails in closed tibial fractures [relative risk (RR): 0.41, 95% confidence interval (CI): 0.21–0.89, P = 0.008 for nonunion and RR: 0.35, 95% CI: 0.22–0.56, P < 0.0001 for implant failures], but no statistical differences in risk reduction of malunion, compartment syndrome, embolism and infection. Our results suggested no statistical differences in risk reduction of all the complications evaluated between reamed and unreamed nails in open tibial fractures. In conclusion, our study recommended reamed nails for the treatment of closed tibial fractures. But the choice for open tibial fractures remains uncertain.
Introduction
Tibial fractures are the most common long bone fractures [1]. Every year, patients with tibial fractures remain in hospital for a total of 569,000 hospital days and incur 825,000 physician visits in the USA [2]. The aims of treatment for tibial shaft fractures are re-establishing pre-injury anatomy and function with lower complication rates [3]. Several methods have been used for treatment of this fracture, including compression plating, reamed or unreamed intramedullary nailing and external fixation [4, 5].
Among them, intramedullary nail fixation has been shown to be an effective method for treating both open and closed tibial fractures [6–8]. However, the choice between two alternative intramedullary nailing approaches, reamed or unreamed, is an ongoing controversy. Reamed intramedullary nailing has the advantage of providing optimal biomechanical stability; however, reaming of the medullary canal may also lead to endosteal blood flow damage, bone necrosis, compartment syndrome and infection [9–11]. In theory, unreamed intramedullary nailing does not have the above-mentioned problems associated with reaming, but the mechanical stability may limit its application. Both of them have strong rationales; which is better?
Several review articles have addressed the use of reamed and unreamed intramedullary nailing for the treatment of open and closed tibial shaft fractures; however, the search methodology and the criteria for including studies may bias the results [12–14]. To date, there are still no published systematic reviews and meta-analyses comparing the use of reamed and unreamed intramedullary nailing for open and closed tibial fractures. Recently, a number of high quality randomised controlled trials have addressed this issue [15–20]. However, the optimal intramedullary nailing approach for open and closed tibial fractures is still unclear. We therefore carried out a systematic review and meta-analysis of randomised controlled trials to compare reamed and unreamed intramedullary nailing for the treatment of open and closed tibial fractures.
Materials and methods
Search strategy
This study was conducted with a prospectively developed protocol, which included the study objective, search strategy, study eligibility criteria, and the methods of data extraction and statistical analysis. The reporting of the study’s results was in accordance with the Quality of Reporting of Meta-analyses (QUOROM) conference statement [21].
To identify published and unpublished reports of relevant randomised studies, we searched relevant electronic databases, including MEDLINE (1966–May 2009), EMBASE (1980–May 2009), Science Citation Index (1981–May 2009), Cochrane Central Register of Controlled Trials (CENTRAL) and Cochrane Database of Systematic Reviews (Cochrane Library, issue 2, 2009). We also searched for unpublished trials and those in progress using repositories of clinical trials, including the National Institute of Health (May 2009), the National Research Register (May 2009) and Current Controlled Trials (May 2009). Searches were not restricted by year of publication or language. The search strategy used the terms: “tibial* AND fracture* AND intramedullary”. Reference lists of all studies included were scanned to identify additional potentially relevant studies. Two reviewers independently screened the titles and abstracts of identified papers, and full text copies of all potentially relevant studies were obtained.
Eligibility criteria and study outcomes
We included all randomised trials if they compared reamed and unreamed intramedullary nailing for the treatment of tibial fractures.
The primary outcome was fracture nonunion. The secondary outcomes were malunion, failure of implants, compartment syndrome, infection and embolism. We undertook a subgroup analysis for open fractures and closed fractures.
Data extraction
Data were extracted independently by three reviewers; disagreements were resolved by discussion. To quantify the level of agreement between reviewers, a κ statistic was calculated. The κ statistic is a chance-corrected proportional index, with values ranging from +1 (perfect agreement) to –1 (complete disagreement). Information extracted included personal information, methodology, details on interventions and reported outcomes.
Study quality assessment
We assessed the methods of every study according to the Cochrane Handbook for Systematic Reviews of Interventions, including reporting of randomisation method, allocation concealment, blinding of outcome assessment and completeness of follow-up.
Statistical analysis
Relative risk (RR) was used as the summary statistic to perform statistical analysis of dichotomous variables, and the weighted mean difference (WMD) was used to analyse continuous variables. Both were reported with 95% confidence intervals (CI). We used the χ2 statistic to assess heterogeneity between trials and the I2 statistic to assess the extent of inconsistency. A P value of 0.05 was used as the cut-off value to determine statistical significance. We used a fixed-effects model for calculations of summary estimates and their 95% CI unless there was significant heterogeneity, in which case results were confirmed using a random-effects model. Meta-analyses were carried out by using Review Manager 5.0 provided by The Cochrane Collaboration.
Results
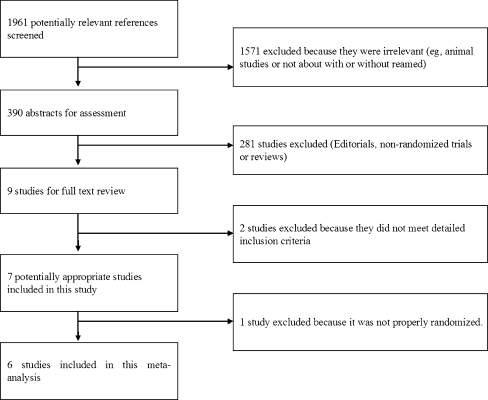
Of the1,961 references screened, six studies were included in the final analysis (Fig. 1) [15–20]. Five trials reported fracture nonunion, malunion and failure of implants as outcomes [15–17, 19, 20]; three trials reported infection [16, 17, 20]; and two trials reported embolism [16, 17]. All of the trials reported compartment syndrome (Table 1). Three studies only included closed fractures [15, 16, 18], one study only included open fractures [17] and two studies included both [19, 20]. However, one study [19], which included both fractures, only contained one open fracture in the reamed group, thus it was not suitable for subgroup analysis. During analysis, we excluded the open fracture patient and treated it as a study that only included closed fractures. There were 1,698 tibias analysed, 872 of which were treated with reamed intramedullary nailing (Table 1).
Fig. 1.
Flow chart of study selection
Table 1.
| Study (country) | Year | No. of tibias | No. of two fracture types tibias (open:closed) | Age (years) (mean) | Outcomes |
|---|---|---|---|---|---|
| Court-Brown et al. [15] (UK) | 1996 | 25/25 | 0:25/0:25 | 35/36.1 | Nonunion, malunion, compartment syndrome, failure of implants |
| Blachut et al. [16] (Canada) | 1997 | 77/64 | 0:77/0:64 | 35/35 | Nonunion, infection, failure of implants, malunion, compartment syndrome, embolism |
| Keating et al. [17] (Canada) | 1997 | 50/44 | 50:0/44:0 | 37a | Nonunion, infection, failure of implants, malunion, compartment syndrome, embolism |
| Nassif et al. [18] ( USA) | 2000 | 24/25 | 0:24/0:25 | 36.1a | Compartment syndrome |
| Larsen et al. [19] (Norway) | 2004 | 21/16 | 0:21/0:16 | 41/47.5 | Nonunion, malunion, failure of implants, infection, compartment syndrome |
| Bhandari et al. [20] (Canada, USA and Netherlands) | 2008 | 675/652 | 221:454/214:438 | 38.9/39.5 | Nonunion, infection, compartment syndrome, failure of implants |
aMean age of all participants
The methodological quality of the studies included is summarised in Table 2. All studies were randomised controlled trials. The κ coefficient on the agreement of the studies included was 0.91, suggesting good agreement between reviewers in data extraction.
Table 2.
| Study | Randomisation | Allocated concealment | Blinding | Withdrawal/lost to follow-up (%) |
|---|---|---|---|---|
| Court-Brown et al. (1996) [15] | Adequate | Unclear | Unclear | 0 |
| Blachut et al. (1997) [16] | Adequate | Unclear | Unclear | 0 |
| Keating et al. (1997) [17] | Adequate | Unclear | Unclear | 6 |
| Nassif et al. (2000) [18] | Adequate | Unclear | Unclear | 0 |
| Larsen et al. (2004) [19] | Adequate | Unclear | Unclear | 5 |
| Bhandari et al. (2008) [20] | Adequate | Adequate | Adequate | 7 |
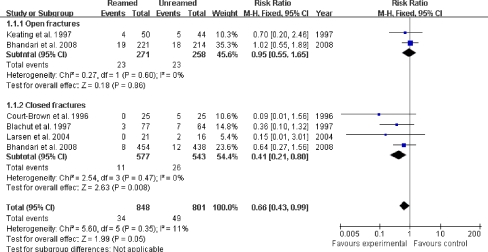
Fracture nonunion
Of the five trials reporting nonunion as an outcome (n = 1649), three trials only included closed fractures and one trial included both open and closed fractures. In the closed fracture subgroups, reamed intramedullary nailing was associated with a 59% risk reduction in fracture nonunion compared with unreamed (RR: 0.41, 95% CI: 0.21–0.89, P = 0.008; Fig. 2). The direction of effect was consistent in all studies and heterogeneity tests indicated no statistical evidence of heterogeneity. Of the two trials in the open fracture subgroup, a fixed-effects model was used. There was no statistical evidence of heterogeneity by heterogeneity tests. The result showed no significantly different nonunion rate between reamed and unreamed groups (RR: 0.95, 95% CI: 0.55–1.65, P = 0.86; Fig. 2). Ignoring fracture types, a fixed-effects model indicated a higher rate of fracture nonunion in the unreamed intramedullary nailing group (RR: 0.66, 95% CI: 0.43–0.99, P = 0.05; Fig. 2).
Fig. 2.
Comparison of nonunion rates between reamed and unreamed nails
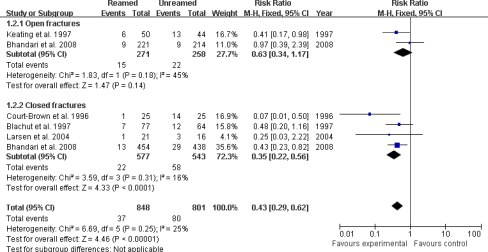
Failure of implants
Five studies provided data about implant failures (n = 1,649), three trials only included closed fractures and one trial included both open and closed fractures. In the closed fracture subgroups, reamed intramedullary nailing was associated with a 65% risk reduction in implant failures compared with unreamed nails (RR: 0.35, 95% CI: 0.22–0.56, P < 0.0001; Fig. 3). The subgroup analysis of nail failure and screw failure in the closed fracture group showed that reamed nails significantly decreased screw failure risk compared with unreamed nails (RR: 0.34, 95% CI: 0.21–0.55, P < 0.0001). However, there was no difference in nail failures between the reamed and unreamed groups in closed fractures (RR: 0.91, 95% CI: 0.13–6.62, P = 0.93). Of the two trials in the open fracture subgroup, no significant difference in implant failures was found between the reamed and unreamed groups (RR: 0.63, 95% CI: 0.34–1.17, P = 0.14; Fig. 3). And the subgroup analysis of nail failure and screw failure in the open fracture group also indicated no significant difference between the two subgroups. Heterogeneity tests showed no statistical evidence of heterogeneity in the above analysis.
Fig. 3.
Comparison of implant failure rates between reamed and unreamed nails
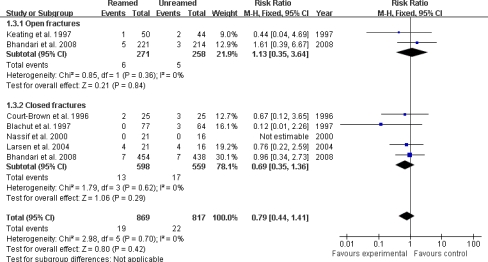
Compartment syndrome
Of the six trials reporting nonunion as an outcome (n = 1,686), four trials only included closed fractures and one trial included both open and closed fractures. In the closed fracture subgroups, there was no significantly different compartment syndrome rate between the reamed and unreamed groups (RR: 0.69, 95% CI: 0.35–1.36, P = 0.29; Fig. 4). Of the two trials in the open fracture subgroup, no significant difference in risk reduction of compartment syndrome was found between the reamed and unreamed groups (RR: 0.84, 95% CI: 0.35–3.64, P = 0.84; Fig. 4). Heterogeneity tests indicated no statistical evidence of heterogeneity.
Fig. 4.
Comparison of compartment syndrome rates between reamed and unreamed nails
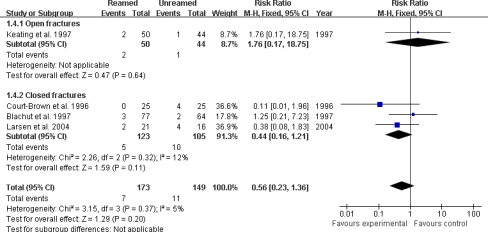
Malunion
Four studies provided data about malunion (n = 322), three trials only included closed fractures and one trial only included open fractures. In the closed fracture subgroups, there was no significantly different incidence of compartment syndrome between the reamed and unreamed groups (RR: 0.44, 95% CI: 0.16–1.21, P = 0.11; Fig. 5). One study included open fractures and also showed no different compartment syndrome rate between the reamed and unreamed groups (P = 0.64; Fig. 5). There was no statistical evidence of heterogeneity by heterogeneity tests.
Fig. 5.
Comparison of malunion rates between reamed and unreamed nails
Only two studies reported embolism as an outcome [16, 17]. We had not carried out subgroup analysis, because there were limited studies. The pooled data analysis indicated a significantly different embolism rate between the reamed and unreamed groups (RR: 0.94, 95% CI: 0.11–7.84, P = 0.96). When we compared infection rates both in open fractures and closed fractures, there was no significant difference between the reamed and unreamed groups. There was no statistical evidence of heterogeneity by heterogeneity tests.
Discussion
Principle findings
Our meta-analysis has shown that reamed intramedullary nailing significantly reduced the risk of nonunion and implant failures (especially screw failures) compared with unreamed nails in closed tibial fractures. There was no statistical difference in compartment syndrome, malunion and infection rates between reamed and unreamed nails in closed fractures. In open tibial shaft fractures, our analysis results have not found any statistically different risk reduction of nonunion, implant failures, compartment syndrome, malunion and infection between reamed and unreamed nails. Because only two studies reported embolism, we had not carried out subgroup analysis. The results demonstrated no statistical difference between the reamed and unreamed groups. Overall, our findings support reamed intramedullary nailing for the treatment of closed tibial fractures.
Strengths and limitations
Our meta-analysis differs from earlier analyses in several ways [14, 22]. We included several recently published studies targeted at reamed and unreamed intramedullary nailing for the treatment of tibial shaft fractures [18–20]. Bhandari et al. [22] compared reamed and unreamed tibial and femoral nails together, making the validity questionable. Forster et al. [14] only included three studies and chose odds ratios, which are mainly used for retrospective study, and they compared reamed and unreamed techniques for open and closed tibial fractures together. The clinical heterogeneity limited the power of results. Our study is strengthened by the comprehensive search and broad clinical eligibility criteria (including publications in any language) and by including only randomised controlled trials. We undertook a subgroup analysis, so the clinical consistency is high and the results are more reliable.
However, all meta-analyses are subject to potential bias and our study was not excluded. Firstly, the number of the studies included and participants in the open fracture subgroup was relatively small. This limited the power of analysis results. Secondly, methodological limitations resulted from variations in operative technique and treatment protocols between trials investigating the same technology. A differential expertise bias might have existed in our study. Thirdly, although we have undertaken a comprehensive search strategy, we have not included any unpublished trials. A publication bias might exist. Inconsistent reporting of outcomes across trials also raises the possibility of selective reporting bias [23].
Clinical implications
The choice of reamed versus unreamed intramedullary nailing for the treatment of open and closed tibial fractures remains controversial. Our meta-analysis showed that reamed intramedullary nailing had a lower risk of nonunion in closed tibial fractures. Several reasons may account for this. Firstly, reaming allows the use of larger diameter nails, providing better resistance to fatigue failure and increasing endosteal contact with better stability [24]. Secondly, reaming increases the periosteum and surrounding soft tissue envelope hyperaemic reaction which will revascularise the diaphysis by a centripetal blood supply, though it may destroy the endosteal blood flow. However, the soft tissue and periosteum damage in open fractures would interrupt the process of revascularisation. This may be the reason why our analysis results showed no statistical difference in nonunion rates between reamed and unreamed nailing in open fractures. Finally, reaming material deposited at the fracture site is thought to have an osteogenic effect, much like a bone graft [25]. There was also evidence of a lower relative risk of implant failures in closed tibial fractures. This is mainly due to reaming increasing the contact area between the nails and the bone surface. Thus our analysis results recommend that reamed intramedullary nailing is a safer procedure with lower nonunion rates than unreamed nailing for closed tibial fractures. However, our study has not found any statistical difference between reamed and unreamed nails for open tibial fractures. More large randomised trials should be performed to clarify the choice.
Acknowledgment
We thank all the patients and clinical researchers who were involved in the publications we mentioned in this article.
References
- 1.Mashru RP, Herman MJ, Pizzutillo PD. Tibial shaft fractures in children and adolescents. J Am Acad Orthop Surg. 2005;13:345–352. doi: 10.5435/00124635-200509000-00008. [DOI] [PubMed] [Google Scholar]
- 2.Russell TA. Fractures of the tibial diaphysis. In: Levine AM, editor. Orthopaedic knowledge update: trauma, vol 1. Rosemont: American Academy of Orthopaedic Surgeons; 1996. [Google Scholar]
- 3.Gregory P, Sanders R. The treatment of closed, unstable tibial shaft fractures with unreamed interlocking nails. Clin Orthop Relat Res. 1995;315:48–55. [PubMed] [Google Scholar]
- 4.Kádas I, Magyari Z, Vendégh Z, Gloviczki B. Changing the treatment to reduce complication rate in open tibial fractures. Int Orthop. 2008 doi: 10.1007/s00264-008-0670-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fan CY, Chiang CC, Chuang TY, Chiu FY, Chen TH. Interlocking nails for displaced metaphyseal fractures of the distal tibia. Injury. 2005;36:669–674. doi: 10.1016/j.injury.2004.10.018. [DOI] [PubMed] [Google Scholar]
- 6.Busse JW, Morton E, Lacchetti C, Guyatt GH, Bhandari M. Current management of tibial shaft fractures: a survey of 450 Canadian orthopedic trauma surgeons. Acta Orthop. 2008;79:689–694. doi: 10.1080/17453670810016722. [DOI] [PubMed] [Google Scholar]
- 7.Schmidt AH, Finkemeier CG, Tornetta P., 3rd Treatment of closed tibial fractures. Instr Course Lect. 2003;52:607–622. [PubMed] [Google Scholar]
- 8.Lee YS, Lo TY, Huang HL. Intramedullary fixation of tibial shaft fractures: a comparison of the unlocked and interlocked nail. Int Orthop. 2008;32:69–74. doi: 10.1007/s00264-006-0271-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Petrisor B, Anderson S, Court-Brown CM. Infection after reamed intramedullary nailing of the tibia: a case series review. J Orthop Trauma. 2005;19:437–441. doi: 10.1097/01.bot.0000161542.93624.8d. [DOI] [PubMed] [Google Scholar]
- 10.Grundnes O, Reikerås O. Acute effects of intramedullary reaming on bone blood flow in rats. Acta Orthop Scand. 1993;64:203–206. doi: 10.3109/17453679308994571. [DOI] [PubMed] [Google Scholar]
- 11.Ochsner PE, Baumgart F, Kohler G. Heat-induced segmental necrosis after reaming of one humeral and two tibial fractures with a narrow medullary canal. Injury. 1998;29(Suppl 2):B1–B10. doi: 10.1016/S0020-1383(98)80057-0. [DOI] [PubMed] [Google Scholar]
- 12.Coles CP, Gross M. Closed tibial shaft fractures: management and treatment complications. A review of the prospective literature. Can J Surg. 2000;43:256–262. [PMC free article] [PubMed] [Google Scholar]
- 13.Rand N, Mosheiff R, Liebergall M. The role of intramedullary nailing in modern treatment of open fractures of the tibia and femur. Mil Med. 1994;159:709–713. [PubMed] [Google Scholar]
- 14.Forster MC, Bruce AS, Aster AS. Should the tibia be reamed when nailing? Injury. 2005;36:439–444. doi: 10.1016/j.injury.2004.09.030. [DOI] [PubMed] [Google Scholar]
- 15.Court-Brown CM, Will E, Christie J, McQueen MM. Reamed or unreamed nailing for closed tibial fractures. A prospective study in Tscherne C1 fractures. J Bone Joint Surg Br. 1996;78:580–583. [PubMed] [Google Scholar]
- 16.Blachut PA, O’Brien PJ, Meek RN, Broekhuyse HM. Interlocking intramedullary nailing with and without reaming for the treatment of closed fractures of the tibial shaft. A prospective, randomized study. J Bone Joint Surg Am. 1997;79:640–646. doi: 10.2106/00004623-199705000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Keating JF, O’Brien PJ, Blachut PA, Meek RN, Broekhuyse HM. Locking intramedullary nailing with and without reaming for open fractures of the tibial shaft. A prospective, randomized study. J Bone Joint Surg Am. 1997;79:334–341. doi: 10.2106/00004623-199703000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Nassif JM, Gorczyca JT, Cole JK, Pugh KJ, Pienkowski D. Effect of acute reamed versus unreamed intramedullary nailing on compartment pressure when treating closed tibial shaft fractures: a randomized prospective study. J Orthop Trauma. 2000;14:554–558. doi: 10.1097/00005131-200011000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Larsen LB, Madsen JE, Høiness PR, Øvre S. Should insertion of intramedullary nails for tibial fractures be with or without reaming? A prospective, randomized study with 3.8 years' follow-up. J Orthop Trauma. 2004;18:144–149. doi: 10.1097/00005131-200403000-00003. [DOI] [PubMed] [Google Scholar]
- 20.Bhandari M, Guyatt G, Tornetta P, 3rd, Schemitsch EH, Swiontkowski M, Sanders D, Walter SD. Randomized trial of reamed and unreamed intramedullary nailing of tibial shaft fractures. J Bone Joint Surg Am. 2008;90:2567–2578. doi: 10.2106/JBJS.G.01188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF. Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Quality of Reporting of Meta-analyses. Lancet. 1999;354:1896–1900. doi: 10.1016/S0140-6736(99)04149-5. [DOI] [PubMed] [Google Scholar]
- 22.Bhandari M, Guyatt GH, Tong D, Adili A, Shaughnessy SG. Reamed versus nonreamed intramedullary nailing of lower extremity long bone fractures: a systematic overview and meta-analysis. J Orthop Trauma. 2000;14:2–9. doi: 10.1097/00005131-200001000-00002. [DOI] [PubMed] [Google Scholar]
- 23.Chan AW, Hróbjartsson A, Haahr MT, Gøtzsche PC, Altman DG. Empirical evidence for selective reporting of outcomes in randomized trials: comparison of protocols to published articles. JAMA. 2004;291:2457–2465. doi: 10.1001/jama.291.20.2457. [DOI] [PubMed] [Google Scholar]
- 24.Chapman MW. The effect of reamed and nonreamed intramedullary nailing on fracture healing. Clin Orthop Relat Res. 1998;355(Suppl):S230–S238. doi: 10.1097/00003086-199810001-00023. [DOI] [PubMed] [Google Scholar]
- 25.Reynders PA, Broos PL. Healing of closed femoral shaft fractures treated with the AO unreamed femoral nail. A comparative study with the AO reamed femoral nail. Injury. 2000;31:367–371. doi: 10.1016/S0020-1383(00)00005-X. [DOI] [PubMed] [Google Scholar]