Abstract
Total hip arthroplasty (THA) has been used as a successful form of treatment in patients with long-standing tuberculosis, but it is unclear whether THA should be performed in patients with current infection. We performed THA in six patients with advanced active tuberculosis of the hip from 2002 to 2006. Tuberculosis was confirmed in all cases by histological examination. All patients were treated with antituberculous medications for at least two weeks followed by thorough debridement and THA. Antituberculous medications were administered postoperatively for at least 12 months. The duration of postoperative follow-up was an average of 49 months. No reactivation of the infection was detected in our series. Using the Harris hip score system, five of the patients were classified as excellent and one as good. THA in advanced active tuberculosis of the hip is a safe procedure providing symptomatic relief and functional improvement. Thorough debridement of infected tissues and postoperative antituberculous therapy are the keys to lowering the potential risk of reactivation of tuberculosis.
Introduction
Tuberculosis of the hip constitutes approximately 15% of all cases of osteoarticular tuberculosis and is the most frequent site of bone involvement after the spine [1]. If osteoarticular tuberculosis is diagnosed and treated at an early stage, approximately 90–95% of patients achieve healing with near normal function [2]. Unfortunately, since the presenting symptoms, physical signs, and radiographic findings of the synovial form or intra-articular tuberculosis can mimic those of other intraarticular diseases, only a few patients are treated with antituberculous medications in early stages of the disease. If the disease is diagnosed after considerable bone destruction, surgical procedures such as arthrodesis, excisional arthroplasty or total hip arthroplasty may be required [1]. Arthrodesis or excisional arthroplasty may relieve the pain and control infection, but the function of the hip is unsatisfactory.
Total hip arthroplasty (THA) has been well established as a successful form of treatment in the quiescent tuberculous hip [3–5]. However, it is unclear whether THA should be performed in a patient with active tuberculosis of the hip. Babhulkar et al. [1] insisted that joint replacement in patients with the active stage of the disease was containdicated because of a probable high reactivation rate. In fact, a few cases of THA in patients with active tuberculosis have been reported. Yoon et al. [6] reported seven cementless THA in patients with active tuberculosis of the hip and no reactivation of the infection was detected in any of the cases after an average follow-up period of 4.8 years.
Since 2002, we have performed THA in six patients with advanced active tuberculosis of the hip. The details of the patients’ general data and clinical results are presented here.
Patients and methods
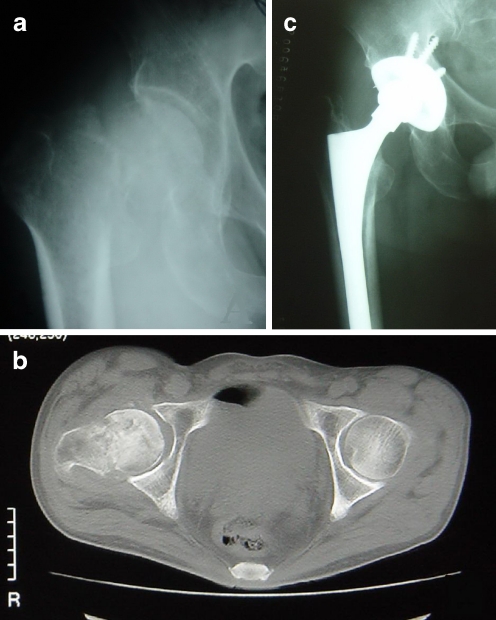
From 2002 to 2006, six patients with advanced active tuberculosis of the hip were treated by THA. In each patient the diagnosis was made by clinical and radiographic features before surgery and was confirmed by histological examination (caseous granulomatous inflammation with positive acid-fast staining bacilli) postoperatively. There were four men and two women. At the time of operation, their mean age was 33.8 years ranging from 18 to 51. Three of the patients had involvement of the right hip. Two patients had associated pulmonary tuberculosis and one of them was complicated by a pathological fracture of the femoral neck (Fig. 1). Two patients presented with a sinus. The erythrocyte sedimentation rate (ESR) was high in all patients (>20 mm/h).
Fig. 1.
a A preoperative radiograph of a 50-year-old man with tuberculosis of the hip revealing bony destruction and pathological fracture of the femoral neck. b The CT scan showing bony destruction and pathological fracture of the femoral neck and cold abscess within the joint cavity. c Thirty-five months postoperatively, the patient has a normal gait and there are no signs of prosthetic loosening
For the management of active tuberculosis of the hip, all patients were given antituberculous medication for at least 14 days before surgery and at least 12 months postoperatively. To prevent additional infection cephalosporins were given to all patients for three days before surgery and seven days postoperatively. The patients were treated with the following antituberculous medications: isoniazid (300 mg/d), rifampicin (450 mg/d), ethambutol (750 mg/d), and streptomycin (750 mg/d × 3 months). The inflamed soft tissues and the necrotic bone were completely curetted out at the time of operation. Total hip arthroplasty was performed using cementless press-fit fixation of the stem and the socket in four patients and cemented prostheses in two. In no cases were antibiotics mixed with the cement, but local rifampicin (600 mg) and streptomycin (750 mg) were administered in all cases intraoperatively. The patients were encouraged to walk with crutches from seven to ten days after the operation, and full weight bearing without crutches was allowed after four to ten weeks.
The duration of follow-up was on an average 49 months ranging from 34 to 80 months. The function of the hip was evaluated by the Harris hip score (HHS) system (Table 1).
Table 1.
Summary of six patients treated with total hip arthroplasty (THA) for advanced active tuberculosis of the hip and their clinical results at an average follow-up of 49 months
| Case | Gender | Age at diagnosis (years) | Side | Concurrent medical problem | Preoperative ESR (mm/h) | Antituberculous medications | Length of antituberculous therapy | Prosthesis | Histology | Length of follow-up (months) | Reactivation | Harris hip score (HHS) | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-op (days ) | Post-op (months) | Pre-op | Post-op | |||||||||||
| 1 | Male | 18 | Left | Pulmonary TB | 80 | I.R.E.S | 44 | 12 | Cement | Positive | 80 | No | 4 | 96 |
| 2 | Female | 19 | Left | None | 45 | I.R.E.S | 16 | 12 | Cementless | Positive | 55 | No | 46 | 92 |
| 3 | Male | 33 | Right | None | 60 | I.R.E.S | 21 | 12 | Cementless | Positive | 48 | No | 40 | 97 |
| 4 | Female | 32 | Left | Sinus | 40 | I.R.E.S | 19 | 12 | Cementless | Positive | 44 | No | 35 | 96 |
| 5 | Male | 50 | Right | Fracture of the femoral neck and pulmonary TB | 90 | I.R.E.S | 14 | 12 | Cementless | Positive | 35 | No | 30 | 95 |
| 6 | Male | 51 | Right | Sinus | 120 | I.R.E.S | 54 | 18 | Cement | Positive | 34 | No | 6 | 89 |
Results
Within the average follow-up period of 49 months (range 34–48), no reactivation of tuberculosis was detected. The ESR became normal below 20 mm/h within six months after THA in all patients, and none of the patients had an elevated ESR at the subsequent follow-up examinations. The mean HHS was 26.8 points (range 4–46) preoperatively and was 94.2 (range 89–97) points at the last follow-up. No postoperative hip dislocation, infection, neurological or vascular complications were observed in any of the patients. At the last follow-up, all patients ambulated without walking aids, and roentgenograms did not reveal any loosening of the prostheses (Figs. 1 and 2).
Fig. 2.
a A preoperative radiograph of an 18-year-old man with tuberculosis of the hip revealing bony destruction. b The CT scan showing bony destruction and cold abscess around the femoral head. c Eighty months after surgery, the patient had a normal gait and the radiograph showed no loosening of the prosthesis
Discussion
Total hip arthroplasty in a hip with active tuberculous infection is a controversial issue due to the potential risk of reactivation of tuberculosis [6]. Traditionally, two treatment modalities were suggested for treating advanced active tuberculosis of the hip. These were arthrodesis in position of function and Girdlestone excision arthroplasty [1, 7, 8]. Total hip arthroplasty for active tuberculous infection was opposed by some authors because they believed the risks were too high [1]. Other authors recommended a long interval between the treatment of the active infection and arthroplasty [9, 10]. They suggested that if the interval between the active infection and the surgery is shorter than ten years, antituberculous therapy should be given so as to lower the reactivation rate.
To date, only a few cases of THA in patients with active tuberculosis have been reported. Yoon et al. [6] reported seven successful primary THA in patients with active tuberculosis of the hip. Postoperatively, all cases were given antituberculous medication for one year, and no reactivation was detected after an average period of 4.8 years. In our study, our patients were also successfully treated with primary THA and antituberculous therapy, and no reactivation was detected in an average period of 49 months. In our experience, thorough debridement of infected tissues and postoperative antituberculous therapy are the keys to lower the potential risk of reactivation of tuberculosis. The former can eradicate the disease, and the latter is used to control the residual foci. We recommend a combination of antituberculous drugs for at least two weeks prior to the operation and subsequently for at least 12 months after the operation. This policy was also adopted in spinal tuberculosis in our hospital.
Many orthopaedic surgeons are reluctant to treat tuberculous coxitis with the THA because there is a risk of reactivating the tuberculous infection [3, 9, 11]. However, Mycobacterium tuberculosis has biologically very specific behavioural characteristics which differ from pyogenic bacteria. A good understanding of these characteristics is vital as is knowledge of bacterial response to implanted material and chemotherapy [12]. M. tuberculosis lesions represent a planktonic form which reproduces slowly, producing minimal adhesion molecules and slime, and occasionally becomes dormant. Thus, M. tuberculosis has little tendency to adhere to implants that can be safely used in tuberculous lesions, but they do form a nidus to perpetuate tuberculous infection, so THA followed by antituberculous chemotherapy is crucial to the treatment of advanced active tuberculous coxitis. Even if the tuberculosis has been reactivated, the disease can be controlled by antituberculous medications alone or in combination with debridement without removal of the prosthesis in most cases [3, 9, 13].
Kim et al. [9] reported that the prevalence of reactivation of infection in the hips with the cemented prosthesis was comparable to the cementless prosthesis and that mean tuberculous reactivation was not affected by the use of cemented prosthesis or cementless prosthesis; thus, both of these two kinds of prostheses could be used in the treatment of tuberculous coxitis. In our study, the tuberculous reactivation was not detected both in patients with the cemented prostheses and in patients with the cementless prostheses.
The functional results of THA seemed to be satisfying in patients with tuberculosis of the hip. Kim et al. [9] reported 38 total hip arthroplasties in patients who had tuberculous hip arthritis. The interval between active disease and total hip arthroplasty ranged from three months to 45 years. The duration of follow-up averaged four years. The mean functional rating of the hip, using the Harris hip score, was 85 at the final follow-up. Eskola et al. [14] reported cementless total hip arthroplasty in 18 patients with old tuberculosis of the hip performed, on average, 34 years after onset of infection. The mean follow-up was 3.5 years. On the basis of the Mayo hip score, 15 patients had excellent or good results, two a fair rating and one poor rating. Yoon et al. [6] reported the results of a primary THA in seven patients with advanced active tuberculous arthritis of the hip. The average follow-up period was 4.8 years. The result was excellent in all patients according to the HHS. In our study, the HHS raised from 26.8 points preoperatively to 94.2 points after the operation, and an excellent result was recorded in five patients with a good result in one at the final follow-up. These results are comparable with the reports mentioned above.
Conclusions
In our opinion, THA in advanced active tuberculosis of the hip is a safe procedure providing symptomatic relief and functional improvement. Thorough debridement of infected tissues and postoperative antituberculous chemotherapy are the keys to lowering the potential risk of reactivation of tuberculosis.
References
- 1.Babhulkar S, Pande S. Tuberculosis of the hip. Clin Orthop Relat Res. 2002;398:93–99. doi: 10.1097/00003086-200205000-00013. [DOI] [PubMed] [Google Scholar]
- 2.Tuli SM. General principles of osteoarticular tuberculosis. Clin Orthop Relat Res. 2002;398:11–19. doi: 10.1097/00003086-200205000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Kim YY, Ahn JY, Sung YB, Ko CU, Shim JC, Park HS, Bai GH. Long-term results of Charnley low friction arthroplasty in tuberculosis of the hip. J Arthroplasty. 2001;211:106–110. doi: 10.1054/arth.2001.28720. [DOI] [PubMed] [Google Scholar]
- 4.Santavirta S, Eskola A, Konttinen YT, Tallroth K, Lindholm ST. Total hip replacement in old tuberculosis. A report of 14 cases. Acta Orthop Scand. 1988;59:391–395. doi: 10.3109/17453678809149388. [DOI] [PubMed] [Google Scholar]
- 5.Wang JW. Uncemented total arthroplasty in old quiescent infection of the hip. J Formos Med Assoc. 1997;96:634–640. [PubMed] [Google Scholar]
- 6.Yoon TR, Rowe SM, Santosa SB, Jung ST, Seon JK. Immediate cementless total hip arthroplasty for the treatment of active tuberculosis. J Arthroplasty. 2005;20:923–926. doi: 10.1016/j.arth.2004.08.002. [DOI] [PubMed] [Google Scholar]
- 7.Chen H, Lee T. Arthrodesis of the tuberculous. Int Surg. 1966;46:125–130. [PubMed] [Google Scholar]
- 8.Tuli SM, Mukherjee SK. Excision arthroplasty for tuberculous and pyogenic arthritis of the hip. J Bone Joint Surg Br. 1981;63:29–32. doi: 10.1302/0301-620X.63B1.7204469. [DOI] [PubMed] [Google Scholar]
- 9.Kim YH, Han DY, Park BM. Total hip arthroplasty for tuberculous coxarthrosis. J Bone Joint Surg Am. 1987;69:718–727. [PubMed] [Google Scholar]
- 10.Jupiter JB, Karchmer AW, Lowell JD, Harris WH. Total hip arthroplasty in the treatment of adult hips with current or quiescent sepsis. J Bone Joint Surg Am. 1981;63:194–200. [PubMed] [Google Scholar]
- 11.Johnson R, Barnes KL, Owen R. Reactivation of tuberculosis after total hip replacement. J Bone Joint Surg Br. 1979;61:148–150. doi: 10.1302/0301-620X.61B2.438263. [DOI] [PubMed] [Google Scholar]
- 12.Moon MS. Tuberculosis of spine—Contemporary thoughts on current issues and perspective views. Spine. 2007;21:364–379. [Google Scholar]
- 13.Lin E, Oliver S, Caspi I, Ezra E, Bubis JJ, Nerubay J. Hip arthroplasty in quiescent mycobacterial infection of hip. Orthop Rev. 1986;15:232–236. [PubMed] [Google Scholar]
- 14.Eskola A, Santavirta S, Konttinen YT, Tallroth K, Hoikka V, Lindholm ST. Cementless total replacement for old tuberculosis of the hip. J Bone Joint Surg (Br) 1988;70:603–606. doi: 10.1302/0301-620X.70B4.3403606. [DOI] [PubMed] [Google Scholar]