Abstract
Background
Data on the long-term association between low-carbohydrate diets and mortality are sparse.
Objective
To examine the association of low-carbohydrate diets with mortality during 26 years of follow-up in women and 20 years in men.
Design
A prospective cohort study of women and men, followed from 1980 (women) or 1986 (men) until 2006. Low-carbohydrate diets, either animal-based (emphasizing animal sources of fat and protein), or vegetable-based (emphasizing vegetable sources of fat and protein) were computed from multiple validated food frequency questionnaire assessed during follow-up.
Setting
Nurses' Health Study and Health Professionals' Follow-up Study
Participants
85,168 women (aged 34-59 years at baseline) and 44,548 men (aged 40-75 years at baseline) without heart disease, cancer, or diabetes.
Measurement
Investigator documented 12,555 deaths (2,458 cardiovascular, 5,780 cancer) in women and 8,678 deaths (2,746 cardiovascular, 2,960 cancer) in men.
Results
The overall low-carbohydrate score was associated with a modest increase in overall mortality in pooled analysis (Hazard Ratio, HR, comparing extreme deciles=1.12 (95% CI=1.01-1.24, p-trend=0.14). The animal low-carbohydrate score was associated with a higher all-cause mortality (pooled HR comparing extreme deciles=1.23, 95% CI=1.11-1.37, p-trend=0.05), cardiovascular mortality (corresponding HR=1.14, 95% CI=1.01-1.29, p-trend=0.029), and cancer mortality (corresponding HR=1.28, 95% CI 1.02-1.60, p for trend = 0.09). In contrast, a higher vegetable low-carbohydrate score was associated with lower all-cause (HR=0.80, 95% CI=0.75-0.85, p-trend<0.001) and cardiovascular mortality (HR=0.77, 95% CI=0.68-0.87, p-trend<0.001).
Limitations
Diet and lifestyle characteristics were assessed with some degree of error, however, sensitivity analyses indicated that results were not unlikely to be substantially affected by residual or confounding or an unmeasured confounder. In addition, participants were not a representative sample of the U.S. population.
Conclusion
A low-carbohydrate diet based on animal sources was associated with higher all-cause mortality in both men and women, whereas a vegetable-based low-carbohydrate diet was associated with lower all-cause and cardiovascular disease mortality rates.
Primary funding source
NIH grants CA87969, HL60712, and CA95589
Keywords: diet, nutrition, mortality, carbohydrate, protein
Introduction
Low-carbohydrate diets have claimed to promote weight loss, improve blood cholesterol levels, and blood pressure(1, 2). Weight loss trials lasting 6 months to 2 years have found them to be as effective(3, 4) or more effective(5, 6) than diets with higher carbohydrate content. However, effects on blood lipid profiles for low-carbohydrates diets with substantial animal products were mixed, with low-carbohydrate diets resulting in greater improvements in high density lipoprotein but possibly less favorable change in low density lipoprotein than higher carbohydrate diets(6-9). In addition, these diets can be high in red meat and low in fruits, vegetables, and whole grains which has been shown to increase risk of chronic diseases(10-12). On the other hand, the “Eco-Atkins” diet, a low-calorie, low-carbohydrate diet with high amounts of plant protein and oils has shown to improve low density lipoprotein levels when compared with a high carbohydrate, lacto-ovo vegetarian diet (13). Because the leading causes of death in the U.S.–cardiovascular disease (CVD) and cancer(14)–develop over many years, long-term studies of low-carbohydrate diets are needed to evaluate effects on mortality. However, randomized trials of low-carbohydrate diets on mortality are not feasible because of the difficulty in maintaining compliance and follow-up over many years.
We previously developed three scores to characterize low-carbohydrates based on the proportion of carbohydrate, fat, and protein in the diet, and the contribution to these macronutrients from animal or vegetable sources(15). We found that women with higher low-carbohydrate diet scores did not have greater risk of type 2 diabetes and coronary heart disease and that a low-carbohydrate dietary pattern that emphasized vegetable sources of fat and protein was associated with a lower risk of both(15, 16). However, long-term data on low-carbohydrate diets and mortality are scarce. Two European cohorts reported that a low-carbohydrate-high protein diet was associated with a weak but statistical significant higher mortality(17, 18). These studies included only a few hundred deaths, and did not evaluate different sources of proteins and fat.
Therefore, we prospectively examined the relation between different types of low-carbohydrates diets and all-cause and cause-specific mortality in two large cohorts in the U. S.
Methods
Study Population
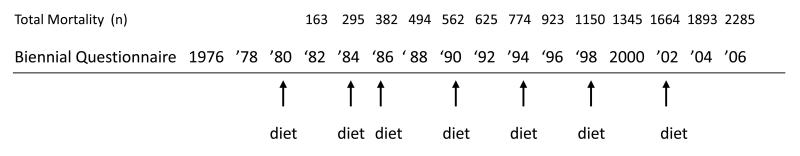
The Nurses' Health Study (NHS) is a cohort study of 121,700 female nurses aged 30-55 years living in 11 U.S. states established in 1976 (figure 1a). Questionnaires are sent biennially to collect medical, lifestyle, and other health-related information(19). In 1980, participants completed a 61-item food frequency questionnaire (FFQ). This was expanded to 116 items in 1984 and similar FFQs were sent in 1986, 1990, 1994, 1998, and 2002.
Figure 1a.
Timeline for Nurses' Health Study
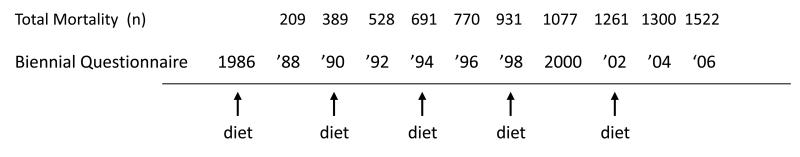
The Health Professionals' Follow-up Study (HPFS) was established in 1986 with 51,529 male podiatrists, optometrist, pharmacists, dentists, and veterinarians, aged 40 to 75 years (figure 1b). Questionnaire similar to the NHS are sent every two years, and an FFQ was sent every four years(20). Each FFQ contained approximately 130 questions on food intake. Follow-up was complete for over 90% in each 2-year cycle for both cohorts.
Figure 1b.
Timeline for Health Professionals' Follow-up Study
For this analysis, we used 1980 as baseline for NHS when the first dietary data were collected. We included women who completed the 1980 FFQ with <10 missing items and a plausible total energy intake (calculated from the FFQ, between 500 and 3500 kcal/day)(21). For HPFS, we included men with total energy intake (calculated from the FFQ) of 800 to 4200 kcal/day at baseline and <70 missing items. After excluding those with a history of cancer (women: 1579, men: 1998) (except non-melanoma skin cancer), heart disease (women: 772, men: 2077), and diabetes mellitus at baseline (women: 1858, men: 1284), we included 85,168 women with follow-up from 1980 through 2006, and 44,548 men with follow-up from 1986 to 2006. This study was approved by the Institutional Review Board of the Brigham and Women's Hospital, Boston, MA.
Dietary Assessment
Self-administered semi-quantitative FFQs were designed to assess average food intake over the preceding year. A standard portion size and nine possible consumption frequency categories, from “never, or <1/month” to “6+ times per day” were given for each food. Total energy and nutrient intake was calculated by summing up from all foods. Previous validation studies revealed reasonably good correlations between energy-adjusted nutrients assessed by the FFQ and multiple food records completed over the preceding year in both NHS(21) and HPFS(20).
The computation of low-carbohydrate diet scores was previously described in detail(15). Briefly, percentages of energy from fat, protein, and carbohydrate were divided into deciles. For fat and protein, participants in the highest decile received 10 points for that macronutrient and participants in the ninth decile received 9 points, and so forth. For carbohydrate, the lowest decile received 10 points and the highest zero points. The fat, protein, and carbohydrate scores were summed to create the overall low-carbohydrate-diet score, which ranged from 0-30. In addition, we also created a vegetable low-carbohydrate score, based on percent of energy of carbohydrate, vegetable protein, and vegetable fat; and an animal low-carbohydrate score based on percent energy as carbohydrate, animal protein, and animal fat. Thus, each participant was given the overall, animal and vegetable scores.
Ascertainment of deaths
Deaths were identified from state vital statistics records, the National Death Index, reported by the families, and the postal system. Cause of death was identified from death certificates or review of medical records. For this analysis, we evaluated all-cause mortality, death from CVD (International Classification of Diseases, eighth revision [ICD-8] codes 390 through 458), cancer (ICD-8 codes 140 through 207), death from colorectal (ICD-8 codes 153-154), lung (ICD-8 code 162), breast (ICD-8 code 174), and prostate (ICD-8 code 185) cancers. The follow-up for death in both cohorts is at least 95% complete(22).
Assessment of covariates
Body mass index (BMI) was calculated from weight reported on each biennial questionnaire and height reported at the first questionnaire. Smoking status and number of cigarette use, history of hypertension, aspirin use (number of tablets and frequency of use), regular intake of multivitamin, menopausal status and use of postmenopausal hormone therapy, parity, and age at first birth were assessed every 2 years. In the NHS, hours per week of vigorous activities was collected in 1980, 1982, and 1984. Leisure-time physical activity was measured 7 times beginning in 1986 with validated questions on 10 common activities in NHS and biennially from baseline in HPFS. The information was then summed and calculated as Metabolic Equivalent Hours (METs)(23). In NHS, we inquired about physical examinations (for screening purposes or to evaluate symptoms) at baseline and in both cohorts every two years beginning in 1988. Family history (1st degree relatives) of colorectal cancers, breast (women only), prostate cancer (men only), and information on having undergone colonoscopy and prostate specific antigen (PSA, men only) screening were also collected several times during follow-up.
Statistical analysis
We used Cox proportional hazard models to assess the association between the three low-carbohydrate diet scores and risk of all-cause mortality during follow-up. In addition, we separately analyzed CVD mortality, overall cancer mortality, and the leading causes of cancer deaths: lung, colorectal, breast (women only), and prostate (men only). All analyses were conducted separately for each cohort.
For analyses of all-cause, CVD, and cancer mortality, participants were divided into 10 categories (deciles) for each of the low-carbohydrate diet scores. For specific cancer deaths, participants were categorized into quintiles of low-carbohydrate diet scores because of smaller numbers of cases. To reduce random within-person variation and to best represent long-term dietary intake, we calculated cumulative averages of the 3 low-carbohydrate diet scores from our repeated FFQs (24). For example, in NHS, the low-carbohydrate diet score in 1980 was used to predict mortality between 1980 and 1984, the average score from 1980 and 1984 was used to predict mortality from 1984 to 1986, and so forth with cumulative dietary information for the entire follow-up duration. The same procedure was used in HPFS. However, dietary intake was not updated when the participants reported a diagnosis of cancer (except non-melanoma skin cancer), diabetes, stroke, coronary heart disease, or angina because these conditions may lead to changes in diet.
In multivariate analyses, we adjusted for age (continuous), physical activity (quintiles), BMI (5 categories), energy intake (quintiles), alcohol intake (4 categories), history of hypertension (yes/no), smoking (5 categories), and multivitamin use (yes/no) with updated information at each 2 year questionnaire cycle. In women, we also adjusted for menopausal status and post menopausal hormone use (4 categories). In secondary analysis, we also adjusted for having gone through a physical examination (yes/no) at each 2 year questionnaire cycle as this may be related to early disease detection and hence better prognosis. Individuals with missing BMI were excluded from baseline (2%). Smoking status was missing for 0.2% of the participants in NHS and 4% participants in HPFS at baseline. These individuals were represented by a missing indicator variable for smoking.
For analyses of deaths due to specific cancers, we used multivariate models that additionally included disease-specific risk factors. For breast cancer, we additionally adjusted for family history of breast cancer (yes/no), weight change since age 18 (7 categories), history of benign breast disease (yes/no), BMI at age 18 (4 categories), and height (4 categories). For analysis of prostate cancer, we additionally adjusted for family history of prostate cancer (yes/no), history of diabetes (yes/no), ethnicity (4 categories), height (5categories), vigorous (6+ METs) physical activity (quintiles), history of vasectomy (3 categories), BMI at age 21 (5categories), PSA screening (yes/no). For analysis of colorectal cancer, we additionally adjusted for history of colorectal polyps (yes/no), family history of colorectal cancer (yes/no), history colonoscopy (yes/no), aspirin use (yes/no). Cigarette smoking was modeled as pack years (5 categories). In analysis of lung cancer, covariates used in each cohort were slightly different due to availability of data. Therefore in women, we additionally adjusted for age at smoking initiation (continuous), and smoking status was modeled using six categories. In men, we adjusted for pack years (5 categories), parental smoking in childhood (3 categories), and adult environmental tobacco smoke exposure (4 categories).
Hazard ratios from each cohort were also pooled to obtain a summary risk estimate using a random effects model that allows for between-study heterogeneity(25). P-values for heterogeneity of study results were calculated using the Cochran Q test. Proportional hazard assumption for total mortality was tested with a time dependent variable by including an interaction term between the low carbohydrate diet score and the “month to death” variable. Statistical analysis was conducted with SAS version 9.1 (Cary, NC).
As a sensitivity analysis, we repeated our analysis using only baseline dietary information, and corrected for measurement error (26) in the assessment of the overall low-carbohydrate diet score using data from validation studies conducted in NHS (21) and HPFS (20). To explore residual confounding, we adjusted for major confounders with finer categories or as continuous variables in separate regression models, as well as computing and adjusting for a propensity score (27). We also conducted sensitivity analysis to examine the robustness of our results from influence of unmeasured confounding (28). We did not observe any material difference in results from these precautionary measures and therefore presented results with covariates adjusted in their original categories. We used a multiple imputation procedure, with 20 rounds of imputation and including all covariates to account for missing dietary and covariate data. We then repeated the analysis using non-cumulative updating of dietary information in which we use the most recent diet data to predict mortality (29).
Role of funding source
This study was supported by the National Institutes of Health. It had no role in the design and conduct of the study, analysis or interpretation of the data, or preparation or final approval of the manuscript before publication.
Results
In NHS with up to 26 years of follow-up, we documented 12,555 deaths, of which, 2,458 were cardiovascular deaths, and 5,780 were cancer deaths. Among the cancer deaths, 1,605 were from breast cancer, 547 from colorectal cancer, and 1,280 from lung cancer. In the HPFS with up to 20 years of follow-up, there were 8,678 deaths, of which 2,746 were CVD deaths, and 2,960 were cancer deaths. Among cancer deaths, 335 cases were from colorectal cancer, 563 from lung cancer, and 416 from prostate cancer.
Both men and women who had higher overall and animal low-carbohydrate scores had higher BMI and more likely to be current smokers, but lower intakes of fruits and vegetables (table 1). Conversely, those with higher vegetable low-carbohydrate score tended to have higher alcohol and whole grain intake. 1986 was chosen for consistency of data for men and women.
Table 1.
Age adjusted baseline lifestyle and 1986 dietary characteristics of participants according of deciles of low carbohydrate score*
| Overall score | Animal score | Vegetable score | |||||||
|---|---|---|---|---|---|---|---|---|---|
| D1 | D5 | D10 | D1 | D5 | D10 | D1 | D5 | D10 | |
| Women | |||||||||
| 1986 median score | 3 | 14 | 27 | 2 | 13 | 28 | 5 | 14 | 24 |
| BMI | 24.0 | 24.2 | 24.8 | 23.9 | 24.3 | 24.8 | 24.4 | 24.4 | 23.9 |
| Current smokers % | 30 | 27 | 33 | 27 | 28 | 32 | 30 | 27 | 30 |
| Physical activity (hours/wk) | 3.0 | 3.2 | 3.0 | 3.0 | 3.2 | 3.0 | 3.1 | 3.1 | 3.1 |
| Multivitamin use % | 33 | 34 | 35 | 33 | 35 | 35 | 36 | 34 | 35 |
| Energy intake (kcal) | 1821 | 1795 | 1641 | 1817 | 1804 | 1630 | 1811 | 1759 | 1748 |
| Alcohol intake (g) | 4 | 7 | 5 | 4 | 7 | 6 | 4 | 7 | 7 |
| Carbohydrates (% energy) | 60.5 | 50.9 | 37.2 | 59.6 | 50.4 | 37.4 | 56.0 | 48.8 | 42.8 |
| Animal protein (% energy) | 9.6 | 12.7 | 17.8 | 9.1 | 12.5 | 18.5 | 13.4 | 14.2 | 12.7 |
| Vegetable protein (% energy) | 5.4 | 5.2 | 4.5 | 5.9 | 5.2 | 4.2 | 4.1 | 4.9 | 6.0 |
| Animal fat (% energy) | 12.9 | 16.6 | 25.2 | 11.6 | 16.5 | 26.3 | 17.9 | 19.1 | 17.2 |
| Vegetable fat (% energy) | 12.9 | 13.8 | 14.7 | 15.5 | 15.0 | 12.2 | 9.4 | 12.3 | 21.1 |
| Saturated fat (g)† | 16 | 19 | 26 | 16 | 20 | 26 | 19 | 21 | 22 |
| Trans fat (g)† | 2.1 | 2.3 | 2.7 | 2.2 | 2.4 | 2.6 | 1.9 | 2.3 | 2.7 |
| Monounsaturated fat (g)† | 16 | 21 | 27 | 17 | 21 | 26 | 17 | 21 | 26 |
| Polyunsaturated fat (g)† | 9 | 11 | 12 | 10 | 11 | 11 | 8 | 10 | 15 |
| Omega 3 fatty acids (g)† | 1.0 | 1.2 | 1.3 | 1.1 | 1.2 | 1.3 | 1.0 | 1.2 | 1.4 |
| Whole grains (g)† | 19 | 16 | 9 | 21 | 15 | 9 | 12 | 15 | 14 |
| Fruits and vegetables (servings/day) | 7.4 | 6.8 | 5.2 | 7.6 | 6.7 | 5.1 | 6.5 | 6.5 | 6.0 |
| Red/processed meats (servings/day) | 0.6 | 0.8 | 1.3 | 0.5 | 0.8 | 1.3 | 0.8 | 0.9 | 0.8 |
| Sweetened soft drinks (servings/day) | 0.7 | 0.2 | 0.1 | 0.6 | 0.2 | 0.1 | 0.8 | 0.2 | 0.1 |
| Men | |||||||||
| 1986 median score | 3 | 14 | 27 | 2 | 14 | 28 | 6 | 14 | 24 |
| BMI | 24.7 | 25.4 | 26.5 | 24.5 | 25.4 | 26.6 | 25.5 | 25.6 | 25.6 |
| Current smokers % | 5 | 9 | 13 | 5 | 9 | 14 | 10 | 9 | 9 |
| Physical activity (METs/wk) | 27 | 22 | 17 | 28 | 21 | 16 | 21 | 22 | 20 |
| Multivitamin use % | 44 | 41 | 40 | 46 | 41 | 39 | 40 | 40 | 44 |
| Energy intake (kcal) | 2012 | 2007 | 1881 | 2010 | 1995 | 1867 | 2012 | 1971 | 2034 |
| Alcohol intake (g) | 9 | 13 | 8 | 7 | 12 | 10 | 8 | 12 | 12 |
| Carbohydrates (% energy) | 60.6 | 47.6 | 35.2 | 60.2 | 47.3 | 35.2 | 53.7 | 46.9 | 40.1 |
| Animal protein (% energy) | 9.2 | 13.1 | 18.2 | 8.9 | 13.2 | 18.8 | 13.7 | 13.9 | 12.6 |
| Vegetable protein ((% energy) | 5.7 | 5.0 | 4.3 | 6.2 | 5.0 | 3.9 | 4.0 | 4.8 | 6.1 |
| Animal fat (% energy) | 11.8 | 17.6 | 26.2 | 10.6 | 17.8 | 27.4 | 18.4 | 19.0 | 17.1 |
| Vegetable fat (% energy) | 12.3 | 13.5 | 13.8 | 14.4 | 13.9 | 11.5 | 8.9 | 12.5 | 21.1 |
| Saturated fat (g)† | 18 | 24 | 32 | 24 | 40 | 57 | 23 | 25 | 26 |
| Trans fat (g)† | 2.2 | 2.8 | 3.2 | 2.3 | 2.9 | 3.2 | 2.4 | 2.9 | 3.0 |
| Monounsaturated fat (g)† | 20 | 26 | 35 | 21 | 27 | 33 | 23 | 27 | 34 |
| Polyunsaturated fat (g)† | 11 | 13 | 15 | 12 | 13 | 14 | 10 | 13 | 18 |
| Omega 3 fatty acids (g)† | 1.2 | 1.4 | 1.6 | 1.3 | 1.4 | 1.5 | 1.1 | 1.4 | 1.6 |
| Whole grains (g)† | 32 | 22 | 14 | 36 | 21 | 13 | 18 | 22 | 21 |
| Fruits and vegetables (servings/day) | 7.3 | 5.5 | 4.3 | 7.6 | 5.5 | 4.2 | 5.7 | 5.7 | 5.3 |
| Red/processed meats (servings/day) | 0.4 | 0.6 | 1.2 | 0.3 | 0.8 | 1.3 | 0.8 | 0.8 | 0.8 |
| Sweetened soft drinks (servings/day) | 0.8 | 0.3 | 0.1 | 0.6 | 0.4 | 0.2 | 0.9 | 0.3 | 0.1 |
Baseline deciles for lifestyle characteristics and 1986 deciles for dietary intake. Data are means unless otherwise stated. BMI=body mass index, MET=metabolic equivalent hours.
energy adjusted by the residual method
After adjusting for potential confounders, we observed a modest but statistically higher risk for all-cause mortality with the animal low-carbohydrate score (HR comparing extreme deciles of animal score for HPFS=1.31, 95% CI=1.19-1.44, p trend<0.001; for NHS: HR=1.17, 95% CI=1.08-1.26, p trend<0.001) (table 2). The pooled HR was 1.23 (95% CI=1.11-1.37, p trend=0.051). In both cohorts, similar inverse associations were observed between the vegetable score and all-cause mortality, with the pooled HR comparing extreme deciles=0.80 (95% CI=0.75-0.85, p trend<0.001).
Table 2.
Hazard ratios (95% CI) for all-cause mortality by deciles of low carbohydrate scores
| D1 | D2 | D3 | D4 | D5 | D6 | D7 | D8 | D9 | D10 | P trend | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall low carbohydrate score | |||||||||||
| MEN | |||||||||||
| Number of cases | 871 | 834 | 916 | 877 | 872 | 868 | 861 | 871 | 880 | 828 | |
| Age and energy adjusted | 1 | 0.91 | 1.05 | 0.98 | 0.96 | 1.07 | 1.07 | 1.14 | 1.17 | 1.33 (1.20, 1.46) | <0.001 |
| Multivariate* | 1 | 1.03 | 1.14 | 1.11 | 1.05 | 1.25 | 1.20 | 1.19 | 1.22 | 1.19 (1.07, 1.31) | <0.001 |
| WOMEN | |||||||||||
| Number of cases | 1406 | 1350 | 1262 | 1297 | 1227 | 1146 | 1178 | 1258 | 1199 | 1232 | |
| Age and energy adjusted | 1 | 0.94 | 0.92 | 0.94 | 0.91 | 0.95 | 0.94 | 1.02 | 1.05 | 1.19 (1.10, 1.28) | 0.47 |
| Multivariate* | 1 | 1.08 | 1.08 | 1.14 | 1.04 | 1.13 | 1.10 | 1.15 | 1.14 | 1.07 (0.99, 1.15) | 0.135 |
| POOLED (multivariate) | 1 | 1.06 | 1.10 | 1.13 | 1.04 | 1.18 | 1.15 | 1.14 | 1.17 | 1.12 (1.01, 1.24) | 0.136† |
| Animal low carbohydrate score | |||||||||||
| MEN | |||||||||||
| Number of cases | 832 | 808 | 877 | 837 | 876 | 811 | 899 | 926 | 893 | 919 | |
| Age and energy adjusted | 1 | 1.00 | 1.03 | 1.03 | 1.07 | 1.10 | 1.19 | 1.27 | 1.33 | 1.52 (1.38, 1.67) | <0.001 |
| Multivariate* | 1 | 1.07 | 1.12 | 1.13 | 1.17 | 1.24 | 1.26 | 1.32 | 1.32 | 1.31 (1.19, 1.44) | <0.001 |
| WOMEN | |||||||||||
| Number of cases | 1350 | 1269 | 1271 | 1185 | 1252 | 1106 | 1252 | 1218 | 1324 | 1328 | |
| Age and energy adjusted | 1 | 0.94 | 0.99 | 0.95 | 1.00 | 0.97 | 1.03 | 1.13 | 1.22 | 1.35(1.25, 1.46) | <0.001 |
| Multivariate* | 1 | 1.07 | 1.16 | 1.09 | 1.14 | 1.13 | 1.16 | 1.22 | 1.26 | 1.17 (1.08, 1.26) | <0.001 |
| POOLED (multivariate) | 1 | 1.07 | 1.14 | 1.12 | 1.15 | 1.18 | 1.20 | 1.26 | 1.28 | 1.23 (1.11, 1.37) | 0.051† |
| Vegetable low carbohydrate score | |||||||||||
| MEN | |||||||||||
| Number of cases | 1095 | 971 | 903 | 936 | 767 | 903 | 788 | 830 | 764 | 721 | |
| Age and energy adjusted | 1 | 0.92 | 0.83 | 0.92 | 0.80 | 0.81 | 0.75 | 0.79 | 0.80 | 0.77 (0.70, 0.85) | <0.001 |
| Multivariate* | 1 | 0.97 | 0.94 | 0.98 | 0.92 | 0.93 | 0.84 | 0.96 | 0.87 | 0.81 (0.74, 0.89) | <0.001 |
| WOMEN | |||||||||||
| Number of cases | 1565 | 1470 | 1342 | 1330 | 1101 | 1323 | 1180 | 1093 | 1029 | 1122 | |
| Age and energy adjusted | 1 | 0.91 | 0.860 | 0.79 | 0.81 | 0.75 | 0.75 | 0.73 | 0.69 | 0.76 (0.71, 0.82) | <0.001 |
| Multivariate* | 1 | 1.01 | 1.02 | 0.91 | 1.00 | 0.87 | 0.86 | 0.87 | 0.81 | 0.79 (0.73, 0.85) | <0.001 |
| POOLED (multivariate) | 1 | 0.99 | 0.98 | 0.94 | 0.97 | 0.90 | 0.85 | 0.91 | 0.85 | 0.80 (0.75, 0.85) | <0.001 |
adjusted for age, physical activity, BMI, energy intake, alcohol intake, menopausal status and post menopausal hormone use, history of hypertension, smoking, multivitamin use.
p<0.05 for test for heterogeneity
For CVD mortality, a modest but statistically significant direct association was observed with the overall low-carbohydrate score in men only (table 3). However, the animal-based score showed a direct association in the pooled analysis (HR=1.14, 95% CI=1.01-1.29, p trend=0.029 for animal score). Results for the vegetable-based score were similar for men and women, and the pooled HR for CVD mortality was 0.77 (95% CI=0.68-0.87, p trend<0.001) for extreme deciles.
Table 3.
Hazard ratios (95% CI) for cardiovascular mortality by deciles of low carbohydrate scores
| D1 | D2 | D3 | D4 | D5 | D6 | D7 | D8 | D9 | D10 | P trend§ | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall low carbohydrate score | |||||||||||
| MEN | |||||||||||
| Number of cases | 284 | 264 | 295 | 296 | 281 | 275 | 267 | 276 | 263 | 245 | |
| Age and energy adjusted | 1 | 0.90 | 1.05 | 1.05 | 0.99 | 1.07 | 1.07 | 1.18 | 1.13 | 1.31 (1.10, 1.56) | <0.001 |
| Multivariate* | 1 | 0.98 | 1.10 | 1.14 | 1.04 | 1.17 | 1.14 | 1.20 | 1.14 | 1.15 (0.96, 1.37) | 0.008 |
| WOMEN | |||||||||||
| Number of cases | 280 | 284 | 251 | 274 | 248 | 207 | 214 | 239 | 224 | 237 | |
| Age and energy adjusted | 1 | 1.01 | 0.94 | 1.05 | 0.96 | 0.91 | 0.91 | 1.06 | 1.08 | 1.27 (1.07, 1.51) | 0.43 |
| Multivariate* | 1 | 1.16 | 1.08 | 1.24 | 1.08 | 1.03 | 1.01 | 1.12 | 1.09 | 1.00 (0.84, 1.20) | 0.54 |
| POOLED (multivariate) | 1 | 1.07 | 1.08 | 1.18 | 1.06 | 1.10 | 1.08 | 1.16 | 1.11 | 1.08 (0.95, 1.22) | 0.153 |
| Animal low carbohydrate score | |||||||||||
| MEN | |||||||||||
| Number of cases | 270 | 269 | 270 | 271 | 306 | 254 | 267 | 284 | 291 | 264 | |
| Age and energy adjusted | 1 | 1.03 | 0.99 | 1.07 | 1.20 | 1.09 | 1.11 | 1.25 | 1.40 | 1.42 (1.20, 1.69) | <0.001 |
| Multivariate* | 1 | 1.09 | 1.04 | 1.13 | 1.25 | 1.19 | 1.13 | 1.25 | 1.36 | 1.21 (1.01, 1.44) | <0.001 |
| WOMEN | |||||||||||
| Number of cases | 278 | 231 | 269 | 234 | 255 | 232 | 226 | 247 | 233 | 255 | |
| Age and energy adjusted | 1 | 0.85 | 1.04 | 0.96 | 1.04 | 1.04 | 0.97 | 1.19 | 1.15 | 1.39 (1.17, 1.65) | 0.29 |
| Multivariate* | 1 | 0.95 | 1.19 | 1.07 | 1.14 | 1.15 | 1.03 | 1.21 | 1.09 | 1.07 (0.90, 1.28) | 0.102 |
| POOLED (multivariate) | 1 | 1.01 | 1.11 | 1.10 | 1.20 | 1.17 | 1.08 | 1.23 | 1.22 | 1.14 (1.01, 1.29) | 0.029 |
| Vegetable low carbohydrate score | |||||||||||
| MEN | |||||||||||
| Number of cases | 373 | 308 | 281 | 291 | 245 | 310 | 237 | 255 | 235 | 211 | |
| Age and energy adjusted | 1 | 0.86 | 0.79 | 0.78 | 0.78 | 0.85 | 0.69 | 0.76 | 0.76 | 0.72 (0.61, 0.86) | <0.001 |
| Multivariate* | 1 | 0.91 | 0.88 | 0.93 | 0.88 | 0.98 | 0.77 | 0.91 | 0.84 | 0.77 (0.65, 0.92) | 0.002 |
| WOMEN | |||||||||||
| Number of cases | 331 | 320 | 271 | 280 | 203 | 242 | 209 | 193 | 186 | 223 | |
| Age and energy adjusted | 1 | 0.94 | 0.82 | 0.79 | 0.72 | 0.67 | 0.63 | 0.63 | 0.61 | 0.74 (0.62, 0.87) | <0.001 |
| Multivariate* | 1 | 1.06 | 0.99 | 0.92 | 0.89 | 0.79 | 0.75 | 0.76 | 0.73 | 0.77 (0.66, 0.91) | <0.001 |
| POOLED (multivariate) | 1 | 0.98 | 0.93 | 0.93 | 0.89 | 0.88f | 0.76 | 0.84 | 0.79 | 0.77 (0.68, 0.87) | <0.001 |
adjusted for age, physical activity, BMI, energy intake, alcohol intake, menopausal status and post menopausal hormone use, history of hypertension, smoking, multivitamin use.
p<0.05 for test for heterogeneity
For total cancer deaths, a statistically significant direct association was observed with the overall low-carbohydrate score in men (HR comparing extreme deciles1.32, 95% CI=1.11-1.57, p trend<0.001) (table 4). A slightly stronger association was observed with the animal low-carbohydrate score in men (HR=1.45, 95% CI=1.23-1.72, p trend<0.001). However, the same association was weaker in women and did not reach statistical significance in the sensitivity analysis when smoking and physical activity was modeled in finer categories. In addition, no association was observed with the vegetable low-carbohydrate score in either men or women.
Table 4.
Hazard ratios (95% CI) for cancer mortality by deciles of low carbohydrate scores
| D1 | D2 | D3 | D4 | D5 | D6 | D7 | D8 | D9 | D10 | P trend | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall low carbohydrate score | |||||||||||
| MEN | |||||||||||
| Number of cases | 260 | 270 | 303 | 311 | 296 | 302 | 293 | 307 | 327 | 291 | |
| Age and energy adjusted | 1 | 0.98 | 1.14 | 1.13 | 1.07 | 1.23 | 1.16 | 1.28 | 1.37 | 1.45 (1.22, 1.71) | <0.001 |
| Multivariate* | 1 | 1.08 | 1.22 | 1.25 | 1.15 | 1.40 | 1.29 | 1.33 | 1.41 | 1.32 (1.11, 1.57) | <0.001 |
| WOMEN | |||||||||||
| Number of cases | 595 | 592 | 580 | 584 | 567 | 539 | 565 | 602 | 583 | 573 | |
| Age and energy adjusted | 1 | 0.95 | 0.96 | 0.96 | 0.94 | 0.99 | 1.00 | 1.06 | 1.11 | 1.16 (1.04, 1.31) | 0.28 |
| Multivariate* | 1 | 1.06 | 1.10 | 1.12 | 1.05 | 1.15 | 1.14 | 1.17 | 1.20 | 1.10 (0.98, 1.23) | 0.056 |
| POOLED (multivariate) | 1 | 1.07 | 1.16 | 1.16 | 1.08 | 1.26 | 1.20 | 1.23 | 1.29 | 1.19 (0.99, 1.42) | 0.128† |
| Animal low carbohydrate score | |||||||||||
| MEN | |||||||||||
| Number of cases | 255 | 253 | 316 | 272 | 287 | 293 | 338 | 312 | 307 | 327 | |
| Age and energy adjusted | 1 | 1.01 | 1.20 | 1.05 | 1.12 | 1.25 | 1.45 | 1.33 | 1.41 | 1.66 (1.40, 1.96) | <0.001 |
| Multivariate* | 1 | 1.07 | 1.28 | 1.15 | 1.21 | 1.38 | 1.53 | 1.38 | 1.40 | 1.45 (1.23, 1.72) | <0.001 |
| WOMEN | |||||||||||
| Number of cases | 591 | 585 | 565 | 530 | 590 | 499 | 607 | 550 | 659 | 604 | |
| Age and energy adjusted | 1 | 0.98 | 0.97 | 0.93 | 1.02 | 0.95 | 1.07 | 1.08 | 1.27 | 1.26 (1.13, 1.41) | 0.005 |
| Multivariate* | 1 | 1.08 | 1.10 | 1.04 | 1.14 | 1.08 | 1.19 | 1.15 | 1.32 | 1.15 (1.02, 1.29) | 0.001 |
| POOLED (multivariate) | 1 | 1.08 | 1.17 | 1.07 | 1.16 | 1.21† | 1.33† | 1.25 | 1.34 | 1.28 (1.02, 1.60) † | 0.089† |
| Vegetable low carbohydrate score | |||||||||||
| MEN | |||||||||||
| Number of cases | 310 | 341 | 288 | 336 | 276 | 292 | 275 | 301 | 274 | 267 | |
| Age and energy adjusted | 1 | 1.16 | 0.93 | 1.01 | 1.02 | 0.88 | 0.93 | 0.85 | 0.99 | 0.97 (0.82, 1.15) | 0.120 |
| Multivariate* | 1 | 1.21 | 1.03 | 1.16 | 1.15 | 0.98 | 1.02 | 1.11 | 1.09 | 1.00 (0.84, 1.18) | 0.35 |
| WOMEN | |||||||||||
| Number of cases | 612 | 637 | 632 | 538 | 535 | 634 | 567 | 557 | 522 | 546 | |
| Age and energy adjusted | 1 | 1.00 | 1.03 | 0.83 | 0.98 | 0.89 | 0.92 | 0.91 | 0.88 | 0.91 (0.81, 1.02) | 0.36 |
| Multivariate* | 1 | 1.08 | 1.17 | 0.93 | 1.15 | 0.99 | 1.04 | 1.06 | 0.99 | 0.94 (0.84, 1.06) | 0.39 |
| POOLED (multivariate) | 1 | 1.13 | 1.12 | 1.03† | 1.15 | 0.99 | 1.04 | 1.07 | 1.03 | 0.96 (0.87, 1.05) | 0.23 |
adjusted for age, physical activity, BMI, energy intake, alcohol intake, menopausal status and post menopausal hormone use, history of hypertension, smoking, multivitamin use.
p<0.05 for test for heterogeneity
A direct association was observed between the animal low-carbohydrate score and colorectal cancer death when data were combined (HR comparing extreme quintiles=1.31, 95% CI=1.06-1.62, p trend=0.048) (table 5, online appendix). In both cohorts, the overall and animal low-carbohydrate scores were positively associated with lung cancer mortality, with the pooled hazard ratio for the overall low-carbohydrate score of 1.22 (95% CI=1.05-1.42, p trend=0.003) comparing top to bottom quintiles (table 5). The vegetable low-carbohydrate score was not associated with lung cancer deaths. After adjusting for risk factors relevant to specific cancers, none of the low-carbohydrate scores was associated with breast cancer or prostate cancer death.
Additional adjustment for physical examinations to reduce the possibility of confounding by late detection and hence more fatal diseases showed similar results. We also repeated our analysis with continuous updating dietary information even after diagnosis of chronic diseases, but adjusted for the self-reported diagnosis in the regression models. In both cohorts, neither the relative risks nor the p-values were changed. Bonferroni correction for multiple comparison for gender-specific analysis did not change the conclusion of the results for all-cause, CVD, or cancer mortality, and statistically significant associations remained significant.
Less than 25% of either NHS or HPFS participants missed more than 2 FFQs during the follow-up period. However, results for the animal and vegetable low carbohydrate scores remained statistically significant when the multiple imputation procedure was used to account for missing data. In NHS, the HR for a 10 point increase in the animal score was 1.09 (p<0.0001) for total mortality and the corresponding HR in HPFS was 1.06 (p=0.0003). Using baseline dietary data and after adjusting for measurement error in diet, conclusions for the overall low-carbohydrate diet score and total mortality were not materially changed. For example, HR for 10 points increase in baseline overall score was 1.04 (p=0.38) for corrected data and 1.01 (p=0.65) for uncorrected data in NHS. In HPFS, HR for 10 points increase in the baseline overall score was 1.20 (p<0.0001) for corrected data and 1.10 (p=0.0004) for uncorrected data. The test for proportional hazard assumption for total mortality analysis was not significant (p= 0.42 for NHS and p = 0.45 for HPFS).
Discussion
In our two cohorts of U.S. men and women with up to 20-26 years of follow-up, we observed that the overall low-carbohydrate diet score was only weakly associated with all-cause mortality. However, a higher animal low-carbohydrate diet score was associated with higher all-cause and cancer mortality, while a higher vegetable low-carbohydrate score was associated with lower mortality, particularly CVD mortality.
A search in the English medical literature of the past 10 years found only two long term observational studies of low carbohydrate diet and mortality. A Swedish study in women used an overall score with a scoring algorithm similar to ours, but only considered protein and carbohydrate intakes(17). After up to 12 years of follow-up, the high-protein-low-carbohydrate score was associated with CVD death only among women aged 40-49 years at baseline but not among younger women (HR=1.21 for each 10% increment in score). There was no association with all-cause or cancer mortality. Using the same calculation as the Swedish study, the high protein-low-carbohydrate score was associated with a weak but statistically significant increased risk in all-cause mortality (HR=1.08 for each 10% increment) among Greek participants of the European Prospective Investigation Cancer and Nutrition (EPIC) study during 10 years of follow-up(18). Similar associations were observed for cardiovascular and cancer mortality. Dietary protein and fat can come from foods with widely different nutrient profiles. Our animal and vegetable low-carbohydrate scores allowed us to better discern whether any association between low-carbohydrate scores and mortality is due mainly to different sources of macronutrients especially fat and protein. We observed stronger direct associations with mortality with the animal but not with the vegetable low-carbohydrate score, suggesting that animal- and plant-based foods have a differential impact on mortality.
Consistent with our results, higher intake of vegetable protein, but not animal protein, was associated with a lower risk of coronary heart disease mortality in the Iowa Women's Health Study(30). The lower CVD mortality observed with higher vegetable low-carbohydrate score in our study is likely in part due to the established benefit of unsaturated fats, dietary fiber, and micronutrients such as magnesium and potassium, as well as other bioactive compounds including vitamins, minerals, and phytochemical (31). Because low-carbohydrate diets may have variable amounts of plant or animal fat, this may explain why low-carbohydrate diets showed mixed results on lipid profile(9).
We found a positive association between animal and low-carbohydrate score and cancer mortality. Diets high in red and processed meats have been associated with higher risk of lung cancer in case-control(32, 33) and prospective studies(34). Therefore, the direct association with the animal based low-carbohydrate score in our study may be partly due to higher red and processed meat intake. Dietary fat, however, does not appear to be associated with lung cancer risk(35). The association between red and processed meats intake and risk of colorectal cancer is well established(36), and may explain the higher risk of colorectal cancer deaths among participants with higher animal low-carbohydrate score.
Low-carbohydrate diets from animal and vegetable sources may have similar major macronutrient content, but the source of the macronutrients can result in large differences in dietary components that may affect mortality, such as specific fatty acids, protein, fiber, vitamins and minerals, and phytochemicals. Therefore, the associations that we observed are more likely to be mediated by these bioactive components rather the carbohydrate content.
The large number of cases in our cohort allowed us to conduct meaningful statistical analysis for specific causes of death. The availability of detailed and updated data on covariates allowed us to better control for confounding. But as with other observational studies, some degree of measurement error in reporting dietary and other lifestyle characteristics is inevitable. Therefore, we used multiple strategies in an attempt to reduce some of those biases. We used a validated FFQ, and our participants' training in clinical sciences would allow them to report health data accurately. In sensitivity analyses, we modeled major confounders in finer categories, included a propensity score, explored the influence of residual confounding. We compared our main results with those corrected for measurement error in baseline diet with data from validation studies. Most of the risk estimates were not changed substantially and the conclusions remained unchanged. We also considered the influence of unmeasured confounding using a sensitivity analysis (28). We found that for HPFS, the unmeasured confounder would have to have a prevalence of 40% among those at the highest decile of the animal score and a hazard ratio of 2.0 with total morality to attenuate the association to non-statistical significance. In NHS, the corresponding parameters for the unmeasured confounder would have to be 20% prevalence and HR of 2.0 to attenuate the association to non-significance. Since important confounders for the analyses of total and disease-specific mortality were controlled for, it is unlikely that such strong confounding would remain to explain the observed associations.
Because of the long follow-up, participants could have changed their diet after developed non-fatal CVD or cancer. We reduced the impact of this by not updating dietary information after such diagnosis in our main analysis. In a different approach, we updated dietary information regardless of a diagnosis of chronic disease but adjust for the diagnosis in the regression model. Missing data were imputed using a sophisticated procedure. None of these additional analyses materially changed the results.
The low-carbohydrate diet scores used in this study was not designed to mimic any particular versions of low-carbohydrate diets available in the popular literature. Therefore the risk estimates do not directly translate to the assessment of benefit or risk associated with the popular versions of the diet. In addition, the participants of our cohorts have higher educational status and better availability of health care coverage. Therefore, results may not be directly generalizable to the general population.
In conclusion, consumption of a vegetable-based low-carbohydrate diet were associated with a lower risk of all-cause and CVD mortality whereas a high scores for the animal-based low-carbohydrate diet were associated with a higher risk of overall mortality. These results suggest that the health effects of a low-carbohydrate diet may depend on the type of protein and fat, and that a diet including mostly vegetable sources of protein and fat is preferable to a diet with mostly animal sources of protein and fat.
Supplementary Material
Acknowledgement
The authors thank Dr. Tricia Y. Li for statistical and programming support.
Funding: National Institutes of Health grants CA87969, HL60712, and CA95589
References
- 1.Atkins Nutritionals I. 2008 [Google Scholar]
- 2.Chauncey KB. Low-carb dieting for dummies. John Wiley & Sons, Inc; 2003. [Google Scholar]
- 3.Foster GD, Wyatt HR, Hill JO, et al. A randomized trial of a low-carbohydrate diet for obesity. New England Journal of Medicine. 2003;328:2082–2090. doi: 10.1056/NEJMoa022207. [DOI] [PubMed] [Google Scholar]
- 4.Sacks FM, Bray GA, Carey VJ, et al. Comparison of weight-loss diets with different compositions of fat, protein, and carbohydrates. New England Journal of Medicine. 2009;360:859–873. doi: 10.1056/NEJMoa0804748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gardner CD, Kiazand A, Alhassan S, et al. Comparison of the Atkins, Zone, Ornish, and LEARN diets for change in weight and related risk factors among overweight premenopausal women: the A TO Z Weight Loss Study: a randomized trial. Journal of the American Medical Association. 2007;297:969–977. doi: 10.1001/jama.297.9.969. [DOI] [PubMed] [Google Scholar]
- 6.Shai I, Schwarzfuchs D, Henkin Y, et al. Weight Loss with a Low-Carbohydrate, Mediterranean, or Low-Fat Diet. New England Journal of Medicine. 2008;359:229–241. doi: 10.1056/NEJMoa0708681. [DOI] [PubMed] [Google Scholar]
- 7.McMillian-Price J, Petocz P, Atkinson F, et al. Comparison of 4 diets of varying glycemic load on weight loss and cardiovascular risk reduction in overweight and obese young adults: a randomized controlled trial. Archives of Internal Medicine. 2006;166:1466–1475. doi: 10.1001/archinte.166.14.1466. [DOI] [PubMed] [Google Scholar]
- 8.Muzio F, Mondazzi L, Harris WS, Sommariva D, Branchi A. Effects of moderate variations in the macronutrient content of the diet on cardiovascular disease risk factors in obese patients with the metabolic syndrome. American Journal of Clinical Nutrition. 2007;86:946–951. doi: 10.1093/ajcn/86.4.946. [DOI] [PubMed] [Google Scholar]
- 9.Nordmann AJ, Nordmann A, Briel M, et al. Effects of low-carbohydrate vs low-fat diets on weight loss and cardiovascular risk factors: a meta-analysis of randomized controlled trials. Archives of Internal Medicine. 2006;166:285–293. doi: 10.1001/archinte.166.3.285. [DOI] [PubMed] [Google Scholar]
- 10.Chao A, Thun MJ, Connell CJ, et al. Meat consumption and risk of colorectal cancer. Journal of the American Medical Association. 2005;293:172–182. doi: 10.1001/jama.293.2.172. [DOI] [PubMed] [Google Scholar]
- 11.Sandhu MS, White IR, McPherson K. Systematic review of the prospective cohort studies on meat consumption and colorectal cancer risk: a meta-analytical approach. Cancer Epidemiology, Biomarkers & Prevention. 2001;10:439–446. [PubMed] [Google Scholar]
- 12.Benetou V, Orfanos P, Lagiou P, Trichopoulos D, Boffetta P, Trichopoulou A. Vegetables and fruits in relation to cancer risk: evidence from the Greek EPIC cohort study. Cancer Epidemiology, Biomarkers & Prevention. 2008;17:387–392. doi: 10.1158/1055-9965.EPI-07-2665. [DOI] [PubMed] [Google Scholar]
- 13.Jenkins DJ, Wong JM, Kendall CW, et al. The effect of a plant-based low-carbohydrate (“Eco-Atkins”) diet on body weight and blood lipid concentrations in hyperlipidemic subjects. Archives of Internal Medicine. 2009;169:1046–1054. doi: 10.1001/archinternmed.2009.115. [DOI] [PubMed] [Google Scholar]
- 14.Kung HC, Hoyert DL, Xu J, Murphy SL. (National Center for Health Statistics) Deaths: Final Data for 2005. 2008 [PubMed] [Google Scholar]
- 15.Halton TL, Willett WC, Liu S, et al. Low-Carbohydrate-Diet Score and the Risk of Coronary Heart Disease in Women. New England Journal of Medicine. 2006;355:1991–2002. doi: 10.1056/NEJMoa055317. [DOI] [PubMed] [Google Scholar]
- 16.Halton TL, Liu S, Manson JE, Hu FB. Low-carbohydrate-diet score and risk of type 2 diabetes in women. American Journal of Clinical Nutrition. 2008;87:339–346. doi: 10.1093/ajcn/87.2.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lagiou P, Sandin S, Weiderpass E, et al. Low carbohydrate-high protein diet and mortality in a cohort of Swedish women. Journal of Internal Medicine. 2007;261:366–374. doi: 10.1111/j.1365-2796.2007.01774.x. [DOI] [PubMed] [Google Scholar]
- 18.Trichopoulou A, Psaltopoulou T, Orfanos P, Hsieh CC, Trichopoulos D. Low-carbohydrate–high-protein diet and long-term survival in a general population cohort. European Journal of Clinical Nutrition. 2007;61:575–581. doi: 10.1038/sj.ejcn.1602557. [DOI] [PubMed] [Google Scholar]
- 19.Colditz GA, Martin P, Stampfer MJ, et al. Validation of questionaire information on risk factors and disease outcomes in a prospetive cohort of women. American Journal of Epidemiology. 1986;123:894–900. doi: 10.1093/oxfordjournals.aje.a114319. [DOI] [PubMed] [Google Scholar]
- 20.Rimm EB, Giovannucci EL, Stampfer MJ, Colditz GA, Litin LB, Willett WC. Reproducibility and validity of an expanded self-administered semiquantitative food frequency questionnaire among male health professonals. American Journal of Epidemiology. 1992;135:1114–1126. doi: 10.1093/oxfordjournals.aje.a116211. [DOI] [PubMed] [Google Scholar]
- 21.Willett WC. Nutritional Epidemiology. Oxford Univeristy Press; New York: 1998. [Google Scholar]
- 22.Rich-Edwards JW, Corsano KA, Stampfer MJ. Test of the National Death Index and Equifax Nationwide Death Search. American Journal of Epidemiology. 1994;140:1016–1019. doi: 10.1093/oxfordjournals.aje.a117191. [DOI] [PubMed] [Google Scholar]
- 23.Ainsworth BE, Haskell WL, Whitt MC, et al. Compendium of physical activities: an update of activity codes and MET intensities. Medicine and Science in Sports and Exercise. 2000;32(9 Suppl):S498–504. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- 24.Hu FB, Stampfer MJ, Rimm E, et al. Dietary fat and coronary heart disease: a comparison of approaches for adjusting for total energy intake and modeling repeated dietary measurements. American Journal of Epidemiology. 1999;149:531–540. doi: 10.1093/oxfordjournals.aje.a009849. [DOI] [PubMed] [Google Scholar]
- 25.DerSimonian R, Laird N. Meta-analysis in clincial trials. Control Clinical Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 26.Spiegelman D, McDermott A, Rosner BA. Regression calibration method for correcting measurement-error bias in nutritional epidemiology. American Journal of Clinical Nutrition. 1997;65(suppl):1179s–1186s. doi: 10.1093/ajcn/65.4.1179S. [DOI] [PubMed] [Google Scholar]
- 27.D'Agostino RBJ. Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Statistics in Medicine. 1998;17:2265–2281. doi: 10.1002/(sici)1097-0258(19981015)17:19<2265::aid-sim918>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 28.Lin DY, Psaty BM, Kronmal RA. Assessing the sensitivity of regression results to unmeasured confounders in observational studies. Biometrics. 1998;54:948–963. [PubMed] [Google Scholar]
- 29.Rubin D. Multiple imputation for nonresponse in surveys. Wiley; New York: 1987. [Google Scholar]
- 30.Kelemen LE, Kushi LH, Jacobs DRJ, Cerhan JR. Associations of Dietary Protein with Disease and Mortality in a Prospective Study of Postmenopausal Women. American Journal of Epidemiology. 2005;161:239–249. doi: 10.1093/aje/kwi038. [DOI] [PubMed] [Google Scholar]
- 31.Hu FB, Willett WC. Optimal diets for prevention of coronary heart disease. Journal of the American Medical Association. 2002;288:2569–2578. doi: 10.1001/jama.288.20.2569. [DOI] [PubMed] [Google Scholar]
- 32.De Stefani E, Boffetta P, Ronco AL, et al. Nutrient patterns and risk of lung cancer: a factor analysis in Uruguayan men. Lung Cancer. 2008;3:283–291. doi: 10.1016/j.lungcan.2008.01.004. [DOI] [PubMed] [Google Scholar]
- 33.Lam TK, Cross AJ, Consonni D, et al. Intakes of red meat, processed meat, and meat mutagens increase lung cancer risk. Cancer Research. 2009;69:932–939. doi: 10.1158/0008-5472.CAN-08-3162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cross AJ, Leitzmann MF, Gail MH, Hollenbeck AR, Schatzkin A, Sinha R. A prospective study of red and processed meat intake in relation to cancer risk. PLoS Medicine. 2007;12:e325. doi: 10.1371/journal.pmed.0040325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Smith-Warner SA, Ritz J, Hunter D, et al. Dietary fat and risk of lung cancer in a pooled analysis of prospective studies. Cancer Epidemiology, Biomarkers & Prevention. 2002;11:987–992. [PubMed] [Google Scholar]
- 36.Larsson SC, Wolk A. Meat consumption and risk of colorectal cancer: a meta-analysis of prospective studies. International Journal of Cancer. 2006;119:2657–2664. doi: 10.1002/ijc.22170. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.