Abstract
Odontoid fractures currently account for 9–15% of all adult cervical spine fractures, with type II fractures accounting for the majority of these injuries. Despite recent advances in internal fixation techniques, the management of type II fractures still remains controversial with advocates still supporting non-rigid immobilization as the definitive treatment of these injuries. At the NSIU, over an 11-year period between 1 July 1996 and 30 June 2006, 66 patients (n = 66) were treated by external immobilization for type II odontoid fractures. The medical records, radiographs and CT scans of all patients identified were reviewed. Clinical follow-up evaluation was performed using the Cervical Spine Outcomes Questionnaire (CSOQ). The objectives of this study were to evaluate the long-term functional outcome of patients suffering isolated type II odontoid fractures managed non-operatively and to correlate patient age and device type with clinical and functional outcome. Of the 66 patients, there were 42 males and 24 females (M:F = 1.75:1) managed non-operatively for type II odontoid fractures. The mean follow-up time was 66 months. Advancing age was highly correlated with poorer long-term functional outcomes when assessing neck pain (r = 0.19, P = 0.1219), shoulder and arm pain (r = 0.41, P = 0.0007), physical symptoms (r = 0.25, P = 0.472), functional disability (r = 0.24, P = 0.0476) and psychological distress (r = 0.41, P = 0.0007). Patients >65 years displayed a higher rate of pseudoarthrosis (21.43 vs. 1.92%) and established non-union (7.14 vs. 0%) than patients <65 years. The non-operative management of type II odontoid fractures is an effective and satisfactory method of treating type II odontoid fractures, particularly those of a stable nature. However, patients of advancing age have been demonstrated to have significantly poorer functional outcomes in the long term. This may be linked to higher rates of non-union.
Keywords: Cervical spine, Odontoid fracture, Non-operative, Functional outcome
Introduction
Odontoid fractures currently account for 9–15% of all adult cervical spine fractures [1–4], with type II fractures accounting for the vast majority of these injuries. The mechanism of injury is usually a traumatic hyperextension or hyperflexion of the cervical spine. Fortunately, the prevalence of associated neurologic injury is low, ranging from 2 to 27%. Neurologic injury, if present, usually results in catastrophic or fatal consequences due to the high level of spinal cord involved. Concomitant spinal injuries are present in up to 34% of patients; 85% occurring in the cervical spine, with the atlas most commonly affected [5–8]. The number of associated injuries is significantly more common in younger patients.
Although odontoid fractures occur in all age groups, there are two peaks in incidence with differing associated injury etiologies [8]. The younger patient cohort (17–30 years) usually sustains these injuries secondary to high energy trauma, most commonly road traffic accidents (RTA). The elderly patient cohort (>70 years) most commonly receive these injuries in low energy trauma such as falls from a standing height.
Despite recent advances in internal fixation techniques, the management of type II fractures still remains controversial with advocates still supporting non-rigid immobilization as the definitive treatment of these injuries. The aim of our study was to evaluate the long-term functional outcome of patients suffering isolated type II odontoid fractures managed non-operatively and to correlate patient age and device type with clinical and functional outcome.
Patients and methods
Sixty-six patients (n = 66) were treated by external immobilization for type II odontoid fractures at our institution over an 11-year period between 1 July 1996 and 30 June 2006. Both the Hospital Inpatient Enquiry (HIPE) System and the NSIU database were used to identify our study cohort. Exclusion criteria included neurological injury and concomitant spinal fractures.
The medical records, radiographs and CT scans of all patients identified were reviewed. Odontoid fractures were classified as type II according to the Anderson and d’Alonzo classification system [9]. Diagnosis was established radiographically and agreed by a team of five consultant spinal surgeons using standard antero-posterior, lateral and open-mouth radiographs, and lateral flexion/extension views. Radiological investigation was performed immediately on admission to hospital. Flexion/extension views were performed within 24 h of admission as guided by the consulting physician. Computed tomography (CT) was used to confirm the diagnosis when necessary.
The stability and the status of fracture healing was determined radiographically on follow-up using specific criteria for osseous union, which included evidence of trabeculation across the fracture site and absence of movement of the odontoid on lateral flexion–extension views. When necessary, CT was used to confirm fracture union. Bony union was classified according to a three-point scale: solid fusion (i.e., definitely healed with bone trabeculae bridging the fracture site), stable pseudoarthrosis (i.e., not healed, bone trabeculae could not be seen bridging the fracture site, but with no signs of mechanical failure) and established non-union (i.e., persistent instability, the fracture line still visible or a radiolucent zone across the fracture site).
The National Spinal Injuries Unit (NSIU) is the tertiary referral center for all spinal injuries and diseases of the spine warranting surgical intervention in the Republic of Ireland. Treatment options at the NSIU for type II odontoid fractures include traction followed by immobilization with a non-rigid cervical orthosis (i.e., cervical collar, Miami J) for undisplaced fractures and rigid immobilization with a halo device or custom-made cervical orthosis (i.e., Minerva PoP) for minimally displaced fractures. The type of rigid immobilization used (i.e., Halo device or Minerva POP) was based on a combination of factors, including patient factors (e.g., compliance issues) and surgeon’s preference.
Surgical stabilization (i.e., anterior screw fixation or posterior C1–2 fusion) was performed for unstable fractures and fractures likely resulting in non-union (>4 mm initial displacement, posterior displacement and fracture angulation >10°) for patients unable to tolerate halo immobilization and as a delayed procedure for non-union. During the time period of this study, 9% of patients presenting to the NSIU for management of type II odontoid fractures had surgical stabilization performed as either a primary treatment strategy or as a delayed procedure.
Clinical follow-up evaluation was performed using the Cervical Spine Outcomes Questionnaire (CSOQ). The CSOQ ‘pain severity’, ‘physical symptoms’, ‘functional disability’ and ‘psychological distress’ measures were used to evaluate patient outcome. ‘Pain severity’ is assessed using standardized questions related to neck or shoulder/arm pain. Responses are based on a six-point scale. The ‘physical symptoms’ measures were used to evaluate the presence of symptoms other than pain, such as numbness, clumsiness, weakness or tingling in extremities. ‘Functional disability’ was assessed using questions indicating how much of the patients’ usual activities they were able to perform. Their choices of responses were ‘all’, ‘most’, ‘some’ and ‘none’. CSOQ measures have scales adjusted to range from 0 to 100 with lower scores indicating a more favorable outcome [10].
Age, length of hospitalization and CSOQ outcome measures were represented as mean ± standard deviation. Correlation and linear regression analysis was performed between age and clinical outcome measures, using the Pearson correlation. P values <0.05 were considered to be statistically significant. All data analysis performed and graphs generated utilized the Analyse-it software package in conjunction with Microsoft Excel.
Results
Demographics
There were 66 patients managed non-operatively for type II odontoid fractures at the NSIU over an 11-year period. This cohort was composed of 42 men and 24 women (M:F = 1.75:1). The mean age at the time of injury was 41.92 years (±20.58). The age distribution demonstrated two distinct peaks (Table 1): the first occurring in the third decade, followed by a second peak in the eighth decade.
Table 1.
Age distribution of patient cohort
| Age distribution (years) | Percentage | Patient no. |
|---|---|---|
| <20 | 13.64 | 9/66 |
| 21–30 | 30.30 | 20/66 |
| 31–40 | 12.12 | 8/66 |
| 41–50 | 9.09 | 6/66 |
| 51–60 | 9.09 | 6/66 |
| 61–70 | 9.09 | 6/66 |
| 71–80 | 16.67 | 11/66 |
Mechanism of injury
The mechanism of injury of the type II odontoid fractures suffered by our patient cohort (Table 2) included RTA (66.67%, 44/66) in the vast majority, followed by falls (25.76%, 17/66) and, to a much lesser extent, equestrian injuries (4.55%, 3/66) and assaults (3.03%, 2/66).
Table 2.
Mechanism of injury of patient cohort
| Mechanism of injury | Percentage | Patient no. |
|---|---|---|
| RTA | 66.67 | 44/66 |
| Fall | 25.76 | 17/66 |
| Equestrian | 4.55 | 3/66 |
| Assault | 3.03 | 2/66 |
Associated injuries
Apart from the type II odontoid fractures, associated non-spinal injuries received (Table 3) included head injuries (10.61%, 7/66), chest trauma (6.06%, 4/66), pelvic fractures (1.52%, 1/66) and extremity fractures (15.15%, 10/66).
Table 3.
Associated injuries of patient cohort
| Associated injuries | Percentage | Patient no. |
|---|---|---|
| Head injury | 10.61 | 7/66 |
| Chest trauma | 6.06 | 4/66 |
| Pelvic fracture | 1.52 | 1/66 |
| Extremity fracture | 15.15 | 10/66 |
Length of stay
The mean duration of hospitalization was 11 days (±15 days). The shortest mean hospitalization was for the cervical orthosis group (4.5 days ± 4.81 days), followed by the custom-made cervical orthosis group (6.9 days ± 5.39 days), and finally the halo device group (13.2 ± 17.87 days). There was not a statistically significant association between age and length of hospitalization (r = 0.04, 95% CI −0.20 to 0.28, P = 0.75).
Management
Non-operative management divided our patient cohort into three separate treatment groups based on the type of device used. The treatment groups included cervical orthosis (9.09%, 6/66 patients), custom-made cervical orthosis (24.24%, 16/66 patients), and halo device (66.67%, 44/66 patients) (Table 4).
Table 4.
Orthopaedic management of patient cohort
| Management | Percentage | Patient no. |
|---|---|---|
| Halo device | 66.67 | 44/66 |
| Custom-made cervical orthosis | 24.24 | 16/66 |
| Cervical orthosis | 9.09 | 6/66 |
Of the primary treatments, 9.09% (6/66) failed and required subsequent use of an alternative treatment strategy; 5/6 were managed with an alternative non-operative device and all five cases were initially managed with a Minerva POP and subsequently converted to halo immobilization due to poor compliance. In one case, initial treatment with custom-made cervical orthosis required subsequent surgical stabilization (C1–C2) was performed due to persistent instability.
Radiographic follow-up evaluation
In 92.42% (61/66 patients), fracture healing was uneventful (Table 5). These patients developed a solid bony union and their treatment was discontinued at 3 months (12 weeks); 6.06% (4/66 patients) developed a stable pseudoarthrosis, where there was insufficient evidence of bony fusion in the absence of mechanical failure. All four patients were >65 years of age and 1.52% (1/66 patients) developed a non-union, with persistent instability.
Table 5.
Radiographic outcome of patient cohort
| Radiographic fracture outcome | Percentage | Patient no. |
|---|---|---|
| Solid fusion | 92.42 | 61/66 |
| Stable pseudoarthrosis | 6.06 | 4/66 |
| Established non-union | 1.52 | 1/66 |
The patient who developed a non-union was a 65-year-old gentleman who sustained a fall and was initially managed in a custom-made cervical orthosis and subsequently treated operatively with a C1/2 fusion.
When the patient cohort was broken into two groups based on age (i.e., <65 and >65 years) and radiographic fusion rates were assessed, patients >65 years (n = 14) displayed a higher rate of pseudoarthrosis (21.43%, 3/14) and established non-union (7.14%, 1/14) than patients <65 years (n = 52) (1.92%, 1/52; 0%, 0/52).
Clinical follow-up evaluation
Clinical follow-up evaluation was performed using the CSOQ. The mean time to follow-up was 66 months (±36 months). Follow-up evaluation assessed ‘pain’, ‘physical symptoms’, ‘functional disability’, ‘psychological distress’ and ‘health-care utilization’ as outlined on the CSOQ (Table 6).
Table 6.
Clinical outcome of patient cohort
| CSOQ scores | Mean ± SD |
|---|---|
| Neck pain | 24.67 ± 19.25 |
| Shoulder and arm pain | 17.58 ± 21.07 |
| Physical symptoms | 21.76 ± 23.04 |
| Functional disability | 21.46 ± 22.60 |
| Psychological distress | 24.83 ± 23.19 |
Neck pain
On follow-up evaluation of our non-operative cohort (n = 66), the mean CSOQ score for neck pain (out of 100) was 24.67 (±19.25). When analyzing the severity of neck pain-based form of treatment, the cervical orthosis group (n = 6) had the best outcome with a mean score of 21.91 (±11.94), followed by the halo device group (n = 44) with a mean score of 23.70 (±20.57) and finally the custom-made cervical orthosis group (n = 16) with a mean score of 28.39 (±17.99).
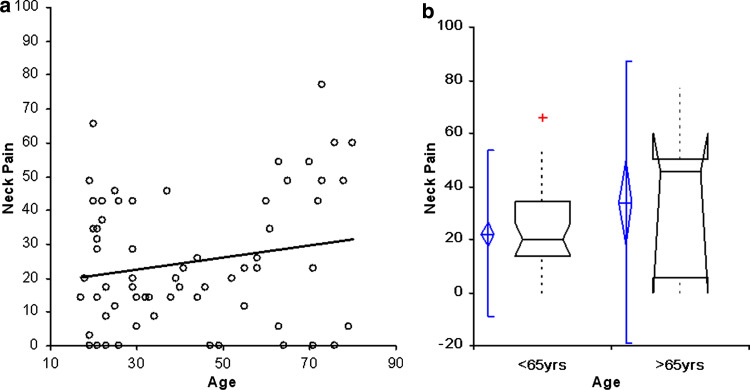
The severity of neck pain was found to be positively correlated with advancing age (Fig. 1a), although the association was found to be outside the range of statistical significance (r = 0.19, 95% CI −0.05 to 0.42, P = 0.1219). When the patient cohort was broken into two groups based on age (i.e., <65 and >65 years) and severity of neck pain assessed (Fig. 1b), patients >65 years (n = 14) displayed a greater mean score (33.88 ± 27.08) and poorer outcome than those <65 years (n = 52) (22.20 ± 15.99).
Fig. 1.
a Pearson correlation representing the association between advancing age and severity of neck pain. Severity of neck pain was positively correlated with advancing age, although the association was found to be outside the range of statistical significance (r = 0.19, 95% CI −0.05 to 0.42, P = 0.1219). b Comparative analysis of neck pain with box plots representing patients aged <65 and ≥65 years. Patients >65 years displayed a greater mean score (33.88 ± 27.08) and poorer outcome than those <65 years (22.20 ± 15.99)
Shoulder and arm pain
On follow-up, the mean CSOQ score for shoulder and arm pain (out of 100) was 17.58 (±21.07). Patients managed with cervical orthosis had a best outcome with the lowest mean pain severity (5.24 ± 8.56), followed by halo device (18.05 ± 22.09) and finally custom-made cervical orthosis (20.89 ± 20.67).
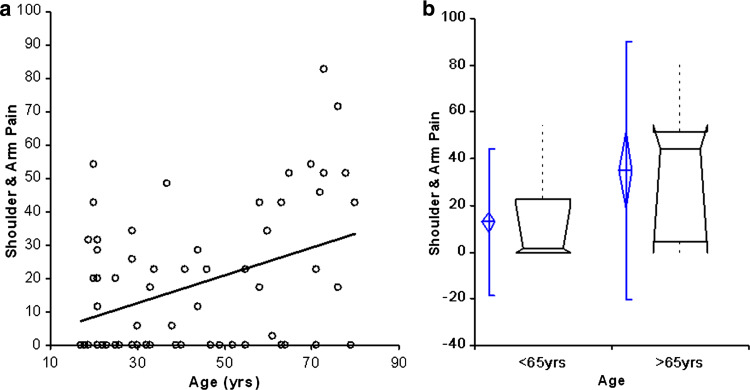
The severity of shoulder and arm pain positively correlated with advancing age (Fig. 2a), with a statistically significant association established (r = 0.41, 95% CI 0.18 to 0.59, P = 0.0007). Breaking the patient cohort into two groups based on age (Fig. 2b), patients >65 years (n = 14) had a poorer outcome and higher mean pain score (35.10 ± 28.20) than patients <65 years (n = 52) (12.86 ± 16.00).
Fig. 2.
a Pearson correlation representing the association between advancing age and severity of shoulder and arm pain. The severity of shoulder and arm pain was positively correlated with advancing age (r = 0.41, 95% CI 0.18–0.59, P = 0.0007). b Comparative analysis of shoulder and arm pain with box plots representing patients aged <65 and ≥65 years. Patients >65 years had a poorer outcome and higher mean pain score (35.10 ± 28.20) than patients <65 years (12.86 ± 16.00)
Physical symptoms
On follow-up evaluation of our non-operative cohort, the mean CSOQ score for physical symptoms (out of 100) was 21.76 (±23.04). Patients managed with cervical orthosis had the best outcome with the lowest mean score (16.00 ± 17.34), followed by custom-made cervical orthosis (20.75 ± 19.33) and finally halo device (22.91 ± 25.11).
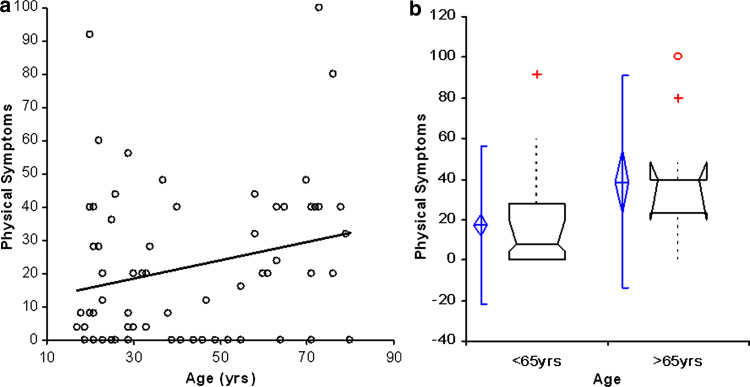
The severity of physical symptoms was positively correlated with advancing age (Fig. 3a), with a statistically significant association (r = 0.25, 95% CI 0.00 to 0.46, P = 0.0472). When we looked at patients <65 and >65 years and compared physical symptoms (Fig. 3b), we found that patients >65 years (n = 14) had a poorer outcome with higher mean score (38.57 ± 26.75) than those <65 years (n = 52) (17.23 ± 19.89).
Fig. 3.
a Pearson correlation representing the association between advancing age and physical symptoms. The severity of physical symptoms was positively correlated with advancing age, with a statistically significant association (r = 0.25, 95% CI 0.00–0.46, P = 0.0472). b Comparative analysis of physical symptoms with box plots representing patients aged <65 and ≥65 years. Patients >65 years had a poorer outcome with higher mean score (38.57 ± 26.75) than those <65 years (17.23 ± 19.89)
Functional disability
On follow-up evaluation of our non-operative cohort, the mean CSOQ score for functional disability (out of 100) for was 21.46 (±22.60). Patients managed with halo device had the best outcome with the lowest mean score (18.75 ± 22.74), followed by custom-made cervical orthosis (26.56 ± 18.81) and finally cervical orthosis (27.78 ± 30.58).
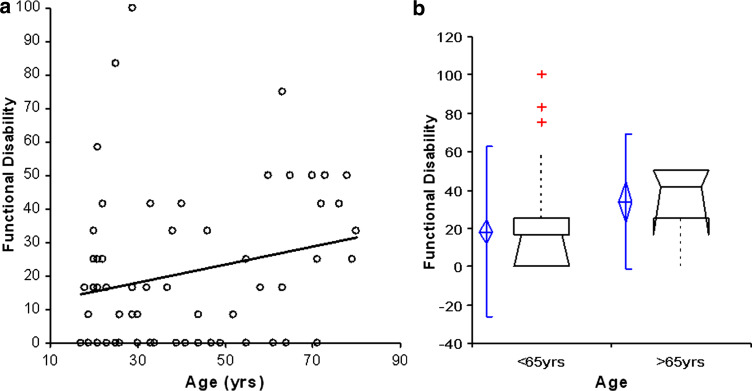
The severity of functional disability was positively correlated with advancing age (Fig. 4a), with a statistically significant association (r = 0.24, 95% CI 0.00 to 0.46, P = 0.0476). Patients >65 years (n = 14) were found to have greater functional disability and higher mean score (33.93 ± 18.04) when compared to patients <65 years (n = 52) (18.11 ± 22.67) (Fig. 4b).
Fig. 4.
a Pearson correlation representing the association between advancing age and functional disability. The severity of functional disability was positively correlated with advancing age (r = 0.24, 95% CI 0.00–0.46, P = 0.0476). b Comparative analysis of functional disability with box plots representing patients aged <65 and ≥65 years. Patients >65 years were found to have greater functional disability and higher mean score (33.93 ± 18.04) when compared to patients <65 years (18.11 ± 22.67)
Psychological distress
On follow-up evaluation of our non-operative cohort, the mean CSOQ score for psychological distress (out of 100) was 24.83 (±23.19). Patients treated using cervical orthosis had the best functional outcome and lowest mean score (8.33 ± 10.39), followed by custom-made cervical orthosis (26.04 ± 20.86) and finally halo device (26.64 ± 24.63).
The severity of psychological distress correlated positively with advancing age, with a statistically significant association (r = 0.41, 95% CI 0.19 to 0.59, P = 0.0007). Patients >65 years (n = 14) were found to suffer the greatest psychological distress with a higher mean score (45.24 ± 24.64) than those <65 years (n = 52) (19.34 ± 16.63).
Discussion
Our patient cohort had a mean age of 41.92 years which was slightly younger than the mean age of 59.1 years observed by Müller et al. [11], who retrospectively analyzed 26 cases of stable type II and type III odontoid fractures managed with non-rigid immobilization. Additionally, our patient cohort had a stronger male predominance with male:female ratio of 1.75:1, which was higher than the 1:1 ratio usually observed [11].
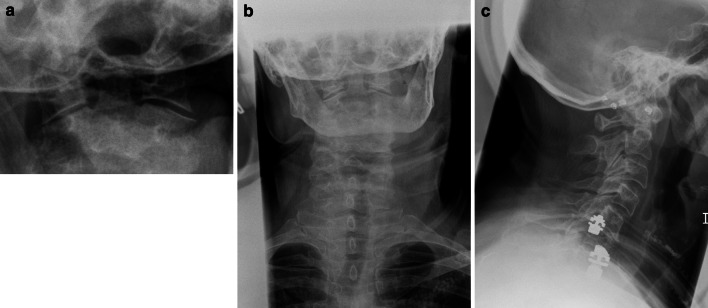
The treatment of odontoid fractures is determined by multiple factors, including fracture type, presence of associated injuries, patient age and comorbidities [4, 8, 12]. It is generally widely accepted that type I and type II injuries can be managed satisfactorily with non-operative treatment. However, for type II fractures (Fig. 5a–c) there are no standard treatment guidelines, only a variety of operative and non-operative options.
Fig. 5.
a Odontoid view b anteroposterior and c lateral cervical spine radiographs of a fracture of the base of the odontoid peg with slight forward subluxation of C1 on C2. This is the case of a 65-year-old lady involved in a road traffic accident sustaining a type II odontoid fracture treated with a halo device
Assessing the integrity of the transverse atlantal ligament in patients with odontoid fractures is an important consideration in selecting the appropriate treatment option. Transverse atlantal ligament disruption occurs in approximately 10% of cases. Injuries of this ligament can result in atlantoaxial instability after odontoid fracture osseous healing, and the chance of odontoid fracture non-union is increased with its disruption. In this situation, early surgical stabilization to avoid delayed instability and non-union is recommended. Furthermore, anterior odontoid screw fixation will not provide C1–C2 stability if the transverse atlantal ligament is not competent.
For the non-operative management of odontoid fractures, use of halo devices has been the method of choice, with high documented success rates. However, the number of complications associated with this form of treatment is high [13–16]. When we evaluated the role of device type on long-term functional outcome, we found that use of cervical orthosis devices, such as cervical collars, had superior outcome results with regard to neck pain, shoulder and arm pain, physical symptoms and psychological distress. This is probably not surprising as the type of injuries managed using non-rigid immobilization are more stable and more likely to heal without complications. Interestingly, when we looked at the outcome scores of the two forms of rigid immobilization, we found that halo device had superior outcome scores compared to custom-made cervical orthosis when looking at neck pain, shoulder and arm pain, and functional disability. However, the halo device had poorer outcome scores compared to custom-made cervical orthosis when taking physical symptoms and psychological distress into consideration.
Odontoid fractures are the most common individual cervical spine fracture for persons ≥70 years and are the most common of all spinal fractures for persons aged ≥80 years [17].
To delineate the role played by advancing age on long-term functional outcome, we performed correlation and linear regression analysis between age and outcome scores. We found that severity of neck pain was positively correlated with advancing age, although this was outside statistical significance. Statistically significant associations were found between advancing age and severity of shoulder and arm pain, physical symptoms, functional disability and psychological distress, clearly demonstrating a strong association between age and long-term functional outcome.
The radiographic results of our patient cohort displayed that patients >65 years had a higher rate of pseudoarthrosis/non-union than those <65 years. This could certainly contribute to poorer functional outcomes in the >65 years group. Patient age as a risk factor for non-union in halo immobilization has been previously examined [7, 18, 19]. Some have suggested that age is not an important factor with regard to outcome, although patients >60 years of age with a dens fracture have a higher complication rate and lower cervical range of motion when treated with a halo. According to Müller et al. [7], this high complication rate is primarily accounted for by loss of reduction and non-union after non-operative treatment, a complicated post-operative course and complications due to associated injuries [7]. In a second study by Müller et al. [11], in spite of demonstrating that elderly patients had a higher rate of pseudoarthrosis, it was concluded that in a stable situation there is no need for internal fixation in the elderly, further supporting our findings.
Conclusion
Despite the high incidence of type II odontoid fractures, much debate still exists regarding the optimum management of these injuries. With no treatment standards currently available to guide physicians in the management of type II odontoid fractures, our group has found the non-operative management of type II odontoid fractures to be an effective and satisfactory way to treat these injuries, particularly those of a stable nature.
Patients of advancing age have been clearly demonstrated to have a significantly poorer functional outcome in the long term. Elderly patients with odontoid fractures should be considered a high-risk group with a high associated morbidity and mortality rate. We would suggest that an aggressive diagnostic approach should be adopted to detect unstable fractures and early primary internal stabilization of these fractures should be considered in favorable selected cases. Clinicians managing these fractures conservatively in the elderly should have patients adequately counseled prior to treatment regarding long-term functional outcome.
References
- 1.Lee PC, Chun SY, Leong JC. Experience of posterior surgery in atlanto-axial instability. Spine. 1984;9:231–239. doi: 10.1097/00007632-198404000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Subach BR, Morone MA, Haid RW, Jr, et al. Management of acute odontoid fractures with single-screw anterior fixation. Neurosurgery. 1999;45:812–819. doi: 10.1097/00006123-199910000-00015. [DOI] [PubMed] [Google Scholar]
- 3.Vaccaro AR, Madigan L, Ehrler DM. Contemporary management of adult cervical odontoid fractures. Orthopedics. 2000;23:1109–1113. doi: 10.3928/0147-7447-20001001-11. [DOI] [PubMed] [Google Scholar]
- 4.Maak TG, Grauer JN. The contemporary treatment of odontoid injuries. Spine. 2006;31(11):53–60. doi: 10.1097/01.brs.0000217941.55817.52. [DOI] [PubMed] [Google Scholar]
- 5.Clark CR, White AA., 3rd Fractures of the dens. A multicenter study. J Bone Joint Surg Am. 1985;67(9):1340–1348. [PubMed] [Google Scholar]
- 6.Greene KA, Dickman CA, Marciano FF, et al. Transverse atlantal ligament disruption associated with odontoid fractures. Spine. 1994;19(20):2307–2314. doi: 10.1097/00007632-199410150-00010. [DOI] [PubMed] [Google Scholar]
- 7.Müller EJ, Wick M, Russe O, et al. Management of odontoid fractures in the elderly. Eur Spine J. 1999;8(5):365–369. doi: 10.1007/s005860050188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ochoa G. Surgical management of odontoid fractures. Injury. 2005;36:S-B54–S-B64. doi: 10.1016/j.injury.2005.06.015. [DOI] [PubMed] [Google Scholar]
- 9.Anderson LD, D’Alonzo RT. Fractures of the odontoid process of the axis. J Bone Joint Surg Am. 1974;56(8):1663–1674. [PubMed] [Google Scholar]
- 10.BenDebba M, Heller J, Ducker TB, Eisinger JM. Cervical spine outcomes questionnaire: its development and psychometric properties. Spine. 2002;27(19):2116–2123. doi: 10.1097/00007632-200210010-00007. [DOI] [PubMed] [Google Scholar]
- 11.Müller EJ, Schwinnen I, Fisher K, Wick M, Muhr G. Non-rigid immobilization of odontoid fractures. Eur Spine J. 2003;12:522–525. doi: 10.1007/s00586-003-0531-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sasso RC. C2 dens fractures: treatment options. J Spinal Disord. 2001;14(5):455–463. doi: 10.1097/00002517-200110000-00015. [DOI] [PubMed] [Google Scholar]
- 13.Ekong CEU, Schwartz ML, Tator CH, Rowed DW, Edmonds VE. Odontoid fracture: management with early mobilisation using the halo device. Neurosurgery. 1981;9:631–637. doi: 10.1227/00006123-198112000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Garfin SR, Botte MJ, Waters RL, Nickel VL. Complications in the use of the halo fixation device. J Bone Joint Surg Am. 1986;69:320–325. [PubMed] [Google Scholar]
- 15.Schweigel JF. Management of the fractured odontoid with halo-thoracic bracing. Spine. 1987;12:838–839. doi: 10.1097/00007632-198711000-00002. [DOI] [PubMed] [Google Scholar]
- 16.Lind B, Nordwall A, Sihlbom H. Odontoid fractures treated with halovest. Spine. 1987;12:173–177. doi: 10.1097/00007632-198703000-00014. [DOI] [PubMed] [Google Scholar]
- 17.Ryan MD, Henderson JJ. The epidemiology of fractures and fracture-dislocations of the cervical spine. Injury. 1992;23:38–40. doi: 10.1016/0020-1383(92)90123-A. [DOI] [PubMed] [Google Scholar]
- 18.Seybold EA, Bayley JC. Functional outcome of surgically and conservatively managed dens fractures. Spine. 1998;23(17):1837–1846. doi: 10.1097/00007632-199809010-00006. [DOI] [PubMed] [Google Scholar]
- 19.Bednar DA, Parikh J, Hummel J. Management of type II odontoid process fractures in geriatric patients: a prospective study of sequential cohorts with attention to survivorship. J Spinal Disord. 1995;8(2):166–169. doi: 10.1097/00002517-199504000-00013. [DOI] [PubMed] [Google Scholar]