Abstract
C2 laminar screws have become an increasingly used alternative method to C2 pedicle screw fixation. However, the outcome of this technique has not been thoroughly investigated. A total of 35 cases with upper cervical spinal instability undergoing C2 laminar screw fixation were reviewed. All cases had symptoms of atlantoaxial instability, such as craniocervical junction pain, and were fixed with the Vertex cervical internal fixation system. A total of 68 screws were placed and hybrid constructs (a C2 translaminar screw combined with a C2 pars screw) were incorporated in two patients. In this series, there were no intraoperative complications and no cases of neurological worsening or vascular injury from hardware placement. Computed tomographic scans demonstrated a partial dorsal laminar breach in ten patients. None of these resulted in neurological symptoms. None of the patients was found to have a breach of the ventral laminar cortex. All the C2 laminar screws fixations were performed successfully. There was no instability seen on the films with no evidence of hardware failure or screw loosening during the follow-up period in all patients. In conclusion, C2 laminar screw technique is straightforward and easily adopted; it can efficiently and reliably restore upper cervical stability. It is an alternative method to C2 pedicle screw fixation, especially in patients with unilateral occlusion of vertebral artery and pedicle deformity of C2.
Keywords: C2 translaminar screws, Atlantoaxial stabilization, Cervical fusion, Screw fixation, Posterior instrumentation
Introduction
Instability of the upper cervical spine requiring surgical stabilization may be treated with a variety of techniques that have evolved from wiring techniques to more rigid fixations of the axis, in which transarticular, pedicle/pars or laminar screws attached to rods are implanted [1–4]. Older methods of atlantoaxial fixation, such as the Brooks-Jenkins or modified Gallie wiring techniques, are simpler procedures but require rigid immobilization after surgery and have nonunion rates of up to 30% [1, 2]. Several biomechanical studies have suggested that these posterior wiring techniques may not provide sufficient immobilization of the atlantoaxial complex [3, 5, 6]. As a result, newer techniques effectively limit motion along all axes. Two more popular methods are the transarticular screw technique of Jeanneret and Magerl [1, 2] and the Harms C1 lateral mass technique. The first technique involves placing a transarticular screw across the C1–C2 joint, while the second involves screw placement in the C1 lateral masses and the C2 pedicles, which are then longitudinally connected via rods. Both techniques involve screw fixation into the C2 pars/pedicle, which can result in a significant risk to the vertebral artery. Several authors have shown up to a 20% incidence of vertebral anomalies that would not allow safe placement of these screws [7, 8]. Injury to the vertebral artery has been identified in multiple large case series and is generally believed to occur with an incidence of 2–8% [7]. For these reasons, a technique using crossing screws placed directly onto the cancellous bone of the laminar of C2 was devised [4]. In this study, we used crossing C2 laminar screws to effect C2 fixation in 35 patients. The axis was successfully stabilized using this technique.
Materials and methods
From October 2004 to October 2008, 35 consecutive patients with upper cervical spinal instability who underwent C2 laminar screw fixation were reviewed. Prior to surgery, all patients underwent preoperative radiological evaluation of the cervical spine, including CT scanning with multiplanar reconstruction to assess the posterior anatomy of C2 and ensure adequate thickness of the laminae. There were 19 males and 16 females, with a mean age of 45 years (ranging from 23 to 73 years old).There were 19 cases of delayed odontoid fracture, 1 case of rupture of the axis transverse ligament, 2 cases of congenital loose odontoid process, 7 cases of Jefferson fracture combined with atlantoaxial instability, 5 cases of traumatic instability of C2–3 and 1 case of an atypical Hangman fracture. All cases had symptoms of atlantoaxial instability, such as craniocervical junction pain, and were fixed with the Vertex cervical internal fixation system. A total of 68 laminar screws were placed and, in two patients, hybrid constructs (a C2 translaminar screw combined with a C2 pars screw) were incorporated because the lamina was found to be too thin. The patients were then assessed both clinically and radiographically with postoperative computed tomographic scans.
Surgical technique
Patients were placed in the prone position with the head and cervical spine maintained in the neutral position using the Mayfield head holder. Exposure of the posterior upper cervical spine was then accomplished in the usual manner. The posterior arch of C1 was identified to the lateral aspect. The spinous process, laminae and medial lateral masses of C2 were then exposed. The spinous processes, laminae and lateral masses of the subaxial spine were exposed as needed. C1 lateral mass screws were placed using the technique described by Tan [9], with 4.0 × 26 to 4.0 × 30 mm polyaxial lag screws (Vertex; Medtronic Sofamor Danek, Memphis, TN) inserted bilaterally. For constructs involving the subaxial spine, 3.5 × 14 mm polyaxial screws were inserted in the lateral masses using the technique described by Roy-Camille [10] or pedicle screw fixation.
For fixation of C2, using crossing screws placed directly onto the cancellous bone of the laminar of C2 described by Wright [4], a high-speed drill was then used to open a small cortical window at the junction of the C2 spinous process and lamina on the right, close to the rostral margin of the C2 lamina. With a hand drill, the contralateral lamina was carefully drilled to a depth of 30 mm, with the drill visually aligned along the angle of the exposed contralateral laminar surface. To avoid injury to the spinal canal, the trajectory of insertion was kept slightly less than the downslope of the lamina to ensure that any possible cortical breakthrough would occur dorsally through the laminar surface, rather than ventrally into the spinal canal. Additionally, a small ball probe was used to palpate the length of the hole to verify that no cortical breakthroughs into the spinal canal had occurred. A 4.0 × 26 to 4.0 × 32 mm polyaxial screw was then carefully inserted along the same trajectory. In the final position, the screw head remained at the junction of the spinous process and lamina on the right with the length of the screw within the left lamina.
A small cortical window was then made at the junction of the spinous process and lamina of C2 on the left, close to the caudal aspect of the lamina. Using of the same technique as above, a 4.0 × 26 to 4.0 × 32 mm screw was then placed onto the right lamina, with the screw head remaining on the left side of the spinous process. After screw placement, all exposed laminar surfaces were decorticated with a high-speed drill. Rods were contoured and then secured to the remaining screw heads in the construct. Local autograft and morselized autologous iliac crest bone graft were packed around the remaining exposed bone surfaces and into the decorticated facet complexes. An intraoperative lateral cervical spine radiograph was always obtained to corroborate positioning of the instrumentation.
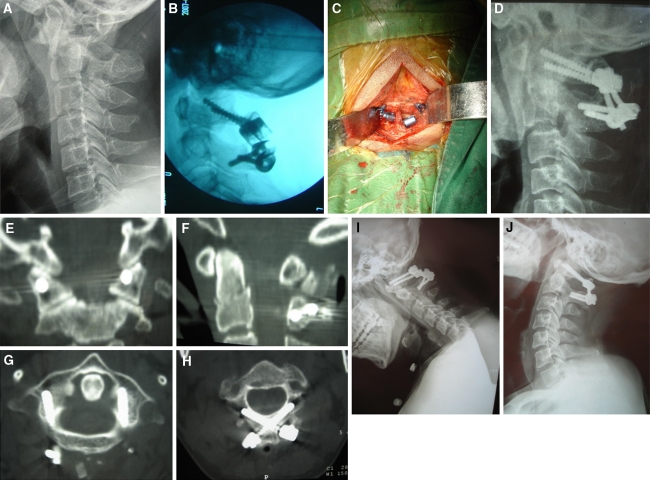
All patients were immobilized with rigid cervical collars for 6 weeks. Radiographs and CT scans obtained in the immediate postoperative period were used to confirm accurate placement of hardware. All patients were evaluated at 6 weeks, 3 and 6 months with flexion and extension lateral radiographs (Fig. 1).
Fig. 1.
A 35-year-old female with type II delayed odontoid fracture. a Lateral X-ray view; b intraoperative X-ray view; c intraoperative picture; d postoperative lateral X-ray view; e, f postoperative CT reconstruction; g, h postoperative CT scan; i, j flexion and extension lateral X-ray views, postoperative 6 months
Results
The average operative time was 102 min (with a range from 78 to 129 min). No patient received blood transfusion. The average length of hospitalization was 8.2 days (range 4–19 days). There were no intraoperative complications and no cases of neurological worsening or vascular injury from hardware placement. Computed tomographic scans demonstrated a partial dorsal laminar breach in ten patients. None of these resulted in neurological symptoms. None of the patients was found to have a breach of the ventral laminar cortex. All patients were followed up from 6 to 54 months, with the average being 29 months. There was no instability seen on these films and no clinical evidence of hardware failure or screw loosening during the follow-up period in all patients.
Discussion
Instrumentation of C1–2 instability can be accomplished via multiple possible constructs. The traditional transarticular technique, combined with various wiring methods, has demonstrated enhanced biomechanical outcomes when compared with stand-alone wiring methods [3, 5]. However, variations in bone anatomy may result in an increased risk of vertebral artery injury during transarticular screw placement procedures. Vertebral artery injuries can cause serious complications, such as brain infarction in the regions of the cerebellum and posterior cerebral artery, as well as life-threatening brain stem infarction [7, 8]. Harms described posterior C1–C2 fusion using a polyaxial screw into the lateral mass of C1 as well as C2 pedicle screws [2]. This technique is thought to have less risk of injury to the vertebral artery secondary to a more superior and medial trajectory of the C2 pedicle screw. However, risk of injury to the vertebral artery still exists, and the technique can be technically challenging. Variable pedicle size, angle and location of the foramen transversarium and either asymmetry or hypoplasia of the vertebral artery can make placement of this screw difficult with a high risk of injuring either the adjacent vertebral artery or spinal cord [7, 8]. Igarashi et al. [11] showed that 20% of specimens had a pedicle diameter less than 3.5 mm. Ebraheim et al. [8] showed a high rate of violation of the foramen transversarium with attempted pedicle screw placement.
Wright [4] recently described a novel technique of screw fixation into the axis using bilateral, crossing laminar screws. This technique allows for immobilization of the axis without risk to the vertebral artery. The technique was thought to be advantageous because of the large size of the C2 lamina and the ability to directly visualize all relevant structures, potentially decreasing the need for intraoperative navigation. The screw is placed parallel to the downslope of the contralateral lamina to avoid penetration into the spinal canal. Dissection under the C2 lamina can be performed to prevent canal penetration. These screws can be connected to C1 lateral mass screws. The lateral mass screw is connected to the ipsilateral screw head of the C2 laminar screw using a connecting rod, thus stabilizing the lateral mass to the contralateral C2 lamina. A similar connection can be undertaken for incorporation of C2 into subaxial constructs.
Biomechanical stability of this fixation technique has recently been evaluated by Gorek et al. [12], who found intralaminar screw constructs to be biomechanically equivalent to the Harms construct, and by extrapolation to the Magerl-Gallie construct for atlantoaxial fixation. In a similar study, Lapsiwala et al. [13] have reported on a cadaveric biomechanical study comparing intralaminar to pedicle and transarticular screws for C1–C2 fixation. They demonstrated in both intact and destructive cadaveric models that C2 fixation was equivalent to other methods in flexion/extension and axial rotation, but somewhat less rigid in lateral bending.
The anatomic study of Cassinelli et al. [14] showed that 71% of specimens had a laminar thickness of C2 ≥ 5 mm and 93% had ≥4 mm, but there was a wide range of laminar thicknesses noted (1.35–9.77 mm). As a result, insertion of the screw at the junction of the contralateral spinolaminar junction would permit placement of at least a 20-mm screw in virtually all adult patients without entering the lateral mass. This study shows that C2 laminar screws can be safely used in a large percentage of patients.
Besides avoiding vertebral artery injuries, the insertion of a laminar screw into C2 has another advantage: a navigation system is not necessary because the screws can be inserted under direct vision of the lamina. On the other hand, one disadvantage of this method is that injuries to the spinal canal located in the ventral area cannot be easily observed. Wang [15] reported on 30 patients who underwent high cervical intralaminar fixation with crossing intralaminar screws. Computed tomographic scans demonstrated a partial dorsal laminar breach in 11 patients and violation of the spinal canal in 1. None of these resulted in neurological symptoms. In this series, there were no intraoperative complications and no cases of neurological worsening or vascular injury from hardware placement in 35 patients. Computed tomographic scans demonstrated a partial dorsal laminar breach in 10 patients. None of these resulted in neurological symptoms. None of the patients was found to have a breach of the ventral laminar cortex.
From our clinical experience, the ability to place a laminar screw under direct visualization may allow a size of 3.5–4.0 × 26–30 mm screw to be acceptable. The only major structure at risk with placement of these screws is penetration into the spinal canal. If there is concern of this occurring, a slightly more dorsal trajectory can be used resulting in slight penetration of the dorsal cortex. Another option is to introduce a blunt dissector extraperiosteally onto the canal side of the lamina to help against screw penetration into the canal. Even if penetration of the spinal canal occurs, however, the risk of injury to the neural elements is low since the screw trajectory is virtually tangential to the spinal cord. The author used a hand drill to carefully advance down the contralateral lamina to prevent breakout into the spinal canal and probed the hole carefully prior to screw placement. Therefore, when planning screw insertion, a preoperative evaluation of the laminar diameter is necessary to select screws with an appropriate diameter and length before the operation. Preoperative CT scans are useful to determine whether the laminae are of sufficient thickness and height to accommodate two crossed laminar screws at the same level.
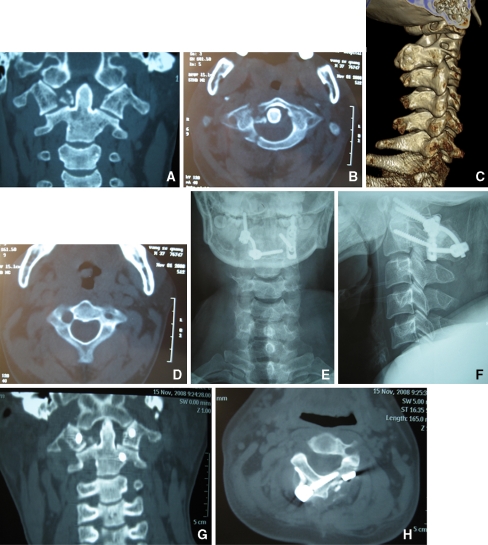
Therefore, crossed laminar screws are a useful alternative for fixation as a salvage technique when there is anomalous anatomy, when other spinal fixation techniques have failed or as a primary fixation technique. Particularly, the laminar screw of C2 basically should be used for the following cases: a small pedicle of the vertebral arch to which even a screw of 3.5 mm in diameter cannot be inserted (Fig. 2), cases with remarkably severe osteosclerosis of the pedicle of he vertebral arch that has no medullary space, the dominant side of the asymmetric vertebral arteries, the opposite side of unilateral vertebral artery occlusion or patients with a high-riding vertebral artery [16]. This technique is not suited for patients who have thin laminae or severe osteoporosis.
Fig. 2.
A 28-year-old male. a Preoperative reconstructed CT showed C1 fracture combined with C1–C2 instability; b preoperative CT scan; c preoperative three-dimension CT showed a small pedicle of the left side of C2; d preoperative CT scan of C2; e, f postoperative AP and lateral X-ray views; g postoperative CT reconstruction; h postoperative CT scan
Conclusion
Crossing C2 laminar screws provide the surgeon with an expanded armamentarium for fixation in the high cervical spine. This technique is straightforward and easily adopted. Posterior C2 laminar screw fixation is an efficient and reliable technique and has the advantage of being a relatively simple and safe operation, especially using a laminar screw (intralaminar screw) in a patient with unilateral occlusion of vertebral artery and pedicle deformity of C2.
References
- 1.Jeanneret B, Magerl F. Primary posterior fusion C1/2 in odontoid fractures: indications, technique, and results of transarticular screw fixation. J Spinal Disord. 1992;5:464–475. doi: 10.1097/00002517-199212000-00012. [DOI] [PubMed] [Google Scholar]
- 2.Harms J, Melcher RP. Posterior C1–C2 fusion with polyaxial screw and rod fixation. Spine. 2001;26:2467–2471. doi: 10.1097/00007632-200111150-00014. [DOI] [PubMed] [Google Scholar]
- 3.Reilly TM, Sasso RC, Hall PV. Atlantoaxial stabilization: clinical comparison of posterior cervical wiring technique with transarticular screw fixation. J Spinal Disord Tech. 2003;16:248–253. doi: 10.1097/00024720-200306000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Wright NM. Posterior C2 fixation using bilateral, crossing C2 laminar screws: case series and technical note. J Spinal Disord Tech. 2004;17:158–162. doi: 10.1097/00024720-200404000-00014. [DOI] [PubMed] [Google Scholar]
- 5.Richter M, Schmidt R, Claes L, Puhl W, Wilke HJ. Posterior atlantoaxial fixation: biomechanical in vitro comparison of six different techniques. Spine. 2002;27:1724–1732. doi: 10.1097/00007632-200208150-00008. [DOI] [PubMed] [Google Scholar]
- 6.Grob D, Crisco JJ, III, Panjabi NM, Wang P, Dvorak J. Biomechanical evaluation of four different posterior atlantoaxial fixation techniques. Spine. 1992;17:480–490. doi: 10.1097/00007632-199205000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Wright NM, Lauryssen C. Vertebral artery injury in C1-2 transarticular screw fixation: Results of a survey of the AANS/CNS section on disorders of the spine and peripheral nerves. American Association of Neurological Surgeons/Congress of Neurological Surgeons. J Neurosurg. 1998;88:634–640. doi: 10.3171/jns.1998.88.4.0634. [DOI] [PubMed] [Google Scholar]
- 8.Ebraheim N, Rollins JR, Jr, Xu R, Jackson WT. Anatomic consideration of C2 pedicle screw placement. Spine. 1996;21:691–695. doi: 10.1097/00007632-199603150-00005. [DOI] [PubMed] [Google Scholar]
- 9.Tan M, Wang H, Wang Y, Zhang G, Yi P, Li Z, Wei H, Yang F. Morphometric evaluation of screw fixation in atlas via posterior arch and lateral mass. Spine. 2003;28:888–895. doi: 10.1097/00007632-200305010-00010. [DOI] [PubMed] [Google Scholar]
- 10.Roy-Camille R, Bouchet TH, Saillant G (1984) Fractures des predicles d l’axi.Journees d’orthopedie a la Pitie. Masson, Paris, pp 119–134
- 11.Igarashi T, Kikuchi S, Sato K, kayama S, Otani K (2003) Anatomic study of the axis for surgical planning of transarticular screw fixation. Clin Orthop Relat Res (408):162–166. doi:10.1097/01.bl0.0000048136.30533.4f [DOI] [PubMed]
- 12.Gorek J, Acaroglu E, Berven S, Yousef A, Puttlitz CM. Constructs incorporating intralaminar C2 screws provide rigid stability for atlantoaxial fixation. Spine. 2005;30:1513–1518. doi: 10.1097/01.brs.0000167827.84020.49. [DOI] [PubMed] [Google Scholar]
- 13.Lapsiwala SB, Anderson PA, Oza A, Resnick DK. Biomechanical comparison of four C1 to C2 rigid fixative techniques: anterior transarticular, posterior transarticular, C1 to C2 pedicle, and C1 to C2 intralaminar screws. Neurosurgery. 2006;58:516–521. doi: 10.1227/01.NEU.0000197222.05299.31. [DOI] [PubMed] [Google Scholar]
- 14.Cassinelli EH, Lee M, Skalak A, Ahn UN, Wright NM. Anatomic considerations for the placement of C2 laminar screws. Spine. 2006;31:2767–2771. doi: 10.1097/01.brs.0000245869.85276.f4. [DOI] [PubMed] [Google Scholar]
- 15.Wang MY. Cervical crossing laminar screws: early clinical results and complications. Neurosurgery. 2007;61:311–316. doi: 10.1227/01.neu.0000303987.49870.7b. [DOI] [PubMed] [Google Scholar]
- 16.Matsubara T, Mizutani J, Fukuoka M, Hatoh T, Kojima H, Otsuka T. Safe atlantoaxial fixation using a laminar screw (intralaminar screw) in a patient with unilateral occlusion of vertebral artery: case report. Spine. 2007;32:E30–E33. doi: 10.1097/01.brs.0000250994.24462.ec. [DOI] [PubMed] [Google Scholar]