Abstract
Short segment posterior fixation is the preferred method for stabilizing thoracolumbar fractures. In case of significant disruption of the anterior column, the simple short segment construct does not ensure adequate stability. In this study, we tried to evaluate the effect of inclusion of the fractured vertebra in short segment fixation of thoracolumbar fractures. In a prospective randomized study, eighty patients with thoracolumbar fractures treated just with posterior pedicular fixation were randomized into two groups receiving either the one level above and one level below excluding the fracture level (bridging group), or including the fracture level (including group). Different clinical and radiological parameters were recorded and followed. A sum of 80 patients (42 patients in group 1 and 38 patients in group 2) were enrolled in the study. The patients in both the groups showed similar clinical outcome. There was a high rate of instrumentation failure in the “bridging” group. The “bridging” group showed a mean worsening (29%) in kyphosis, whereas the “including” group improved significantly by a mean of 6%. The significant effect of the “including” technique on the reduction of kyphotic deformity was most prominent in type C fractures. In conclusion, inclusion of the fracture level into the construct offers a better kyphosis correction, in addition to fewer instrument failures, without additional complications, and with a comparable-if not better-clinical and functional outcome. We recommend insertion of screws into pedicles of the fractured thoracolumbar vertebra when considering a short segment posterior fixation, especially in Magerl type C fractures.
Keywords: Thoracolumbar instrumentation, Short segment, Including, Pedicular fixation, Fracture level
Introduction
Acute fracture of the thoracolumbar spine is a major cause of disability in adult population. Posterior transpedicular fixation has been the preferred method for stabilizing acute unstable thoracolumbar fractures [1, 2].
Short segment fixation of the fracture level has replaced the traditional long segment instrumentation to decrease the number of motion segments sacrificed in the fusion process [2–5]. However, when there is significant disruption of the load-sharing anterior column, the simple one level above and one level below short segment fixation does not ensure adequate stability, resulting in poor reduction in the kyphotic deformity and occurrence of instrument failure [6]. This necessitates more extensive approaches, such as anterior reconstruction via an anterior approach or posteriorly using balloon-assisted vertebroplasty [7].
A few studies have shown that by inserting screws at the fracture level, the construct will be biomechanically stronger [8]; which in turn may omit the need for further anterior reconstruction. Only two studies [8, 9] have considered the inclusion of the fracture level in short segment fixation. In this study, we have tried to compare the one level above and one level below excluding the fracture level, and the one level above and one level below including the fracture level. For more precise evaluation, the fracture classification system proposed by Magerl et al. [10] and modified by Gerzbein has been utilized. Different parameters important in outcome will be evaluated and discussed.
Methods
Between March 2002 and August 2008, 80 patients with fractures occurring between T12 and L2 who were treated just with posterior fusion and instrumentation were enrolled in this prospective randomized study. Surgical indications included more than 50% loss of vertebral body height, kyphosis progressing 20% or more, or more than 50% of canal involvement. The neurological status of the patient was recorded based on the Frankel classification. Plain spinal X-rays, computed tomography and magnetic resonance imaging were used to evaluate the fracture. Fracture of any of the pedicles was not considered a contraindication to screw placement.
Patients were randomized into two groups and received either the one level above and one level below excluding the fracture level (group 1, also labeled as the “bridging” group), or the one level above and one level below including the fracture level (group 2, also labeled as the “including” group).
All fractures were classified based on the radiographic identification of the mechanism of injury into three groups as classified by Magerl et al. [10]: compression injury force (A); distraction injury force (B); or multidirectional with translational injury force (C). The groups were further subclassified into 1–3 based on the same classification. A fracture could have occurred due to one, two or all three injury forces in a single patient, hence labeled as A2–B2–C1. However, due to the high number of possible combinations and difficulty in analysis, only the main type (A, B or C) was used in analysis.
All operations were performed by the senior author, utilizing the same instrumentation system, with screw size chosen accordant to the size of vertebra (6.5 × 45-mm screws and 5-mm rods at most of the time). The appropriate force (either compression or distraction) in addition to a slight lordosis were applied over the screwed levels. In group two, fracture level screws were inserted at the same time with the other screws prior to compression/distraction, and were included into the lordosing-distracting maneuver. Laminectomy and decompression were performed when indicated by the presence of compression over neural tissue in MRI. In just two cases in group two, we had to remove a small part of the fractured pedicle which was medially displaced, to avoid canal compromise. Fusion was performed in all patients using either autologous bone or tricalcium phosphate granules. All patients got out of bed on the second day after surgery. Patients were followed for a minimum period of 6 months. Mean follow-up time was 37 ± 11 months (range 6–84 months).
Pre-operative and follow-up radiographs at sixth month were evaluated by an independent observer who did not take part in surgeries. Different parameters were used to compare the two groups, including the duration of operation, amount of blood loss, length of hospital stay; complications including instrument failure and infections; pain severity as measured by the visual analog scale (VAS) at follow-up; limitation of motion as measured roughly during follow-up examination; kyphotic angle; and functional quality of life as measured by Denis work scale. Sagittal plane deformity (kyphotic angle) was calculated in all radiographs using the Cobb’s method. The difference between pre-operative and follow-up kyphotic angles and the percentage of correction, as calculated by the difference divided by the pre-operative kyphotic angle, were also taken into consideration. During the whole follow-up time, further radiographs were taken if there were any new complaints or problems to the patients.
Student’s t test was used for statistical analysis of kyphotic angle parameters. Mann–Whitney and χ2 tests were performed for statistical analysis of surgical outcomes. Any value of P smaller than 0.05 was considered statistically significant.
Results
A sum of 80 patients (42 patients in group 1 and 38 patients in group 2) were enrolled in the study. Mean age at the time of operation was 34.5 ± 14.2 years (range 18–75). There were 58 male and 22 female patients, with a male to female ratio of 2.64. The majority of fractures resulted due to falls (48 cases; 60.0%), the remaining cases resulted from car accidents (32 cases; 40.0%).
There were no significant differences between groups regarding age, fracture level, neurological deficit, Magerl class, and mechanism of injury (Tables 1, 2). Regarding fusion with either bone or tricalcium phosphate, and whether decompressive laminectomy had been performed, there were also no significant differences (P > 0.05).
Table 1.
Summary of demographic and clinical data distribution in both groups
| Characteristics | Group 1 | Group 2 | P value |
|---|---|---|---|
| Mean age (years) | 34.9 (SD = 14.2) | 34.0 (SD = 14.4) | 0.778 |
| Mechanism of injury | |||
| Falls | 25 | 23 | 0.433 |
| Accidents | 17 | 15 | |
| Neurological deficit | |||
| Frankel A | 1 | 0 | 0.656 |
| Frankel B | 5 | 4 | |
| Frankel C | 6 | 4 | |
| Frankel D | 0 | 0 | |
| Frankel E | 30 | 30 | |
| Fracture level | |||
| T12 | 18 | 13 | 0.085 |
| L1 | 20 | 22 | |
| L2 | 4 | 3 | |
| Magerl typea | |||
| A (compressive) | 37 | 33 | 0.211 |
| B (distractive) | 28 | 25 | |
| C (rotational) | 6 | 6 | |
aIn many cases, more than one mechanism of injury has been responsible (for instance A3B1C1); therefore, the sum of the groups exceeds 80
Table 2.
Detailed description of fracture types based on Magerl classification
| Magerl type | Group 1 | Group 2 |
|---|---|---|
| A1 | 2 | 1 |
| A2 | 3 | 2 |
| A3 | 6 | 7 |
| B1 | 3 | 2 |
| A1B1 | 5 | 4 |
| A1B2 | 3 | 2 |
| A2B1 | 8 | 9 |
| A2B2 | 2 | 2 |
| A3B1 | 4 | 3 |
| A3B3 | 0 | 1 |
| C1 | 1 | 3 |
| A2B2C1 | 3 | 2 |
| C3 | 1 | 1 |
| A2C3 | 1 | 0 |
| Total | 42 | 38 |
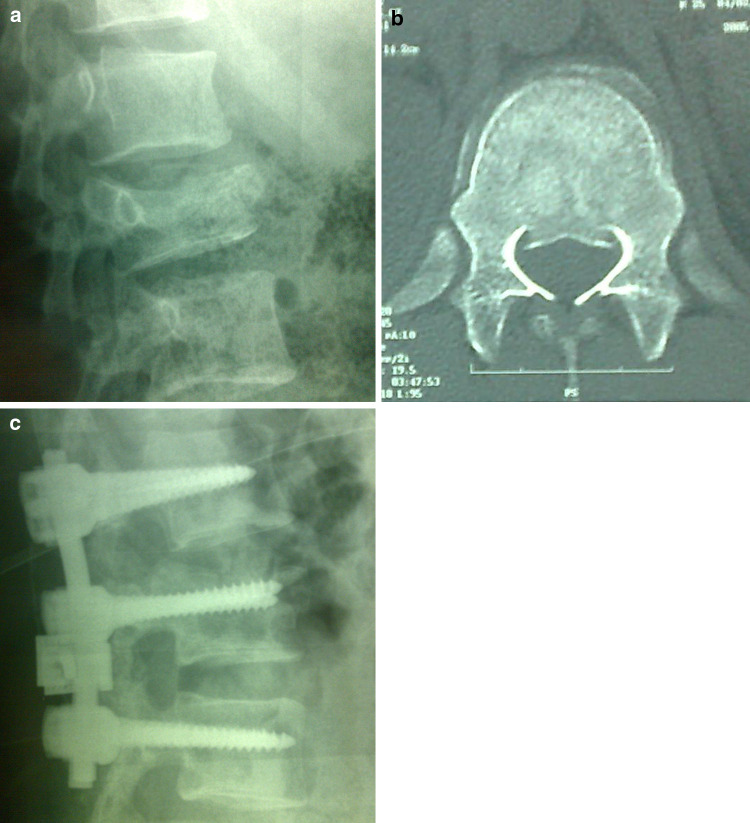
The groups were also similar in regard to the duration of operation, length of hospitalization, amount of blood loss, and infectious complications (Table 3). Post-operative VAS score was similar in both the groups (P = 0.125); and limitation of motion was non-significantly higher in group one (P = 0.14). Implant failures occurred with a higher frequency in group one (21.4%) than in group two (5.3%) (P = 0.02) (Fig. 1; Table 4).
Table 3.
Summary of operation and outcome values
| Group 1 | Group 2 | P value | |
|---|---|---|---|
| Mean operation time (min) | 168 ± 72 | 169 ± 59 | 0.950 |
| Mean hospitalization (day) | 9 ± 7 | 13 ± 10 | 0.269 |
| Mean blood loss (mL) | 515 ± 485 | 430 ± 305 | 0.368 |
| Post-op infections | 4 | 2 | 0.691 |
| Implant failure | 9 | 2 | 0.020 |
| VAS score | 3.6 ± 1.8 | 2.9 ± 1.4 | 0.068 |
| Limitation of motion (°) | 19 ± 14 | 14 ± 14 | 0.141 |
Values in italics refer to the statistically significant P values
Fig. 1.
Early post-operative biplanar radiograph (a, b) of a patient in the “bridging” group shows poor reduction in kyphosis and coronal plane deformity at the injured segment (c, d). Twelve-month follow-up biplanar radiograph shows failure of the anterior column and worsening kyphosis and scoliosis
Table 4.
Types of implant failure
| Type | Group 1 | Group 2 |
|---|---|---|
| Screw breakage | 1 | 1 |
| Rod displacement/breakage | 7 | 1 |
| Screw head dislodgement | 1 | 0 |
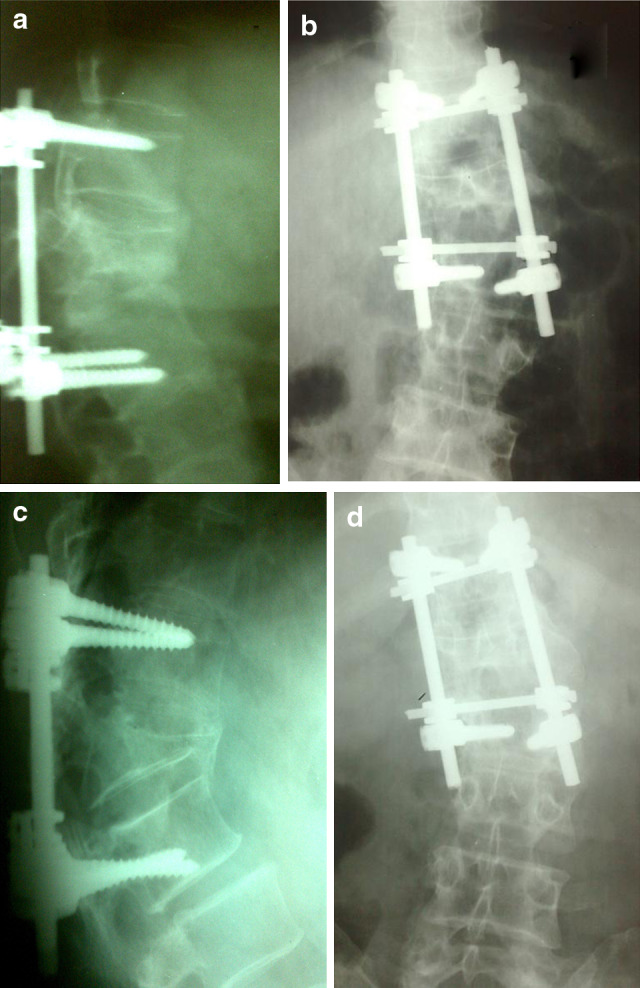
The pre-operative kyphotic angle was similar in both groups (P = 0.94); however, the post-operative kyphotic angle, and the percentage of correction showed significant differences (P = 0.008, and P = 0.04; respectively); showing a higher degree of kyphosis correction in the “including” group (Table 5; Fig. 2). When considering each Magerl type separately, these differences were significant only in type C fractures (P = 0.018).
Table 5.
Kyphotic angle parameters in two groups
| Mean | Group 1 | Group 2 | P value |
|---|---|---|---|
| Pre-op kyphotic angle (°) | 20 ± 13 | 19 ± 13 | 0.613 |
| Follow-up kyphotic angle (°) | 19 ± 10 | 14 ± 8 | 0.008 |
| Difference (°) | 1 ± 12 | 5 ± 10 | 0.094 |
| Percentage of correction | −29% | 6% | 0.040 |
Values in italics refer to the statistically significant P values
Fig. 2.
Pre-operative plane radiograph (a), axial computed tomography (b) and 12-month post-operative radiographs (c) of a patient in the “including” group show optimal correction of kyphosis at the injured segment
Further analysis on Denis work scale did not show any significant difference between the two groups (P = 0.08).
Discussion
Almost all independent variables showed great similarity between the two groups, hence the aim of having two relatively homogenous groups was achieved. Inclusion of the fracture level in the construct did not lengthen the operation or hospitalization, nor did it increase the amount of blood loss or post-operative infections. The patients in the “including” group also showed insignificant reductions in VAS score and limitation of motion, and a similar (and not worse) functional quality of life in comparison to the other group. All of the above data, although not in favor of any of the two groups, introduce the “including” technique as relatively safe and without additional complications to the patient. In contrast to some other studies [9], we did not keep from inserting screws into fractured pedicles; and observed no related complications.
Although the insertion of additional two screws in group two is more demanding than the first group, the difference between operation times has not been statistically significant. This may be due to the fact that other parts of the operation (e.g. posterolateral exposure, laminectomy-decompression, fusion, etc.) have taken relatively equal time in both groups; therefore, the smaller contribution of additional screw placement has not shown statistical significance.
The correction of kyphosis, as measured by Cobb angles at pre-op and 6-month post-operative radiographs, favor the second group completely. The “bridging” group showed a mean worsening (29%) in kyphosis (Fig. 1), whereas the “including” group improved significantly by a mean of 6% (Fig. 2) (P = 0.04) and such a worsening may be due to a failed load-sharing anterior column. It is possible that the inclusion of the fracture level in the second group has led to a stronger 3-point posterior support (instead of a 2-point fixation in the “bridging” method) for the failed anterior column in eligible cases. Indeed, we have tried to use the “including” technique in a few cases, where there were equivocal indications for an anterior approach, with success. The high rate of instrumentation failure in the “bridging” group (9 out of 42; 21.4%) when compared with the “including” group (2 out of 38; 5.3%) favors the above explanation. A more detailed radiological analysis, incorporating the load-sharing classification proposed by McCormack et al. [11], may better clarify such an explanation.
There is certainly no need to emphasize that fractures with load-sharing scores of 7 or more will need an anterior-only approach, or a staged anterior reconstruction or augmentation following a posterior approach [11]. Although we have tried to use a short segment construct with fracture level screws in a few borderline cases, the eventual need for a delayed anterior augmentation in more severe cases should not be ignored. Anterior procedures offer good visualization of the fracture and allow a more direct visualization of the defect [12, 13]; however, they take longer time in causing more blood loss and morbidity [12], and are unfamiliar and demanding to many surgeons. Another important point to mention is that in cases for which an anterior augmentation by partial corpectomy is anticipated in future for any reason, at least one screw at the fractured vertebra must be short enough to allow for such a corpectomy. Therefore, not both screws at the fracture site should be so long to penetrate the distal cortex, and they can be scaled down to screw length of about 25−35 mm.
In a similar study conducted by Guven et al. [9], the authors studied the inclusion of the fracture level in both short and long segment fixation. They observed that fracture level fixation had lowered the rates of correction failure which was most significant on short segment constructs. They concluded that fracture level screw combination can achieve and maintain kyphosis correction. In addition, in a cadaveric biomechanical study, Mahar et al. [8] showed that insertion of the screws at the fracture level improved biomechanical stability by providing additional fixation points which may aid in fracture reduction and kyphosis correction. They also concluded that segmental fixation with additional screws at the level of the fracture increases construct stiffness and shields the fractured vertebral body from anterior loads [8]. Even in the case of a burst and completely disconnected pedicle, insertion of the screw into the pedicle will probably stiffen the rod through additional screw linkage and also by vertebral body fixation.
The superiority of the “including” technique could not of course be extended to the other regions of the vertebral column. In fact in another study, Carl et al. [13] reported that in thoracolumbar region where compressive forces act more anteriorly, inclusion of two further levels above the fracture is necessary to achieve a stable fusion; whereas in the more lordotic middle and lower lumbar spine where the compressive forces act more posteriorly, no implant failure occurred while using a short segment two-level fixation construct.
The novelty of this study was to consider the fracture dynamics based on the Magrel classification, in contrast to the other studies which have used the simpler Denis classification. The significant effect of the “including” technique on the reduction of kyphotic deformity was most prominent in type C fractures (P = 0.018). This is because the more severe type C rotational fracture with uni- or multi-directional translation is the least stable and does better when fused by the stronger 3-point fixation construct in the “including” technique. It is therefore recommended that inclusion of the fracture level be performed at least in all type C fractures.
In conclusion, inclusion of the fracture level into the construct has offered a better kyphosis correction, in addition to fewer instrument failures, without additional complications, and with a comparable -if not better- clinical and functional outcome. We recommend insertion of screws into pedicles of the fractured thoracolumbar vertebra when considering a short segment posterior fixation, especially in Magerl type C fractures.
Conflict of interest statement
We do not have any financial relationships with the organization that sponsored the research.
References
- 1.Akbarnia BA, Crandall DG, Burkus K, Matthews T. Use of long rods and a short arthrodesis for burst fractures of the thoracolumbar spine A long-term follow-up study. J Bone Joint Surg Am. 1994;76(11):1629–1635. doi: 10.2106/00004623-199411000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Knop C, Bastian L, Lange U, Oeser M, Zdichavsky M, Blauth M. Complications in surgical treatment of thoracolumbar injuries. Eur Spine J. 2002;11(3):214–226. doi: 10.1007/s00586-001-0382-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Parker JW, Lane JR, Karaikovic EE, Gaines RW. Successful short segment instrumentation and fusion for thoracolumbar spine fractures: a consecutive 4 1/2-year series. Spine. 2000;25(9):1157–1170. doi: 10.1097/00007632-200005010-00018. [DOI] [PubMed] [Google Scholar]
- 4.Tezeren G, Kuru I. Posterior fixation of thoracolumbar burst fracture: short-segment pedicle fixation versus long-segment instrumentation. J Spinal Disord Tech. 2005;18(6):485–488. doi: 10.1097/01.bsd.0000149874.61397.38. [DOI] [PubMed] [Google Scholar]
- 5.Altay M, Ozkurt B, Aktekin CN, Ozturk AM, Dogan O, Tabak AY. Treatment of unstable thoracolumbar junction burst fractures with short- or long-segment posterior fixation in Magerl type A fractures. Eur Spine J. 2007;16(8):1145–1155. doi: 10.1007/s00586-007-0310-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McLain RF (2006) The biomechanics of long versus short fixation for thoracolumbar spine fractures. Spine 15 31(11 Suppl):S70–S79 [DOI] [PubMed]
- 7.Marco RAW, Kushwaha VP. Thoracolumbar burst fractures treated with posterior decompression and pedicle screw instrumentation supplemented with balloon-assisted vertebroplasty and calcium phosphate reconstruction. J Bone Joint Surg Am. 2009;91(1):20–28. doi: 10.2106/JBJS.G.01668. [DOI] [PubMed] [Google Scholar]
- 8.Mahar A, Kim C, Wedemeyer M, Mitsunaga L, Odell T, Johnson B, Garfin S. Short-segment fixation of lumbar burst fractures using pedicle fixation at the level of the fracture. Spine. 2007;32(14):1503–1507. doi: 10.1097/BRS.0b013e318067dd24. [DOI] [PubMed] [Google Scholar]
- 9.Guven O, Kocaoglu B, Bezer M, Aydin N, Nalbantoglu U. The Use of screw at the fracture level in the treatment of thoracolumbar burst fractures. J Spinal Disord Tech. 2009;22:417–421. doi: 10.1097/BSD.0b013e3181870385. [DOI] [PubMed] [Google Scholar]
- 10.Magerl F, Aebi M, Gertzbein SD, Harms J, Nazarian S. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1994;3(4):184–201. doi: 10.1007/BF02221591. [DOI] [PubMed] [Google Scholar]
- 11.McCormack T, Karaikovic E, Gaines RW. The load sharing classification of spine fractures. Spine (Phila Pa 1976) 1994;19(15):1741–1744. doi: 10.1097/00007632-199408000-00014. [DOI] [PubMed] [Google Scholar]
- 12.Dimar JR, Wilde PH, Glassman SD, Puno RM, Johnson JR. Thoracolumbar burst fractures treated with combined anterior and posterior surgery. Am J Orthop. 1996;25:159–165. [PubMed] [Google Scholar]
- 13.Carl AL, Tromanhauser SG, Roger DL. Pedicle screw instrumentation for thoracolumbar burst fractures and fracture-dislocation. Spine. 1992;17:S317–S324. doi: 10.1097/00007632-199208001-00018. [DOI] [PubMed] [Google Scholar]