Abstract
Family functioning and parenting were hypothesized to mediate the relation between remission of maternal depression and children's psychosocial adjustment. Participants were 114 mother-child dyads participating in the Sequenced Treatment Alternatives to Relieve Depression Child 3-month follow-up. All mothers had been diagnosed with major depressive disorder and were treated initially with citalopram; 33% of mothers experienced remission of depressive symptoms. Youth ranged in age from 7 to 17. Remission of maternal depression was associated with changes in children's reports of their mothers' warmth/acceptance, which in turn partially mediated the relation between maternal depression remission and youth internalizing symptoms, accounting for 22.9% of the variance.
Maternal depression is a significant risk factor for children, increasing a child's odds of developing both internalizing (e.g., depression, anxiety) and externalizing (e.g., behavioral) problems (Munson, McMahon, & Spieker, 2001; Weissman, Wickramaratne, et al., 2006). In addition, maternal depression negatively impacts parenting, family functioning, and family relationships (Goodman & Gotlib, 2002; Lovejoy, Graczyk, O'Hare, & Neuman, 2000). Theories (e.g., Cummings, Davies, & Campbell, 2000) suggest that one mechanism by which maternal depression may impact children's functioning is via its deleterious effects on parenting and the family environment.
Although there are several efficacious treatments for adult major depression (Elkin, Shea, Watkins, & Imber, 1989), few studies have examined the extent to which bringing a mother's depression into remission, or significantly reducing her symptoms, may beneficially impact her children. Furthermore, even fewer studies have examined the impact of maternal depression remission on parenting, family functioning, or family relationships. The Sequenced Treatment Alternatives to Relieve Depression (STAR*D) Child study was designed to address these questions. STAR*D Child is an ancillary study to the larger STAR*D, which was a multisite study of treatment for adults with major depressive disorder (MDD;Rush et al., 2004). The primary aim of the STAR*D Child study was to examine the relation between remission or amelioration of maternal depression and children's psychiatric and social functioning (Pilowsky et al., 2006). Weissman, Pilowsky et al. (2006) reported that after 3 months of treatment with citalopram, remission of maternal depression was significantly associated with decreased rates of children's (ages 7-17) psychiatric diagnoses and lower levels of internalizing and externalizing symptoms.
This report seeks to extend these findings by determining whether parenting and family functioning might mediate the relation between remission of maternal depression and children's psychosocial outcomes. Improvements in maternal depression may alter parenting behaviors and parent-child interactions, although few prospective, longitudinal studies are available. In a cross-sectional study, Kaplan, Bachorowski, Smoski, and Zinser (2001) found improvements in the amount of infant-directed speech used by depressed women whose symptoms were either partially or fully remitted following antidepressant treatment. Other studies have examined whether women with a history of depression, who are no longer symptomatic, exhibit parenting behaviors more characteristic of currently depressed or healthy mothers. In these studies, history of depression typically was defined as having at least one past episode of depression, usually within the child's lifetime. Consequently, the timing of mothers' remissions can be quite variable both between and within study samples. Murray and colleagues (2006) reported that history of postpartum depression was not significantly predictive of maternal interactions with children 8 years later. In contrast, women who either were currently depressed or had been depressed in the prior year displayed lower levels of emotional support, higher levels of coercive control, and less support for their child's cognitive development during a homework task. These findings suggest that women with a history of depression, who are not currently symptomatic, may be indistinguishable from their healthy counterparts.
In contrast, several studies have shown that improvement in maternal depression may not impact parent-child interactions or child outcomes. For example, Weinberg and Tronick (1998) found that depressed women whose symptoms improved during treatment continued to behave less positively with their infants compared to healthy controls. Similarly, a study of psychotherapy treatment (nondirective counseling, psychodynamic, or parenting-focused cognitive behavioral therapy) for women with postpartum depression (Murray, Cooper, Wilson, & Romaniuk, 2003) found that despite reductions in depressive symptoms, mothers did not improve their infant behavior management skills and children did not improve in terms of attachment security or cognitive development. Finally, a recent study of interpersonal psychotherapy (Forman et al., 2007) for women with postpartum depression demonstrated that although the therapy was effective at treating depression, it did not impart benefits in terms of children's adjustment or maternal behavior with or perceptions of the infant.
In sum, there is contradictory evidence about whether a reduction of mothers' depressive symptoms or a remission of illness may improve youth outcomes via improvements in family and parental functioning. The vast differences in methodology across studies make comparison of findings difficult. Only two of the aforementioned studies (Forman et al., 2007; Murray et al., 2003) included a longitudinal design. Most studies focused on depression during the postpartum period and the impact of treatment on the mother-infant relationship. In addition, types of treatment varied across studies. Some studies used psychotherapies specifically designed to target parenting (Cooper, Murray, Wilson, & Romaniuk, 2003; Murray et al., 2003), whereas others relied only on antidepressant medications (Kaplan et al., 2001), and a final study used an evidence-based psychotherapy for depression (interpersonal psychotherapy; Forman et al., 2007).
The current study was designed to improve on past work by enrolling a homogenous group of mothers, all of whom were in a current episode of nonpsychotic major depressive disorder and all of whom received identical initial treatment (citalopram). Mothers and children were assessed prospectively to examine the relation of maternal depression remission to the family environment, parenting, and children's adjustment.
We hypothesized that family/parental functioning would mediate the relation between maternal depression remission and youth psychiatric symptoms and psychosocial impairment measured at the 3-month follow-up. The link between remission of maternal depression and improvement in youth outcomes at this time point has been reported previously for this sample (Weissman, Pilowsky, et al., 2006). In accordance with established procedures for testing mediation (Baron & Kenny, 1986), we further hypothesized the following direct relations: (a) Maternal remission would be related to more adaptive levels of family/parental functioning, and (b) positive family/parental functioning would be related to more positive youth outcomes.
METHOD
Participants
Participants were 151 mothers and children who participated in the STAR*D Child study. The STAR*D multisite study (http://www.star-d.org) was designed to compare the effectiveness and acceptability of different treatment options for major depressive disorder (MDD; Rush et al., 2004). Participants in STAR*D were outpatients, ages 18 to 75, with a current diagnosis of nonpsychotic MDD (Trivedi et al., 2006) and without a lifetime diagnosis of bipolar disorder, schizophrenia, or schizoaffective disorder. The rationale, methods, and design of the STAR*D study have been described elsewhere (Fava et al., 2003; Rush et al., 2004; Rush et al., 2006). To summarize, participants in STAR*D were all initially treated with citalopram (Level 1 treatment). Those not experiencing remission and/or those who did not tolerate this initial medication could receive subsequent treatment levels provided in a randomized design. Subsequent treatments included adding or switching medication or cognitive behavioral therapy according to a predetermined sequence while giving patients some choice in the selection of these treatment options.
STAR*D Child participants were recruited from 8 primary care and 11 psychiatric clinics participating in the adult STAR*D study (Weissman, Pilowsky, et al., 2006). Women, 25 to 60 years of age with a biological child between 7 and 17 years were eligible (N=177). The child had to reside with the mother at least 50% of the time. Children with confirmed severe developmental disabilities or psychotic disorders were excluded. Ninety-eight percent of the 177 mother-child pairs met all study-entry criteria. Of these 174 families, 151 (87%) consented to participate in the baseline evaluation, and 114 (75%) completed an evaluation 3 months later. There were no demographic or clinical differences between mothers who dropped out following the baseline evaluation and those who completed the 3-month evaluation (Weissman, Pilowsky, et al., 2006). Families with male children were more likely to drop out prior to the 3-month evaluation. There were no other significant differences among youth completers and noncompleters. Children were not provided with treatment through this study, but those receiving treatment in the community were not excluded. Only 12 children received outpatient treatment during the 3-month time frame described in this study. There was no association between child treatment and remission of maternal depression (Weissman, Pilowsky, et al., 2006). Additional information regarding eligibility and recruitment are described elsewhere (Pilowsky et al., 2006). Table 1 presents demographic information for those families who participated in the 3-month evaluation.
TABLE 1.
Demographic Characteristics of Sample
| n (%) | |
|---|---|
| Child's Age at Baseline | Mean = 11.7 (SD = 2.7) |
| Child Gender | |
| Boys | 53 (46.5) |
| Girls | 61 (53.5) |
| Ethnicity | |
| White | 52 (45.6) |
| Black | 52 (45.6) |
| Hispanic | 18 (15.8) |
| Other | 6 (5.3) |
| Child's Grade at Baseline | |
| Grade 1-6 | 56 (49.1) |
| Grade 7-12 | 58 (50.9) |
| Remedial/Resource Class | 20 (17.5) |
| Mother's Employment Status | |
| Employed Full or Part Time | 73 (64.0) |
| Homemaker | 17 (14.9) |
| Student/Unemployed | 23 (20.2) |
| Household Income | |
| Under $14,999 | 26 (22.8) |
| $15,000-$39,999 | 44 (38.6) |
| $40,000 and above | 38 (33.3) |
| Child Living Situation | |
| Biological Mother Only | 53 (46.5) |
| Both Biological Parents | 43 (37.7) |
| Biological Mother and Stepfather | 18 (15.8) |
Mother-child pairs (N = 114)
Measures
Material depression
Participants in STAR*D received an initial clinical diagnosis of MDD that was confirmed using a checklist interview (Rush et al., 2004) based on the Diagnostic and Statistical Manual of Mental Disorders (4th ed.; American Psychiatric Association, 1994). The 17-item Hamilton Rating Scale for Depression (HRSD17; Hamilton, 1967) was used to assess eligibility and symptom severity. The HRSD17 is the most widely used measure of depressive symptoms in research settings; it has good reliability and is well correlated with other observer-rated instruments (Rush et al., 2003). All women had a raw score of 14 or higher on the HRSD17 at study entry. Remission of maternal depression at the 3-month evaluation was defined using criteria established by the STAR*D study (Trivedi et al., 2006) as an HRSD17 raw score of 7 or lower, which is within the normal range on this measure.
Children's adjustment
The Child Behavior Checklist (CBCL/4-18; Achenbach, 1991) was used to assess internalizing and externalizing symptoms as reported by mothers. The CBCL has strong short-term test-retest reliability and discriminates between clinic- and nonclinic-referred samples of youth (Achenbach, 1991). In this study, coefficient alpha at baseline was .82 for the Internalizing scale and .88 for the Externalizing scale. Mothers completed the CBCL at baseline and the 3-month follow-up. Instructions were altered slightly so that mothers reported only about children's functioning since the baseline evaluation.
The Social Adjustment Inventory for Children and Adolescents (SAICA; John, Gammon, Prusoff, & Warner, 1987) assesses children's social functioning in school (e.g., grades, relationships with teachers and peers, social/behavioral problems), spare-time activities (e.g., hobbies, jobs, television, lack of age-appropriate activities), and peer relationships (popularity, choice of pro-social vs. antisocial peers, peer rejection) using a structured interview with the child as informant. Interrater agreement is high for subscales (King, Segal, Naylor, & Evans, 1993), and the authors report convergent validity with both the CBCL competence scales (.51) and the General Assessment of Functioning (.46-.51; (John et al., 1987). The SAICA was administered at both baseline and 3-month evaluation. Higher scores indicate more impairment. SAICA scales were summed to form one measure of functioning; internal consistency of this summary scale was .84.
Family and parental functioning
The quality of parent-child relationships and the family environment were assessed with two instruments. Children completed the Children's Report of Parenting Behavior Inventory (CRPBI-30: Schludermann & Schludermann, 1970, 1988) at baseline and the 3-month evaluation. The CRPBI measures children's perceptions of their mother's childrearing behaviors. It includes a 10-item Acceptance subscale (“My mother is a person who gives me a lot of care and attention”) and a 9-item Psychological Control subscale (“My mother is a person who always tries to change how I feel or think about things”). Factor structure of the shortened CRPBI is similar to that of the original longer version and supports the presence of the acceptance and psychological control scales (eigenvalues >2.0; Schludermann & Schludermann, 1988). The CRPBI correlates well with other measures of parenting; scores suggesting parenting impairments have been linked to both parental and child psychopathology (e.g., Safford, Alloy, & Pieracci, 2007). Items are scored on a scale from 0 to 2, and subscale scores are calculated using means of component items. Internal consistency in this sample was .81 for Acceptance and .72 for Psychological Control.
The Family Relationship Index (Holahan & Moos, 1982) of the Family Environment Scale (FES; Moos & Moos, 1994) was calculated using the following subscales: Family Cohesion (α=.70), Expressiveness (e.g., open communication; α=.62), and Conflict (α=.71). Construct validity of the Family Relationship Index (FRI) has been supported by studies finding intergenerational continuities in these aspects of family climate (Belsky, Jaffee, Sligo, Woodward, & Silva, 2005) as well as convergent validity with other measures of family social support (Holahan & Moos, 1982). Individual items on the FES are scored either 0 or 1 (true/false), and each scale consists of nine items. Mothers completed the FES at baseline and the 3 month follow-up.
Procedure
Following enrollment and completion of the STAR*D baseline evaluation, women eligible for STAR*D Child were invited to participate. In accordance with each site's Institutional Review Board, maternal consent and child assent were obtained. STAR*D Child baseline assessments were completed by independent evaluators not affiliated with the STAR*D treatment team. Baseline assessments occurred within 2 weeks of the mother's entry into the STAR*D protocol and were timed to occur prior to the onset of any therapeutic benefit of mother's antidepressant medication. Mothers and children were reassessed 3 months after the baseline assessment by an evaluator blind to mother's treatment response.
RESULTS
Descriptive Analyses
Table 2 presents means and standard deviations for study variables at baseline and 3-month follow-up. Table 3 presents correlations among these variables.
TABLE 2.
Family Functioning and Psychosocial Adjustment of Youth Participating in the 3-Month Follow-Up Evaluation
| Baseline |
3 Month |
|||||
|---|---|---|---|---|---|---|
| Measure | All n = 150 M (SD) | Remitted n = 38 M (SD) | Not Remitted n = 76 M (SD) | All 3 Month n = 114 M (SD) | Remitted n = 38 M (SD) | Not Remitted n = 76 M (SD) |
| Family Functioning | ||||||
| FES Family Rel Index | 7.19 (5.03) | 8.08 (4.87) | 6.75 (5.08) | 9.29 (4.48) | 10.88 (4.20) | 8.57 (4.46)* |
| CRPBI Acceptance | 1.60 (.35) | 1.57 (.37) | 1.62 (.34) | 1.62 (.40) | 1.67 (.35) | 1.59 (.42) |
| CRPBI Psych. Control | .56 (.40) | .56 (.41) | .56 (.40) | .54 (.40) | .49 (.47) | .56 (.36) |
| Child Adjustment | ||||||
| CBCL Internalizing | 56.62 (10.34) | 59.34 (9.27) | 55.26 (10.27) | 52.37 (10.54) | 47.68 (7.76) | 54.65 (11.07)* |
| CBCL Externalizing | 54.72 (9.92) | 57.08 (8.85) | 53.54 (10.27) | 51.12 (10.52) | 47.19 (8.26) | 53.07 (11.07)* |
| SAICA Summary Score | 9.99 (1.62) | 9.90 (1.40) | 10.03 (1.73) | 9.68 (1.57) | 9.46 (1.32) | 9.81 (1.68) |
Note. Remitted groups are based on mother's depression measured at 12 weeks. FES = Family Environment Scale; CRPBI = Children's Report of Parenting Behavior Inventory; CBCL = Child Behavior Checklist; SAICA = Social Adjustment Inventory for Children and Adolescents.
Significant difference (p < .05) between the remitted and nonremitted group at 3-month evaluation. There were no group differences at baseline.
TABLE 3.
Correlations Among Measures
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Maternal Remission | - | .13 | -.12 | -.07 | .01 | .13 | .13 | .13 | -.04 | .09 | -.09 | .24* | -.33** | -.27** | -.10 |
| 2. Child Age | - | .08 | -.29** | .16 | .10 | -.05 | -.07 | .01 | -.34** | .02 | .08 | -.12 | -.13 | -.05 | |
| 3. Child Gender | - | -.11 | .03 | -.09 | .07 | .01 | -.02- | .03 | .03 | -.09 | -.13 | -.14 | -.07 | ||
| 4. T1 Maternal Warmth/Acceptance | - | -.46* | .13 | .00 | -.01 | -.26** | .64** | -.38** | .15 | .00 | .02 | -.23* | |||
| 5. T1 Maternal Psychological Control | - | -.04 | -.04 | .02 | .25* | -.26* | .63 | -.03 | .10 | .24* | .27* | ||||
| 6. T1 Family Relations Index | - | -.15 | -.10 | -.10 | .17 | -.04 | .59** | -.17 | .27** | -.20* | |||||
| 7. T1 Internalizing | - | .55** | .01 | .02 | -.02 | -.19* | .23* | .14 | -.01 | ||||||
| 8. T1 Externalizing | - | -.07 | .06 | .09 | -.08 | .07 | .17 | -.02 | |||||||
| 9. T1 SAICA Summary Score | - | -.20* | .28** | -.18 | .19* | .18 | .73* | ||||||||
| 10. 3mo Maternal Warmth/Acceptance | - | -.30** | .24* | -.20* | .07 | -.20* | |||||||||
| 11. 3mo Maternal Psychological Control | - | -.13 | 22* | .29* | .32** | ||||||||||
| 12. 3mo Family Relations Index | - | -.27** | .29** | .18 | |||||||||||
| 13. 3mo Internalizing | - | .50** | .34** | ||||||||||||
| 14. 3mo Externalizing | - | .30** | |||||||||||||
| 15. 3mo SAICA summary score | - |
Note. T1 = baseline evaluation; 3mo = 3-month follow-up; SAICA = Social Adjustment Inventory for Children and Adolescents.
p<.05.
p<.01.
Mothers
Of the 114 mothers who participated in the 3-month evaluation, 38 (33%) met criteria for remission (Weissman, Pilowsky, et al., 2006). Most of the remitting mothers were treated successfully with citalopram only (Level 1 treatment). Three mothers remitted with Level 2 treatments (2 with a switch to extended release venlafaxine-XR and one with a combination of citalopram and buproprion-SR). Baseline characteristics of mothers as a function of remission status are detailed by Weissman, Pilowsky, and colleagues. Briefly, women who remained depressed after 3 months were of lower socioeconomic status, had more severe depressive symptoms at baseline, and were more likely to have concurrent anxiety disorders at baseline. They did not differ from remitting mothers by age of onset of depression, number of previous episodes, or on their children's demographic or clinical characteristics.
Children
At the 3-month-follow-up, children's CBCL T scores ranged from 31 to 80 (M=52.37, SD=10.59) for internalizing symptoms and 32 to 78 (M=51.13, SD=10.56) for externalizing symptoms; 14.9% of youth were in the clinical range (T score >65) for internalizing symptoms and 11.4% for externalizing symptoms.
Mediational Analyses
Relation between remission of maternal depression and youth outcomes
As reported in Weissman, Pilowsky, et al., (2006), remission of maternal depression was related to improvements in youth outcomes. Controlling for child age, gender, baseline maternal depression severity, and baseline levels of child symptoms (Table 4), maternal remission was related to lower levels of both internalizing and externalizing symptoms in youth (β=-.38, p=.000, and β=-.32, p=.001, respectively). This relation was maintained after controlling for demographic variables such as marital status, education, occupation, and race/ethniethnicity. Because these variables did not contribute significantly to the model, they were trimmed from the final analysis. There was no significant relation between mother's remission status and youth psychosocial functioning as measured by the SAICA.
TABLE 4.
Hierarchical Multiple Regression Analyses: Relation Between Remission of Maternal Depression and Youth Internalizing and Externalizing Symptoms
| Dependent Variable |
||||||
|---|---|---|---|---|---|---|
| 3-Month Internalizing Symptoms |
3-Month Externalizing Symptoms |
|||||
| Step and Predictor | Δ in R2 | t | β | Δ in R2 | t | β |
| 1. Control Variables | .09* | .06 | ||||
| Child Age | -1.05 | -.09 | -1.23 | -.12 | ||
| Child Gender | -1.42 | -.13 | -1.42 | -.13 | ||
| Maternal Depression | .59 | .06 | .089 | .01 | ||
| T1 Symptoms | 2.51* | .23 | 1.68 | .16 | ||
| 2. Maternal Remission | .13*** | -4.20*** | -.38 | .09** | -3.35** | -.32 |
| Cumulative R2 | .22 | .15 | ||||
| Final F (4, 107) | 5.83*** | 3.77** | ||||
Note. β = standardized beta coefficients; Maternal Depression = baseline score on Hamilton Depression Rating Scale.
p<.05.
p<.01.
p<.001.
Relation between remission of maternal depression and family/parental functioning
Controlling for child age, gender, baseline maternal depression severity, baseline levels of family/parental functioning, and baseline levels of youth symptoms, remission of maternal depression was significantly related to children's reports of maternal acceptance on the CRPBI (β=.20, p=.007) obtained at the 3-month follow-up (Table 5). That is, remission of maternal depression significantly predicted changes in mothers' expressions of warmth and acceptance as reported by children in the 3 months following the initiation of mothers' antidepressant treatment. Controlling for child age, gender, baseline family relationships, and baseline youth symptoms, there was a significant relation between maternal remission status and scores on the 3-month FRI (β=.18, p=.032). This finding became nonsignificant when family household income was included in the model. Maternal remission status was not related to changes in maternal use of psychologically controlling parenting practices as reported by the child at 3 months.
TABLE 5.
Hierarchical Multiple Regression Analyses: Relation Between Remission of Maternal Depression and Children's Reporting of Parenting
| Dependent Variable |
||||||
|---|---|---|---|---|---|---|
| 3-Month Maternal Acceptance |
3-Month Maternal Control |
|||||
| Step and Predictor | Δ in R2 | t | β | Δ in R2 | t | β |
| 1. Control Variables | .49* | .41*** | ||||
| Child Age | -2.89 | -.21 | -.64 | -.05 | ||
| Child Gender | .39 | .03 | .39 | .03 | ||
| Maternal Depression | 2.34 | .17* | .35 | .03 | ||
| T1 Internalizing | .21* | .02 | -.10 | -.09 | ||
| T1 Externalizing | .41 | .04 | .87 | .08 | ||
| T1 Parenting | 8.11 | .59*** | 8.09 | .63*** | ||
| 2. Maternal Remission | .04** | 2.75** | .20 | .005 | -.94 | -.08 |
| Cumulative R2 | .52*** | .42*** | ||||
| Final F (6, 101) | 15.75*** | 10.15*** | ||||
Note. β = standardized beta coefficients; Maternal Depression = baseline score on Hamilton Depression Rating Scale; T1 Parenting = baseline scores on the dependent variable (Children's Report of Parenting Behavior Inventory Acceptance or Control).
p<.05.
p<.01.
p<.001.
Relation between family/parental functioning and youth outcomes
Controlling for child age, gender, baseline maternal depression severity, baseline levels of maternal acceptance, and baseline levels of child symptoms, maternal acceptance measured at 3-month follow-up was negatively related to youth internalizing symptoms measured at the same time point (β=-.46, p=.000), indicating that changes in maternal warmth and acceptance were significantly associated with changes in children's internalizing symptoms over the 3-month interval.
In addition, change in maternal psychological control measured at the 3-month follow-up was positively related to change in youth internalizing symptoms (β=.27, p=.03), controlling for age, gender, baseline maternal depression severity, and initial levels of psychological control and internalizing symptoms. The relation between maternal psychological control and youth externalizing symptoms at the 3-month assessment (β=22, p=.06) was not significant.
A similar pattern was found for the 3-month FRI. Controlling for child age, gender, baseline maternal depression severity, and baseline levels of symptoms and family relationships, the 3-month FRI was significantly negatively related to youth internalizing symptoms (β=-.27, p=.02). The relation between the FRI and youth externalizing symptoms measured at 3 months (β=-.22, p=.063) was nonsignificant. Thus, change in family relationships over time (i.e., higher cohesion and expressiveness and lower conflict) were significantly related to improvements in youth internalizing problems but not externalizing problems.
None of the family/parental functioning variables measured at the 3-month follow-up were related to youth psychosocial impairment measured by the SAICA. In addition, none of the demographic control variables (i.e., race, maternal education, occupation, marital status, family income) were included in final analyses as they did not contribute significantly to the models.
Mediation
All three paths in the mediational model testing the relations among maternal remission, maternal acceptance, and youth internalizing symptoms were significant. As shown in Table 6, when the hypothesized mediator (child report of maternal acceptance) was added to the regression model examining the relation between maternal remission and youth internalizing symptoms, the magnitude of the relation was reduced from β=-.37, p=.000 to β=-.30, p=.002. Using equations suggested by Sobel (1988) and Holmbeck (2002), a z statistic was computed based on unstandardized beta weights and standard errors; this figure was compared to a table of critical values, which requires a z score to exceed 1.96 for p<.05 significance. The z score was 2.26, indicating that the amount of mediation was significant. Using an equation recommended by MacKinnon and Dwyer (1993), we found that 22.9% of the variance in the relation between remission of maternal depression and internalizing symptoms was accounted for by children's perceptions of their mother as an accepting and warm parent.
TABLE 6.
Hierarchical Multiple Regression Analyses: Parenting as a Potential Mediator of Relation Between Maternal Remission and Youth Outcomes
| Dependent Variable |
||||||
|---|---|---|---|---|---|---|
| 3-Month Internalizing Symptoms |
3-Month Externalizing Symptoms |
|||||
| Step and Predictor | Δ in R2 | t | β | Δ in R2 | t | β |
| 1. Control Variables | .09 | .07 | ||||
| Child Age | -1.11 | -.11 | -1.33 | -.13 | ||
| Child Gender | -1.54 | -.15 | -1.62 | -.16 | ||
| T1 Symptoms | 2.42* | .23* | 1.76 | .17 | ||
| T1 Maternal Acceptance | -.38 | -.04 | -.42 | -.04 | ||
| Maternal Depression | .60 | .06 | .15 | .01 | ||
| 2. Maternal Remission | .13*** | -4.04** | -.37 | .08** | -3.07** | -.30 |
| 3. 3mo Maternal Acceptance | .06** | -2.87** | -.36 | .01 | -.93 | -.13 |
| Cumulative R2 | .28** | .16** | ||||
| Final F (7, 99) | 5.39*** | 2.68* | ||||
Note. β = standardized beta coefficients; Maternal Depression = baseline score on Hamilton Depression Rating Scale.
p<.05.
p<.01.
p<.001.
DISCUSSION
This study investigated parental functioning (maternal acceptance and psychological control) as well as family functioning (family cohesion, positive communication/expressiveness, and family conflict) as possible mediators of the relation between remission of maternal depression and children's psychiatric symptoms. Results showed that improvement of mother's depressive symptoms, even within a short period (3 months), was related to changes in mothers' parenting, which was in turn related to changes in youth internalizing symptoms. This study is one of the first to examine family-level mediators of the relation between remission of maternal depression and youth outcomes in older children and adolescents.
Maternal parenting strategies that included warmth and acceptance of the child partially mediated the relation between remission of maternal depression and youth internalizing symptoms, accounting for almost 23% of the variance. These findings have important clinical significance, as they suggest that short-term treatment with an antidepressant alone, if sufficient to produce maternal remission (as was the case for 33% of mothers in this sample), also may impact mothers' expressions of warmth and acceptance toward their children. These parenting changes are also significantly related to changes in depressive and anxiety symptoms in offspring. The negative impact of maternal depression on parenting has been known for years (Weissman & Paykel, 1974). These data suggest that remission of mothers' depressive symptoms may have potentially far-reaching implications for the families of depressed women.
These findings are consistent with one previous cross-sectional study (Kaplan et al., 2001) of mothers and their infants that found that women who experienced at least partial remission of depressive symptoms following antidepressant treatment evidenced more adaptive mother-infant interactions. In addition, our findings converge with previous studies (e.g., Murray et al., 2006) showing a stronger relation between current compared to prior (i.e., remitted) depressive symptoms and maternal parenting behaviors. Similarly, Ewell Foster, Garber, and Durlak (2008) found that mothers' current depressive symptoms mediated the relation between history of maternal depression and mothers' behaviors in interaction with their early adolescent children. Taken together, these results are encouraging as they imply that some aspects of parenting may improve when depressed mothers get well.
Several other studies (Forman et al., 2007; Murray et al., 2003; Weinberg & Tronick, 1998), however, have failed to show a relation between maternal depression treatment and improvements in parenting and/or child outcomes. These previous studies differed from the current study in several respects. Each study examined parenting in the context of mother-infant relationships, and two of the three studies relied on psychotherapy exclusively, with some therapies focusing more on parenting than on reduction of mothers' symptoms. With so few studies available and such differences in samples and methodology, it is difficult to determine a conclusive reason for the different patterns of results. One possible explanation is that only certain aspects of parenting are impacted by remission of mother's depression. Another possibility is that focusing on parenting without first treating maternal depression is not a useful strategy. It is likely that changing parenting behaviors is harder for a mother who is depressed than for a mother who has recovered from depression.
In this sample, remission of maternal depression was related to changes in accepting/warm/positive parental behaviors from baseline to the 3-month follow-up. For example, children rated their mothers as smiling at them, helping them to feel better when upset, showing love, and praising them. It is important to note that these behaviors were reported not by the mother but by the child, suggesting a large enough change that the children noticed. Furthermore, child reports are not subject to potential reporting biases associated with maternal depression. Maternal depression remission was not associated with changes in mothers' reports about family relationships (family cohesion, expressiveness, and an absence of conflict) or children's ratings of coercive/controlling parenting practices (e.g., My mother tries to change how I feel about things; my mother brings up my past mistakes when she criticizes; my mother would like to tell me what to do all the time) from baseline to the 3-month follow-up. Perhaps these types of parenting strategies are less responsive to maternal mood and may require direct and focused remediation in the form of a parenting intervention. Alternatively, these behaviors may require a longer time to change (i.e., beyond the 3-month interval measured in this study).
Other studies (e.g., Cohen et al., 1999; Cooper et al., 2003) have attempted to address the impact of maternal depression on children by enrolling mother-infant dyads in treatment specifically designed to modify the parenting deficits (i.e., low maternal sensitivity and responsiveness) characteristic of interactions between depressed women and their infants. Antidepressant medication was the sole treatment used in this study, with no effort made to address parenting or family functioning. The STAR*D Study was not designed to be a randomized controlled trial in which mothers were randomized to medication versus another treatment; therefore, we cannot conclude that the remission of depression found in the current study was a result of the medication they received. Nevertheless, our results do provide initial evidence that easily administered, economical, and widely available antidepressant treatment may benefit the families of some depressed women, by altering specific aspects of parenting.
An interesting pattern of results was found when examining relations between family/parental functioning and youth internalizing and externalizing symptoms. In all cases, changes in family/parental functioning (maternal acceptance, psychological control, and family relationships) at 3 months were significantly related to internalizing symptoms, but not externalizing symptoms. Although this finding was unexpected and in need of replication, it suggests that children's externalizing problems may be more related to a long history of parent-child maladaptive interactions, whereas youth internalizing problems may be more responsive to immediate changes in the parenting environment.
We did not find a relation between maternal remission and child report of psychosocial functioning on the SAICA. It may be that in this brief 3-month interval, symptom changes have not yet translated into improvements in youth psychosocial functioning. We expect that over time, functional improvements in school achievement, school behavior, peer relationships, and choices of activities may occur in children whose psychiatric symptoms have improved. Continued monitoring of the STAR*D mother-child dyads will help to elucidate the relation between improvements in symptoms and changes in child functioning.
Limitations
Although this study contributes to the field by incorporating a carefully recruited sample (all women with current nonpsychotic MDD), a controlled intervention (all women initially treated with the same antidepressant), and a longitudinal design that included multiple informants, several important limitations should be noted. First, the primary outcome measure (the CBCL) is based on mother report. When a mother's mood improved, her ratings of her child's symptoms also may have improved whether the child's behavior actually had changed. There is disagreement in the literature regarding whether the reports of depressed women are biased by their negative mood or whether they accurately reflect deficits in their children's behavior (e.g., Najman et al., 2000; Richters, 1992). Although such potential mono-method bias could partially explain the association between changes in mothers' depressive symptoms and changes in children's internalizing and externalizing symptoms, it would not account for the relation of the child-reported parenting variable in the mediation analyses. Mothers' parenting had changed sufficiently so as to be noticed by their children. Moreover, although the outcome variable used in this study (CBCL) was a mother-report instrument, in a previous report (Weissman, Pilowsky, et al., 2006) with this sample, we found change in children's psychiatric status at 3 months using diagnostic interviews that rely on a combination of child, mother, and clinician input and therefore are less subject to maternal depressive bias alone.1 The use of observational measures of parenting and parent-child interactions would have strengthened the assessment of family functioning by providing an independent and richer perspective.
These data are based on reports of parenting and youth outcomes measured 3 months after the initiation of mothers' treatment for depression. Longer term data are needed to investigate whether youth and/or parenting improvements are sustained over time. One recent study (Murray et al., 2003) demonstrated mild improvements in maternal symptoms and perceptions of the mother-infant relationship after 4 months of treatment, but these benefits did not persist. By age 5, children whose depressed mothers had received treatment looked no different than children of depressed mothers who had not received treatment. An additional limitation of this study is the fact that both the mediator (parenting) and the outcome variable (child adjustment) were measured simultaneously. It would have been preferable to establish that parenting changed prior to children's adjustment improving. With the current design, it is possible that an improvement in children's functioning could have caused both increases in maternal warmth and decreases in mothers' depressive symptoms. Although possible, it is unlikely that a group of children who were not undergoing systematic mental health treatment would have improved sufficiently over a 3-month period to cause a remission of depression in their mothers.
Despite the fact that this study is one of the first to examine relations between maternal depression remission, parenting, and outcomes in youth older than infancy/preschool, the wide age range (7-17) among participants may obscure important developmental differences. Finally, generalizability may be limited, because of both attrition of subjects between baseline and 3 month follow-up and the fact that all women participating in this study were seeking treatment for depression. Whether these results apply to community samples is unknown, as it is clear that the majority of women of childbearing age do not seek mental health services for themselves (Kessler et al., 1996).
Implications for Research, Policy, and Practice
As one of the first studies to document parenting changes as a result of maternal depression remission, this study has a number of important implications. Future research should continue to examine the relation between improvement/remission of maternal depression, parenting, and youth adjustment, specifically focusing on the following questions: Is remission required to produce parenting changes, or can changes occur with gradual reductions in symptoms? What specific parenting domains are affected when mothers' depression improves? To what extent does mothers' depression need to be reduced for her to benefit from parenting interventions? Does child age or gender moderate the relation between maternal remission, parenting, and youth adjustment?
Findings also have several important practice and policy implications. Most important is the suggestion that successful treatment of mothers with an antidepressant may result in significant parenting changes, which have implications for reducing children's risk of psychopathology. This suggests the value of mothers' treatment as a prevention strategy for children. In this study, remission of maternal depression resulted in a change in child symptoms equivalent to two thirds of a standard deviation, within 3 months. This study supports the need to reach out to depressed women (who often do not seek their own mental health treatment) through nontraditional mechanisms, such as via proactive voluntary screening in adult and pediatric primary and emergency care centers, specialty care (such as OB-GYN offices), and schools. Further studies are needed to document the potential benefits of these approaches to develop a strong case for improved public and/or third-party payor funding.
FIGURE 1.
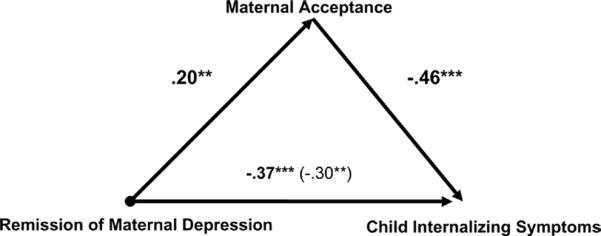
Results of linear regression analyses testing maternal acceptance as a mediator in the relation between maternal depression remission and youth internalizing symptoms. Note. Child age, gender, baseline maternal depression severity, and baseline levels of the dependent variable are controlled in each regression analysis. *p < .05,**p < .01, ***p < .001.
Acknowledgments
This study was supported by NIMH grant # R01MH063852 (M. M. Weissman, PI) and by an NIMH contract (#N01 MH90003) (A. John Rush, PI). Dr. Garber was supported in part by an Independent Scientist Award (K02 MH66249) and Dr. King was supported by an NIMH award (K24 MH077705) during completion of this project.
We are grateful to the seven participating STAR-D Regional Centers: Massachusetts General Hospital, Boston, Primary Investigator: Andrew Nierenberg, M.D.; University of California, San Diego, Primary Investigator: Sid Zisook, M.D.; University of Michigan, Ann Arbor, Primary Investigator: Elizabeth Young, M.D.; University of North Carolina, Chapel Hill, Primary Investigator: Bradley Gaynes, M.D., M.P.H.; University of Texas Southwestern Medical Center, Dallas, Primary Investigator: Mustafa Husain, M.D.; Vanderbilt University, Nashville, TN, Primary Investigator: Steven Hollon, Ph.D.; and Virginia Commonwealth University, Richmond, Co-Principal Investigator: A. Bela Sood, M.D.
Footnotes
Kiddie Schedule for Affective Disorders and Schizophrenia for School-Age Children (KSADS) diagnoses were not included as an outcome measure in this study because continuous variables are needed for linear regression analyses. Moreover, although we considered using child reported KSADS symptom counts as a continuous variable, we elected not to do so, because only data from the screening portion of the KSADS were available.
REFERENCES
- Achenbach T. Manual for the CBCL 4-18, 1991 Profile. Department of Psychiatry, University of Vermont; Burlington: 1991. [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed. Author; Washington, DC: 1994. [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategies, and statistical considerations. Journal of Personality and Social Psychology. 1986;61:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Belsky J, Jaffee SR, Sligo J, Woodward L, Silva P. Intergenerational transmission of warm-sensitive-stimulating parenting: A prospective study of mothers and fathers of 3-year-olds. Child Development. 2005;76:384–396. doi: 10.1111/j.1467-8624.2005.00852.x. [DOI] [PubMed] [Google Scholar]
- Cohen NJ, Muir E, Lojkasek M, Muir R, Parker CJ, Barwick M, et al. Watch, wait and wonder: Testing the effectiveness of a new approach to mother-infant psychotherapy. Infant Mental Health Journal. 1999;20:429–451. [Google Scholar]
- Cooper PJ, Murray L, Wilson A, Romaniuk H. Controlled trial of the short- and long-term effect of psychological treatment of post-partum depression: 1. Impact on maternal mood. British Journal of Psychiatry. 2003;182:412–419. [PubMed] [Google Scholar]
- Cummings EM, Davies PT, Campbell SB. Developmental psychopathology and family process: Theory, research, and clinical implications. Guilford; New York: 2000. [Google Scholar]
- Elkin I, Shea TM, Watkins JT, Imber SD. National Institute of Mental Health treatment of depression collaborative research program: General effectiveness of treatments. Archives of General Psychiatry. 1989;46:971–982. doi: 10.1001/archpsyc.1989.01810110013002. [DOI] [PubMed] [Google Scholar]
- Ewell Foster C, Garber J, Durlak JA. Current and past maternal depression, maternal interaction behaviors, and children's externalizing and internalizing symptoms. Journal of Abnormal Child Psychology. 2008;26:527–537. doi: 10.1007/s10802-007-9197-1. [DOI] [PubMed] [Google Scholar]
- Fava M, Rush AJ, Trivedi MH, Nierenberg AA, Thase ME, Sackeim HA, et al. Background and rationale for the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study. Psychiatric Clinics of North America. 2003;26:457–494. doi: 10.1016/s0193-953x(02)00107-7. [DOI] [PubMed] [Google Scholar]
- Forman DR, O'Hara MW, Stuart S, Gorman LL, Larsen KE, Coy KC. Effective treatment for postpartum depression is not sufficient to improve the developing mother-child relationship. Development and Psychopathology. 2007;19:585–602. doi: 10.1017/S0954579407070289. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Gotlib IH, editors. Children of depressed parents: Mechanisms of risk and implications for treatment. American Psychiatric Association; Washington, DC: 2002. [Google Scholar]
- Hamilton M. Development of a rating scale for primary depressive illness. British Journal of Social and Clinical Psychology. 1967;6:278–296. doi: 10.1111/j.2044-8260.1967.tb00530.x. [DOI] [PubMed] [Google Scholar]
- Holahan CJ, Moos RH. Social support and adjustment: Predictive benefits of social climate indices. American Journal of Community Psychology. 1982;10:403–415. doi: 10.1007/BF00893979. [DOI] [PubMed] [Google Scholar]
- Holmbeck GN. Post-hoc probing of significant moderational and mediational effects in studies of pediatric populations. Journal of Pediatric Psychology. 2002;27:87–96. doi: 10.1093/jpepsy/27.1.87. [DOI] [PubMed] [Google Scholar]
- John K, Gammon GD, Prusoff BA, Warner V. The social adjustment inventory for children and adolescents (SAICA): Testing of a new semi-structured interview. Journal of the American Academy of Child and Adolescent Psychiatry. 1987;26:898–911. doi: 10.1097/00004583-198726060-00015. [DOI] [PubMed] [Google Scholar]
- Kaplan PS, Bachorowski J, Smoski MJ, Zinser M. Role of clinical diagnosis and medication use in effects of maternal depression on infant-directed speech. Infancy. 2001;2:537–548. doi: 10.1207/S15327078IN0204_08. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Nelson CB, McKinagle KA, Edlund MJ, Frank RG, Leaf PJ. The epidemiology of co-occurring addictive and mental disorders: Implications for prevention and service utilization. American Journal of Orthopsychiatry. 1996;66:17–31. doi: 10.1037/h0080151. [DOI] [PubMed] [Google Scholar]
- King C, Segal H, Naylor M, Evans T. Family functioning and suicidal behavior in adolescent inpatients with mood disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 1993;32:1198–1206. doi: 10.1097/00004583-199311000-00013. [DOI] [PubMed] [Google Scholar]
- Lovejoy MC, Graczyk PA, O'Hare E, Neuman G. Maternal depression and parenting: A meta-analytic review. Clinical Psychology Review. 2000;20:561–592. doi: 10.1016/s0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Dwyer JH. Estimating mediated effects in prevention studies. Evaluation Review. 1993;17:141–158. [Google Scholar]
- Moos RH, Moos BS. Family Environment Scale manual. 3rd ed. Consulting Psychologists Press; Palo Alto, CA: 1994. [Google Scholar]
- Munson J, McMahon R, Spieker S. Structure and variability in the developmental trajectory of children's externalizing problems: Impact of infant attachment, maternal depressive symptomatology, and child sex. Development and Psychopathology. 2001;13:277–296. doi: 10.1017/s095457940100205x. [DOI] [PubMed] [Google Scholar]
- Murray L, Cooper PJ, Wilson A, Romaniuk H. Controlled trial of the short- and long-term effect of psychological treatment of post-partum depression: 2. Impact on the mother—child relationship and child outcome. British Journal of Psychiatry. 2003;182:420–427. [PubMed] [Google Scholar]
- Murray L, Woolgar M, Martins C, Christaki A, Hipwell A, Cooper P. Conversations around homework: Links to parental mental health, family characteristics and child psychological functioning. British Journal of Developmental Psychology. 2006;24:125–149. [Google Scholar]
- Najman JM, Williams GM, Nikles J, Spence S, Bor W, O'Callaghan M, et al. Mothers' mental illness and child behavior problems: Cause-effect association or observation bias? Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:592–602. doi: 10.1097/00004583-200005000-00013. [DOI] [PubMed] [Google Scholar]
- Pilowsky DJ, Wickramaratne P, Rush AJ, Hughes CW, Garber J, Malloy E, et al. Children of currently depressed mothers: A STAR* D ancillary study. Journal of Clinical Psychiatry. 2006;67:126–136. doi: 10.4088/jcp.v67n0119. [DOI] [PubMed] [Google Scholar]
- Richters JE. Depressed mothers as informants about their children: A critical review of the evidence for distortion. Psychological Bulletin. 1992;112:485–499. doi: 10.1037/0033-2909.112.3.485. [DOI] [PubMed] [Google Scholar]
- Rush AJ, Fava M, Wisniewski SR, Lavori PW, Trivedi MH, Sackheim HA, et al. Sequenced Treatment Alternatives to Relieve Depression (STAR* D): Rationale and design. Control Clinical Trials. 2004;25:119–142. doi: 10.1016/s0197-2456(03)00112-0. [DOI] [PubMed] [Google Scholar]
- Rush AJ, Trivedi MH, Ibrahim HM, Carmody TJ, Arnow B, Klein DN, et al. The 16- Item Quick Inventory of Depressive Symptomatology (QIDS), Clinician Rating (QIDS-C), and Self-Report (QIDS-SR): A Psychometric Evaluation in Patients with Chronic Major Depression. Biological Psychiatry. 2003;54:573–583. doi: 10.1016/s0006-3223(02)01866-8. [DOI] [PubMed] [Google Scholar]
- Rush AJ, Trivedi MH, Wisniewski SR, Nierenberg AA, Stewart JW, Warden D, et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: A STAR* D report. American Journal of Psychiatry. 2006;163:1905–1917. doi: 10.1176/ajp.2006.163.11.1905. [DOI] [PubMed] [Google Scholar]
- Safford S, Alloy L, Pieracci A. A comparison of two measures of parental behavior. Journal of Child and Family Studies. 2007;16:375–384. [Google Scholar]
- Schludermann EH, Schludermann SM. Replicability of factors in children's report of parent behavior (CRPBI) The Journal of Psychology. 1970;76:239–249. [Google Scholar]
- Schludermann EH, Schludermann SM. Children's Report on Parent Behavior (CRPBI-108, CRPBI-30) for older children and adolescents (Tech. Rep.) University of Manitoba Department of Psychology; Winnipeg, Canada: 1988. [Google Scholar]
- Sobel ME. Direct and indirect effect in linear structural equation models. In: Long JS, editor. Common problems/proper solutions: Avoiding error in quantitative research. Sage; Beverly Hills, CA: 1988. pp. 46–64. [Google Scholar]
- Trivedi MH, Rush JA, Wisniewski SR, Nierenberg A, Warden D, Ritz L, et al. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR* D: Implications for clinical practice. American Journal of Psychiatry. 2006;163:2841. doi: 10.1176/appi.ajp.163.1.28. [DOI] [PubMed] [Google Scholar]
- Weinberg MK, Tronick EZ. The impact of maternal psychiatric illness on infant development. Journal of Clinical Psychiatry. 1998;59:53–61. [PubMed] [Google Scholar]
- Weissman MM, Paykel ES. The depressed woman: A study of social relationships. University of Chicago Press; Chicago: 1974. [Google Scholar]
- Weissman MM, Pilowsky DJ, Wickramaratne PJ, Talati A, Wisniewski SR, Fava M, et al. Remissions in maternal depression and child psychopathology: A STAR* D-child report. Journal of the American Medical Association. 2006;295:1389–1398. doi: 10.1001/jama.295.12.1389. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Wickramaratne P, Nomura Y, Warner V, Pilowsky D, Verdeli H. Offspring of depressed parents: 20 years later. American Journal of Psychiatry. 2006;163:1001–1008. doi: 10.1176/ajp.2006.163.6.1001. [DOI] [PubMed] [Google Scholar]
- Williams JB. A structured interview guide for the Hamilton Depression Rating Scale. Archives of General Psychiatry. 1988;45:742–747. doi: 10.1001/archpsyc.1988.01800320058007. [DOI] [PubMed] [Google Scholar]


