Abstract
Open-door laminoplasty is a commonly performed procedure for the treatment of multiple level cervical spinal stenosis. One complication of this procedure is closure of the hinge and subsequent restenosis. Twinfix suture anchor was used in laminoplasty to stabilize cervical canal expansion. 53 patients with multiple level cervical spinal stenosis underwent laminoplasty. A unilateral open-door technique was performed for the lesion level and the elevated lamina was fixed to the lateral mass using Twinfix suture anchors. Radiography, magnetic resonance imaging, and computed tomography (CT) scanning were used for imaging studies. The Japanese Orthopedic Association score was adopted to compare clinical outcome before and after surgery. None of 53 patients who had the door secured with Twinfix suture anchors had closure of the hinge. Additionally, the suture anchors maintained their position without loosening or “pull-outs” on postoperative follow-up radiographs. The Japanese Orthopedic Association score increased significantly from 8.5 ± 3.2 before surgery to 14.2 ± 1.36 at final follow-up. Postoperative radiography and CT scan demonstrated significantly increased anteroposterior diameter of the spinal canal. There were four short-term complications: two were small dural-tears which were repaired intraoperatively without further sequelae, and the other 2 were both epidural hematomas that required emergent return to the operating room for evacuation. There were no Twinfix suture anchor-related complications. This Twinfix suture anchor can provide a firm and secure anchor for elevated open laminae in laminoplasty.
Keywords: Laminoplasty technique, Open door, Suture anchor
Introduction
Multiple level cervical spinal stenosis with myelopathy caused by degenerative disc disease or ossification of posterior longitudinal ligaments (OPLL) is common, especially in old people. The surgical treatment involves an anterior or a posterior approach. A posterior approach including total laminectomy or laminoplasty is the most common procedure for treating multilevel cervical canal stenosis with myeloradiculopathy. In the past few decades, several variations of cervical laminoplasty such as expansive open-door laminoplasty [1–3], double-door laminoplasty [4], and hardware-assisted laminoplasty have been reported. One of the known complications of the “open-door” technique is postoperative reclosure of the hinge, causing restenosis of the canal [5, 6]. Liu reported that the rate of reclosure of laminoplasty was 2.4% [7]. Kashihara [8] reported a reclosure rate of 28.3% in his series of 30 patients treated with double-door laminoplasty. In order to prevent lamina reclosure, a multitude of other techniques have been described, involving miniature implants to augment canal expansion [3, 9–11]. However, these mini implants can be technically difficult to handle during surgery. In our study, Twinfix suture anchors to maintain canal expansion were used at alternate cervical levels to stabilize the posterior elements in open-door laminoplasty since 2004.
Materials and methods
Hospital and office visit records, operative notes, and final follow-up radiographs of 53 retrospective patients who used Twinfix suture anchors (Smith & Nephew Inc, UK) to maintain cervical canal expansion since 2004 were reviewed.
The average age of the patients was 63.2 years (range 50–74). All patients had myelopathy symptoms such as bilateral hand clumsiness and numbness, unstable gait, increasing deep tendon reflex, and positive Hoffman and Babinski signs. Magnetic resonance imaging (MRI) showed multiple level cervical spinal stenosis. Suture anchors were fixed at C3, C5, and C7 levels or C4 and C6 levels based on the MRI. The computed tomograph (CT) radiographic evaluations were conducted during preoperative, postoperative, and follow-up examinations of patients. These records were analyzed for technical difficulties, intraoperative or postoperative complications, and radiographic signs of suture anchor failure or reclosure of the laminae.
Surgical technique
The indication for laminoplasty and open-door technique of decompression had been described extensively in prior publications [1–3]. In the experiment, 2.0-mm hand awl was used to start a pilot hole at 1-mm medial and inferior to the lateral mass midpoint on the hinge side. Twinfix suture anchors (Smith & Nephew, Inc, Endoscopy Division) were then inserted into the pilot holes (Fig. 1). Suture anchors were pointed 15° cephalad and 30°–40° laterally (An’s technique16) [12]. The open-door laminoplasty was performed with a 3-mm high-speed burr as described previously [1–3]. After burring the gutter and the hinge, nonabsorbable sutures were threaded into the previously made holes in the spinous processes at C3, C5, and C7 levels or C4 and C6 levels. Using bone clamps, with the force applied to the spinal process from the open side to the hinged side, the whole laminae were elevated until the laminae of the open side became almost horizontal to the ground. The sutures were tightened and tied firmly to anchor the laminae. A drain was left in the wound and removed 48 h postoperatively. Patients were placed in a soft collar and encouraged to perform range of motion of the neck as tolerated by pain. The soft collar was taken off at 6 week follow-up visit.
Fig. 1.

The picture shows a Twinfix suture anchor (a). The suture anchors were inserted at the C4 and C6 lateral masses and nonabsorbable sutures were passed through the drilled holes in the spinous process (b)
Postoperative assessment
Treatment outcome was evaluated by directly questioning the patients before the procedure and at final follow-up using the Japanese Orthopedic Association (JOA) criteria [13]. At 6 months after surgery, a CT scan was used to compare the postoperative anteroposterior (AP) diameter of the spinal canal with the results from the previous CT scan.
Statistical analysis
Results were analyzed statistically with paired Student t test using SPSS 13.0 software (SPSS Inc, USA). The level of significance was set to P < 0.05.
Results
The average final radiographic follow-up was 32.5 weeks (range 10–49). A total of 147 of 148 suture anchors were placed successfully intraoperatively, with 1 suture anchor abandoned owing to poor bone on the lateral mass. The mean JOA score increased significantly from 8.5 ± 3.2 (range 6–11) before surgery to 14.2 ± 1.3 (range 13–15) at final follow-up. There was significant difference between the score before surgery and at final follow-up (P < 0.05). The results of cervical canal expansion were analyzed as follows: mean AP diameter significantly expanded from 9.5 ± 0.7 to 13.4 ± 1.2 at the C3 level in 42 patients, from 9.3 ± 1.0 to 13.7 ± 1.1 at the C4 level in 53, from 9.3 ± 0.9 to 14.3 ± 1.6 at the C5 level in 53, from 9.2 ± 0.8 to 13.9 ± 1.2 at the C6 level in 53, and from 9.9 ± 0.9 to 13.6 ± 1.1 at the C7 level in 35 patients (Fig. 2, Table 1). None of 53 patients had evidence of loosening or “pull-out” of the anchors on final postoperative follow-up radiographs (Figs. 3 and 4). None developed a cervical kyphotic deformity after surgery. Two patients had a small dural-tear not related to the suture anchors, which was repaired intraoperatively without further clinical sequelae. Two patients had postoperative epidural hematomas and were urgently taken back to the operating room for evacuation. At the time of the hematoma evacuation, all suture anchors were noted to be intact. Both patients recovered uneventfully without new neurologic deficits.
Fig. 2.
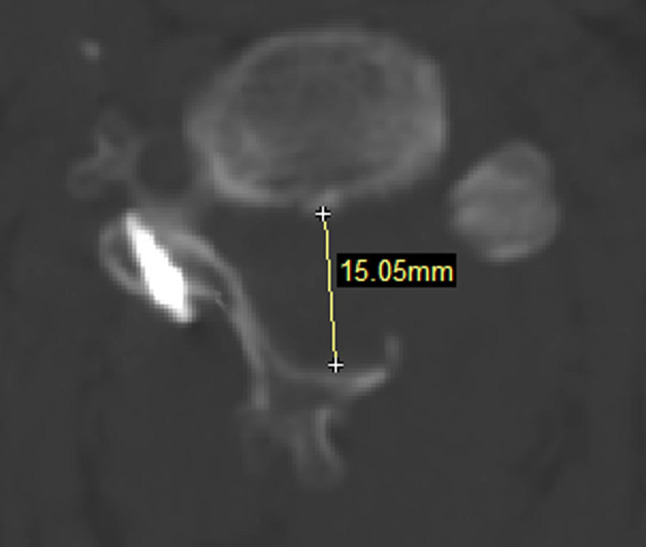
Anteroposterior diameter of the spinal canal was measured on the CT scan. The Twinfix suture anchor in the lateral mass was in proper position
Table 1.
Comparison of AP diameter before and after operation
| Level | Cases | Before operation (mm) | After operation (mm) | Increase (%) |
|---|---|---|---|---|
| C3 | 42 | 9.5 ± 0.7 | 13.4 ± 1.2 | 41.1 |
| C4 | 53 | 9.3 ± 1.0 | 13.7 ± 1.1 | 47.3 |
| C5 | 53 | 9.3 ± 0.9 | 14.3 ± 1.6 | 53.7 |
| C6 | 53 | 9.2 ± 0.8 | 13.9 ± 1.2 | 51.1 |
| C7 | 35 | 9.9 ± 0.9 | 13.6 ± 1.1 | 37.4 |
Fig. 3.

CT 3D reconstruction showed that the suture anchors were fixed at cervical level at C4 and C6, and Twinfix suture anchors did not pull-out or loose at 40 weeks follow-up
Fig. 4.

CT 3D reconstruction showed that unilateral open-door laminoplasty with Twinfix suture anchor fixation effectively kept the lifted lamina open and preserved cervical alignment at 40 weeks follow-up
Discussion
In the study, we found that Twinfix suture anchor could effectively maintain cervical canal expansion in laminoplasty. Cervical laminoplasty was developed as an alternative treatment to laminectomy for multilevel cervical stenosis with the belief that it would avoid instability, progressive kyphotic deformity, and the late neurologic deterioration caused by the “postlaminectomy membrane” [4, 14]. More recently, this technique has gained worldwide interest, developing many derivatives of the originally described technique. In our patients, Twinfix suture anchor was used to prevent the reclosure of the hinge of open-door laminoplasty.
The cervical level fixed with Twinfix suture anchors was decided based on the level of the cervical spinal stenosis before surgery. If multilevel cervical spinal stenosis was from C4 to C6, the Twinfix suture anchor was inserted into the lateral mass of C4 and C6 to maintain the “open-door” from C4 to C6. If spinal stenosis was from C3 to C7, the suture anchor was fixed at the lateral mass of C3, C5 and C7. None of the patients showed restenosis in postoperative follow-up radiographs. We thought that two surgery plans were sufficient for the stabilization of open-door laminoplasty on the basis of our follow-up results.
Chen and Yang reported that unilateral open-door laminoplasty with lateral mass screw fixation maintained expansion of the spinal canal [15, 16]. No displacement of the suture anchors and hinge reclosure were observed during their follow-up period. There were some differences between their lateral mass screw and Twinfix suture anchor. Lateral mass screws were firstly fixed into the lateral mass, and then nonabsorbable sutures were passed through the holes in the screws or wrapped around the neck of the screw. In our surgery, two nonabsorbable sutures had been already fixed at the end of Twinfix suture anchor by the manufacturer. A special tool provided by the manufacturer was conveniently used to insert Twinfix suture anchor into the lateral mass.
This is a preliminary study aimed to evaluate the benefits of Twinfix suture anchors for cervical laminoplasty. There are some limitations for this study. First, the investigation was retrospective without controls for comparison. Operative outcomes for various techniques have been reported as equivalent in literature. Surgeons chose different laminoplasty technique based on their preference and familiarity. For rigorous evaluation of the feasibility of this modified technique, more cases with prospective controlled comparison are required. Second, the follow-up of study was still short. For some reasons, the patients of China usually came to author’s hospital during the first year of follow-up. Longer follow-up are needed to effectively assess the efficacy and facility of the method. Despite the above-mentioned limitations, we have shown that Twinfix suture anchors could effectively maintain the cervical canal expansion in laminoplasty.
Conclusion
The study demonstrated that Twinfix suture anchors could provide a firm and secure anchor for elevated open lamina and maintain canal expansion in laminoplasty.
Contributor Information
Hai-long Yu, Email: yuhailong118@yahoo.com.cn.
Liang-bi Xiang, Email: xiangliangbi1963@sina.com.
References
- 1.Hirabayashi K, Satomi K. Operative procedure and results of expansive open-door myelopathy. Spine. 1988;13:870–876. doi: 10.1097/00007632-198807000-00032. [DOI] [PubMed] [Google Scholar]
- 2.Hirabayashi K, Watanabe K, Wakano K, Suzuki N, Satomi K, Ishii Y. Expansive opendoor laminoplasty for cervical spinal stenotic myelopathy. Spine. 1983;8:693–699. doi: 10.1097/00007632-198310000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Park AE, Heller JG. Cervical laminoplasty: use of a novel titanium plate to maintain canal expansion—surgical technique. J Spinal Disord Tech. 2004;17:265–271. doi: 10.1097/01.bsd.0000095401.27687.c0. [DOI] [PubMed] [Google Scholar]
- 4.Seichi A, Takeshita K, Ohishi I, Kawaguchi H, Akune T, Anamizu Y, Kitagawa T, Nakamura K. Long-term results of doubledoor laminoplasty for cervical stenotic myelopathy. Spine. 2001;26:479–487. doi: 10.1097/00007632-200103010-00010. [DOI] [PubMed] [Google Scholar]
- 5.Patel CK, Cunningham BJ, Herkowitz HN. Techniques in cervical laminoplasty. Spine. 2002;2:450–455. doi: 10.1016/S1529-9430(01)00158-9. [DOI] [PubMed] [Google Scholar]
- 6.Satomi K, Ogawa J, Ishii Y, Hirabayashi K. Short-term complications and long-term results of expansive open-door laminoplasty for cervical stenotic myelopathy. Spine. 2001;1:26–30. doi: 10.1016/S1529-9430(01)00008-0. [DOI] [PubMed] [Google Scholar]
- 7.Liu G, Buchowski JM, Bunmaprasert T, Yeom JS, Shen H, Riew KD. Revision surgery following cervical laminoplasty: etiology and treatment strategies. Spine. 2009;34:2760–2768. doi: 10.1097/BRS.0b013e3181b11ee1. [DOI] [PubMed] [Google Scholar]
- 8.Kashihara M. Analysis of reclosure of lamina in spinous process-splitting cervical laminoplasty. Cent Jpn J Orthop Trumat. 2006;49:779–780. [Google Scholar]
- 9.Deutsch H, Mummaneni PV, Rodts GE, Haid RW. Posterior cervical laminoplasty using a new plating system: technical note. J Spinal Disord Tech. 2004;17:317–320. doi: 10.1097/01.bsd.0000091070.73042.23. [DOI] [PubMed] [Google Scholar]
- 10.Goto T, Ohata K, Takami T, Nishikawa M, Tsuyuguchi N, Morino M, Matusaka Y, Nishio A, Inoue Y, Hara M. Hydroxyapatite laminar spacers and titanium miniplates in cervical laminoplasty. J Neurosurg. 2002;97:323–329. doi: 10.3171/spi.2002.97.3.0323. [DOI] [PubMed] [Google Scholar]
- 11.Tsuzuki N. A novel technique for laminoplasty augmentation of spinal canal area using titanium miniplate stabilization: a computerized morphometric analysis. Spine. 1997;22:926–927. doi: 10.1097/00007632-199704150-00022. [DOI] [PubMed] [Google Scholar]
- 12.Anderson PA, Henley MB, Grady MS, Montesano PX, Winn HR. Posterior cervical arthrodesis with AO reconstruction plates and bone graft. Spine. 1991;16:S72–S79. doi: 10.1097/00007632-199103001-00012. [DOI] [PubMed] [Google Scholar]
- 13.Kawai S, Sunago K, Doi K, Saika M, Taguchi T. Cervical laminoplasty (Hattori’s method). Procedure and follow-up results. Spine. 1988;13:1245–1250. doi: 10.1097/00007632-198811000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Tomita K, Kawahara N, Toribatake Y, Heller JG. Expansive midline T-saw laminoplasty (modified spinous process-splitting) for the management of cervical myelopathy. Spine. 1998;23:32–37. doi: 10.1097/00007632-199801010-00007. [DOI] [PubMed] [Google Scholar]
- 15.Yang SC, Yu SW, Tu YK, Niu CC, Chen LH, Chen WJ. Open-door laminoplasty with suture anchor fixation for cervical myelopathy in ossification of the posterior longitudinal ligament. J Spinal Discord Tech. 2007;20:492–498. doi: 10.1097/BSD.0b013e318033e844. [DOI] [PubMed] [Google Scholar]
- 16.Chen HC, Chang MC, Yu WK, Wang ST, Liu CL, Chen TH. Lateral mass anchoring screws for cervical laminoplasty: preliminary report of a novel technique. J Spinal Disord Tech. 2008;21:387–392. doi: 10.1097/BSD.0b013e318157c699. [DOI] [PubMed] [Google Scholar]


