Abstract
The study design includes prospective evaluation of percutaneous osteosynthesis associated with cement kyphoplasty on 18 patients. The objective of the study is to assess the efficacy of a percutaneous method of treating burst vertebral fractures in patients without neurological deficits. Even if burst fractures are frequent, no therapeutic agreement is available at the moment. We report in this study the results at 2 years with a percutaneous approach for the treatment of burst fractures. 18 patients were included in this study. All the patients had burst vertebral fractures classified type A3 on the Magerl scale, between levels T9 and L2. The patients’ mean age was 53 years (range 22–78 years) and the neurological examination was normal. A percutaneous approach was systematically used and a kyphoplasty was performed via the transpedicular pathway associated with percutaneous short-segment pedicle screw osteosynthesis. The patients’ follow-up included CT scan analysis, measurement of vertebral height recovery and local kyphosis, and clinical pain assessments. With this surgical approach, the mean vertebral height was improved by 25% and a mean improvement of 11.28° in the local kyphotic angle was obtained. 3 months after the operation, none of the patients were taking class II analgesics. The mean duration of their hospital stay was 4.5 days (range 3–7 days) and the mean follow-up period was 26 months (range 17–30 months). No significant changes in the results obtained were observed at the end of the follow-up period. Minimally invasive methods of treating burst vertebral fractures can be performed via the percutaneous pathway. This approach gives similar vertebral height recovery and kyphosis correction rates to those obtained with open surgery. It provides a short hospital stay, however, and might therefore constitute a useful alternative to open surgical methods.
Keywords: Percutaneous surgery, Burst fracture, Kyphoplasty, Pedicle screw fixation
Introduction
Vertebral fractures have been studied in detail in terms of their instability and the underlying mechanisms. They tend to occur preferentially at the thoraco-lumbar spine junction (60% of these fractures are located between T11 and L2), and Magerl [1] has subdivided vertebral fractures into three main types: type A compression fractures (lesions of the anterior spine), type B (transversal lesions involving both spinal columns) and type C (rotational lesions involving both columns). According to this system of classification, burst fractures belong to class A3. They account for 28% of all fractures of the thoracolumbar spine and are associated with an intact posterior ligamentous complex [1]. A second subdivision is done for burst fractures: A3.1 corresponds to an incomplete burst frature, A3.2 to a burst-split fracture and A3.3 to a complete axial burst fracture.
The management of burst fractures not associated with any neurological deficits has not yet been properly codified. The treatment used to be purely conservative [1–3], but the risk of secondary neurological complications due to the occurrence of local kyphosis and the development of novel osteosynthetic materials have given rise to new surgical methods. Since the last decades various techniques have been described for the treatment of burst fractures with satisfactory results. Richter et al. [4] described an original procedure of transpedicular grafting of the vertebral body to prevent loss of correction by consolidation of the anterior column. At this time, posterior approach with short-segment pedicle screw fixation seems to be the most widely used approach [3, 5], and some surgeons systematically also perform an anterior intervention at a later date. This two-stage procedure considerably lengthens the patients’ hospital stay and increases the surgical risks involved, especially for patients with co-morbidities. On the other hand, recent development of percutaneous techniques to stabilize the vertebral body with cement have emerged and have been used alone in association with posterior osteosynthesis for traumatic lesions with good outcomes [6–9].
We present here the results of a new method of dealing with type A3 burst fractures, using a single posterior transcutaneous approach combining a balloon kyphoplasty with percutaneous osteosynthesis. The aim of this method is two-fold: to reduce the fracture by performing kyphoplasty, and then to consolidate this reduction using posterior osteosynthesis and the cement to buttress the anterior part of the damaged vertebral body.
Materials and methods
Eighteen patients were included in this prospective study: there were 12 males and 6 females with a mean age of 53 years (range 22–78 years). All the patients had vertebral compression burst fractures classified as type A3 on the Magerl scale, without any neurological complications. All the patients in this series underwent preoperative clinical assessments, neurological tests and pain assessments using the visual analog scale (VAS). The radiological tests performed prior to surgery included standard frontal and lateral X-rays of the fractured vertebrae, CT scans with axial, sagittal and coronal reconstruction, and magnetic resonance imaging (MRI) in order to check that the spinal cord and the posterior ligamentous complex were intact.
Surgery was indicated for patients with thoracolumbar burst fractures without spinal cord compromise, with a normal disc on the MRI and more than 15° of local kyphosis and/or 25% of vertebral height loss. All patients showing discal damage on MRI or with neurological signs were excluded from the study.
Exactly the same surgical method was used on all the patients under general anaesthesia in the prone position on a radio-transparent operating table. Patients were installed with surgical bolsters placed under the thorax and the iliac crests in order to induce spinal lordosis and facilitate the reduction of the fracture.
The first surgical stage consisted of performing percutaneous kyphoplasty with 2 balloons after cannulation of the pedicles of the fractured vertebra under scopic control. The fracture was reduced by the combination of the method of installation and the inflatable balloons applied. Each balloon was inserted on the anterior part of the vertebral body under control of a lateral fluoroscopic guidance. Positioning of the balloons was guided by the type of the fracture. On the lateral view, the ideal direction was parallel to the superior endplate of the vertebral body in case of type A3.1 or A3.2 lesion and in the middle of the fracture body in A3.3 lesion. On the anteroposterior view, the direction of each balloon was convergent to the middle of the vertebral body. Cement was then injected into the anterior part of the vertebral body to consolidate the reduction and prevent the occurrence of secondary kyphosis. Polymethylmethacrylate (PMMA) acrylic cement was systematically used for the first patients of the series. In a second time, PMMA was used for patients older than 50 years and phosphocalcic cement (Calcibon™, Biomet, Warsaw, Indiana) was used for patients under 50 years.
In the second surgical phase, percutaneous osteosynthesis was performed using Sextant™ device (Sofamor Danek Medtronic, Memphis, Tennesse) and pedicular screws were installed under frontal and lateral scopic control. Short-segment screw fixation bridging only the fractured parts was used. No external contention devices or braces were prescribed after the operation.
During the follow-up period, all the patients underwent clinical assessments, tests to check that they had no neurological deficits and VAS pain assessments. The radiographic check-up systematically included CT scan reconstruction in order to check that the implants were properly placed and that no cement leakage had occurred into the spinal canal.
After leaving hospital, the patients were followed up as outpatients at the hospital ward: residual pain was assessed and the results of CT scan radiography performed 3 months, 6 months, 1 year and 2 years post-operatively were analysed.
Recovery of vertebral height (Fig. 1) was measured on the sagittal reconstructions, using two indices: first by comparing the height of the anterior face of the fractured vertebral body with that of the adjacent body both pre- and post-operatively, as described by Acosta [10]; and secondly, using the Beck index, as described by Maestretti [6], to compare the height of the anterior face of the fractured vertebral body with that of the posterior face of the same body. The presence of any local segmental vertebral kyphosis was checked both before and after surgery.
Fig. 1.

Restoration of vertebral height measured between the anterior part of the fractured vertebra (1) and the anterior part of the adjacent vertebral body (2). Beck’s index measured between the anterior part of the fractured vertebra and the posterior part (3)
The results obtained were analysed statistically using the Kolmogorov–Smirnov test to check the normality of the data distribution and Pearson’s coefficient of correlation was determined on paired series of pre- and post-operative measurements. Student’s t test for paired series was used to test the significance of the differences between pre- and post-operative measurements with an alpha risk level of 5%.
Results
Eighteen patients with vertebral burst fractures (12 males and 6 females) were treated using the surgical method described above. The patients’ characteristics are summarized in Table 1. The lesions were located at T9 level in one case, T11 level in one case, T12 level in four cases, L1 level in nine cases and L2 level in three cases. The fractures were classified as type A3.1 in seven cases (38.9%), A3.2 in two cases (11.1%) and A3.3 in nine cases (50%).
Table 1.
Summary of patients’ clinical data
| Patient | Genre | Age | Fracture type | Level | Pre-operative VAS | Post-operative VAS | Cement |
|---|---|---|---|---|---|---|---|
| 1 | F | 54 | A3.1 | T12 | 7 | 0 | PMMA |
| 2 | M | 78 | A3.3 | L1 | 8 | 2 | PMMA |
| 3 | M | 54 | A3.2 | L1 | 6 | 0 | PMMA |
| 4 | M | 70 | A3.3 | L1 | 7 | 0 | PMMA |
| 5 | M | 36 | A3.1 | T12 | 7 | 0 | PCC |
| 6 | M | 61 | A3.3 | T9 | 7 | 1 | PMMA |
| 7 | M | 47 | A3.3 | L2 | 6 | 1 | PCC |
| 8 | M | 71 | A3.3 | T12 | 6 | 2 | PMMA |
| 9 | M | 47 | A3.3 | T11 | 7 | 2 | PMMA |
| 10 | M | 56 | A3.3 | L1 | 7 | 2 | PMMA |
| 11 | M | 22 | A3.1 | L1 | 5 | 1 | PCC |
| 12 | F | 41 | A3.1 | L1 | 4 | 1 | PCC |
| 13 | M | 54 | A3.1 | L2 | 7 | 1 | PMMA |
| 14 | F | 53 | A3.1 | L1 | 7 | 1 | PMMA |
| 15 | F | 76 | A3.3 | L1 | 8 | 2 | PMMA |
| 16 | F | 59 | A3.3 | L2 | 8 | 1 | PMMA |
| 17 | M | 40 | A3.1 | L1 | 8 | 2 | PCC |
| 18 | F | 36 | A3.1 | T12 | 8 | 1 | PMMA |
PMMA polymethylmethacrylate, PCC phosphocalcic cement
None of the patients were found to have any post-operative neurological complications. The mean pre-operative pain intensity level was 6.8 on the VAS (range 4–8). 20-mL inflatable balloons were used during the surgical procedure on all the patients, and the mean amount of cement injected was 6.4 mL (range 3.5–9 mL). The mean duration time of the operation was 100 min (range 90–120 min) and since there was very little loss of blood, no blood perfusions were required. PMMA acrylic cement was used in 13 cases (72.2% of the patients) and phosphocalcic cement in 5 cases (27.8% of the patients). The phosphocalcic cement was used later in our experience, associated to our learning curve, due to the fact that such cement is less radiopaque with a fast crystallization that requires a quick injection in a more liquid phase than PMMA, increasing the risk of leakage.
The patients’ pain levels improved significantly after the operation, since the mean VAS dropped to 1.1 (range 0–2) (p < 0.001) on the day of discharge and at final follow-up. No neurological complications and scare infections were noticed during the follow-up period.
Analysis of the post-operative radiographic and scanographic images confirmed that all the pedicular screws were properly positioned. The CT scan images also showed that no cement leakage had occurred into the spinal canal (Fig. 2), and two cases of lateral leakage were diagnosed without clinical consequences. On post-operative examinations, no signs of significant phosphocalcic cement resorption or bridging of intervertebral segment were noticed.
Fig. 2.
Axial CT-scan immediate post-operative reconstruction, verification of pedicular screws positioning and search for cement leakage
Based on the post-operative radiographic and scanographic images (Figs. 3 and 4), the restored vertebral height was judged to be satisfactory in all the patients in this series. The results of the statistical analysis showed the occurrence of a significant increase (p < 0.001) in the values of the two vertebral height indices used. The mean ratio between the height of the anterior face of the fractured vertebral body and that of the adjacent body, which amounted to 65% pre-operatively (range 36–83%), increased to 89% (range 67–100) post-operatively, corresponding to a vertebral improvement of 24.2%. The mean value of the Beck vertebral height index also increased significantly by 26.4%, from 65% (range 40–83%) to 92% (range 82–100%) post-operatively.
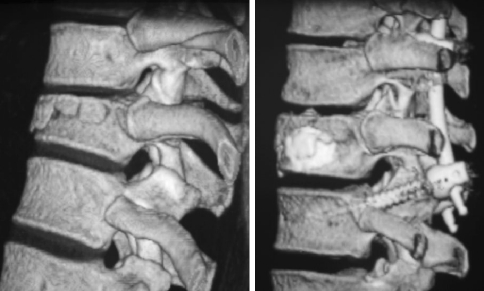
Fig. 3.
Pre-operative sagittal view of the burst fracture (a), post-operative sagittal reconstruction (b) and evolution after 2 years follow-up (c) without significant loss of correction on the same patient: cement and postoperative percutaneous posterior osteosynthesis are visible on the right
Fig. 4.
Sagittal three-dimensional CT-scan reconstruction showing the fractured level before (left) and immediately after the surgical procedure with a satisfactory restoration of vertebral height (right)
Similar significant differences (p < 0.001) were also observed in the local kyphosis measured at the level of the fracture, which improved by 11.3° (mean pre-operative value 14.4° (range 5°–35°) vs. mean post-operative value 3.2° (range −5°–10°).
The results of all the statistical tests carried out are given in Tables 2 and 3.
Table 2.
Results of Student test
| Pre-operative | Post-operative | p | Mean variations | |||
|---|---|---|---|---|---|---|
| Mean values | Range | Mean values | Range | |||
| Local kyphosis | 14.44° | 5°–35° | 3.17° | −5°, 10° | <0.001 | −11.28° |
| Anterior/adjacent vertebral height index | 65% | 36–83% | 89% | 67–100% | <0.001 | +24.17% |
| Beck index | 65% | 40–83% | 92% | 82–100% | <0.001 | +26.44% |
Table 3.
Variations of each measured parameters from the initial evaluation to the last follow-up
| Pre-operative | Post-operative | 3 months | 6 months | 12 months | 24 months | Loss of correction | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | Range | Mean | Range | Mean | Range | Mean | Range | Mean | Range | Mean | Range | Mean | Range | |
| Ant/Adj | 65% | 36–83 | 89% | 66–100 | 88% | 64–100 | 87% | 64–100 | 86% | 62–100 | 86% | 62–100 | 3% | 0–5 |
| Beck index | 65% | 40–83 | 92% | 78–100 | 90% | 78–100 | 88% | 76–100 | 88% | 77–99 | 88% | 77–99 | 4% | 0–6 |
| Local Kyphosis | 14.4° | 5–35 | 3.2° | −5, 10 | 4.5° | −3, 10 | 4.6° | −2, 10 | 4.8° | −2, 9 | 5.2° | –2, 9 | 2° | 1–7 |
The mean duration of the hospital stay was 4.5 days (range 3–7 days) and the mean timing of resuming work was 3 months.
The patients in this series were followed up for 26 months on an average (range 17–30 months). The vertebral height showed an average loss of 3% and local kyphotic an average loss of 2° on the measurements performed at the end of the follow-up period. No statistical difference was observed concerning vertebral loss and disc height between the different types of fractures, but this may be due to the reduce size of each group.
Discussion
The management of thoracolumbar burst fractures in patients with no neurological deficits has not been properly coded to date. No consensus has been reached between those using orthopaedic and surgical approaches to these lesions, and none of the methods proposed in the literature seem to stand out significantly from the others [11].
However, surgical treatment of these fractures seems to reduce pain and mobilize the patients more quickly, and the duration of the hospital stay is therefore shorter in this case. The development of new minimal invasive strategies can be therefore an interesting alternative for the treatment of burst fractures and the results of a recent prospective study [6] with standalone balloon kyphoplasty showed satisfactory outcomes, especially for A3.1 fractures.
Like all surgical interventions, pedicular screw stabilization is not devoid of risks, since it can cause nerve injuries. Pedicular screws were implanted in this study using a percutaneous approach under frontal and lateral control, which ensures for greater safety, as confirmed by the fact that the post-operative CT scan images showed that the screws were all properly positioned in the present series of patients.
Cementoplasty also involves risks of complications, including cement leakage into the spinal canal. In the context of traumatology, the risk of cement leaking into the spinal canal is greater when the posterior wall has been damaged, as in the case of burst A3 [12] type fractures. In a study by Ryu [13], the risk of leakage was assessed depending on the volume of cement injected and the level treated. Greater leakage was found to occur when the level treated was superior to T7, where the risk could be as high as 26.5% of the patients treated. The use of balloon kyphoplasty makes it possible to reduce the risk of leakage and thus the risk of occurrence of mechanical compression and exothermic reactions involving nerve structures [14]. After reducing the fracture using inflatable balloons, the reduced fracture can be consolidated by injecting cement as anteriorly as possible, which prevents the cement from entering the spinal canal [15].
The most original feature of the method presented in this study is the fact that the fracture was reduced and the spinal column was stabilized using a purely posterior approach. Applying a single posterior osteosynthesis is known to involve the risk of secondary kyphosis, corresponding to an angle of 5° in 68% of the patients in a series studied by Been [2]. The loss of correction is most important when short-segment osteosynthesis is used, which is becoming increasingly common in the field of traumatology. The use of the percutaneous Sextant™ system involves the implantation of polyaxial screws which are less rigid [16] and might therefore increase the risk of loss of correction with time, as reported by Palmisani [17] (5.1° of loss of correction on local kyphosis with a mean follow-up of 14 months). It is therefore necessary to stiffen the reduction by consolidating the anterior part of the vertebral column. For this purpose, some authors have suggested using a combined posterior and anterior approach. Uchida [18] recently reported that vertebral kyphosis could be corrected more efficiently using a posterior approach, but that the correction was gradually lost, which meant that the outcome at the final follow-up was equivalent to that obtained using an anterior pathway. The method described in the present study, which is based on the use of a single posterior approach, combines the advantages of efficient reduction obtained via the posterior technique and stable reduction obtained via an anterior approach. The results obtained here are in line with those of a previous study on a balloon kyphoplasty procedure, where vertebral height was restored by more than 20% [19] and local kyphosis was improved by 9.9° [20]. According to our study, correction obtained is also stable in time with a nonsignificant loss of correction at final follow-up (3% of vertebral height and 2° of kyphosis after 2 years) and seems to occur during the first months after surgery.
The combined method presented here, involving both kyphoplasty and percutaneous osteosynthesis, therefore provides a useful strategy for dealing with Magerl A3 type burst fractures not associated with neurological deficits. After undergoing this minimally invasive surgery (Fig. 5), patients are able to return home quickly after a mean hospital stay of only 4.5 days compared to 10.1 days in the case of patients treated via the posterior pathway and 7.2 days in patients treated via the anterior approach [3]. However, length of stay and the time of resuming work must be considered with caution due to various factors like organization of medical system or insurance reimbursement system that may influence these parameters. It is also possible to perform hardware removal through a minimally invasive approach and we recommend it especially in young patients to preserve mobility of adjacent levels.
Fig. 5.

Minimally invasive access: cosmetic results obtained after the insertion of pedicular screws and balloon kyphoplasty (day 5 after surgery)
This percutaneous method therefore seems to provide a useful approach to these vertebral lesions when no neurological deficits are present: no significant changes were observed in the results obtained 2 years after the operation was performed. In our opinion, this is a promising method of treating A3 burst fractures in patients without neurological deficits.
References
- 1.Magerl F, Aebi M, Gertzbein SD, Harms J, Nazarian S. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1994;3:184–201. doi: 10.1007/BF02221591. [DOI] [PubMed] [Google Scholar]
- 2.Been HD, Bouma GJ. Comparison of two types of surgery for thoraco-lumbar burst fractures: combined anterior and posterior stabilisation vs. posterior instrumentation only. Acta Neurochir (Wien) 1999;141:349–357. doi: 10.1007/s007010050310. [DOI] [PubMed] [Google Scholar]
- 3.Wood KB, Bohn D, Mehbod A. Anterior versus posterior treatment of stable thoracolumbar burst fractures without neurologic deficit: a prospective, randomized study. J Spinal Disord Tech. 2005;18(Suppl):S15–S23. doi: 10.1097/01.bsd.0000132287.65702.8a. [DOI] [PubMed] [Google Scholar]
- 4.Richter-Turtur M, Krueger P, Stephan F, Mandelkow H, Sauer T. Expanded trans-pedicular spongiosa grafting–dorsal approach to filling of the intervertebral spaces with cancellous bone. Unfallchirurg. 1990;93:387–389. [PubMed] [Google Scholar]
- 5.Okuyama K, Abe E, Chiba M, Ishikawa N, Sato K. Outcome of anterior decompression and stabilization for thoracolumbar unstable burst fractures in the absence of neurologic deficits. Spine. 1996;21:620–625. doi: 10.1097/00007632-199603010-00016. [DOI] [PubMed] [Google Scholar]
- 6.Maestretti G, Cremer C, Otten P, Jakob RP. Prospective study of standalone balloon kyphoplasty with calcium phosphate cement augmentation in traumatic fractures. Eur Spine J. 2007;16:601–610. doi: 10.1007/s00586-006-0258-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cho DY, Lee WY, Sheu PC. Treatment of thoracolumbar burst fractures with polymethyl methacrylate vertebroplasty and short-segment pedicle screw fixation. Neurosurgery. 2003;53:1354–1360. doi: 10.1227/01.NEU.0000093200.74828.2F. [DOI] [PubMed] [Google Scholar]
- 8.Verlaan JJ, Dhert WJ, Verbout AJ, Oner FC. Balloon vertebroplasty in combination with pedicle screw instrumentation: a novel technique to treat thoracic and lumbar burst fractures. Spine (Phila Pa 1976) 2005;30:E73–E79. doi: 10.1097/01.brs.0000152162.64015.fb. [DOI] [PubMed] [Google Scholar]
- 9.Afzal S, Akbar S, Dhar SA. Short segment pedicle screw instrumentation and augmentation vertebroplasty in lumbar burst fractures: an experience. Eur Spine J. 2008;17:336–341. doi: 10.1007/s00586-008-0587-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Acosta FL, Jr, Aryan HE, Taylor WR, Ames CP. Kyphoplasty-augmented short-segment pedicle screw fixation of traumatic lumbar burst fractures: initial clinical experience and literature review. Neurosurg Focus. 2005;18:e9. doi: 10.3171/foc.2005.18.3.10. [DOI] [PubMed] [Google Scholar]
- 11.Thomas KC, Bailey CS, Dvorak MF, Kwon B, Fisher C. Comparison of operative and nonoperative treatment for thoracolumbar burst fractures in patients without neurological deficit: a systematic review. J Neurosurg Spine. 2006;4:351–358. doi: 10.3171/spi.2006.4.5.351. [DOI] [PubMed] [Google Scholar]
- 12.Chen JF, Lee ST. Percutaneous vertebroplasty for treatment of thoracolumbar spine bursting fracture. Surg Neurol. 2004;62:494–500. doi: 10.1016/j.surneu.2003.10.049. [DOI] [PubMed] [Google Scholar]
- 13.Ryu KS, Park CK, Kim MC, Kang JK. Dose-dependent epidural leakage of polymethylmethacrylate after percutaneous vertebroplasty in patients with osteoporotic vertebral compression fractures. J Neurosurg. 2002;96:56–61. doi: 10.3171/spi.2002.96.1.0056. [DOI] [PubMed] [Google Scholar]
- 14.Fourney DR, Schomer DF, Nader R, Chlan-Fourney J, Suki D, Ahrar K, Rhines LD, Gokaslan ZL. Percutaneous vertebroplasty and kyphoplasty for painful vertebral body fractures in cancer patients. J Neurosurg. 2003;98:21–30. doi: 10.3171/jns.2003.98.1.0021. [DOI] [PubMed] [Google Scholar]
- 15.Atalay B, Caner H, Gokce C, Altinors N. Kyphoplasty: 2 years of experience in a neurosurgery department. Surg Neurol. 2005;64(Suppl 2):S72–S76. doi: 10.1016/j.surneu.2005.07.039. [DOI] [PubMed] [Google Scholar]
- 16.Foley KT, Gupta SK, Justis JR, Sherman MC. Percutaneous pedicle screw fixation of the lumbar spine. Neurosurg Focus. 2001;10:E10. doi: 10.3171/foc.2001.10.4.11. [DOI] [PubMed] [Google Scholar]
- 17.Palmisani M, Gasbarrini A, Brodano GB, Iure F, Cappuccio M, Boriani L, Amendola L, Boriani S. Minimally invasive percutaneous fixation in the treatment of thoracic and lumbar spine fractures. Eur Spine J. 2009;18(Suppl 1):71–74. doi: 10.1007/s00586-009-0989-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Uchida K, Kobayashi S, Matsuzaki M, Nakajima H, Shimada S, Yayama T, Sato R, Baba H. Anterior versus posterior surgery for osteoporotic vertebral collapse with neurological deficit in the thoracolumbar spine. Eur Spine J. 2006;15:1759–1767. doi: 10.1007/s00586-006-0106-z. [DOI] [PubMed] [Google Scholar]
- 19.Majd ME, Farley S, Holt RT. Preliminary outcomes and efficacy of the first 360 consecutive kyphoplasties for the treatment of painful osteoporotic vertebral compression fractures. Spine J. 2005;5:244–255. doi: 10.1016/j.spinee.2004.09.013. [DOI] [PubMed] [Google Scholar]
- 20.Voggenreiter G. Balloon kyphoplasty is effective in deformity correction of osteoporotic vertebral compression fractures. Spine. 2005;30:2806–2812. doi: 10.1097/01.brs.0000190885.85675.a0. [DOI] [PubMed] [Google Scholar]