Abstract
Opinions have varied regarding the optimal treatment of an unstable Hangman’s fracture. C2 pedicle screw instrumentation is a biomechanically strong fixation which although done through a simple posterior approach, is a technically demanding procedure. This prospective, non-randomized multicentre study included 15 consecutive patients with displaced type II traumatic spondylolisthesis of the axis. There were nine males and six females with a mean age of 37 years at surgery. The cause of injury was a road traffic accident in 11 patients and a fall from height in 4 patients. All patients had a single stage reduction and direct transpedicular screw fixation through the C2 pedicles. During follow-up, clinical evaluation and plain X-rays were performed at each visit; at 6-month follow-up, additional dynamic lateral flexion/extension views and a CT scan were performed. The average follow-up period was 32 months (range 25–56 months). At final follow-up, all patients were asymptomatic and regained a good functional outcome with no limitation of range of motion; all the patients showed solid union with no implant failure. There were no neurological complications. At 6-month follow-up, CT evaluation showed fusion in all patients and an adequate position of 28 screws. Two pedicle screws (6.6%) showed minimal (defined as <2 mm) intrusion; one into the spinal canal and the other into the vertebral foreamen. Transpedicular screw fixation through the C2 pedicles is a safe and effective method in treating type II traumatic spondylolisthesis of the axis resulting in good clinical and radiological outcomes. Adequate reduction was achieved and motion segments were preserved with its use.
Keywords: Hangman’s fracture, Transpedicular screw, Motion preservation, Cervical spine
Introduction
Traumatic spondylolisthesis of the axis (TSA) is the second most common fracture of the second cervical vertebra (C2) and accounts for 4–20% of all cervical spine injuries [1, 2]. It involves a bilateral fracture of the C2 pars interarticularis with variable displacement of C2 on C3. In 1965, Schneider et al. [3] coined the term “Hangman’s” fracture to describe this injury based on its superficial similarity to the injury seen after judicial hanging caused by severe hyperextension and distraction [4].
On the contrary, TSA was considered to be a flexion injury because of the forward displacement of the second cervical vertebra [5]; others have considered it to be primarily a hyperextension-axial loading injury [6–8].
The fracture is usually classified according to the method of Effendi et al. [9] and its modification by Levine and Edwards [10]. Effendi Type II fractures show significant angulation and translation and are considered to be unstable injuries. Levine and Edwards described a modification (Type IIA) consisting of slight or no displacement, but severe angulation due to severe circumferential discoligamentous injury [10].
Opinions have varied regarding the optimal treatment of Hangman’s fractures; some recommended use of the halo vest [6–8] while others considered this to be a grossly unstable fracture and recommended surgical stabi1ization [11]. In 1964, Leconte [12] described a C2 direct transpedicular fixation technique which was further illustrated by Judet et al. [13].
The aim of this study is to evaluate the results of C2 transpedicular fixation in Type II TSA including clinical outcome, X-ray and CT evaluation of fracture reduction, union and accuracy of screw placement.
Patients and methods
This multicentre study, approved by the Institutional Review Board and the Ethics Committee, included 15 patients with “Hangman’s” fracture who gave their informed consent to be incorporated in this research. It consisted of a prospectively collected consecutive series of 15 patients with displaced Type II TSA treated between 2000 and 2007.
The study included nine males and six females with a mean age of 37 years (range 22–61 years) at surgery. The cause of injury was a road traffic accident in 11 patients (73%) and fall from a height in 4 patients (27%). Other injuries included pelvic fractures (2 patients), head injuries (3 patients) and fracture of extremities (4 patients). All patients had neck pain and restricted motion of the cervical spine. Patients had a complete neurological evaluation on admission and were preoperatively neurologically free.
The radiographic assessment included preoperative standard anteroposterior, lateral and open-mouth views of the cervical spine with the patient in the supine position and a computerized tomography (CT) scan. Magnetic resonance imaging (MRI) was performed in five patients to exclude spinal cord compression and evaluate the integrity of the C2/3 intervertebral disc. Fractures were classified according to the Levine–Edwards [10] classification; 12 patients were Type II and 3 were Type IIA. Thirteen patients had bilateral symmetric isthmus fractures and only two patients had fractures involving the vertebral body.
Surgical technique
All patients underwent transpedicular screw fixation through the C2 pedicles. Patients were position-prone immobilized in a hard collar, which was removed after the application of cervical tongs using a 3 kg weight. Under image control, initial reduction was achieved by placing the head in a slightly flexed position and applying gentle traction until alignment was achieved (Fig. 1a); the head was then gently extended to neutral position to close the remaining gap (Fig. 1b). The skin incision extended from the external occipital protuberance along the midline to the level of C5/6 cervical vertebrae. The septum nuchae was split along the midline. The muscles were then freed from the occipital bone and posterior arches of Cl, C2 and C3. Extreme care was taken to avoid injury of the C2/3 facet capsule during dissection and injury of the vertebral artery at the upper border of C1 by avoiding dissection more than 1.5 cm from the middle line at the posterior elements of the atlas.
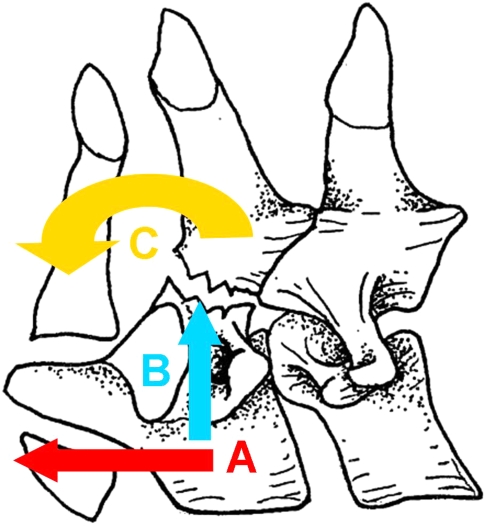
Fig. 1.
Diagram revealing sequential forces used to reduce the fracture. (A) Traction until fracture alignment is achieved, (B) extension to neutral position to close the fracture gap, (C) manipulation of the spinous process of C2 to completely close any remaining gap
At the level of C2, the lateral margins of the inferior articular processes were exposed bilaterally in order to precisely locate the point of entry of the screw on the posterior surface of inferior articular process of C2. The pedicle was recognized after detaching the atlantoaxial ligament. Its superomedial aspect was identified using a dissector carefully placed at the superior border of the lamina of C2. The fracture site was often felt at this stage. If reduction was not completely achieved by positioning of the patient, manipulation at the fracture level helped achieving complete reduction by applying more traction in the neutral position and gentle manipulation of the spinous process of C2 for complete closure of the remaining gap (Fig. 1c). Extension of the cervical spine hinders reduction and was thus avoided. Reduction must be performed before drilling the screws (Fig. 2a).
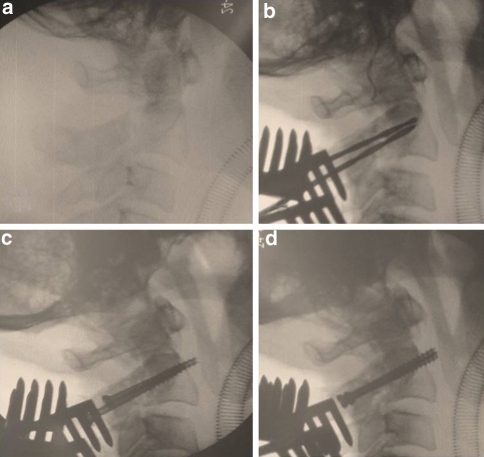
Fig. 2.
Intraoperative images revealing a adequate reduction through patient positioning and gentle manipulation, b drilling towards the C2 vertebral body, c tightening of the screws allowed for adequate compression across the fracture site, d the final reduction and position of the screws
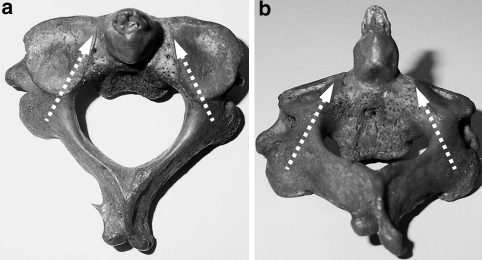
An assistant maintained a fine dissector in position at the inner aspect of the pedicle; this not only allowed for direct vision, but also helped to protect the spinal cord while drilling the holes. The drilling proceeded towards the C2 vertebral body keeping an inclination of approximately 20° inwards and upwards in the axial and sagittal planes, respectively (Fig. 3a, b). Drilling was performed using two successive drill bits of different diameters to achieve a lag effect. The first drill bit had a diameter of 2 mm and was fitted with a stopper to limit the drilling depth to 30 mm. The drill hole passed through the posterior part of the pedicle, fracture site and true pedicle, anteriorly stopping within the C2 vertebral body. The second drill bit had a diameter of 2.7 mm and was inserted through the previous hole only up to the fracture site. Drill holes were performed bilaterally before any screw placement was attempted (Fig. 2b). The reduction and drill holes were checked using an image intensifier.
Fig. 3.
Image revealing ideal screw position in a axial and b sagittal planes
A standard AO 3.5 mm cortical screw or 4.00 mm cancellous screw was placed on either side; the 2 screws were inserted simultaneously pulling, in an equal manner, the C2 vertebral body towards the fractured pedicles and final tightening of the screws allowed adequate compression across the fracture site (Fig. 2c). The final reduction and position of the screws were confirmed via image intensification (Fig. 2d).
Closure of the wound was performed in layers with the routine use of a suction drain which was removed at 48 h. All patients had prophylactic antibiotic coverage for 1 week and were placed in a Philadelphia cervical collar for 8–10 weeks and then gradually weaned off it over another 4 weeks.
Follow-up
Patients were followed for an average of 32 months (range 25–56 months). All patients were viewed at 6 weeks, 12 weeks, 36 weeks and 1 year postoperatively and were later followed up at yearly intervals. Clinical evaluation and plain X-rays were performed at each visit; at 6-month follow-up, additional dynamic lateral flexion/extension views and a CT scan were performed.
Results
The operative data, clinical and radiological results were evaluated; complications of the surgical procedure were reported.
Operative notes
The average total operative time was 95 min (range 85–140 min) while blood loss was 300 cc (range 175–1,250 cc). The average hospital stay was 6 days (range 4–18 days).
Clinical evaluation
At final follow-up, a standard Visual Analogue Scale (VAS) of 10 points was used to assess neck pain and had an average score of 1 (range 0–2). Range of motion was examined as patients were asked to first hold their head in a neutral position and then to turn their head to the maximum right, left and forward bending position. All patients regained an excellent functional outcome with no limitation of the range of motion; flexion 46.1° ± 2.2°, extension 55.4° ± 1.9°, right rotation 74.6° ± 2.8°, left rotation 75.8° ± 1.7°.
Radiological evaluation
An independent expert radiologist evaluated the plain X-rays and CT scans of all the patients.
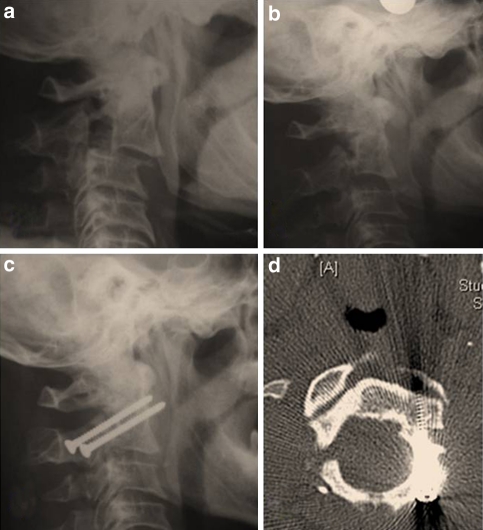
Anterior translation was measured as the distance between lines drawn parallel to the posterior borders of the bodies of C2 and C3. A significant reduction was achieved when comparing pre to postoperative films (Fig. 4) from an average of 6 mm to 1.5 mm, which was maintained at the final follow-up (P < 0.001).
Fig. 4.
A 59-year-old male patient a pre-op lat X-ray, b intra-op Lat X-ray following reduction maneuvers, c post-op lat X-ray and d follow-up CT showing solid union and accurate screw placement
A solid union was considered to be present when there was evidence of healing across the fracture site, no metal failure and no evidence of instability on dynamic views. All patients showed solid union with no migration or breakage of the screws at the latest follow-up. Standard AO 3.5 mm cortical screws were used in 10 patients while 4.00 mm cancellous screws were used in 5 patients with no difference in clinical or radiological outcome. No ossification of C2/3 disc was observed during the follow-up period and flexion–extension views, the range of motion at C2–3 was 4.7° ± 2.9°.
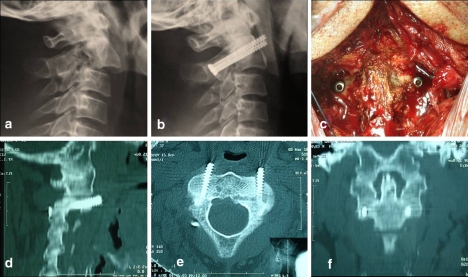
At 6-month follow-up, CT evaluation showed fusion in all patients and an adequate position of 28 screws (Fig. 5). Two pedicle screws (6.6%) showed minimal (defined as <2 mm) intrusion; one into the spinal canal and the other into the vertebral foreamen.
Fig. 5.
A 35-year-old male patient a, b pre-op and follow-up lat X-rays showing adequate fracture reduction; c intra-op photograph and d, e, f follow-up CT with sagittal, axial and coronal reconstruction showing solid fusion and adequate screw placement
Complications
There were no neurological complications or dural tears.
One patient had severe bleeding during the drilling of one of the screws which was presumed to be due to a vertebral artery/vein injury. This was promptly controlled by the application of screw. Postoperatively the patient had no neurological deficit—was asymptomatic at the final follow-up and showed a solid fusion. CT scan confirmed the malpositioned screw to be minimally intruding the foramen—nevertheless, no further intervention was required.
Discussion
The optimal treatment for traumatic fractures of the neural arch of the axis, the so-called Hangman’s fracture, is still controversial.
The treatment of Hangman’s fractures with traction reduction is well established and some authors reported a satisfactory outcome using this technique [2, 3, 7]. The most recent series was published by Vaccaro et al. [14] who reported a retrospective study evaluating early halo immobilization of Types II and IIA Hangman’s fractures. There were a total of 27 Type II and 4 Type IIA fractures. Of the Type II fractures, 21 went onto union after early halo immobilization. Six patients required reapplication of traction reduction because of fracture displacement. All the Type IIA fractures progressed to union. The patients requiring reapplication of traction had an initial fracture angulation of 12° or greater. On the contrary, other series [10, 15] reported nonunion, anterior instability and persistent pain in about 60% of cases of Type II, Type IIA, and Type III which were primarily treated conservatively. The main disadvantage of this technique was the prolonged time in halo immobilization which had an average of 3–6 months [14, 16, 17].
Several surgical techniques have been described, but the traditional approach for unstable Hangman’s fractures has been anterior fusion with a bony graft insertion in the C2–C3 space and segmental fixation with anterior plates [11, 18, 19]. ACDF at C2–C3 is often considered a complex procedure; a high anterior approach risks injury to vital structures especially the facial and hypoglossal nerves, branches of the external carotid artery, contents of the carotid sheath and the superior laryngeal nerve [11, 20].
The posterior approach was preferred for the relative simple procedure of exposure, involving no major visceral and vascular structure and thus lower complication rate. Since its initial description by Leconte [12], several clinical studies have described the use of direct repair of the pars fracture for surgical management of a Hangman’s fracture.
To our knowledge, this is the largest series focusing on the use of direct posterior pedicle screw fixation in Type II and Type IIA fractures. Borne et al. [20] reported on direct screw fixation in 13/18 cases of pedicular fractures of C2 and found it to be a simple and safe method of repair, giving consistently good anatomical and functional results. Muller et al. [21] used this technique in 5 of 15 patients with subtypes of Type II fractures and patients were placed in a hard collar for 5–8 weeks postoperatively. Verheggen and Jansen [22] also reported good results in 13 Type II and Type IIA patients treated with screw fixation and a collar. Later, Boullosa et al. [23] published a series of 10 patients; 9 had a good outcome with satisfactory consolidation of the fractures and disappearance of the symptoms. Finally, Hakało and Wroński [24] compared the results of 17 patients either treated with transoral C2–C3 discectomy with plate–cage stabilization (n = 9) or posterior direct pars screw repair (n = 8). They concluded that posterior direct pars screw repair seems to be safer, cheaper and more technically feasible.
The screw passes through the narrowest part of the vertebra, which is medially bound by the spinal cord and laterally by the vertebral artery. The diameter of the screw is 3.5 mm and the space through which it has to pass has an average of 5–7 mm. Accordingly, the rate of injury to vital structures varied between 11 and 66% [25, 26] which motivated the introduction of several innovations suggested to increase the accuracy of pedicle screw placement. Taller et al. [27] used CT guidance which allows for accurate intraoperative control of instrument and implant placement, determination of an appropriate screw length, anatomical fracture reduction and anchoring of the screw tip in the opposite cortex. Later, Rajasekaran et al. [28] reported the use of Iso-C-based computer navigation which acquires intraoperative real-time images after patient positioning and thus avoids registration errors and improves accuracy.
The biggest risk described in literature for this procedure is the occurrence of neurovascular injuries, and/or penetration into the vertebral canal [16, 29, 30]. In our series, one vertebral artery/vein injury occurred; the bleeding was presumed to be from the vertebral artery due to: the bright red colour of blood, its jetty pulsatile character and the profuse amount of blood loss of almost 1 L in a few minutes. Postoperatively the patient had no neurological deficit—at final follow-up was asymptomatic and showed a solid fusion. Although postoperative CT scan revealed inadequate placement of the screw, no additional measures were seen necessary.
Samaha et al. [31] reported a study of 24 patients investigated by plain radiography and CT, that asymmetry of the fracture did not affect outcome and thus should not influence decisions in treatment. They persisted with the posterior route, which they believed to facilitate correction of kyphosis and stabilization of the fractures. Similarly, in our series, 13 patients had bilateral symmetric isthmus fractures and only 2 patients had fractures involving the vertebral body; fracture asymmetry did not appear to hinder direct posterior pedicle screw fixation.
To our knowledge, very little has been reported on the use of CT scan in clinical trials to postoperatively assess the accuracy of screw placement. Only, 2 out of 30 inserted pedicle screws (6.6%) were minimally intruding into the spinal canal when checked by CT. This accuracy in screw placement is probably attributed to the meticulous identification of C2 pedicle after detaching the atlantoaxial ligament and identifying its superomedial aspect using a dissector carefully placed at the superior border of the lamina of C2. Other factors included correct orientation and angulation during drilling and screw introduction with the use of image intensification. There was no difference in assessing solid union between plain X-rays and CT scans.
Our clinical results suggest that with proper direct transpedicular osteosynthesis of Hangman’s fracture, there is enough stability to lead to clinical and radiological union. The hospitalization period was relatively short (4–18 days with an average of 6 days) and the need for longer hospital stay was due to associated injuries and not because of the surgical procedure. The visual analogue scale (VAS) and range of motion were assessed; all patients regained an excellent functional outcome with no limitation of the range of motion and adequate preservation of valuable motion segments.
Conclusions
Direct pedicle screw fixation appears to be a safe and useful modality in the reduction and stabilization of Hangman’s fracture. Adequate reduction was achieved and motion segments were preserved to a great extent with its use. This procedure is technically demanding and must be performed with extreme care to avoid possible complications. Hopefully, with the availability of modern innovations in our developing countries, these hazards would be reduced to a minimum.
Conflict of interest statement
None.
Contributor Information
Yasser ElMiligui, Email: el_miligui@yahoo.com.
Wael Koptan, Phone: +2-012-3118522, Email: waelkoptan@yahoo.com.
Ihab Emran, Email: ihabemran1@yahoo.co.uk.
References
- 1.Roda JM, Castro A, Blazquez MG. Hangman’s fracture with complete dislocation of C-2 on C-3. J Neurosurg. 1984;60:633–635. doi: 10.3171/jns.1984.60.3.0633. [DOI] [PubMed] [Google Scholar]
- 2.Hadley MN, Browner C, Sonntag VKH. Axis fractures: a comprehensive review of management and treatment in 107 cases. Neurosurgery. 1985;17:281–290. doi: 10.1227/00006123-198508000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Schneider RC, Livingston KE, Cave AJE, Gilbert H. Hangman’s fracture of the cervical spine. J Neurosurg. 1965;22:141–154. doi: 10.3171/jns.1965.22.2.0141. [DOI] [PubMed] [Google Scholar]
- 4.Grogono BJS. Injuries of the atlas and axis. J Bone Joint Surg. 1954;36-B(3):397–410. [Google Scholar]
- 5.Delorme TL. Axis pedicle fractures. J Bone Joint Surg. 1967;49-A:1471. [Google Scholar]
- 6.Brashear HR, Jr, Venters GC, Preston ET. Fractures of the neural arch of the axis. A report of twenty-nine cases. J Bone Joint Surg. 1975;57-A:879–887. [PubMed] [Google Scholar]
- 7.Francis WR, Fielding JW, Hawkins RJ, Pepin J, Hensinger R. Traumatic spondylolisthesis of the axis. J Bone Joint Surg. 1981;63-B(3):313–318. doi: 10.1302/0301-620X.63B3.7263740. [DOI] [PubMed] [Google Scholar]
- 8.Termansen NB. Hangman’s Fracture. Acta Orthop Scandinavica. 1974;45:529–539. doi: 10.3109/17453677408989176. [DOI] [PubMed] [Google Scholar]
- 9.Effendi B, Roy D, Cornish B, Dussault RG, Laurin CA. Fracture of the ring of the axis: a classification based on the analysis of 131 cases. J Bone Joint Surg. 1981;63-B(3):319–327. doi: 10.1302/0301-620X.63B3.7263741. [DOI] [PubMed] [Google Scholar]
- 10.Levine AM, Edwards CC. The management of traumatic spondylolisthesis of the axis. J Bone Joint Surg. 1985;67-A:217–226. [PubMed] [Google Scholar]
- 11.Cornish BL. Traumatic spondylolisthesis of the axis. J Bone Joint Surg. 1968;50-B(2):31–43. [PubMed] [Google Scholar]
- 12.Leconte P. Fracture et luxation des deux premières vertèbres cervicales. In: Judet R, editor. Luxation Congenénitale de la Hanche: Fractures du Cou-de-pied Rachis Cervical. Actualités de Chirurgie Orthopédique de l’Hö pital Raymond-Poincaré. Paris: Masson et Cie; 1964. pp. 147–166. [Google Scholar]
- 13.Judet R, Roy-Camille R, Saillant G. Actuallites de chiirugie orthopedique de l’hopital Raymound-pointcarre: fracture du rachis cervical. Paris: Masson; 1970. pp. 174–195. [Google Scholar]
- 14.Vaccaro AR, Madigan L, Bauerle WB, Blescia A, Cotler JM. Early halo immobilization of displaced traumatic spondylolisthesis of the axis. Spine. 2002;27(20):2229–2233. doi: 10.1097/00007632-200210150-00009. [DOI] [PubMed] [Google Scholar]
- 15.Coric D, Wilson JA, Kelly DL., Jr Treatment of traumatic spondylolisthesis of the axis with nonrigid immobilization: a review of 64 cases. J Neurosurg. 1996;85:550–554. doi: 10.3171/jns.1996.85.4.0550. [DOI] [PubMed] [Google Scholar]
- 16.Alan ML, Alan D. Traumatic spondylolisthesis of the axis: hangman’s fracture. In: Clark CR, editor. The cervical spine. 4. Philadelphia: Lippincott Williams & Wilkins; 2005. pp. 629–649. [Google Scholar]
- 17.Zavanone M, Guerra P, Rampini P, Crotti F, Vaccari U. Traumatic fractures of the craniovertebral junction. Management of 23 cases. J Neurosurg Sci. 1991;35:17–22. [PubMed] [Google Scholar]
- 18.Tuite GF, Papadopoulos SM, Sonntag VK. Caspar plate fixation for the treatment of complex hangman’s fractures. Neurosurgery. 1992;30(5):761–764. doi: 10.1227/00006123-199205000-00019. [DOI] [PubMed] [Google Scholar]
- 19.Ying Z, Wen Y, Xinwei W, Yong T, Hongyu L, Zhu H, Qinggang Z, Weihong Z, Yonggeng C. Anterior cervical discectomy and fusion for unstable traumatic spondylolisthesis of the axis. Spine. 2008;33(3):255–258. doi: 10.1097/BRS.0b013e31816233d0. [DOI] [PubMed] [Google Scholar]
- 20.Borne GM, Bedou GL, Pinaudeau M. Treatment of pedicular fractures of the axis. A clinical study and screw fixation technique. J Neurosurg. 1984;60:88–93. doi: 10.3171/jns.1984.60.1.0088. [DOI] [PubMed] [Google Scholar]
- 21.Muller EJ, Wick M, Muhr G. Traumatic spondylolisthesis of the axis: treatment rationale based on the stability of the different fracture types. Eur Spine J. 2000;9:123–128. doi: 10.1007/s005860050222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Verheggen R, Jansen J. Hangman’s fracture: arguments in favor of surgical therapy for type II and III according to Edwards and Levine. Surg Neurol. 1998;49(3):253–261. doi: 10.1016/S0090-3019(97)00300-5. [DOI] [PubMed] [Google Scholar]
- 23.Boullosa JL, Colli BO, Carlotti CG, Jr, Tanaka K, dos Santos MB. Surgical management of axis’ traumatic spondylolisthesis (Hangman’s fracture) Arq Neuropsiquiatr. 2004;62(3B):821–826. doi: 10.1590/s0004-282x2004000500015. [DOI] [PubMed] [Google Scholar]
- 24.Hakało J, Wroński J. Operative treatment of hangman’s fractures of C2. Posterior direct pars screw repair or anterior plate-cage stabilization? Neurol Neurochir Pol. 2008;42(1):28–36. [PubMed] [Google Scholar]
- 25.Ludwig SC, Kramer DL, Vaccaro AR, Albert TJ. Transpedicle screw fixation of the cervical spine. Clin Orthop Relat Res. 1999;359:77–88. doi: 10.1097/00003086-199902000-00009. [DOI] [PubMed] [Google Scholar]
- 26.Ludwig SC, Kowalski JM, Edwards CC, II, Heller JG. Cervical pedicle screws: comparative accuracy of two insertion technique. Spine. 2000;25:2675–2681. doi: 10.1097/00007632-200010150-00022. [DOI] [PubMed] [Google Scholar]
- 27.Taller S, Suchomel P, Lukas R, Beran J. CT-guided internal fixation of a hangman’s fracture. Eur Spine J. 2000;9(5):393–397. doi: 10.1007/s005860000159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rajasekaran S, Vidyadhara S, Shetty AP. Iso-C3D fluoroscopy-based navigation in direct pedicle screw fixation of Hangman fracture: a case report. J Spinal Disord Tech. 2007;20(8):616–619. doi: 10.1097/BSD.0b013e318074f978. [DOI] [PubMed] [Google Scholar]
- 29.Roy-Camille R, Saillant G, Mazel C. Internal fixation of the unstable cervical spine by a posterior osteosynthesis with plats and screws. In: The Cervical Spine Research Society, editor. The cervical spine. 2. Philadelphia: Lippincott Williams & Wilkins; 1989. pp. 390–403. [Google Scholar]
- 30.Abumi K, Kaneda K. Pedicle screw fixation for non traumatic lesions of the cervical spine. Spine. 1997;22:1853–1863. doi: 10.1097/00007632-199708150-00010. [DOI] [PubMed] [Google Scholar]
- 31.Samaha C, Lazennec JY, Laporte C, Saillant G (2000) Hangman's fracture: the relationship between asymmetry and instability. J Bone Joint Surg 82(7):1046–1052 [DOI] [PubMed]