Abstract
Minimally invasive lumbar fusion techniques have only recently been developed. The goals of these procedures are to reduce approach-related soft tissue injury, postoperative pain and disability while allowing the surgery to be conducted in an effective manner. There have been no prospective clinical reports published on the comparison of one-level transforaminal lumbar interbody fusion in low-grade spondylolisthesis performed with an independent blade retractor system or a traditional open approach. A prospective clinical study of 85 consecutive cases of degenerative and isthmic lower grade spondylolisthesis treated by minimally invasive transforaminal lumbar interbody fusion (MiTLIF) or open transforaminal lumbar interbody fusion (OTLIF) was done. A total of 85 patients suffering from degenerative spondylolisthesis (n = 46) and isthmic spondylolisthesis (n = 39) underwent one-level MiTLIF (n = 42) and OTLIF (n = 43) by two experienced surgeons at one hospital, from June 2006 to March 2008 (minimum 13-month follow-up). The following data were compared between the two groups: the clinical and radiographic results, operative time, blood loss, transfusion needs, X-ray exposure time, postoperative back pain, length of hospital stay, and complications. Clinical outcome was assessed using the visual analog scale (VAS) and the Oswestry disability index. The operative time, clinical and radiographic results were basically identical in both groups. Comparing with the OTLIF group, the MiTLIF group had significantly lesser blood loss, lesser need for transfusion, lesser postoperative back pain, and shorter length of hospital stay. The radiation time was significantly longer in MiTLIF group. One case of nonunion was observed from each group. Minimally invasive TLIF has similar surgical efficacy with the traditional open TLIF in treating one-level lower grade degenerative or isthmic spondylolisthesis. The minimally invasive technique offers several potential advantages including smaller incisions, less tissue trauma and quicker recovery. However, this technique needs longer X-ray exposure time.
Keywords: Comparison, Minimally invasive surgery, Transforaminal lumbar interbody fusion, Isthmic and degenerative spondylolisthesis
Introduction
In 1940, the first successful posterior lumbar interbody fusion (PLIF) was performed using a shaped spinous process autograft [1]. In 1951, Cloward [2] reported satisfactory results in more than 85% of 331 patients using this technique. In addition, because of the moderately high pseudoarthrosis rate encountered with using stand-alone grafts, it has become common to augment the PLIF technique with pedicle screws [3]. Transforaminal lumbar interbody fusion (TLIF) was popularized by Harms et al. [4] as an alternative to PLIF. TLIF offers several advantages including decreased retraction of the dural sac, lessening the risk of postoperative radiculitis [5].
Irrespective of the exact method of arthrodesis, conventionally open lumbar surgery performed via a posterior approach is associated with significant soft tissue morbidity that can adversely affect patient outcomes [6–9]. A minimally invasive transforaminal lumbar fusion (MiTLIF) technique has been described to reduce the iatrogenic soft tissue injury that occurs with muscle stripping and retraction during routine spinal exposure [10, 11–14]. Only three studies are currently available comparing MiTLIF to OTLIF [10, 12, 14]. No study to date, however, has compared prospectively the MiTLIF using an independent blade retractor system (Quadrant system, Medtronic Sofamor Danek, Memphis, TN) to the traditional OTLIF.
Materials and methods
Clinical data
From June 2006 to March 2008, 85 consecutive patients with degenerative or isthmic spondylolisthesis were treated with Quadrant retractor system and Sextant system (percutaneous pedicle screw system, Medtronic Sofamor Danek, USA), with a mean age of 51.7 years. The cases include 46 degenerative spondylolisthesis and 39 isthmic spondylolisthesis: 42 patients underwent single-level MiTLIF by one experienced surgeon; 43 patients received one-level OTLIF by other experienced surgeon at the same hospital. According to random principle, 85 patients were treated by MiTLIF or OTLIF one by one. All of patients in both groups presented low back pain as their predominant complaint, with varying degrees of radiating pain, neurological complaints, or a combination of these. All patients had to have been treated conservatively for at least 3 months without success before consideration for surgical intervention. The patients’ demographic characteristic and procedure data of these comparison groups are listed in Table 1.
Table 1.
Patient demographic data
| MiTLIF group | OTLIF group | |
|---|---|---|
| No. of patients | 42 | 43 |
| Mean age (years) | 47.9 ± 8.5 | 53.2 ± 10.6 |
| Gender (M/F) (% male) | 13/29 (30.1) | 16/27 (37.2) |
| Preoperative diagnosis [no. (%) of patients] | ||
| Degenerative spondylolisthesis | 24 (57.1) | 22 (51.2) |
| Isthmic spondylolisthesis | 18 (42.9) | 21 (48.8) |
| Level of fusion [no. (%) of patients] | ||
| L3–L4 | 3 (7.1) | 3 (6.9) |
| L4–L5 | 21 (50) | 23 (53.5) |
| L5–S1 | 18 (42.9) | 17 (39.5) |
Surgical techniques
Minimally invasive TLIF
After induction of general anesthesia, patients were positioned prone on a radiolucent frame. A 3 cm longitudinal incision was made for placement of Quadrant retractor system. A complete facetectomy was performed and the lateral border of the dura was identified. After identification of the traversing and exiting nerve roots, an aggressive full discectomy was then performed in the Kambin’s triangle [15]. Interbody distractors were introduced in the disc space. Sufficient autologous bone graft obtained from the removed facet was packed in the anterior disc space. A single PEEK cage (OIC, Stryker Inc. USA) was inserted obliquely across the disc space. If disc space was too narrow, an appropriately sized distractor was placed on one side first to maintain the height of disc space. Disc preparation and cage insertion were then performed on the contralateral side. To avoid new radiculopathies occurring during reduction, one side facetectomy and simple decompression on another side were performed in all patients. If there was radiculopathy on two sides, the relatively worse radiculopathy side was chosen to receive interbody graft and cage.
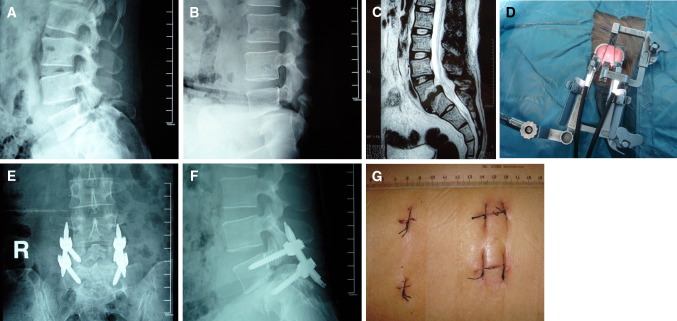
After Quadrant retractor system was removed, pedicle entry point was directly touched through the surgeon’s hand. A modified cannulated needle (used for percutaneous vertebroplasty) was advanced through the pedicle into the vertebral body under fluoroscopic guidance, followed by insertion of a blunt-tipped guidewire into the ventral third of the vertebral body and tapping of the screw path. A representative case is showed in Fig. 1.
Fig. 1.
Lateral (a and b) radiographs of a 38-year-old male with isthmic spondylolisthesis grade 1. The preoperative MRI (c) showed herniated disc and narrow disc space. Quadrant retractor system (d) was placed and attached with the light cables. Anteroposterior (e) and lateral (f) views after MiTLIF and percutaneous pedicle screw fixation showed reduction of the spondylolisthesis and restoration of the disc space height. Small skin incision (g)
Open TLIF
The open TLIF approach was performed as described by Harms et al. [4] using a midline open approach.
Clinical and radiological evaluation
The data collected prospectively for analysis were age, gender, preoperative diagnoses, clinical and radiographic results after surgery, operating time, total amounts of transfusion, X-ray exposure time, postoperative back pain, length of hospital stay and complication. Back pain was quantified by visual analog scores (VAS) collected from the patients preoperatively, postoperatively and in last follow-up. The Oswestry Disability Index (ODI), version 2.0, was used both before surgery and after surgery to give surgeon information about how the patient’s leg (or back) trouble has affected his/her ability to manage in everyday life. The sex question (Section 8) is unacceptable in our culture, and most patients are reluctant to answer this section; therefore, it was omitted in this study. So the total possible score is 45.
Preoperative radiological evaluation included anteroposterior, lateral, oblique, and flexion–extension plain radiograph, CT scans, and magnetic resonance imaging (MRI). Fusion rates were assessed by an independent radiologist using static and dynamic plain X-rays at 6 months. Definitive fusion was identified by formation of trabecular bony bridges between contiguous vertebral bodies at the instrumented levels, and less than 4° segmental movement.
Statistical analysis
Statistical analyses were performed using SPSS 11.0 for windows. Data are shown as mean ± SEM. Student t test was used for the comparison of continuous variables. Fisher’s exact test was used to evaluate the differences of clinical outcomes and fusion rate between the two groups. P values below 0.05 were accepted for significance.
Results
The mean follow-up was 26.3 months with a range of 13–35 months. The preoperative diagnoses and level of fusion showed a similar pattern in both groups. None of the patients in the MiTLIF group needed to be converted to the open surgery. There was no statistical difference in operating time, preoperative and latest back pain VAS, preoperative and latest ODI between the two groups. The statistical evaluation showed a highly significant decrease in the intraoperative and postoperative blood loss as well as total blood transfusion (P < 0.01) with respect to the MiTLIF group. There was significant difference in the X-ray exposure time between both groups with an average of 84 s in the MiTLIF surgery and 37 s in the OTLIF surgery (P < 0.05). MiTLIF group needed significantly shorter hospital stay than OTLIF group (P < 0.05). The patients in MiTLIF group had a lower mean back pain VAS score than the patients in OTLIF group on the third day after surgery (P < 0.05). All these details of clinical data are illustrated in Table 2.
Table 2.
Comparison of clinical data between the MiTLIF and OTLIF groups
| MiTLIF group | OTLIF group | |
|---|---|---|
| Operating time (min) | 156 ± 32 | 145 ± 27 |
| Intraoperative blood loss (ml) | 264 ± 89 ** | 673 ± 145 |
| Postoperative blood loss (ml) | 39 ± 12 ** | 158 ± 65 |
| Total blood transfusion (U) | 0.12 ± 0.3** | 1.47 ± 0.52 |
| X-ray time (s) | 84 ± 21* | 37 ± 19 |
| Hospital stay (days) | 10.6 ± 2.5* | 14.6 ± 3.8 |
| Preoperative back pain VAS | 7.2 ± 2.1 | 7.4 ± 1.6 |
| Back pain VAS at the third day after surgery | 1.34 ± 0.5* | 2.49 ± 0.7 |
| Latest back pain VAS | 0.92 ± 0.5 | 1.1 ± 0.6 |
| Preoperative ODI | 41.2 ± 6.6 | 38.5 ± 7.4 |
| Latest ODI | 10.8 ± 3.3 | 12.2 ± 3.9 |
* P < 0.05; ** P < 0.01
Two patients developed radiculopathies postoperatively in the MiTLIF group: one due to graft dislodgement and the other due to local epidural hematoma. These new radiculopathies resolved with reoperation under METRx microendoscopic system (Medtronic Sofamor Danek, USA) within 1 week. There were two cases of small dural tear during spinal decompression, which were not repaired in MiTLIF group. Postoperative cerebrospinal fluid leakage only lasted 3 or 5 days without any neurological sequelae or wound complication. One patient in OTLIF group had technical complication (one pedicle screw malposition) that needed subsequent revision surgery. The result was good and the new radiculopathy had a full recovery within 1 month. There were two cases of dural tear which were repaired intraoperatively in OTLIF group. Postoperative cerebrospinal fluid leakage stopped within 1 week without clinical sequelae. One case of nonunion was observed from each group. These nonunion cases were determined by more than 4° segmental motion on flexion–extension lateral radiographs. Both patients refused revision surgery because of no obvious complaints of low back pain.
Discussion
The goal of minimally invasive spinal surgery is to achieve the same objectives as the comparable open procedure via a less traumatic approach. Although lessening the approach-related morbidity is a primary aim of minimally invasive spine surgery, this must be accomplished without compromising the efficacy of the procedure. MiTLIF is a relatively new technique attracting increased interest in less invasive surgical fusion techniques [13, 16]. Schwender et al. [11] presented the first clinical series reporting on their initial experience with 49 patients during a 22-month follow-up. In this series of patients they reported two cases of screw malposition, two new radiculopathies, and a 100% fusion rate based on plain radiographs. Only three studies are currently available comparing minimally invasive transforaminal lumbar interbody fusion to traditional surgery [10, 12, 14]. Isaacs et al. recently published their experience treating 20 patients with monosegmental instability of the lumbar spine using microendoscopy-assisted TLIF through a 20-mm working channel. Their results revealed considerable advantages regarding intraoperative blood loss, transfusion rate, and postoperative in-hospital days as compared with a standard open PLIF technique [10]. Scheufler et al. reported their clinical study on percutaneous transforaminal lumbar interbody fusion (pTLIF) for the treatment of degenerative lumbar instability using microscopic illumination and vision through an 18-mm tubular retractor. The operating time was equivalent and the blood loss and postoperative pain reduced compared with open TLIF [12]. Schizas et al. presented initial experience on comparative study between minimally invasive versus classical midline open TLIF through a tubular retractor. The minimally invasive TLIF group resulted in a significant reduction of blood loss and had a shorter length of hospital stay [14].
The results from our study compare well with those reported by the aforementioned studies as we also found a significant difference in blood loss and length of hospital stay between the two groups. In contrast to the study presented by Schizas et al. [14], however, our MiTLIF group had less postoperative back pain at the third day after surgery than OTLIF group. Kim et al. [17] showed that percutaneous versus open internal stabilization is associated with less multifidus muscle atrophy, superior postoperative trunk muscle strength, lower blood loss and less postoperative demand for analgesics. The main advantage with less muscular trauma seems to be within the immediate postoperative period, where a significant reduction in pain is conspicuous [18]. The patients in the MiTLIF group had significantly shorter hospitalization partly because of less postoperative pain in the early stage after surgery. Minimally invasive spinal fusion using the MiTLIF technique is efficacious and safe. However, the need for intraoperative fluoroscopy poses disadvantages. Our study indeed found longer X-ray exposure times in the MiTLIF group. At this point the surgeons’ experience in minimally invasive surgery should not be neglected. Our study found no significant difference in operating time between both groups.
Ozgur et al. found that the minimally invasive TLIF technique using independent blade retractor provides comparable exposure to the traditional open surgery with the benefits of minimally invasive techniques. Additionally, it overcomes the obstacles of working through a tube [13]. In our country, most of the spinal surgeons have no experience on manipulation of operative microscope and endoscope. The Quadrant retractor system is designed to maximize surgical access while minimizing disruption of musculature. It enables the use of standard instruments to perform conventional surgery and allows direct visualization without the requirement of special equipment such as microscope and endoscope.
Due to less tissue trauma and structure damage, MiTLIF may reduce the amount of iatrogenic injury while still safely accomplishing the goals of the conventional open TLIF. Prophylactic neural decompression for the cases without neurological symptoms may increase risk of injury to neural elements and prolong operative time; however, it avoids new radiculopathy occurring during reduction of spondylolisthesis especially in grade 2. The reduction screw holding sleeve is designed to reduce spondylolisthesis which was confirmed to be efficient in our series.
Acknowledgments
No funds were received in support of this work. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
Footnotes
The device(s)/drug(s) is/are FDA-approved or approved by corresponding national agency for this indication.
References
- 1.Cloward RB. History of PLIF: forty years of personal experience. In: Lin PM, editor. Posterior lumbar interbody fusion. Springfield: Charles C. Thomas; 1982. pp. 58–71. [Google Scholar]
- 2.Cloward RB. The treatment of ruptured intervertebral discs by vertebral body fusion: Part I—indications, operative technique, after care. J Neurosurg. 1953;10:154–168. doi: 10.3171/jns.1953.10.2.0154. [DOI] [PubMed] [Google Scholar]
- 3.Steffee AD, Sitkowski DJ. Posterior lumbar interbody fusion and plates. Clin Orthop Relat Res. 1988;227:99–102. [PubMed] [Google Scholar]
- 4.Harms JG, Jeszenszky D. The unilateral transforaminal approach for posterior lumbar interbody fusion. Orthop Traumatol. 1998;6:88–89. [Google Scholar]
- 5.Humphreys SC, Hodges SD, Patwardhan AG, et al. Comparison of posterior and transforaminal approaches to lumbar interbody fusion. Spine. 2001;26:567–571. doi: 10.1097/00007632-200103010-00023. [DOI] [PubMed] [Google Scholar]
- 6.Kawaguchi Y, Matsui H, Tsuji H. Back muscle injury after posterior lumbar spine surgery. A histologic and enzymatic analysis. Spine. 1996;21:941–944. doi: 10.1097/00007632-199604150-00007. [DOI] [PubMed] [Google Scholar]
- 7.Kawaguchi Y, Matsui H, Tsuji H. Back muscle injury after posterior lumbar spine surgery. Part 2: histologic and histochemical analyses in humans. Spine. 1994;19:2598–2602. doi: 10.1097/00007632-199411001-00018. [DOI] [PubMed] [Google Scholar]
- 8.Sihvonen T, Herno A, Paljiarvi L, et al. Local denervation atrophy of paraspinal muscles in postoperative failed back syndrome. Spine. 1993;18:575–581. doi: 10.1097/00007632-199304000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Styf JR, Willen J. The effects of external compression by three different retractors on pressure in the erector spine muscles during and after posterior lumbar spine surgery in humans. Spine. 1998;23:354–358. doi: 10.1097/00007632-199802010-00014. [DOI] [PubMed] [Google Scholar]
- 10.Isaacs RE, Podichetty VK, Santiago P, et al. Minimally invasive microendoscopy-assisted transforaminal lumbar interbody fusion with instrumentation. J Neurosurg Spine. 2005;3:98–105. doi: 10.3171/spi.2005.3.2.0098. [DOI] [PubMed] [Google Scholar]
- 11.Schwender JD, Holly LT, Rouben DP, et al. Minimally invasive transforaminal lumbar interbody fusion (TLIF): technical feasibility and initial results. J Spinal Disord Tech. 2005;18(Suppl):S1–S6. doi: 10.1097/01.bsd.0000132291.50455.d0. [DOI] [PubMed] [Google Scholar]
- 12.Scheufler KM, Dohmen H, Vougioukas VI. Percutaneous transforaminal lumbar interbody fusion for the treatment of degenerative lumbar instability. Neurosurgery. 2007;60:203–212. doi: 10.1227/01.NEU.0000255388.03088.B7. [DOI] [PubMed] [Google Scholar]
- 13.Ozgur BM, Yoo K, Rodriguez G, et al. Minimally invasive technique for transforaminal lumbar interbody fusion (TLIF) Eur Spine J. 2005;14:887–894. doi: 10.1007/s00586-005-0941-3. [DOI] [PubMed] [Google Scholar]
- 14.Schizas C, Tzinieris N, Tsiridis E, et al. Minimally invasive versus open transforaminal lumbar interbody fusion: evaluating initial experience. Int Orthop. 2008;33(6):1683–1688. doi: 10.1007/s00264-008-0687-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kambin P. Arthroscopic microdiscectomy of the lumbar spine. Clin Sports Med. 1993;12:143–150. [PubMed] [Google Scholar]
- 16.Mummaneni PV, Rodts GE., Jr The mini-open transforaminal lumbar interbody fusion. Neurosurgery. 2005;57:256–261. doi: 10.1227/01.NEU.0000176408.95304.F3. [DOI] [PubMed] [Google Scholar]
- 17.Kim DH, Albert TJ. Update on use of instrumentation in lumbar spine disorders. Best Pract Res Clin Rheumatol. 2002;16:123–140. doi: 10.1053/berh.2002.0210. [DOI] [PubMed] [Google Scholar]
- 18.Ringel F, Stoffel M, Stuer C et al (2006) Minimally invasive transmuscular pedicle screw fixation of the thoracic and lumbar spine. Neurosurgery 59(4) Operative Neurosurgery Supplement 2:ONS361–ONS366 [DOI] [PubMed]