Abstract
The purpose of this study was to compare the degree of enlargement of the spinal canal between two methods of cervical laminoplasty (open-door laminoplasty and double-door laminoplasty) and to determine their appropriate surgical indications based on the results. Tension-band laminoplasty (TBL, one method of open-door type) was performed in 33 patients and double-door laminoplasty (DDL) in 20 patients. The operation level ranged from C2 to C7 in all patients. The width of the spinal canal and the inclination angle of the lamina at the C5 and C6 levels were measured using a computer software program (Image J) and pre- and postoperative CT films. Concerning the degree of enlargement of the spinal canal, the mean expansion ratio at the C5 level was 148.9% in TBL and 148.2% in DDL, and there was no significant difference between them. However, at the C6 level, it was 159.0% in TBL and 140.3% in DDL, which was significantly larger in TBL than DDL (p < 0.05). The increase of inclination angle of the lamina was 11.0° in TBL and 19.0° in DDL at the C5 level, and 9.2° in TBL and 19.3° in DDL at the C6 level. At both the C5 and C6 levels, it was significantly larger in DDL than TBL (p < 0.0001). In conclusion, the appropriate surgical indications of TBL were considered to be (1) cervical spondylotic myelopathy (CSM) combined with hemilateral radiculopathy, (2) severe prominence of ossification of the posterior longitudinal ligament (OPLL), and (3) patients with tiny spinous processes who cannot undergo DDL. Those of DDL were considered to be (1) usual CSM, (2) small and slight prominence of OPLL, (3) CSM combined with bilateral radiculopathy, and (4) cervical canal stenosis combined with instability necessitating posterior spinal instrumentation surgery.
Keywords: Cervical laminoplasty, Open-door laminoplasty, Double-door laminoplasty, Spinal canal
Introduction
Compressive cervical myelopathy is caused by various pathognomonic origins such as disc herniation, spondylosis, congenital canal stenosis, ossification of the posterior longitudinal ligament (OPLL), and so on. In Japan, laminectomy has previously been performed as the main surgical method through the posterior approach for cervical myelopathy. However, the postoperative instability and the invasion of scar tissue into the spinal canal have often been recognized as severe complications after laminectomy. These complications were found to considerably relate to exaggeration of neurological conditions after surgery. In 1972, the idea of cervical laminoplasty was first introduced by Oyama and coworkers [1] by the name of “Expansive lamina-Z-plasty” to decrease these complications by preserving the posterior osseous structures of the cervical spine as much as possible. Thereafter, various methods of cervical laminoplasty have been developed in Japan [2–6].
At present, the surgical methods of cervical laminoplasty are broadly divided into two types from the viewpoint of the site of osteotomy: open-door type [2, 3, 6] and double-door type [4, 5]. In the open-door type, osteotomy is performed at one side of the lamina-facet junction. In the double-door type, osteotomy is performed at the central spinous process and lamina. Each method has its own advantages and disadvantages. First of all, the common purpose of both methods is to expand the narrowed spinal canal and afford the opportunity of reactivating the spinal cord. However, the issue of the degree of enlargement of the spinal canal, especially comparison between the two methods, has not been discussed previously.
The purpose of this study was to compare the degree of enlargement of the spinal canal between the two methods and to determine their appropriate surgical indications based on the results.
Subjects
In the first author’s consecutive series since 2002, 53 patients have undergone tension-band laminoplasty [6, 7] (TBL, one method of open-door type) or double-door laminoplasty [5, 7–12] (DDL).
TBL was performed in 33 patients: 22 males and 11 females, 20 with cervical spondylotic myelopathy (CSM) and 13 with OPLL. Ages at the time of operation ranged from 31 to 83 years, with an average of 62.4 years.
DDL was performed in 20 patients with CSM: 17 males and 3 females, ranging in age at the time of operation from 29 to 89 years, with an average of 62.8 years.
The operation level ranged from C2 to C7 in all patients. The follow-up periods ranged from 6 months to 5 years, with an average of 3 years and 4 months.
Methods
The degree of enlargement of the spinal canal is largely influenced by the operated level, especially in TBL, that is, the canal at the C2 and C7 levels cannot be fully opened because of tension of the nuchal ligament or adjacent interspinous ligament. In contrast, the canal at the C5 and C6 levels can consistently be opened despite differences of diseases. Therefore in this series, the degree of enlargement of the spinal canal was examined at only the C5 and C6 levels.
The width of the spinal canal and the inclination angle of the lamina were measured using a commercially available computer software program (Image J: Wayne Rasband (HIH), USA) and pre- and postoperative CT films (Fig. 1).
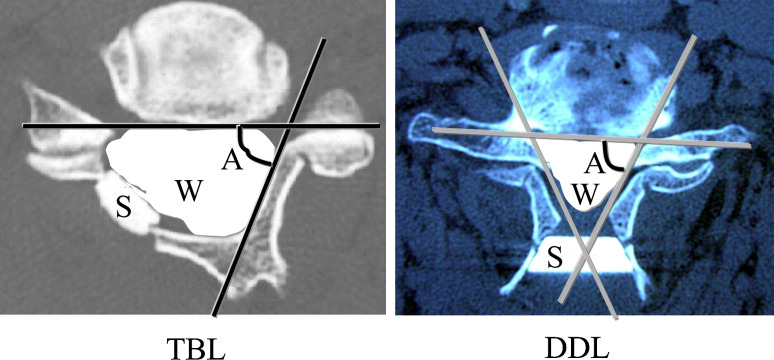
Fig. 1.
The methods of measuring the width of the spinal canal and the inclination angle of the lamina on CT films (left tension-band laminoplasty, TBL right double-door laminoplasty, DDL). W width of the spinal canal, A angle of the lamina, S spacer
The width of the preoperative spinal canal was defined as the region circumscribed by the posterior border of the vertebral body and the inner border of the lamina. That of the postoperative spinal canal was defined as the region circumscribed by the posterior border of the vertebral body, the inner border of the lamina, and the inner border of an artificial spacer. In cases of OPLL, the width of the spinal canal proper, excluding OPLL, was investigated.
The inclination angle of the lamina was defined as the angle made by the two crossed lines of the posterior border of the vertebral body and the inner border of the lamina. The postoperative inclination angle in TBL was defined in the same manner at the hinge side.
The expansion ratio of the spinal canal and the increased inclination angle of the lamina were statistically examined. The statistical analysis was performed using the Wilcoxon method. The significance level was set at p < 0.05.
Surgical methods
The details of the two surgical methods are referenced in other papers [5–7]. The patient is lying prone with the head fixed in slight flexion by a 3-pin skull fixator. The posterior laminae are exposed through a mid-dorsal approach. The postoperative clinical course is almost the same between them. The patient is allowed to walk wearing a soft neck collar after bed rest for a few days. The collar is discarded at the end of 1 month. In this paper, only the essence of the methods of osteotomy and fixation of an artificial spacer are presented.
Tension-band laminoplasty (Fig. 2-left)
Fig. 2.
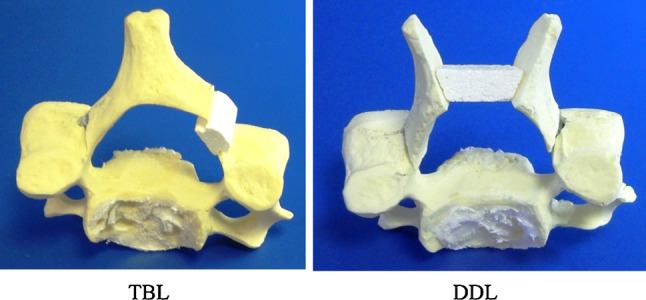
Pictures of a plastic model for presenting the setting of a spacer in TBL and DDL. Views from the cranial side (left TBL, right DDL)
After exposing the operated laminae, a longitudinal groove of 3 mm width is made using an air drill along the lamina-facet junction line at the hinge side of the laminae, leaving the cancellous bone and the inner cortex undisturbed. Then, a similar groove is made at the open side, and finally the inner cortex is severed longitudinally.
Next, the spinous process is pushed by a finger that feels its resistance. During this procedure, the hypertrophied flaval ligament is resected by a Kerrison punch. If hard resistance is felt, the groove in the hinge side is deepened slightly with the air drill. This procedure is repeated until the lamina is opened wide enough to insert a spacer of required width. In our standard method, a spacer of 12 mm in transverse length is fixed at the C5 and C6 levels under good compressive force. After hole-making procedures for thread fixation are completed, a spacer made of hydroxyapatite is fixed using a non-soluble thread at each level.
Double-door laminoplasty (Fig. 2-right)
After exposing the operated laminae, the spinous processes are split centrally in order from the C2 to C7 levels using an air drill. At first, a triangle-shaped dome at the cranial base of the spinous process is made to obtain a good visual field. Next, the tip of the spinous process and inner plate of the lamina are split centrally. Then, a longitudinal groove of 3 mm width is made bilaterally at the lamina-facet junction line taking care not to resect the inner cortex too deeply.
After opening the split spinous processes in a double-door fashion using a scissors, the constricting fibrous band above the dura mater and the hypertrophied flaval ligament are resected. In each split spinous process, the transverse length of the widened space can be observed to be longer at the cranial side than the caudal side. Therefore, the shape of the widened space is trapezoidal both on the axial and frontal sections. Of many types of spacer, the STSS spacer [8–12] (HOYA CORPORATION, Tokyo, Japan) is considered the most useful because both the axial and frontal sections are trapezoidal and well adapted to the widened space. During the fixation to the spinous process, the STSS spacer rotates slightly in the sagittal plane, and as a result, is more firmly stabilized parallel to each spinous process.
A hole to accommodate a thread for fixing the spacer is made at about 8 mm and more superficial from the inner plate of the lamina. The STSS spacer is fixed using a non-soluble thread at each level. The appropriate size of spacer must be selected in accordance with the size of the spinous process. In our standard method, an STSS spacer of 24 mm in cranial transverse length is fixed at the C5 and C6 levels.
Results
The expansion ratio of the spinal canal
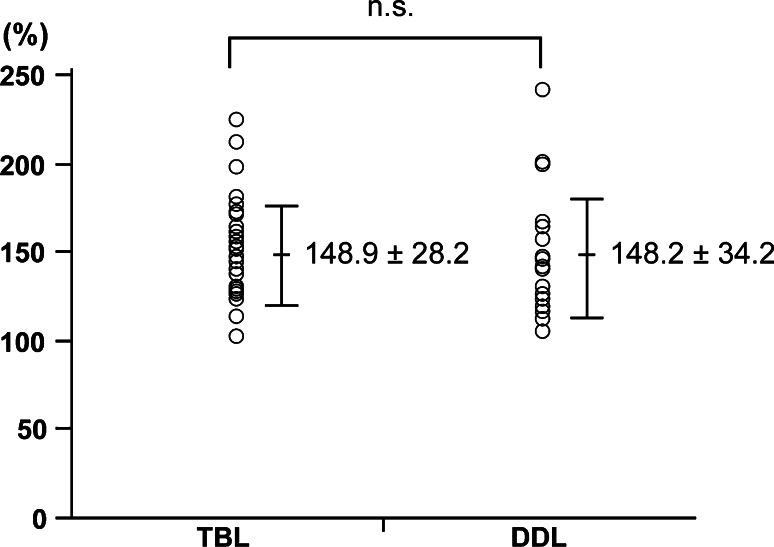
At the C5 level, the mean expansion ratio was 148.9% [standard deviation (SD) 28.2%] in TBL and 148.2% (SD 34.2%) in DDL. There were no significant differences between the two surgical methods (Fig. 3).
Fig. 3.
Expansion ratio of the spinal canal at the C5 level
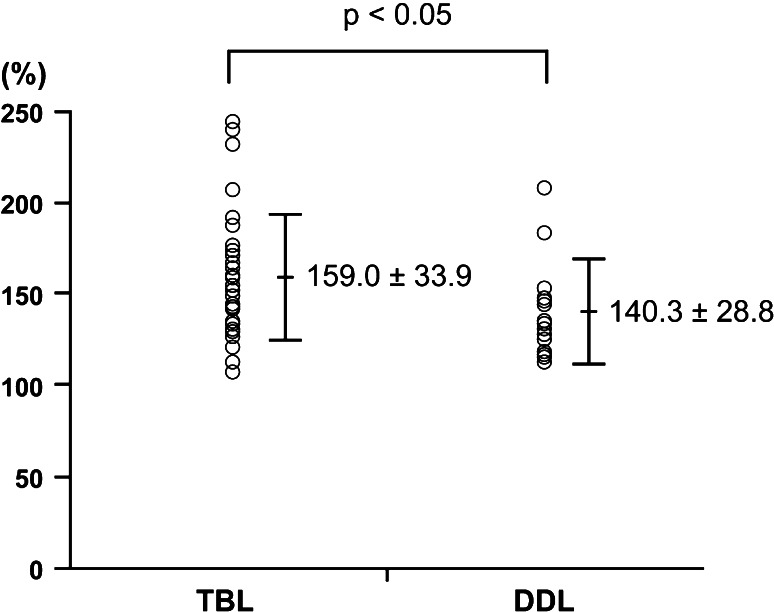
At the C6 level, the mean expansion ratio was 159.0% (SD 33.9%) in TBL and 140.3% (SD 28.8%) in DDL, which was significantly larger in TBL than DDL (p < 0.05) (Fig. 4).
Fig. 4.
Expansion ratio of the spinal canal at the C6 level
The increased inclination angle of the lamina
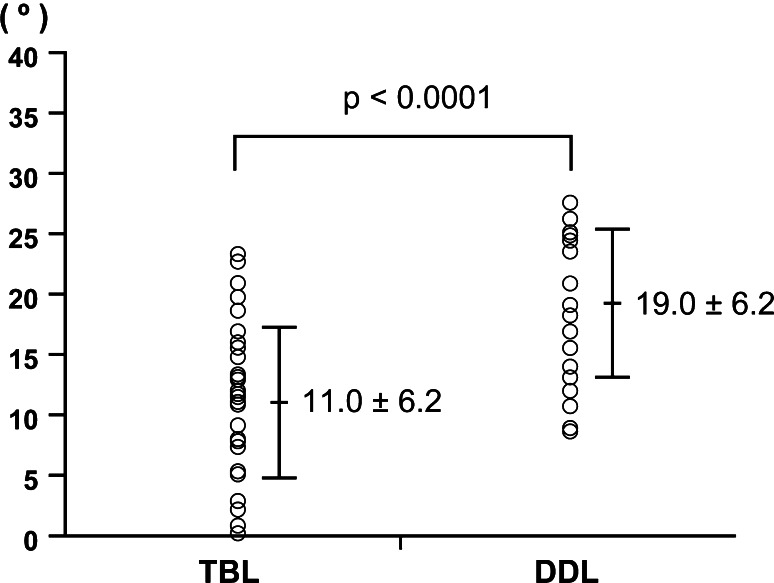
At the C5 level, the mean increase of the inclination angle of the lamina was 11.0° (SD 6.2°) in TBL and 19.0° (SD 6.2°) in DDL (Fig. 5).
Fig. 5.
Increased inclination angle of the C5 lamina
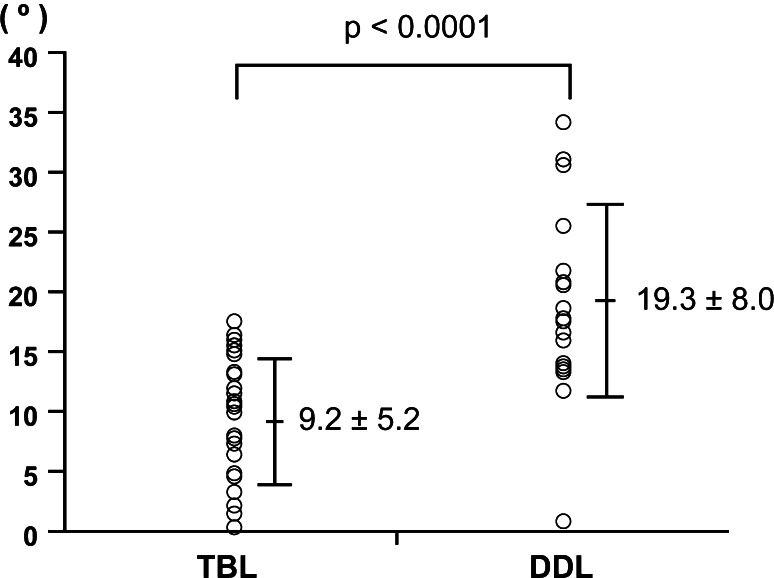
At the C6 level, the mean increase of the inclination angle of the lamina was 9.2° (SD 5.2°) in TBL and 19.3° (SD 8.0°) in DDL (Fig. 6).
Fig. 6.
Increased inclination angle of the C6 lamina
At both C5 and C6 levels, inclination angle was significantly larger in DDL than TBL (p < 0.0001).
Discussion
Respective advantages and disadvantages of TBL and DDL
In TBL [6, 7], the enlargement of the spinal canal depends only on the transverse length of a spacer. In contrast, in DDL, it depends on both the transverse length of the spacer and the depth of spacer fixation. If the same size spacer is used, the deeper it is fixed, the wider the spinal canal becomes. In our standard method, a spacer is fixed at about 8 mm and more superficial from the inner plate of the lamina. In DDL, an appropriate sized spacer can be fixed at the position of an appropriate depth because the split spinous processes are maintained at an adequate length after surgery. The STSS spacer can be stabilized firmly parallel to each spinous process. Therefore, the control of enlargement of the spinal canal is easier in DDL than TBL.
From the technical viewpoint, TBL has the advantage of being an easier decompression procedure than DDL because two longitudinal grooves are made at the bilateral lamina-facet junction line. However, it is slightly difficult in TBL to fix a spacer using a thread between the lamina and the inner edge of the facet joint. Also, the pathological findings at the hinge side cannot be visualized in TBL, and the biggest disadvantage of TBL is that the postoperative posterior skeletal structure of the cervical spine becomes unsymmetrical.
In contrast, DDL [5, 7–12] has the advantages over TBL of easier fixation of spacers and direct visual confirmation of bilateral decompression, and the postoperative posterior skeletal structure of the cervical spine remains symmetrical. However, the procedures of making two longitudinal grooves at the bilateral lamina-facet junction line and one central split just above the dorsal surface of the dura mater must be performed. Also, the central split is slightly difficult to perform in patients with large prominence of OPLL.
Appropriate surgical indications
From the results of this series, the expansion ratio of the spinal canal at the C6 level in TBL was found to be significantly larger than that in DDL. It remains unclear to what minimal extent the spinal canal must be widened in order to obtain good surgical results [13]. In this series, the authors did not discuss the relationship between the expansion ratio and the clinical outcome because not all of the patients had pathognomonic lesions at the C5 and C6 levels. However, the main purpose of this surgery is to decompress the neural structures. Therefore, it is obvious that a wider spinal canal is preferable to obtain good results, especially in patients with OPLL in whom large-volume lesions occupy the spinal canal anteriorly.
In contrast, the increased inclination angle of the lamina was larger in DDL than TBL at both the C5 and C6 levels. This means that bilateral stenosis at the entrance of the foramen can be decompressed in DDL. Of course, the hemilateral stenosis at the entrance of the foramen can well be decompressed at an open side in TBL, which is wider than in DDL, and it can be visualized.
The following are considered the appropriate surgical indications of TBL: (1) CSM combined with hemilateral radiculopathy, (2) large prominence of OPLL, and (3) patients with tiny spinous processes who cannot undergo DDL. From the viewpoint that the postoperative posterior skeletal structure of the cervical spine remains symmetrical in DDL, it is thought that appropriate surgical indications of DDL are (1) usual CSM, (2) small and slight prominence of OPLL, (3) CSM combined with bilateral radiculopathy, and (4) cervical canal stenosis combined with instability necessitating posterior spinal instrumentation surgery such as rheumatoid cervical spine. Posterior spinal instruments can be set bilaterally without being interrupted by inclined spinous processes [12]. From the beginning, the authors had chosen TBL or DDL in accordance with the surgical indications mentioned above. Therefore, DDL was not performed for patients with large prominence of OPLL. From the results of this series, it is considered that the authors’ strategy was reconfirmed to be correct.
In conclusion, even now, it is unclear as to what is the minimum expansion ratio of the spinal canal needed to obtain adequate decompression of the spinal cord. It is thought best for a surgeon to perform surgery by his or her most familiar method. However, it is necessary to recognize the advantages and disadvantages of each surgical method.
References
- 1.Oyama M, Hattori S, Moriwaki N. A new method of cervical laminectomy. Cntrl Jpn Orthop Traumat Surg. 1973;16:792–794. [Google Scholar]
- 2.Hirabayashi K, Watanabe K, Wakano K, et al. Expansive open-door laminoplasty for cervical spinal stenotic myelopathy. Spine. 1983;8:693–699. doi: 10.1097/00007632-198310000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Ito T, Tsuji H. Technical improvements and results of laminoplasty for compressive myelopathy in the cervical spine. Spine. 1985;10:729–736. doi: 10.1097/00007632-198510000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Iwasaki H. Expansive laminoplasty. Seikeigeka. 1987;2(Suppl):228–233. [Google Scholar]
- 5.Kurokawa T, Tsuyama N, Tanaka H, et al. Double-door laminoplasty. Bessatsu Seikeigeka (Suppl Orthop Surg) 1982;2:234–240. [Google Scholar]
- 6.Tsuzuki N, Zhogshi L, Abe R, et al. Paralysis of the arm after posterior decompression of the cervical spinal cord. Anatomical investigation of the mechanism of paralysis. Eur spine J. 1993;2:191–196. doi: 10.1007/BF00299445. [DOI] [PubMed] [Google Scholar]
- 7.Asano T, Hirabayashi S (2006) Surgical management of ossification of the posterior longitudinal ligament. In: Schmidek HH, Roberts DW (ed) Operative neurosurgical techniques indications, methods, and results, 5th edn. Saunders, pp 1879–1895
- 8.Hirabayashi S, Kumano K. Development of a new spacer well adapted to split spinous process in double-door laminoplasty. Seikeigeka (Orthop Surg) 1995;46:110–112. [Google Scholar]
- 9.Hirabayashi S, Koshizuka Y. New method of measuring area of spinal canal after double-door laminoplasty. J Orthop Sci. 1999;4:78–82. doi: 10.1007/s007760050078. [DOI] [PubMed] [Google Scholar]
- 10.Hirabayashi S, Kumano K. Contact of hydroxyapatite spacer with split spinous process in double-door laminoplasty for cervical myelopathy. J Orthop Sci. 1999;4:264–268. doi: 10.1007/s007760050102. [DOI] [PubMed] [Google Scholar]
- 11.Hirabayashi S, Kumano K. Finite element analysis of the space created by split spinous processes in double-door laminoplasty to optimize shape of an artificial spacer. J Musculoskelet Res. 2000;4:47–54. [Google Scholar]
- 12.Hirabayashi S, Saiki K, Sakai H. Occipitocervicothoracic fixation using a rod and hook systemfor patients with rheumatoid cervical spine. Mod Rheumatol. 2004;14:435–441. doi: 10.1007/s10165-004-0339-9. [DOI] [PubMed] [Google Scholar]
- 13.Zhang J, Hirabayashi S, Saiki K, et al. Effectiveness of multiple-level decompression in laminoplasty and simultaneous C1 laminectomy for patients with cervical myelopathy. Eur Spine J. 2005;21:1–8. doi: 10.1007/s00586-005-0025-4. [DOI] [PMC free article] [PubMed] [Google Scholar]