Abstract
Most health services in the United Kingdom provide unacceptable in-hospital care for hip fracture patients. We describe the impact on surgical delay following the introduction of an orthogeriatrician and the addition of one extra trauma list per week at our centre. Prospective data were collected on 101 consecutive patients followed by a second cohort of 105 patients. Mean time to surgery in cohorts 1 and 2 was 4.08 and 4.05 days, respectively (p = 0.71). Diagnosis of medical comorbidity increased with input from the orthogeriatrician from 69.7% to 74.2% (p = 0.24). Length of stay and mortality were comparable in the two groups. A full trauma list accounted for the most frequent orthopaedic delay, which decreased from 18.1% to 12.9% (p = 0.09). Increased recognition of medical comorbidity has financial implications for hospital remuneration. However, lack of orthopaedic provisions accounts for significant avoidable surgical delay requiring further investment if national standards are to be achieved.
Introduction
Most local health services provide unacceptable in-hospital care for patients with hip fractures [1]. With an ageing population, it has been predicted that by 2050, there will be six million fractures per annum worldwide [2]. Mortality in this group can be as high as 50% at one year [3–6], and evidence has emerged in recent years to show that delay to surgery worsens outcome [4, 7–9]. Male sex and obesity are risk factors for poor outcome, and patients with hip fractures frequently have pre-existing medical comorbidity [10]. It is also recognised that common postoperative medical complications such as chest infection and pulmonary oedema are associated with increased mortality [5]. Some centres have now employed delegated care-of-the-elderly physicians who offer routine medical care for such patients, as recommended by the Royal College of Physicians [11] and the British Orthopaedic Association [12].
We present prospective data on causes of surgical delay for patients admitted to a district teaching hospital serving a population of 375,000 people with eight orthopaedic consultant surgeons and describe how performance and outcome changed after employment of an orthogeriatrician and the addition of one extra trauma list per week.
Materials and methods
Prospective data were collected on 101 consecutive patients (16 men, 85 women) presenting with a hip fracture from March to July 2004. Surgical delay was defined as any patient operated on more than 24 hours after admission, in accordance with the Scottish Intercollegiate National Guidelines (SIGN) [13]. Other data collected included reasons for the delay, type of fracture, operation performed, discharge and mortality at one and three months postsurgery. We looked specifically for nonmedical, avoidable reasons for delay, with the aim of making changes to improve overall treatment of subsequent patients with hip fractures.
Following the initial study, an orthogeriatrician was employed to improve the medical optimisation of patients prior to surgery and to treat any medical complications in the postoperative period. The orthogeriatrician carried out daily ward rounds accompanied by an orthopaedic trauma nurse in order to provide continuity of care and communicate with the junior orthopaedic doctors. Before this system was introduced, medical comorbidity had been managed solely by the orthopaedic team’s junior doctor, with supervision provided by the orthopaedic registrar and consultant. Acute medical complications requiring specialist input were traditionally referred to the on-call medical registrar. During the same period as the orthogeriatrician was employed, one extra trauma list per week was introduced, increasing the total number of weekly trauma lists to eight. The total cost of these changes to the trust was £161,750 per annum. A second cohort of 105 consecutive patients (27 men, 78 women) was then prospectively studied between January and June 2006. Identical parameters were recorded, and differences between the two cohorts were evaluated. The mean ages were 83.0 (range 53.8–100.9) years and 81.8 (range 50.4–102.7) years in cohorts 1 and 2, respectively. In cohort 1, three patients were excluded; two died preoperatively and one was transferred to another hospital. In cohort 2, seven patients were excluded: six died preoperatively and one was treated conservatively. Results were analysed using the Mann−Whitney U test and Fisher’s exact test. Pearson’s correlation coefficient was used to calculate the correlation of linear variables. A p value of 0.05 was used for statistical significance. Fracture type and admission source for patients in both cohorts are shown in Table 1.
Table 1.
Patient referral source and type of fracture
| Referral source/fracture type | Cohort 1: n = 98; n (%) | Cohort 2: n = 98; n (%) | |
|---|---|---|---|
| Source of admission (%) | A+E | 95 (96.9) | 95 (97) |
| Physicians | 3 (3.1) | 2 (2.0) | |
| Missing | - | 1 (1.0) | |
| Classification of hip fracture (%) | Extracapsular | 34(34.7) | 38 (39.8) |
| Intracapsular | 64 (65.3) | 60 (60.2) |
A+E Accident and Emergency Department
Table 2.
Medical comorbidity recorded prior to surgery, including frequency of diagnosis per patient
| Cohort 1 | Cohort 2 | |
|---|---|---|
| Chest Infection | 14 | 16 |
| Ischaemic heart disease | 6 | 30 |
| Hypertension | 6 | 18 |
| Atrial fibrillation | 7 | 8 |
| Electrolyte imbalance | 8 | 4 |
| Cardiac failure | 2 | 8 |
| Warfarin | 3 | 6 |
| Cerebrovascular disease | 2 | 7 |
| Parkinson’s disease | 0 | 7 |
| Diabetes mellitus | 2 | 3 |
| Chronic obstructive pulmonayr disease | 2 | 3 |
| Malignancy | 1 | 4 |
| Renal failure | 1 | 2 |
| Mean frequency of preoperative comorbidity per patient | 0.62 | 1.68 |
| Mean frequency of postoperative complications per patient | 0.49 | 0.75 |
Results
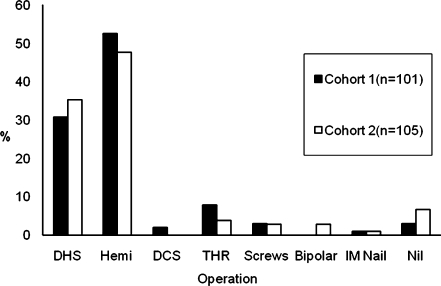
Figure 1 shows the range of operations performed. There were no significant differences between the two groups.
Fig. 1.
Operations performed for patients admitted with hip fracture
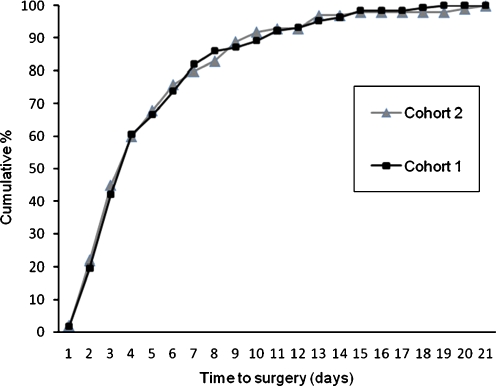
The overall mean time to surgery for all patients in cohorts 1 and 2 was 4.08 (range 0–17) and 4.05 (range 0–20) days, respectively (p = 0.71). Figure 2 shows the cumulative timing of surgery for both patient groups, with no significant statistical difference between the cohorts.
Fig. 2.
Cumulative time to surgery for cohorts 1 and 2
In total, there were 304 and 310 delay days in cohorts 1 and 2, respectively. The majority of delays were due to medical problems, with 212 (69.7%) delay days in cohort 1 compared with 230 (74.2%) in cohort 2 (p = 0.24). Table 2 shows the range of medical comorbidity recorded. Secondary medical complications also occurred. In cohort 1, eight patients developed medical problems after initial delays to surgery for either a full trauma list or lack of an available anaesthetist, accounting for 44 (14.4%) delay days.
Lack of orthopaedic or anaesthetic department provisions accounted for significant delays, with 92 delay days (30.2%) in cohort 1 and 80 (25.3%) in cohort 2 (p = 0.24). Table 3 summarises the nonmedical reasons for delay.
Table 3.
Nonmedical reasons for surgical delay
| Nonmedical reasons for surgical | Delay days (%) cohort 1 (n = 92) | Delay days (%) cohort 2 (n = 80) | P value |
|---|---|---|---|
| Full trauma list | 55 (18.1) | 40 (12.9) | 0.09 |
| No anaesthetist | 15 (4.9) | 4 (1.3) | <0.01 |
| Specialist case on trauma list | 14 (4.6) | 30 (9.7) | 0.018 |
| Name not on trauma board | 6 (2.0) | 0 | 0.014 |
| X-ray not available in theatre | 1 | 0 | 1 |
| No prosthesis | 1 | 1 | 1 |
| Delayed diagnosis | 0 | 2 | 0.50 |
| Patient initially refused surgery | 0 | 3 (1) | - |
Table 4 shows three-month outcome. As shown, the only statistically significant difference between the two groups was for rate of discharge, which was worse in cohort 2. Table 5 summarises the surgical delay for those patients who died. Although surgical delay following the changes was reduced, mortality rates were not significantly different at one (p = 1) or three months (p = 0.27), although three-month mortality was slightly increased in cohort 2.
Table 4.
Three-month outcome for cohorts 1 and 2
| Cohort 1 n = 98 (%) | Cohort 2 n = 98 (%) | P value | ||
|---|---|---|---|---|
| Outcome at 3 months | Discharged | 77 (78.6) | 60 (61.2) | 0.012 |
| In patients | 6 (6.1) | 8 (8.2) | 0.783 | |
| Died | 15 (15.3) | 22 (22.4) | 0.27 | |
| Missing data | - | 8 (8.2) | ||
| Discharge destination (%) | Home | 57 | 46 | |
| Rehabilitation ward/residential or nursing home | 43 | 54 |
Table 5.
Rates of preoperative comorbidity, postoperative complications and surgical delay for patients who died, including overall mortality rates for cohorts 1 and 2
| Cohort 1 | Cohort 2 | P value | |
|---|---|---|---|
| Mortality at 1 month (%) | 9 (8.6) | 9 (8.9) | 1 |
| Mortality at 3 months (%) | 15 (14.9) | 22 (22.4) | 0.27 |
| Medical delay days | 50 | 43 | 0.13 |
| Nonmedical delay days | 6 | 12 | 0.13 |
| Time to surgery (days) | Mean 4.1 | Mean 4.555 | 0.615 |
| Range 1–10 | Range 1–12 | ||
| Median 3 | Median 2 | ||
| No. of recognised comorbid health problems preoperatively | Mean 0.833 | Mean 2.71 | |
| Range 0–3 | Range 0–6 | ||
| No. of recognised postoperative complications | Mean 0.75 | Mean 0.928 | |
| Range 0–3 | Range 0–3 |
Discussion
Impact of orthogeriatric input
The causes of surgical delay for patients with a hip fracture are varied and often complex. In this study, delay to surgery occurred most frequently because of medical comorbidity. The introduction of an orthogeriatrician resulted in an increased rate of diagnosis of medical complications preoperatively, which was associated with a slight increase in medical delays (p = 0.24). This change may be related to the expertise on the part of the orthogeriatrician and the ability to better recognise medical problems compared with the admitting junior orthopaedic doctors. The relative number of observed pre- and postoperative morbidity (Table 2) shows that there was better recognition of disease during the second cohort. It may also have been that the junior orthopaedic doctors were better able to diagnose health problems because of their experience working alongside the orthogeriatrician. The most common medical conditions were chest infection, ischaemic heart disease (IHD) and atrial fibrillation. There was a significant increase in the rate of diagnosis of IHD during the second cohort. This is most likely attributable to the increased availability of the troponin blood test and the national changes in criteria for acute coronary syndrome between the cohorts.
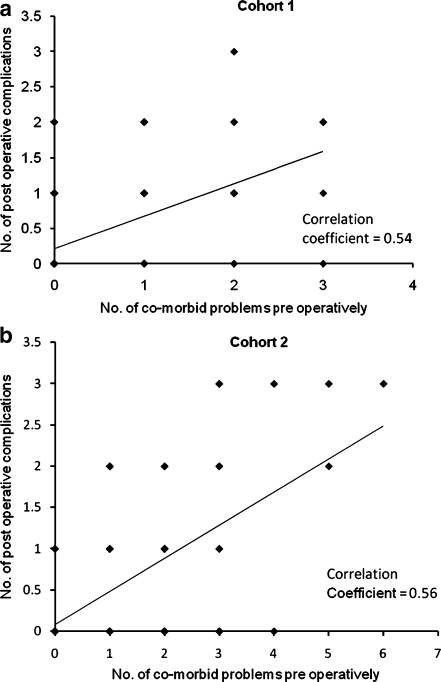
Our data suggest that there is a moderate correlation between the development of postoperative complications and pre-existing comorbidity, and this was true for both groups (Fig. 3a and b). The limitation with interpreting data in this way is that types and degrees of comorbidity are more important than simply the number of health problems.
Fig. 3.
a, b Correlation between the frequency of preoperative comorbidity and postoperative complications for cohorts 1 and 2, respectively
The frequency of postoperative complications appeared to vary slightly according to time to surgery between the two cohorts (Fig. 4). Complications were more frequently diagnosed for patients in cohort 2 who waited up to 12 days for surgery. Patients who waited longer than this, however, tended to do better in cohort 2 compared with cohort 1. Such patients have complex medical problems and are the group most likely to benefit from expert medical input. Although the trend is weak, the better outcome may be related to better optimisation of patients on the ward by the orthogeriatrician prior to theatre. Further research should be carried out to focus on medically complex patients to assess how best to prepare them for surgery.
Fig. 4.
Frequency of postoperative complications according to the delay to surgery for cohorts 1 and 2
Some medical conditions should not delay surgery [13]. For example, there were several incidents where anaesthetists delayed surgery because a chest infection had been identified by the orthogeriatrician. More aggressive treatment of such patients is required, and in order to change attitudes and opinions, good communication and the development of an agreed-upon protocol between the orthogeriatrician, surgeons and anaesthetists is vital.
The identification of medical comorbidity also has implications for the hospital in terms of funding and costs. Since 2004, hospitals in England have been paid according to the work load and complexity of cases by the Primary Care Trust (PCT) fundholders. Patients’ individual medical problems are coded, so that patients with multiple medical problems earn more revenue compared with relatively healthy patients.
The average cost for acute hospital care for a patient admitted with a hip fracture is £12,163 [14]. The presence of comorbid illness increases hospitalisation costs, but the type of comorbidity is more significant than the number of comorbid illnesses. Patients with dementia incur significantly higher costs compared with those with hypertension and diabetes [15]. It is possible that prior to the employment of the orthogeriatrician, the hospital was not adequately reimbursed because such medical problems were not accurately recognised and listed in the patient notes and discharge summaries. In a hospital that admits more than 200 hip fractures per year, this would result in the recoupment of significant costs balanced against the cost of an orthogeriatric consultant and secretary at £119,000 annually.
The biggest cost factor for hip fracture patients is length of stay. In our study, most patients had been discharged by three months, with 6.1% and 8.7 % remaining as in-patients in cohorts 1 and 2, respectively. Early discharge and geriatric hip fracture programmes may be cost effective, and the Cochrane review [16] concluded that geriatric orthopaedic rehabilitation units are probably clinically effective in improving major outcomes associated with hip fracture patients. However, the benefit following the introduction of multidisciplinary teams has traditionally been difficult to prove [17]. Some studies have failed to show any significant improvement at one, three or six month follow-up despite intensive multidisciplinary care [18, 19]. This includes routine input from an internist−geriatrician, physiotherapist, occupational therapist, social worker and clinical nurse specialist [20, 21].
Other studies have shown benefit from geriatric-based postoperative care [22]. Comparing early daily multidisciplinary geriatric intervention and usual surgical care in elderly patients with hip fractures, one centre found hospital mortality was reduced but hospital stay and mortality at six and 12 months was unchanged [23]. A multidisciplinary hip fracture service at a centre in the USA had fewer medical complications, earlier surgery and shorter hospital stays [24]. Further, intensive occupational therapy and physiotherapy combined with early surgery (within two days of admission) resulted in earlier ambulation, a shorter hospital stay and reduction in six-month mortality rates [25]. Regardless of the type of service provided, the most important factor to reduce hospital stay is to perform early surgery [26].
Hospital stay is, however, sometimes difficult to interpret (Table 4). We found virtually no correlation between time to surgery and length of stay (correlation coefficients −0.01 and 0.003 for cohorts 1 and 2, respectively). We believe this relationship was difficult to establish using our data because when patients were identified early to require nursing home or residential care, their discharge from an acute orthopaedic bed was prioritised. However, those patients able to be discharged directly to their own home may have waited longer on the acute ward to allow more time for extended rehabilitation and physiotherapy.
Mortality
The commonest cause of death in both cohorts was chest infection, cardiac failure and myocardial infarction. Mortality rates were the same in both groups at one month despite the increase in medical comorbidity in cohort 2. One might expect that regular orthogeriatric input results in early recognition and treatment of medical complications and therefore improved mortality rates. This was supported by the increased rate of diagnosis of preoperative health problems observed in those patients who died in cohort 2 compared with cohort 1 (Table 5). In the postoperative phase for those patients who died, the observed number of complications leading up to death was similar in the two cohorts. Mean time to surgery was similar in both cohorts for patients who died and was not significantly different compared with the whole group (Table 5). The previously described correlation between delay to surgery and postoperative mortality [13] was therefore not apparent in our data, and this is probably because our study was underpowered in this respect.
Three-month mortality for group 2 slightly increased (not statistically significant) in correlation with the increased incidence of medical comorbidity. This trend may be explained by the fact that the majority of patients at three months had been discharged or had been transferred to rehabilitation wards, residential or nursing homes. Such patients would therefore have lost access to the orthogeriatric care provided on the acute orthopaedic ward. The benefit of extended orthogeriatric care in the community on medium-term mortality needs to be researched further. Overall, our mortality rates are comparable with other studies [4, 9, 10, 27].
Patients who died had more observed preoperative comorbidity compared with patients who survived during the study period. The mean number of recorded preoperative health problems (Table 2) was 0.62 and 1.68 per patient in cohorts 1 and 2, respectively, and was found to be 0.83 and 2.71, respectively, in the mortality groups (see Table 5). Our data suggests that increased comorbidity increases the likelihood of death postoperatively.
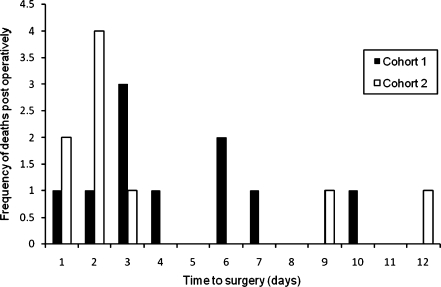
Mortality rates varied between the two groups according to time to surgery. Figure 5 shows that death occurred less frequently in cohort 2 compared with cohort 1 for those patients operated on after 48 hours. Our study does not have the power to show significant differences because the numbers of deaths were low. However, the trend may be explained by input from the orthogeriatrician. Regular medical input by the same medical clinician has the advantage of providing continuity of care in comparison with the previous system in place for cohort 1 in which difficult medical issues were dealt with by the medical registrar on call. Complex medical patients are likely to benefit from the new system, and such patients may have been better optimised during cohort 2 compared with cohort 1, resulting in a lower risk of death.
Fig. 5.
Frequency of deaths in cohorts 1 and 2 according to the time to surgery
Orthopaedic delay
Table 3 shows that surgical delay secondary to departmental provisions decreased following the introduction of an extra trauma list (p = 0.24), especially with regards to lack of theatre space (p = 0.09). This was despite an increase in overall trauma workload for the department during the period of study for cohort 2. Creating extra theatre time is a priority if this is identified as a major source of delay. When significant delay occurs, the department should consider cancelling elective operating lists in order to deal with trauma work load. Further improvements were made through changes to the anaesthetic rota. Cohort 1 showed almost 5% of delays were from lack of an available anaesthetist, which mainly occurred at weekends. Extra staffing resulted in a statistically significant reduction to 1.3%. Delays because of technically challenging cases and high-risk patients more than doubled during cohort 2. This occurred when patients required a consultant surgeon, for example, for a total hip replacement. This problem has since been addressed through employment of an extra consultant orthopaedic surgeon.
Our department recognises the need for improvement upon the current performance. Excluding medical delays, it is possible to achieve surgery within 48 hours for 95% of patients [26]. In order to provide such a service, as this study shows, overall delay is unlikely to change unless all variables are addressed. Patients have a window of opportunity in relation to timing of surgery. Unnecessary delays at the beginning of a patient’s admission can lead to medical complications, and in cohort 1, we calculated that initial delays for nonmedical reasons resulted in the development of secondary medical problems, accounting for 14.4% of the total delay. Our data showed a positive correlation between time to surgery and the development of postoperative complications in both cohorts (Fig. 6a and b), but this relationship was relatively weak. However, the trend is consistent with other studies that show an increased risk of morbidity with surgical delay [3, 8, 13].
Fig. 6.
a, b Correlation between time to surgery and frequency of postoperative complications for cohorts 1 and 2, respectively
Conclusion
The causes of surgical delay for hip fracture patients are multifactorial. Input from an orthogeriatrician is advocated by the British Orthopaedic Association and the Royal College of Physicians, but this failed to show a significant impact at our centre for major outcomes. However, medical comorbidity was more readily diagnosed, and this has cost implications for the hospital in terms of coding and remuneration from the PCT. Based on current evidence, it seems unlikely that the introduction of a lone orthogeriatrician without a dedicated orthopaedic rehabilitation ward and the necessary multidisciplinary support is likely to significantly affect outcome, and we plan further investment in order to develop our services. The addition of one extra trauma list reduced orthopaedic delays, but this was not statistically significant. Time to surgery appears to be the most important factor in reducing morbidity and mortality for patients admitted with hip fractures. Lack of orthopaedic provisions continues to account for a significant proportion of avoidable surgical delay, and further investment is required if national standards are to be achieved.
Acknowledgements
The authors thank the trauma nurse practitioners Jenny Currie and Lorraine Sanderson at Chesterfield Royal Hospital for their valued assistance in data collection during the study.
No financial support was received as part of this study
Conflict of interest The authors declare that they have no conflict of interest.
Contributor Information
Daniel Marsland, Phone: +44-0207-6070452, FAX: +44-02085356936, Email: danielmarsland@yahoo.co.uk.
Carolyn Chadwick, Phone: 0114 2303393, Email: chittychadwick@hotmail.com.
References
- 1.Clinical Effectiveness and Evaluation Unit (2007) National Report: National Clinical Audit of Falls and Bone Health in Older People, Royal College of Physicians. Available via DIALOG. http://www.rcplondon.ac.uk/college/ceeu/fbhop/fbhop-nationalreport.pdf. Accessed 3 Jun 2009
- 2.Cooper C, Campion G, Melton LJ., III Hip fractures in the elderly: A worldwide projection. Osteoporos Int. 1992;2(6):285–289. doi: 10.1007/BF01623184. [DOI] [PubMed] [Google Scholar]
- 3.Keene GS, Parker MJ, Pryor GA. Mortality and morbidity after hip fractures. BMJ. 1993;307:1248–1250. doi: 10.1136/bmj.307.6914.1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moran CG, Wenn RT, Sikand M, et al. Early mortality after hip fracture: is delay before surgery important? J Bone Joint Surg Am. 2005;87:483–489. doi: 10.2106/JBJS.D.01796. [DOI] [PubMed] [Google Scholar]
- 5.Roche JJW, Wenn RT, Sahota O, Moran CG. Effect of co-morbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ. 2005;331(7529):1374. doi: 10.1136/bmj.38643.663843.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roberts SE, Goldacre MJ. Time trends and demography of mortality after fractured neck of femur in an English population, 1968–98. BMJ. 2003;327:771–775. doi: 10.1136/bmj.327.7418.771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barnes R, Brown JT, Garden RS, Nicholl EA. Subcapital fractures of the femur: A prospective review. J Bone Joint Surg Br. 1997;58(1):2–24. doi: 10.1302/0301-620X.58B1.1270491. [DOI] [PubMed] [Google Scholar]
- 8.Rogers FB, Shackford SR, Keller MS. Early fixation reduces morbidity and mortality in elderly patients with hip fractures from low-impact falls. J Trauma. 1995;39(2):261–265. doi: 10.1097/00005373-199508000-00012. [DOI] [PubMed] [Google Scholar]
- 9.Sebestyén A, Boncz I, Sándor J, Nyárády J. Effect of Surgical delay on early mortality in patients with femoral neck fracture. Int Orthop. 2008;32(3):375–379. doi: 10.1007/s00264-007-0331-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jamal Sepah Y, Umer M, Khan A, Ullah Khan Niazi A (2009) Functional outcome, mortality and in-hospital complications of operative treatment in elderly patients with hip fractures in the developing world. Int Orthop May 28 (Epub ahead of print) [DOI] [PMC free article] [PubMed]
- 11.Royal College of Physicians Fractured neck of femur. Prevention and management. Summary and recommendations of a report of the Royal College of Physicians. J R Coll Physicians Lond. 1989;23:8–12. [PMC free article] [PubMed] [Google Scholar]
- 12.British Orthopaedic Association Blue book (2007) The care of patients with fragility fracture. Available via DIALOG. http://www.boa.ac.uk. Accessed 21 Mar 2009
- 13.Scottish Intercollegiate Guidelines Network (2002) The prevention and management of hip fracture in older people. SIGN, Edinburgh. Available via DIALOG. http://www.sign.ac.uk/pdf/sign56. Accessed 21 Mar 2009
- 14.Lawrence TM, White CT, Wenn R, Moran CG. The current hospital costs of treating hip fractures. Injury. 2005;36:88–92. doi: 10.1016/j.injury.2004.06.015. [DOI] [PubMed] [Google Scholar]
- 15.Chen L, Lee JAY, Chua BSY, Howe T. Hip fractures in the elderly: The impact of comorbid illnesses on hospitalisation costs. Ann Acad Med Singapore. 2007;36:784–787. [PubMed] [Google Scholar]
- 16.Cameron ID, Handoll HHG, Finnegan TP, Madhok R, Langhorne P (2001) Co-ordinated multidisciplinary approaches for inpatient rehabilitation of older patients with femoral neck fractures. The Cochrane Database of Systematic Reviews, Issue 3 John Wiley and Sons, Ltd, Chichester [DOI] [PubMed]
- 17.Beaupre LA, Jones CA, Saunders LD, Johnston DW, Buckingham J, Majumdar SR. Best practices for elderly hip fracture patients: a systematic overview of the evidence. J Gen Intern Med. 2005;20(11):1019–1025. doi: 10.1111/j.1525-1497.2005.00219.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hempsall VJ, Robertson DR, Campbell MJ, Briggs RS. Orthopaedic geriatric care—is it effective? A prospective population-based comparison of outcome in fractured neck of femur. J R Coll Physicians Lond. 1990;24(1):47–50. [PMC free article] [PubMed] [Google Scholar]
- 19.Khan R, Fernandez C, Kashifl F, Shedden R, Diggory P. Combined orthogeriatric care in the management of hip fractures: a prospective study. Ann R Coll Surg Engl. 2002;84:122–124. [PMC free article] [PubMed] [Google Scholar]
- 20.Naglie G, Tansey C, Kirkland JL, et al. Interdisciplinary inpatient care for elderly people with hip fracture: a randomized controlled trial. CMAJ. 2002;167(1):25–32. [PMC free article] [PubMed] [Google Scholar]
- 21.Phy MP, Vanness DJ, Melton LJ III, Long KH et al (2005) Effects of a hospitalist model on elderly patients with hip fracture. Arch Intern Med 165(7):796–801 [DOI] [PubMed]
- 22.Adunsky A, Lusky A, Arad M, Heruti RJ. A comparative study of rehabilitation outcomes of elderly hip fracture patients: the advantage of a comprehensive orthogeriatric approach. J Gerontol A Biol Sci Med Sci. 2003;58(6):542–547. doi: 10.1093/gerona/58.6.m542. [DOI] [PubMed] [Google Scholar]
- 23.Vidan M, Serra JA, Moreno C, Riquelme G, et al. Efficacy of a comprehensive geriatric intervention in older patients hospitalized for hip fracture: a randomized, controlled trial. J Am Geriatr Soc. 2005;53(9):1476–1482. doi: 10.1111/j.1532-5415.2005.53466.x. [DOI] [PubMed] [Google Scholar]
- 24.Khasraghi FA, Christmas C, Lee EJ, Mears SC, Wenz JF., Sr Effectiveness of a multidisciplinary team approach to hip fracture management. J Surg Orthop Adv. 2005;14(1):27–31. [PubMed] [Google Scholar]
- 25.Hoenig H, Rubenstein LV, Sloane R, Horner R, Kahn K (1997) What is the role of timing in the surgical and rehabilitative care of community-dwelling older persons with acute hip fracture? Arch Intern Med 10;157(5):513–520 [PubMed]
- 26.Siegmeth AW, Gurusamy K, Parker MJ. Delay to surgery prolongs hospital stay in patients with fractures of the proximal femur. J Bone Joint Surg Br. 2005;87(8):1123–1126. doi: 10.1302/0301-620X.87B8.16357. [DOI] [PubMed] [Google Scholar]
- 27.Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA. Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet. 1999;353:878–882. doi: 10.1016/S0140-6736(98)09075-8. [DOI] [PubMed] [Google Scholar]