Abstract
Placement of C1 lateral mass screws may be facilitated by intentional C2 root sacrifice. Functional outcomes and morbidity following intentional sacrifice of the C2 root have not been reported in the literature. The objective is to find out if intentional C2 nerve root sacrifice affects functional outcomes and operative morbidity in patients undergoing posterior cervical fusion with C1 lateral mass screws. The study is a case report. Twenty-two consecutive elderly patients (10 males, 12 females with an average age of 77 years) with C1–2 instability were treated with posterior cervical fusion using C1 lateral mass screw placement. Five patients had preservation of the bilateral C2 nerve roots (PRES group) and 18 patients had intentional sacrifice of the bilateral C2 nerve root (SAC group). Operative times, blood loss, hospital length of stay, and complications were recorded for each patient. Functional outcomes, pain, and satisfaction scores were compared between the two groups at the time of ultimate follow-up. Average follow-up time was 19.3 months (range 6–66). The SAC group demonstrated significantly decreased operative time (109.4 vs. 187 min) and a trend towards decreased blood loss (344 vs. 1,030 mL). At ultimate follow-up both groups experienced similar mild disability with no significant difference in NDI scores, analog pain, and satisfaction scores. No patient had C2 root dysesthesia, swallowing, or speech difficulty. In this small case series, intentional sacrifice of the bilateral C2 nerve root ganglion resulted in less operative time and decreased blood loss in elderly patents undergoing C1–2 posterior fusion with the Harms technique. Functional outcome, pain and satisfaction scores were not adversely affected when this technique was used in elderly patients.
Keywords: Posterior cervical fusion, Sacrifice, C2 nerve root, Atlantoaxial, Instability
Introduction
The polyaxial screw-rod technique popularized by Harms and Melcher in 2001 has become the gold standard for atlantoaxial fixation on the basis of decreased risk to the vertebral arteries and superior biomechanical fixation [1, 2]. The technique can be very technically demanding. C1 lateral mass screw placement using the Harms technique is frequently made more difficult by the size and location of the C2 ganglion. Placement of the C1 lateral mass screw requires mobilization and preservation of the C2 ganglion in the original technique as described by Harms. This technique is technically demanding and may lead to prolonged intraoperative time, blood loss, and morbidity in elderly patients who require atlantoaxial stabilization for traumatic instability [1]. To our knowledge, few studies have described C2 nerve root sacrifice with respect to methods of posterior atlantoaxial fixation. None of these studies, however, has reported patient functional outcomes or morbidity specific to the process of sacrificing the C2 nerve root [1, 3].
When placing C1 lateral mass screws, intentional sacrifice of the C2 nerve root affords technical advantages over mobilization and preservation of the nerve root. The operation is made easier by eliminating the primary obstacle to visualization of the C1 lateral mass as well as significantly decreasing troublesome bleeding from the rich vascular plexus surrounding the C2 ganglion. Hemorrhage of the venous plexus during the procedure may significantly hinder visualization and increase the risk to adjacent neurovascular structures [4]. Additionally, by sacrificing the C2 ganglion, the C1–2 articulation and C2 foramen become available for the placement of bone graft to enhance fusion of the motion segment.
The purpose of our study was to examine patient functional outcomes and morbidity in two groups of elderly patients who required operative atlantoaxial posterior stabilization by the same surgeon (RWM) for C1–C2 instability. One group was treated with preservation of the C2 nerve (PRES group) and the other with intentional sacrifice of the bilateral C2 nerve root (SAC group). None of the patients in either group had previous cervical spinal surgery or previously reported traumatic injury to the cervical spine. The rationale for our study was to determine whether intentional C2 nerve root sacrifice would positively or negatively affect patient function outcomes and operative morbidity in elderly patients undergoing posterior cervical fixation for upper cervical instability.
Methods
The design of this study is a case report. During the period from 2003 to 2009, 22 consecutive elderly patients with instability at the C1–2 level were treated by the same well-experienced spine surgeon and senior author (RWM) at a Level One Trauma Center. The average age was 79 years (range 60–90). There were 10 males and 12 females. All patients presented through the emergency department with a history of neck pain following a traumatic episode. Seventeen of 22 patients had an American Spinal Injury Association (ASIA) scores of E (neurologically normal) or D (mild sensory deficit only), two were ASIA C (moderate motor and sensory deficit), and one patient was an ASIA B (profound motor and sensory deficit). Computed tomography in three planes with fine cuts revealed acute, unstable C1–2 pathology in all patients. A displaced type II odontoid fracture was the most frequent underlying cause, and was present in 20 patients. Two patients had an atlantoaxial dislocation.
All patients were treated with a posterior cervical fusion using the Harms and Melcher technique with either: (1) mobilization and preservation of the C2 ganglion (PRES, n = 5) or (2) intentional sacrifice of the C2 nerve root (SAC, n = 18). Patients were positioned using a Mayfield® head holder on a Jackson Table™. Manual reduction was performed in closed fashion and verified using fluoroscopy before prepping the patient. A posterior approach exposing the posterior arch of C1 and C2 was performed using electrocautery after subcutaneous injection of 1:500,000 epinephrine solution in the region of the incision.
Patients were not randomized in this study. Those patients who had preservation of the bilateral C2 nerve roots had relatively smaller C2 ganglia with less perceived obstruction of the bilateral C1 lateral mass screw insertion sites as determined intraoperatively by the senior author. No other patient or radiographic factors were considered in the decision to preserve the C2 nerve roots intraoperatively. In these patients, PRES group, the C2 ganglion was mobilized using subperiosteal dissection with a combination of elevators and bipolar electrocautery (Fig. 1). The C2 nerve root was retracted inferiorly while C1 lateral mass screws were placed using Harms and Melcher technique [5]. SAC patients were perceived intraoperatively to have larger C2 nerve roots that occupied a greater portion of the C1 lateral mass. These patients underwent intentional C2 nerve root sacrifice at the mid-portion of the C2 articulation using monopolar electrocautery after first isolating the ganglion with bipolar electrocautery (Fig. 2). Care was taken to perform the C2 ganglion incision in the midsubstance of the ganglion, located at the midpoint of the exposed C2 lateral mass to prevent a cerebrospinal fluid leak. After the nerve root sacrifice was performed, meticulous hemostasis was achieved using a combination of bipolar electrocautery and Surgifoam (Johnson & Johnson, Sommerville, NJ) with packing. Patients then underwent instrumentation in the same fashion as the PRES group. Fusion was performed with morselized autogenous bone graft in all patients. In the SAC group, abundant graft was placed in the C1–2 articulation and foramen after decortication of the bilateral C1–2 joint surfaces with a high-speed burr (Fig. 3). There were no perceived differences between the PRES and SAC groups with respect to age or preoperative radiographic findings (Table 1).
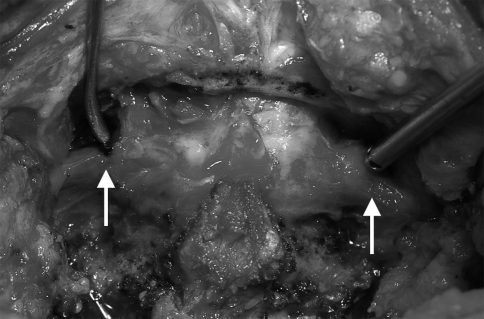
Fig. 1.
Intraoperative photograph demonstrating the mobilization and preservation of the Bilateral C2 nerve roots is shown. Instruments are placed in the approximate location of the C1 screw entry points. Bilateral C2 ganglia are indicated by the arrows
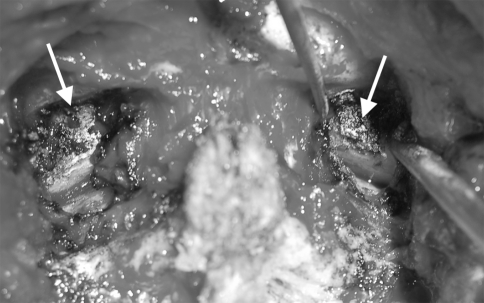
Fig. 2.
Intraoperative image demonstrating bilateral C2 nerve root sacrifice. The C1 lateral masses are well exposed and the C1–2 joint surfaces are well visualized. C1 screw entry points are marked by the arrows
Fig. 3.
Intraoperative photograph of SAC group patient demonstrating abundant bone graft after decortications and bilateral C2 nerve root sacrifice and C1–2 instrumentation
Table 1.
Patient characteristics and surgical results
| Gender | Age | Diagnosis | Follow-up (months) | Estimated blood loss (mL) | Surgical time (min) | Hospital stay (days) | NDI | Pain score | Satisfaction score | |
|---|---|---|---|---|---|---|---|---|---|---|
| Preservation group | ||||||||||
| 1 | M | 89 | Odontoid fracture | 12 | 1,150 | 229 | 3 | 10 | 1 | 9 |
| 2 | F | 73 | Odontoid fracture | 6 | 1,800 | 193 | 4 | 26 | 4 | 8 |
| 3 | F | 69 | C1–2 instability | 66 | 950 | 162 | 5 | 0 | 0 | 10 |
| 4 | F | 67 | Odontoid fracture | 6 | 200 | 150 | 4 | 16 | 1 | 9 |
| 5 | M | 60 | C1–3 instability | 62 | 1,050 | 203 | 9 | 22 | 3 | 7 |
| Average | 71. 6 | 30.4 | 1,030 | 187.4 | 5 | 14.8 | 1.8 | 8.6 | ||
| Sacrifice group | ||||||||||
| 1 | F | 85 | Odontoid fracture | 52 | 300 | 120 | 4 | 32 | 1 | 10 |
| 2 | F | 79 | Odontoid fracture | 48 | 300 | 227 | 6 | 4 | 0 | 10 |
| 3 | M | 90 | Odontoid fracture | 19 | 300 | 108 | 10 | 2 | 9 | |
| 4 | M | 81 | Odontoid fracture | 29 | 550 | 180 | 13 | 0 | 0 | 10 |
| 5 | M | 88 | Odontoid fracture | 700 | 163 | 8 | –a | |||
| 6 | F | 81 | Odontoid fracture | 18 | 100 | 123 | 20 | 12 | 1 | 9 |
| 7 | F | 85 | Odontoid fracture | 400 | 91 | 11 | –a | |||
| 8 | F | 72 | Odontoid fracture | 18 | 500 | 85 | 4 | 12 | 1 | 10 |
| 9 | F | 61 | Odontoid fracture | 18 | 750 | 106 | 3 | 42 | 7 | 7 |
| 10 | M | 74 | Odontoid fracture | 350 | 119 | 5 | –a | |||
| 11 | M | 78 | Odontoid fracture | 6 | 200 | 96 | 10 | 0 | 0 | 10 |
| 12 | F | 79 | Odontoid fracture | 200 | 92 | 3 | –a | |||
| 13 | M | 63 | Odontoid fracture | 6 | 50 | 92 | 4 | 24 | 7 | 6 |
| 14 | F | 82 | Odontoid fracture | 6 | 150 | 95 | 4 | 34 | 3 | 8 |
| 15 | M | 87 | Odontoid fracture | 6 | 150 | 90 | 4 | 40 | 0 | 10 |
| 16 | F | 73 | Odontoid fracture | 6 | 150 | 90 | 4 | 28 | 3 | 10 |
| 17 | M | 81 | Odontoid fracture | 16 | 700 | 110 | 4 | 20 | 3 | 9 |
| 18 | F | 79 | Odontoid fracture | 22 | 350 | 105 | 7 | 19 | 3 | 9 |
| Average | 78.8 | 19.3 | 344.1 | 116.2 | 6.9 | 20.6 | 2.2 | 9.1 | ||
aPatients lost to follow-up
Postoperative bracing used in both groups consisted of a Miami J® collar for comfort only and patients received physical therapy while in the hospital for purposes of mobilization and clearance to return to home. Those patients who were too debilitated to return home were referred to an extended care facility upon discharge.
Hospital medical record review was performed for each patient to determine operating times, estimated blood loss, length of hospital stay and peri-operative complications for each patient. The exact Wilcoxon rank-sum test was used evaluate differences between the groups. At the time of ultimate follow-up, all patients completed functional outcome assessment consisting of neck disability index (NDI) questionnaire, analog pain, and satisfaction scores. The NDI is a standardized, validated questionnaire consisting of ten scaled questions used to assess self-rated disability in patients with neck pain. This disability index has been validated in the elderly population [6]. The NDI is scored using a point scale that ranges from 0 to 50. Each patient’s raw score is doubled to achieve a percent score. Using this scoring system, a score of 10–28% (or 5–14 points) is considered to constitute mild disability; 30–48% is moderate; 50–68% is severe; and >72% is complete disability [7, 8]. Additionally, at the time of ultimate follow-up, patients were questioned regarding dysesthesias, numbness, swallowing, or speech problems related to C2 root anatomy and function. A physical examination was performed including pinprick and light touch stimuli to assess for objective sensory function in the region of the C2 roots bilaterally.
Institutional Review Board approval was obtained for the study, and the data were collected and assimilated in a retrospective manner.
Results
Follow-up was available for all five patients in the PRES group. The SAC group had complete follow-up for 14 of 18 patients. One patient could not be located and was considered lost to follow-up, and three other elderly patients died from unrelated medical causes. Follow-up ranged from 6 to 66 months and averaged 19.3 months (Table 1).
Operative time
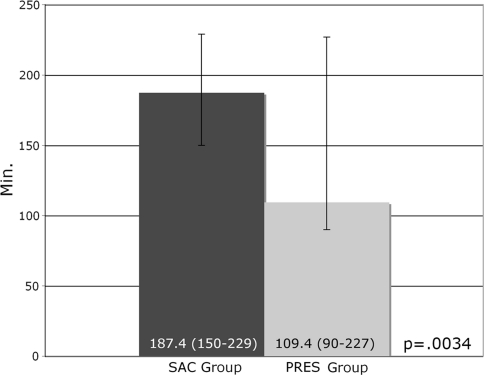
A significant difference between the PRES and SAC groups was noted with respect to operative time. The PRES group had an average of 187.4 min (150–229). The SAC group had an average operative time of 109.4 min (90–227) (p = 0.0034) (Fig. 4).
Fig. 4.
Average operative time is reduced from 187.4 to 109.4 min in the SAC group (p = 0.0034)
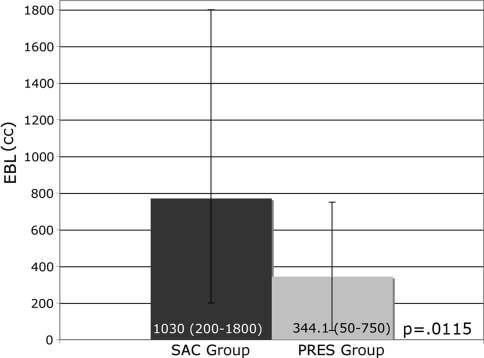
Average EBL
There was a trend towards increased blood loss in the PRES group. The average EBL for the PRES group was 1,030 mL (200–1,800). The SAC group had an average EBL of 344 mL (50–750) (p = 0.0115) (Fig. 5).
Fig. 5.
EBL is reduced from 1,030 to 344 mL in the SAC group (p = 0.0115)
Hospital stay length
The average hospital length of stay was 5 days (3–9) in the PRES group and 6.9 days (3–20) in SAC group (p = 0.4449). Length of stay for patients without significant medical comorbidities or other traumatic injuries was 4 days or less for the majority of patients (PRES group = 60%, SAC group = 52%).
Functional outcomes: neck disability index
The NDI is a validated outcome measure with a minimum score of 0 and a maximum score of 100. There are ten questions that receive each a raw point score of 0–5. The sum of all sections is doubled to achieve a percentage score. A percentage score of 10–28% indicates mild disability, 30–48% is moderate, 50–68% is more severe, and ≥72% indicates complete disability. The average NDI score of patients from the PRES group was 14.8 (0–26). The SAC group had an average NDI of 20.7 (24–34). The NDI for both groups indicated mild disability at ultimate follow-up. There was not a statistical difference between the two groups (p = 0.4293).
Analog pain
Pain was graded on an 11-point analog scale, with 0 indicating no pain and 10 representing the worst pain possible. The PRES group averaged 1.8 (0–4). The SAC group averaged 2.1 (0–7) (p = 1).
Satisfaction scores
Satisfaction was graded on an 11-point analog scale, with 0 indicating completely satisfied and 10 complete dissatisfaction. Satisfaction scores averaged 8.6 (7–10) in the PRES group. The SAC group reported an average satisfaction score of 9.1 (6–10) (p = 0.3321).
Complications
There were no complications in the PRES group and two complications in the SAC group. The first was a cerebral spinal fluid leak that occurred early in the series when the C2 nerve root was sacrificed medial to the ganglion. This was repaired primarily and the patient did not experience any postoperative morbidity. The second complication was a broken C2 pedicle screw that was seen during routine follow-up on X-ray (Fig. 6). The instrumentation failure was asymptomatic and did not result in any instability. No patient in either group demonstrated C1–2 instability at ultimate follow-up.
Fig. 6.
Four-year follow-up hyperextension radiograph demonstrating a single broken C2 pedicle screw and stable C1–2 segment
Physical examination with pin prick and light touch stimuli at the time of ultimate follow-up revealed the absence of sensation to both stimuli in the posterior occipital C2 dermatomal region bilaterally in all 14 patients SAC group patients. All 14 patients also reported that they subjectively experienced numbness in the posterior head region corresponding to the bilateral C2 dermatomal distribution. 13 of the 14 SAC patients (93%) reported that they were not significantly bothered by the posterior head numbness and that it was not considered to be a bothering problem for them. 5 of the 14 SAC patients (36%) were initially unaware of the posterior head numbness until it was demonstrated to them during their postoperative physical examination. One patient in the SAC group (7%) reported being bothered by not feeling the sensation of his pillow while lying awake in bed. No patient in either group experienced postoperative dysesthesias in the region of the C2 dermatome or reported being affected by pain in the same posterior head region. Additionally, no patient in either group reported problems with swallowing or speech.
Discussion
While the Harms and Melcher technique has several advantages over other techniques it can be very technically demanding because of the typically large size of the C2 ganglion, which can completely block access to the C1 lateral mass in some patients resulting in excessive blood loss and increased C2 root manipulation [4]. Mobilization of the C2 roots and proper visualization of the starting point for C1 lateral mass screw placement can be difficult even for the most experienced surgeons during these cases.
Some authors have described alternative methods of C1 lateral mass fixation or a modification of the Harms and Melcher technique, and others have reported in their methods that the C2 nerve root was routinely sacrificed [1, 3, 4, 9]. Unfortunately, none of these authors reported the functional outcomes and patient morbidity related to the process of sacrificing the C2 roots. Goel et al. described posterior atlantoaxial plate fixation in 160 patients using a technique that required sectioning of the C2 nerve roots [10]. The authors in this study did not comment on the extent of patient disability related to C2 root sacrifice with this novel fixation technique. Aryan et al. [1] reported the largest series consisting of 102 patients with and average age of 62 years who had bilateral C2 root sacrifice for C1–2 fixation in a multicenter, multisurgeon study. The authors reported no incidence of cerebrospinal fluid leakage with sacrifice and only one patient had C2 neuropathic pain postoperatively. The authors concluded that routinely sacrificing the C2 roots is still controversial, but it may facilitate C1 screw placement and it does not increase the risk of complications. The study’s methodology is somewhat flawed by the lack of use of a patient functional outcomes instrument and the lack of inclusion of any intraoperative data to evaluate operative blood loss, operative times, and hospital stay with regard to complications or proposed benefits associated with intentional C2 nerve root sacrifice.
To our knowledge the functional outcomes and operative morbidity specifically related to the intentional sacrifice of the bilateral C2 nerve roots during C1 lateral mass screw placement in elderly patients has never been reported The data from our study does suggest decreased operative morbidity in the form of less blood loss, less operative time, and no resultant increase in operative complications in these elderly patients in whom expeditious fixation surgery is warranted. Our outcomes data also suggests that intentional bilateral C2 nerve root sacrifice in elderly patients does not adversely affect their functional outcomes.
Intentional C2 root sacrifice is still not without controversy. Surgeons who choose to sacrifice the C2 roots during spinal procedures must be fully aware of the C2 root anatomy and function. The C2 nerve root gives rise to the dorsal and ventral rami. The ventral rami of the C2 with C3, C4, and occasionally C1, form the cervical plexus. The fibers of C2 also contribute to the hypoglossal nerve. It is these fibers with those of C1 that form the superior root of the ansa cervicalis innervating the nerve to the thyrohyoid muscle and the nerve to the geniohyoid muscle. The superior root of the ansa cervical gives branches to the superior belly of the omohyoid muscle, and the upper parts of the sternothyroid and sternohyoid muscles. The second cervical root sends another branch containing afferent fibers to the spinal accessory nerve to be distributed to the sternocleidomastoid and/or trapezius [11]. The second cervical nerve combines with the third to form the inferior loop of the ansa cervicalis. This is responsible for branches to the inferior belly of the omohyoid muscle, and the lower parts of the sternothyroid and sternohyoid muscles [11].
The involvement of the motor branches is often unapparent with C2 nerve root sacrifice [11]. Not only do the partially denervated muscles receive multiple innervations from other roots but their dysfunction may be concealed by the actions of nearby, uninvolved muscles [12]. The lack of significant complications associated with intentional bilateral C2 root sacrifice was demonstrated in our study as the functional outcomes of patients with C2 nerve root sacrifice did not have any significant difference compared to those with preservation of the nerve and patients had no observable motor deficits. All patients were specifically questioned regarding speech and swallowing problems and no patient with C2 nerve sacrifice reported any postoperative changes.
Cutaneous branches from the C2 nerve root include the lesser occipital nerve, which is a direct branch off of the ventral ramus of C2. The remaining part of this stem combines with afferents of C3 to form the transversecervical and great auricular nerves. The greater occipital nerve is a direct branch of the dorsal ramus of C2. It may also receive contributions from the lesser occipital nerve. This nerve branches to the occipital bone and scalp providing cutaneous sensation to the medial posterior neck and scalp up to the coronal suture and laterally to the mastoid.
The primary side effect of sacrificing the C2 nerve root is hypesthesia in the posterior occipital region. The greater occipital nerve is a direct branch of the dorsal ramus, and the lesser occipital nerve is a direct branch of C2 off the cervical plexus. These nerves are the only two nerves that receive afferents solely from C2. Hypesthesias were expected and patients were counseled preoperatively regarding this. Previous studies of C2 ganglionectomy for occipital headache have reported infrequent complaints of dysesthesias developing postoperatively [2, 13]. Additionally, preservation of the C2 nerve root does not guarantee absence of dysesthesias or occipital neuralgia from nerve root irritation [14, 15]. This has been reported previously with preservation of the C2 nerve. Arthrosis of the C1–2 joint, mechanical compression of the ganglion by C1 lateral mass screws, or vascular engorgement can all lead to occipital neuralgia by compression of the ganglion.
While our study did not show a significant difference in operative blood loss between the two groups, there was a strong trend. Decreased blood loss is an important consideration in the elderly as many patients have significant medical comorbidities. Decreasing blood loss can have a large effect on transfusion requirements, which is important as red blood cell transfusion has been linked to increased postoperative morbidity and mortality. RBC transfusion increases the risk of serious wound and systemic infections, renal failure, prolonged ventilation, myocardial infarction and stroke and lymphoma [16, 17]. This is in addition to the known risks of infectious disease transmission. Higher postoperative hemoglobin has also been shown to decrease length of stay and readmission rates [10].
The limitations of our study include the retrospective nature and the relatively small sample size. C1–2 instability in the elderly population requiring definitive surgical treatment by the same surgeon typically does not result in large numbers of study patients. Our consecutive series treated by the same surgeon spans 6 years at a busy level-1 trauma center. Another weakness of the study exists in the nonrandomization of patients and the arbitrary selection of the comparison group of five patients whom had preservation of the C2 roots based on the perceived smaller C2 root size with less obstruction of the C1 lateral mass screw insertion site. The study data for this comparison group of patients do suggest higher blood loss and longer operative times even when the C2 nerve roots are perceived to be relatively smaller in size and the surgery is performed by an experienced spinal surgeon. It is possible that spinal surgeons may encounter greater blood loss and longer operative times when the C2 roots are preserved in patients with larger C2 nerve root size and increased obstruction of the C1 lateral mass region. A larger randomized, controlled trial is still needed to demonstrate this in a more accurate manner. The results of this small case series do suggest, however, that there is low operative time and morbidity, infrequent complications, and good pain and satisfaction scores associated with intentional C2 nerve root sacrifice.
Conclusion
In this small case series, intentional sacrifice of the bilateral C2 nerve root ganglion resulted in less operative time and decreased blood loss in elderly patents undergoing C1–2 posterior fusion with the Harms technique. Functional outcome, pain and satisfaction scores were not adversely affected when this technique was used in elderly patients.
Acknowledgments
The authors wish to thank Kimberly Napoli for editorial assistance in preparing this manuscript.
References
- 1.Aryan HE, Newman CB, Nottmeier EW, Acosta FL, Jr, Wang VY, Ames CP. Stabilization of the atlantoaxial complex via C-1 lateral mass and C-2 pedicle screw fixation in a multicenter clinical experience in 102 patients: modification of the Harms and Goel techniques. J Neurosurg Spine. 2008;8:222–229. doi: 10.3171/SPI/2008/8/3/222. [DOI] [PubMed] [Google Scholar]
- 2.Lozano AM, Vanderlinden G, Bachoo R, Rothbart P. Microsurgical C-2 ganglionectomy for chronic intractable occipital pain. J Neurosurg. 1998;89:359–365. doi: 10.3171/jns.1998.89.3.0359. [DOI] [PubMed] [Google Scholar]
- 3.Goel A, Desai KI, Muzumdar DP. Atlantoaxial fixation using plate and screw method: a report of 160 treated patients. Neurosurgery. 2002;51:1351–1356. doi: 10.1097/00006123-200212000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Rocha R, Safavi-Abbasi S, Reis C, Theodore N, Bambakidis N, Oliveira E, Sonntag VK, Crawford NR. Working area, safety zones, and angles of approach for posterior C-1 lateral mass screw placement: a quantitative anatomical and morphometric evaluation. J Neurosurg Spine. 2007;6:247–254. doi: 10.3171/spi.2007.6.3.247. [DOI] [PubMed] [Google Scholar]
- 5.Harms J, Melcher RP. Posterior C1–C2 fusion with polyaxial screw and rod fixation. Spine (Phila Pa 1976) 2001;26:2467–2471. doi: 10.1097/00007632-200111150-00014. [DOI] [PubMed] [Google Scholar]
- 6.En MC, Clair DA, Edmondston SJ. Validity of the neck disability index and neck pain and disability scale for measuring disability associated with chronic, non-traumatic neck pain. Man Ther. 2009;14:433–438. doi: 10.1016/j.math.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 7.Vernon H. The neck disability index: state-of-the-art, 1991–2008. J Manip Physiol Ther. 2008;31:491–502. doi: 10.1016/j.jmpt.2008.08.006. [DOI] [PubMed] [Google Scholar]
- 8.McCarthy MJ, Grevitt MP, Silcocks P, Hobbs G. The reliability of the Vernon and Mior neck disability index, and its validity compared with the short form-36 health survey questionnaire. Eur Spine J. 2007;16:2111–2117. doi: 10.1007/s00586-007-0503-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tan M, Wang H, Wang Y, Zhang G, Yi P, Li Z, Wei H, Yang F. Morphometric evaluation of screw fixation in atlas via posterior arch and lateral mass. Spine (Phila Pa 1976) 2003;28:888–895. doi: 10.1097/01.BRS.0000058719.48596.CC. [DOI] [PubMed] [Google Scholar]
- 10.Halm EA, Wang JJ, Boockvar K, Penrod J, Silberzweig SB, Magaziner J, Koval KJ, Siu AL. The effect of perioperative anemia on clinical and functional outcomes in patients with hip fracture. J Orthop Trauma. 2004;18:369–374. doi: 10.1097/00005131-200407000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rosse C, Gaddum-Rose P. The neck. Philadelphia: Hollinshead; 1997. [Google Scholar]
- 12.Wilbourn AJ. Plexopathies. Neurol Clin. 2007;25:139–171. doi: 10.1016/j.ncl.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 13.Acar F, Miller J, Golshani KJ, Israel ZH, McCartney S, Burchiel KJ. Pain relief after cervical ganglionectomy (C2 and C3) for the treatment of medically intractable occipital neuralgia. Stereotact Funct Neurosurg. 2008;86:106–112. doi: 10.1159/000113872. [DOI] [PubMed] [Google Scholar]
- 14.Wang MY, Levi ADO. Ganglionectomy of C-2 for the treatment of medically refractory occipital neuralgia. Neurosurg Focus. 2002;12:3. doi: 10.3171/foc.2002.12.1.15. [DOI] [PubMed] [Google Scholar]
- 15.Rhee WT, You SH, Kim SK, Lee SY. Troublesome occipital neuralgia developed by C1–2 Harms Construct. J Korean Neurosurg Soc. 2008;43:3. doi: 10.3340/jkns.2008.43.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pearson J, Sculco T, Spence R, Keating E (2007) Blood products: maximal use, conservation, pre deposit blood, when to transfuse and erythropoietin. In: Instructional course lecture. AAOS, New Orleans
- 17.Reeves BC, Murphy GJ. Increased mortality, morbidity, and cost associated with red blood cell transfusion after cardiac surgery. Curr Opin Anaesthesiol. 2008;21:669–673. doi: 10.1097/ACO.0b013e32830dd087. [DOI] [PubMed] [Google Scholar]