Abstract
Patellar instability is a common clinical problem affecting a young, active population. A large number of procedures have been described to treat patellar instability. We present the clinical results in a case series of 25 medial patellofemoral ligament reconstructions in 21 patients with up to 30 months follow-up (mean: 7.3). Reconstruction was performed using either the gracilis or semitendinosus tendon autograft. The Tegner activity score improved overall from 3 to 4.4 at follow-up and the mean follow-up Kujala score was 87 (range: 55–100). No patella redislocations were observed. Five patients (20%) required a manipulation under anaesthetic but subsequently regained a satisfactory range of motion. Medial patellofemoral reconstruction with both gracilis and semitendinosus tendon graft using a longitudinal tunnel technique provided good post-operative stability restoring the primary soft tissue restraint to pathological lateral patellar displacement with no complications of post-operative patellar fracture.
Introduction
Patellar instability is a common clinical problem affecting a young, active population. A large number of procedures have been described to treat patellar instability with varying clinical results [1, 2] including fully arthroscopic procedures [3]. Reconstruction of the medial patellofemoral ligament (MPFL) has become popular in the treatment of chronic patellar instability. It has been shown that the MPFL is the primary medial restraining structure to lateral displacement of the patella and contributes up to 80% of the medial restraining forces to the patella [4, 5]. In cases of full patellar dislocation biomechanical studies have shown the MPFL has limited ability to lengthen [6]. The capacity of the MPFL to heal is also limited, which results in increased medial laxity of the patellar retinacular structures [7, 8].
The MPFL is a condensation of the medial retinaculum, which originates from the medial aspect of the patella and inserts into the adductor tubercle of the medial femoral condyle. The numerous described reconstructive techniques have the aim to restore this medial tether of the patella. Various tendon sources have been described including gracilis [9, 12], hamstring [10, 14], semitendinous [11, 13], partial patellar tendon [15] and allografts or artificial tendons [16]. In addition, grafts have been fixed using a variety of techniques including patellar drill holes, sutures, suture anchors and interference screws at the femoral condyle. Generally, the clinical results of MPFL reconstruction have been reported as successful. Redislocation rates of 0–10% have been reported (Table 1). For techniques involving transverse patellae drill holes, a small incidence of patellar fracture has been reported [12, 17].
Table 1.
Study details and results from clinical follow-up studies of MPFL reconstruction with Kujala score used as a clinical end-point
| Study | Graft | N | Follow-up | Redislocation | Kujala score |
|---|---|---|---|---|---|
| Deie et al. 2005 [22] | Semitendinosus transfer | 39 | 5 years | 0% | 92 |
| Schöttle et al. 2005 [19] | Semitendinosus autograft | 15 | 4 years | 1/15 | 87 |
| Steiner et al. 2006 [21] | Adductor tendon autograft | 34 | 2–10 years | 0% | 90 |
| Drez et al. 2001 [23] | Various grafts | 19 | 32 months | 1/19 | 88 |
| Christiansen et al. 2008 [12] | Gracilis | 44 | 12–32 months | 1/44 | 84 |
We report the clinical results of a case series of 25 patients treated with MPFL reconstruction for chronic patellar instability using a surgical technique with either gracilis or semitendinosus autograft fixed in a longitudinal patellar drill hole with an interference screw in the femoral condyle. We hypothesise that results are comparable to previously published results in studies of MPFL reconstruction and in addition the longitudinal patellar drill hole would avoid the potential complication of patellar fracture.
Patients and methods
This study included 21 patients who were consecutively operated on by a single surgeon. Patients underwent surgery from November 2001 to March 2008. All patients who underwent a primary MPFL reconstruction in this period were included in the study. Any revision procedures or patients who had undergone previous surgery except diagnostic arthroscopy were excluded. The mean follow-up was 31 months (range: 3–87 months). The patients’ median age was 24 years (range: 17–44 years). There were 12 male and nine female patients. All patients had chronic patellar instability with a minimum of two total patellar dislocations. Exclusion criteria for this operation were:
Significant patellofemoral degenerative changes (grade III–IV)
Significant patellar malalignment with an increased Q angle [tibial tubercle to trochlear groove distance (TTTG) greater than 15 mm]
Severe trochlear dysplasia (Dejour type B or C)
Four patients had bilateral procedures. Patients were evaluated by preoperative and follow-up Tegner activity scores. At follow-up a subjective Kujala score was obtained. Clinical data included incidence of recurrent subluxation or dislocations. Any complications and re-operations were noted.
A three incision technique was employed. Firstly, the gracilis or semitendinosus tendon was harvested through a 2- to 3-cm incision over the pes anserinus using a tendon stripper. A second incision was made over the medial border of the patella along the proximal two thirds. A dental burr was used to access the superior aspect of the medial patella border and a similar hole was made in the inferior aspect of the medial border to enable a longitudinal tunnel to be created in the patella. The patellar tunnel was ‘banana shaped’ in the longitudinal plane to reduce “killer” turns as the tendon enters and leaves the patella. A No. 0 Ethibond suture was then passed along this longitudinal patella tunnel. The harvested tendon autograft was passed along the tunnel to form a tendon loop. A final incision was then made over the medial femoral condyle. The adductor tubercle was exposed and identified at the medial femoral condyle. The natural MPFL insertion point is just distal to the tubercle (Figs. 1 and 2).
Fig. 1.
A burr is used to fashion a longitudinal tunnel in the medial side of the patellar
Fig. 2.
The gracilis or semitendinosus tendon autograft is looped through the patellar tunnel before being tunnelled to the medial femoral condyle
A guide wire was then passed across the distal femur at this point. It is important to site this wire correctly and the graft must undergo isometry testing prior to definitive fixation. Excessive tension at flexion should be avoided and can be resolved by a slightly more distally placed guide wire. A 7-mm drill hole was then made at the femoral condyle.
The looped tendon free ends were passed under the fascia to the femoral drill hole. Distal fixation was achieved using a titanium interference screw once the tension of the reconstruction had been tested through the arc of motion. The ligament was initially tensioned in 20° of flexion. The appropriate tension in the reconstruction was gauged by observing patellar tracking at arthroscopy using a superolateral portal through a full range of motion. It is important not to over-constrain the reconstruction that can result in chondral overload in flexion (Figs. 3, 4 and 5).
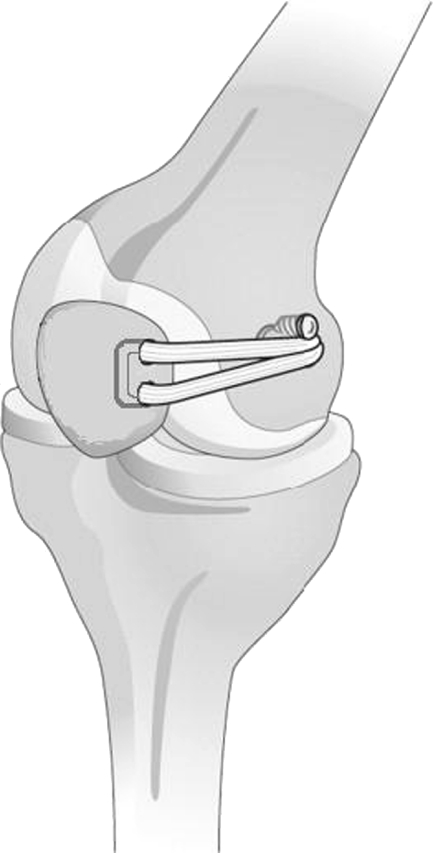
Fig. 3.
The autograft is tunnelled to the natural insertion of the MPFL on the adductor tubercle of the medial femoral condyle
Fig. 4.
An interference screw is used to fix the graft to the MPFL insertion on the medial femoral condyle
Fig. 5.
Surgical technique of MPFL reconstruction. The gracilis or semitendinosus tendon is looped through the longitudinal patellar tunnel, passed under the fascia and fixed in a drill hole in the medial femoral condyle with an interference screw
Patients were rehabilitated in a knee brace locked in extension for the first three weeks with partial weight-bearing. The brace was then unlocked for the next three weeks with a range of motion of 0–90°. After six weeks free activity was allowed. Controlled sports activities after three months and contact sports after six months were allowed. More recently the rehabilitation was accelerated. The initial cases used distal fixation of a blind-ended tunnel with suturing of the graft onto itself. However, after problems with stiffness the more recent cases have used interference screw fixation, which allowed more aggressive mobilisation. These patients were rehabilitated in an unlocked brace with range of motion 0–90° straightaway.
Results
Subjective assessment revealed that 75% of patients had no or occasional slight pain with a mean post-operative Kujala score of 87 points (range: 55–100 points). The Tegner activity score improved overall from 3 points (range: 0–6 points) to 4.4 points (range: 1–7 points) at follow-up. One patient had a reduction in her activity level score and four patients had the same score post-operatively with all the other patients showing an improvement in their scores. Three patients were performing competitive sports at follow-up with one patient competing in international motor-cross competitions. No patellar redislocations occurred although one patient was lost to follow-up.
There were seven re-operations. Five patients required a manipulation under anaesthetic because their flexion ability was less than 90° but subsequently regained a satisfactory range of motion. One patient developed a neuroma related to the hamstring harvest, which was excised. Another patient underwent a washout for infection.
Discussion
The optimal surgical treatment for chronic patellar instability remains controversial. It is generally now accepted that reconstruction of the MPFL is a good procedure to correct chronic patellar instability particularly in patients who have had a history of previous patellar dislocations. However, the choice of graft and surgical technique remains a subject of continued discussion. This study, which contained a patient group with MPFL reconstruction, had a zero redislocation rate. Our follow-up Kujala score of 87 points is comparable to other studies using this score, ranging from 82 to 92 points (Table 1). Some studies have shown poorer outcomes in patients with cartilage damage at the time of surgery [12, 18]. Certainly in our patients, those that had significant lesions noted at operation were the ones with persistent pain post-operatively. Patient selection is extremely important in considering the indications for MPFL reconstructive surgery. The primary indication for MPFL reconstruction is patellar instability and it is important to distinguish common patellofemoral pain syndrome from anterior pain associated with patellar instability. Within the patient cohort with patellar instability three important exclusion criteria must be enforced before consideration of MPFL reconstruction. As already discussed it has been shown that chondral damage on the articular surface of the patella leads to poor surgical outcomes. In the face of advanced patellar chondral damage (grade III–IV) then a patellofemoral off-loading procedure such as a Fulkerson’s osteotomy is more appropriate.
Secondly, a patient’s longitudinal alignment must be carefully assessed. An increased Q angle can be reflected in an increased TTTG measured on the axial cuts of a computed tomography (CT) scan. Patients with a markedly increased torsional profile again would benefit from a distal realignment procedure and not an MPFL reconstruction in isolation. None of the patients in our study had an additional procedure done in combination with their MPFL reconstruction. It is our practice to perform a Fulkerson’s osteotomy in isolation in those patients with significant malalignment. In these patients distal realignment usually achieves satisfactory patellar stability as the underlying anatomical abnormality has been addressed. This cohort of patients have different pathological conditions to the post-traumatic dislocation patients who have injured their MPFL and develop patellar instability due to this rather than an underlying bony abnormality.
Most patients do not require an additional MPFL reconstruction but occasionally this can be performed as a separate procedure if necessary. The use of additional procedures combined with MPFL reconstruction is controversial. In one study [19], a tibial tuberosity transfer was performed when the TTTG distance was greater than 15 mm. However, to date, no studies have indicated any need for additional procedures combined with MPFL reconstruction in cases of increased Q angles. A recent study [20] instigated a management plan to separate those patients with significant malalignment from those with normal alignment. The patients with evidence of lateral patellar subluxation on CT scan were offered a distal realignment procedure using the Elmslie-Trillat or Roux-Goldwaite procedure. All other patients underwent proximal soft tissue medial MPFL reconstruction. Although the study only looked at a small number of cases, [23] it was shown that both groups had significant improvement for both treatment arms emphasising that patients with significant patellar maltracking would benefit from distal realignment, otherwise MPFL reconstruction would be adequate. This reinforces our second exclusion criterion as previously discussed. Finally, the presence of severe trochlear dysplasia again should be a contraindication to isolated MPFL reconstruction. Significant trochlear dysplasia with a completely flattened trochlea (Dejour type B) or an absent or severely dysplastic medial femoral condyle (Dejour type C) would be a contraindication to MPFL reconstruction in our study. These patients would undergo a trochleoplasty possibly combined with an MPFL reconstruction. One study [19], however, did not find poorer results in patients with mild trochlear dysplasia who underwent MPFL reconstruction but did mention that this fact needs further attention in a larger study group. In addition, another study [21] showed MPFL reconstruction provided excellent long-term relief and prevents recurrent dislocation in patients with patellar instability and femoral trochlea dysplasia. Consequently, this exclusion criterion needs further evaluation in future projects. However, it remains clear that patient selection is vital to ensure optimal surgical outcomes in MPFL reconstruction.
Five patients (20%) required a manipulation under anaesthetic. Initially the post-operative rehabilitation started with three weeks in a locked brace in extension, as there were concerns with the strength of the fixation of the graft to the medial femoral condyle using a blind-ended tunnel with suturing of the graft to itself. However, when fixation was achieved with an interference screw mobilisation was started straightaway in an unlocked brace and post-operative stiffness became less of a problem. No patients suffered a post-operative patellar fracture, a reported complication in some case series that used a transverse patellar tunnel technique. Our case series used a technique involving a longitudinal patellar tunnel and consequently avoided this particular surgical complication.
This study is limited by investigating the short-term clinical results after MPFL reconstruction. However, the early results with a mean follow-up of 31 months (2.6 years) with MPFL reconstruction with both gracilis or semitendinosus tendon autografts using a longitudinal patella tunnel technique showed a zero redislocation rate and subjective patient outcome scores compatible with other reported techniques. Patient selection remains vitally important to ensure optimal surgical outcomes.
References
- 1.Davis DK, Fithian DC. Techniques of medial retinacular repair and reconstruction. Clin Orthop Relat Res. 2002;402:38–52. doi: 10.1097/00003086-200209000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Hughston JC. Subluxation of the patella. J Bone Joint Surg Am. 1968;50:1003–1026. [PubMed] [Google Scholar]
- 3.Haspl M, Cicak N, Klobucar H, Pecina M. Fully arthroscopic stabilization of the patella. Arthroscopy. 2002;18(1):E2. doi: 10.1053/jars.2002.30023. [DOI] [PubMed] [Google Scholar]
- 4.Hautamaa PV, Fithian DC, Kaufman KR, Daniel DM, Pohlmeyer AM. Medial soft tissue restraints in lateral patellar instability and repair. Clin Orthop Relat Res. 1998;349:174–182. doi: 10.1097/00003086-199804000-00021. [DOI] [PubMed] [Google Scholar]
- 5.Desio SM, Burks RT, Bachus KN. Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med. 1998;26:59–65. doi: 10.1177/03635465980260012701. [DOI] [PubMed] [Google Scholar]
- 6.Mountney J, Senavongse W, Amis AA, Thomas NP. Tensile strength of the medial patellofemoral ligament before and after repair or reconstruction. J Bone Joint Surg Br. 2005;87:36–40. [PubMed] [Google Scholar]
- 7.Sallay PI, Poggi J, Speer KP, Garrett WE. Acute dislocation of the patella. A correlative pathoanatomic study. Am J Sports Med. 1996;24:52–60. doi: 10.1177/036354659602400110. [DOI] [PubMed] [Google Scholar]
- 8.Nomura E. Classification of lesions of the medial patello-femoral ligament in patellar dislocation. Int Orthop. 1999;23:260–263. doi: 10.1007/s002640050366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schöttle P, Schmeling A, Romero J, Weiler A. Anatomical reconstruction of the medial patellofemoral ligament using a free gracilis autograft. Arch Orthop Trauma Surg. 2009;129:305–309. doi: 10.1007/s00402-008-0712-9. [DOI] [PubMed] [Google Scholar]
- 10.Anbari A, Cole BJ. Medial patellofemoral ligament reconstruction: a novel approach. J Knee Surg. 2008;21(3):241–245. doi: 10.1055/s-0030-1247825. [DOI] [PubMed] [Google Scholar]
- 11.Gomes JL. Medial patellofemoral ligament reconstruction with half width (hemi tendon) semitendinous graft. Orthopedics. 2008;31(4):322–326. doi: 10.3928/01477447-20080401-12. [DOI] [PubMed] [Google Scholar]
- 12.Christiansen SE, Jacobsen BW, Lund B, Lind M. Reconstruction of the medial patellofemoral ligament with gracilis tendon autograft in transverse patellar drill holes. Arthroscopy. 2008;24(1):82–87. doi: 10.1016/j.arthro.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 13.Ostermeier S, Stukenborg-Colsman C, Wirth CJ, Bohnsack M. Reconstruction of the medial patellofemoral ligament by tunnel transfer of the semitendinosus tendon (in German) Oper Orthop Traumatol. 2007;19(5–6):489–501. doi: 10.1007/s00064-007-1022-0. [DOI] [PubMed] [Google Scholar]
- 14.Panagopoulos A, Niekerk L, Triantafillopoulos IK. MPFL reconstruction for recurrent patella dislocation: a new surgical technique and review of the literature. Int J Sports Med. 2008;29(5):359–365. doi: 10.1055/s-2007-965360. [DOI] [PubMed] [Google Scholar]
- 15.Camanho GL, Bitar AC, Hernandez AJ, Olivi R. Medial patellofemoral ligament reconstruction: a novel technique using the patellar ligament. Arthroscopy. 2007;23:108.e1–108.e4. doi: 10.1016/j.arthro.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 16.Nomura E, Horiuchi Y, Kihara M. A mid-term follow-up of medial patellofemoral ligament reconstruction using an artificial ligament for recurrent patellar dislocation. Knee. 2000;7:211–215. doi: 10.1016/S0968-0160(00)00072-7. [DOI] [PubMed] [Google Scholar]
- 17.Ellera Gomes JL, Stigler Marczyk LR, César de César P, Jungblut CF. Medial patellofemoral ligament reconstruction with semitendinosus autograft for chronic patellar instability: a follow-up study. Arthroscopy. 2004;20:147–151. doi: 10.1016/j.arthro.2003.11.006. [DOI] [PubMed] [Google Scholar]
- 18.Ellera Gomes JL. Medial patellofemoral ligament reconstruction for recurrent dislocation of the patella: a preliminary report. Arthroscopy. 1992;8:335–340. doi: 10.1016/0749-8063(92)90064-I. [DOI] [PubMed] [Google Scholar]
- 19.Schöttle PB, Fucentese SF, Romero J. Clinical and radiological outcome of medial patellofemoral ligament reconstruction with a semitendinosus autograft for patella instability. Knee Surg Sports Traumatol Arthrosc. 2005;13:516–521. doi: 10.1007/s00167-005-0659-0. [DOI] [PubMed] [Google Scholar]
- 20.Lim AK, Chang HC, Hui JH. Recurrent patellar dislocation: reappraising our approach to surgery. Ann Acad Med Singapore. 2008;37(4):320–323. [PubMed] [Google Scholar]
- 21.Steiner TM, Torga-Sak R, Teitge RA. Medial patellofemoral ligament reconstruction in patients with lateral patellar instability and trochlear dysplasia. Am J Sports Med. 2006;34(8):1254–1261. doi: 10.1177/0363546505285584. [DOI] [PubMed] [Google Scholar]
- 22.Deie M, Ochi M, Sumen Y, Adachi N, Kobayashi K, Yasumoto M. A long-term follow-up study after medial patellofemoralligament reconstruction using the transferred semitendinosustendon for patellar dislocation. Knee Surg SportsTraumatol Arthrosc. 2005;13:522–528. doi: 10.1007/s00167-005-0641-x. [DOI] [PubMed] [Google Scholar]
- 23.Drez D, Jr, Edwards TB, Williams CS. Results of medialpatellofemoral ligament reconstruction in the treatment of patellardislocation. Arthroscopy. 2001;17:298–306. doi: 10.1053/jars.2001.21490. [DOI] [PubMed] [Google Scholar]