Abstract
Cervical pedicle screws have been reported to be biomechanically superior to lateral mass screws. However, placement of these implants is a technical challenge. The purpose of this investigation was to use an anatomic and a clinical study to evaluate a technique for placement of the pedicle screws in the C7 vertebra using fluoroscopic imaging in only the anteroposterior (A/P) plane. Ten adult cadaver C7 vertebrae were used to record the pedicle width, inclination and a suitable entry point for placement of pedicle screws. A prospective study of 28 patients undergoing posterior instrumentation of the cervical spine with C7 pedicle screw placement was also performed. A total of 55 C7 pedicle screws were placed using imaging only in the A/P plane with screw trajectory values obtained by the anatomic study. Radiographs and CT scans were performed post-operatively. The average posterior pedicle diameter of C7 vertebra was 9.5 ± 1.2 mm in this study. The average middle pedicle diameter was 7.1 mm and the average anterior pedicle diameter was 9.2 mm. The average transverse pedicle angle was 26.8 on the right and 27.3 on the left. CT scans were obtained on 20 of 28 patients which showed two asymptomatic cortical wall perforations. One screw penetrated the lateral wall of the pedicle and another displayed an anterior vertebral penetration. There were no medial wall perforations. The preliminary results suggest that this technique is safe and suitable for pedicle screw placement in the C7 vertebra.
Keywords: Cervical spine, Pedicle screw, C7 vertebra, Anatomy
Introduction
Pedicle screw instrumentation of the cervical spine is technically challenging due to the inherent anatomic variability of the pedicles and a lack of suitable landmarks. Numerous studies have evaluated the morphometry of the cervical pedicles to aid in the placement of pedicle screws; however, their conclusions have been cautious [2, 3, 9, 11]. Traditional methods of placement of pedicle screws in the C7 vertebra advocate the use of an open technique (laminectomy or lamino-foraminotomy) and/or imaging in two planes [6–8, 10]. Recently, computer-assisted techniques have been introduced with promising results [6]. However, these techniques require pre-operative CT scans integrated with expensive and potentially time-consuming instrumentation. We studied the fluoroscopic anatomy of the C7 vertebra and pedicles with a view to describe a reproducible technique of insertion of a C7 pedicle screw. Based on our anatomical results, we then performed C7 pedicle screw insertion on 28 patients using an anteroposterior (AP) fluoroscopic image. This paper describes our technique of C7 pedicle screw placement and evaluates the positioning of the screws with post-operative CT scans.
Materials and methods
Anatomic cadaver study of the C7 vertebra was first performed to delineate the fluoroscopic details and identify a suitable entry point for placement of the pedicle screws. In the second part, a prospective evaluation of 28 patients that underwent C7 pedicle screw instrumentation was carried out.
Anatomic
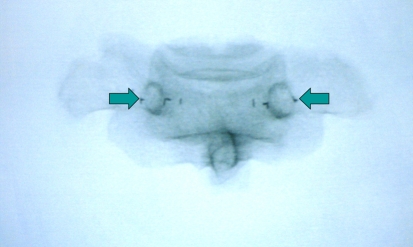
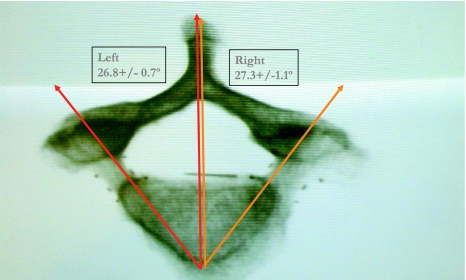
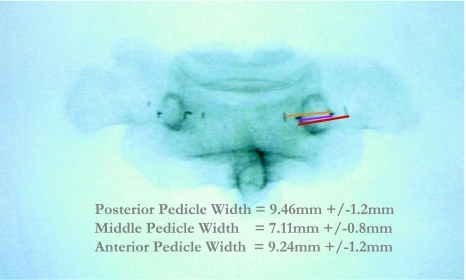
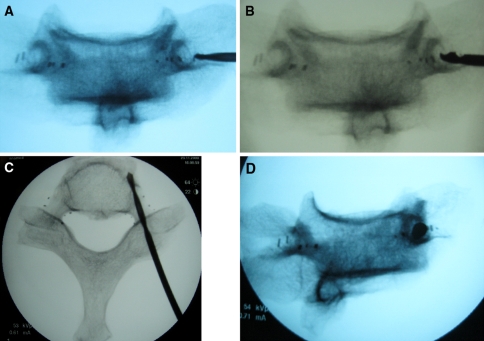
Ten human C7 vertebrae were disarticulated and harvested from six male and four female cadavers. Metal markers were placed to demarcate the width of the anterior and posterior border of each pedicle. Markers were also placed at the waist of each pedicle at its narrowest diameter. Each vertebra was carefully positioned to obtain the best A/P imaging of the pedicles in a single view using the C-arm fluoroscopic image. This was obtained with the C-arm beam lined up parallel to the plane of the superior endplate of the vertebra giving it a sharp image. With the use of the oblique function of the C-arm, the elliptical image of the left and the right pedicles was made to appear identical with the spinous process in the midline (Fig. 1). Another C-arm machine was used to obtain an axial view of the vertebra (Fig. 2). The A/P images were used to measure the anterior, waist and posterior width of each pedicle by measuring the distance between the metal markers (Fig. 3). The transverse pedicle angle was measured (Fig. 2) using the axial images as reported earlier [4]. The A/P images were reviewed to verify that the metal markers placed outlined the outer medial and lateral walls of the pedicles. A single observer made all measurements and observations. To reduce magnification error the measurements of each vertebra were compared with a standard object. Based on these measurements, the entry point of the pedicle screw was selected at the most lateral aspect of the elliptical density that represented the pedicle on the fluoroscopic image. The drill was also medially directed with an obliquity equal to that of the C-arm required to obtain a true AP view. The pedicle was drilled with a 2.5 mm drill bit and fluoroscopic images evaluated for placement of the bit (Fig. 4).
Fig. 1.
True A/P view of bilateral pedicles of C7 vertebra
Fig. 2.
An axial view of C7 vertebra and measurement of transverse pedicle angle
Fig. 3.
A/P view to measure the anterior, middle and posterior width of each pedicle by measuring the distance between the metal markers
Fig. 4.
Pre-drilling of pedicle screw in a cadaver vertebra. a Entry point of the pedicle screw selected at the most lateral aspect of the elliptical density. b Further progression of the drill into the pedicle. c Axial view of the vertebra with drill in situ. d Pedicle axis view of vertebra
Statistical analysis was used to calculate the average and standard deviation. Paired Student’s t test was used to determine statistical differences from the data set obtained from the right and left pedicles. p < 0.05 was considered statistical significant.
Clinical
Between January 2004 and July 2009, 28 patients that underwent posterolateral cervical fusion and instrumentation with pedicle screws (Vertex, Medtronic Sofamor Danek) involving the C7 vertebrae were included in the study. The diagnoses included cervical/foraminal stenosis, cervical instability, cervical spondylosis with myelopathy, nonunion from previous anterior fusion, degenerative disc disease and progressive kyphosis. A total of 29 patients (12 males and 17 females) were identified however, one female patient was excluded due to abnormal anatomy secondary to hyperparathyroidism and previous revision surgeries. Patients underwent 2–8 levels of fusion with an average of 4 levels. A total of 55 pedicle screws in 28 patients were placed using the above technique. Post-operative radiographs were obtained on all patients (Fig. 5) and a CT scan was performed in 20 of the 28 patients (Fig. 6).
Fig. 5.
Post-operative radiographs in a patient following C7 pedicle screw placement
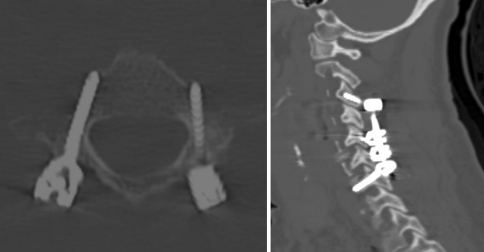
Fig. 6.
Post-operative CT scan of patient in Fig. 5
Technique
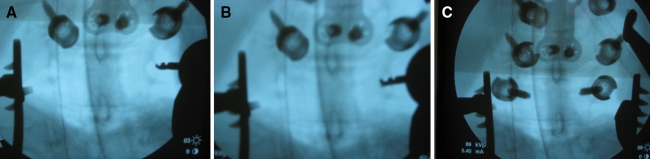
Patients were placed prone on a Jackson spinal table with a prone view device to position the head. Gardner–Wells tongs were applied for cranial traction. The patient’s shoulders were taped back to the table and SSEP and MEP monitoring was used in every case. A C-arm was used to obtain a true A/P image of the C7 pedicles. The images were determined to be true AP if the superior end plate of C7 vertebral body appeared sharp and the spinous process was in the midline. The entry point of each pedicle screw started at the most lateral aspect of the elliptical density that represented the pedicle on the fluoroscopic image. The drill was also medially directed with an obliquity equal to that of the C-arm required to obtain a true AP view. Each pedicle was pre-drilled with a 2.5 mm drill bit till hard bone was encountered and probed to assess for cortical violation. Prior to placement of the pedicle screws, the pedicle was tapped and again probed. A 3.5 or 4.0 mm screw was then placed under C-arm guidance (Fig. 7a–c). After all, implants were in place a final lateral radiograph was obtained prior to closure. However, the pedicles in the lower cervical spine are difficult to visualize in lateral images due to the overlying shoulders and this may not always be successful.
Fig. 7.
Intra-operative fluoroscopic images. a, Starting point b, Pedicle pre-drilled with a 2.5 mm drill bit. c A 3.5 mm screw is then placed under C-arm guidance
Results
Data from the ten cadaver specimens (6 males and 4 females) were grouped together in this study for a total of 20 pedicles. Table 1 shows a summary of the data obtained. There was no statistically significant difference observed between the right and left posterior pedicular width (p < 0.31), anterior pedicle width (p < 0.075) and transverse pedicle angle (p < 0.178). There was statistical significance in the difference in the width of the waist of the pedicle between right and left pedicles (p < 0.039). Pedicle widths were notably wider at its posterior and anterior ends and narrowest at the waist. The left pedicle waist outer diameter was noted to be the narrowest displaying an average measurement of 6.8 mm with a standard deviation of 0.86 mm. Average combined transverse pedicle angle was found to be 27° with a standard deviation of 0.9°.
Table 1.
Summary of C7 pedicle measurements
| Posterior pedicle width (mm) | Middle pedicle width | Anterior pedicle width (mm) | Pedicle inclination (mm) (°) | |
|---|---|---|---|---|
| Right | 9.2 ± 1.4 | 7.4 ± 0.63 | 9.6 ± 0.87 | 27.3 ± 1.1 |
| Left | 9.7 ± 0.96 | 6.8 ± 0.86 | 8.9 ± 1.4 | 26.8 ± 0.7 |
| Combined | 9.5 ± 1.2 | 7.1 ± 0.80 | 9.2 ± 1.2 | 27 ± 0.9 |
All 20 A/P images of C7 pedicles were reviewed. We observed that the marker that designated the lateral border of the pedicle at the middle portion correlated with the outer border of the opacity that represented our ellipse as seen on imaging. This verified that the elliptical density seen in the A/P image is indeed the pedicle and represented a bony overlap of the imaging beam. More importantly, the distance between the two metal markers representing the middle portion of the pedicle was the same as that represented by the ellipse on radiographs. By remaining within this elliptical border, one should be within the pedicle 100% of the time.
During surgery, a total of 55 C7 pedicle screws were successfully placed in 28 patients using this technique. Post-operative radiographs were obtained on all patients. Radiographs verified that the correct levels were instrumented and grossly verified correct positioning of the pedicle screws. In addition, 20 of 28 patients underwent CT scan of the cervical spine post-operatively. Only one pedicle screw (right) violated the lateral wall of the pedicle. Another pedicle screw (right) was found to be long and violated the anterior cortex of the vertebral body. Both patients did not display any neurovascular complications.
Complications were observed in four patients (Table 2). Patient 1 developed a right C6 radiculopathy post-operatively. A CT scan was obtained on this patient and verified that the right C7 pedicle screw was indeed within the pedicle without breech of the cortical wall. This patient underwent complete hardware removal 4.5 months later with partial resolution of symptoms. Patient 2 developed a right C8 hypersensitivity post-operatively after undergoing PLSFI C4–C7 for central canal and foraminal stenosis. A CT scan confirmed that both C7 pedicle screws did not breach the pedicle wall and the patient had complete resolution of symptoms after a brief period of observation. Patient 3 had a long-standing history of Parkinson’s disease and progressive dysphagia. Post-operatively, the patient had an acute exacerbation of dysphagia that required temporary PEG tube placement. Patient 4 developed a hematoma and wound drainage requiring wound exploration and irrigation and debridement on the second post-op day followed by an uneventful recovery.
Table 2.
Prospective study post-op complications
| Sex, age | Procedure | Diagnosis | Complication | Intervention | Resolution | |
|---|---|---|---|---|---|---|
| Patient 1 | Female, 60 | PLSFI C3–C7 | Central stenosis, DDD | R C6 radiculopathy | Removal of hardware | Partial |
| Patient 2 | Male, 46 | PLSFI C4–C7 | Central stenosis, foraminal stenosis | R C8 hypersensitivity | Observation | Complete |
| Patient 3 | Male, 52 | PLSFI C2–T3 | Parkinson’s, cervical kyphosis w/flexion deformity | Progressing dysphagia | PEG tube placement | Partial |
| Patient 4 | Male, 33 | PLSFI C4–C7 | Cervical instability, central stenosis | Post-op hematoma and wound drainage | Wound exploration w/I&D | Complete |
Discussion
Cervical pedicle screw insertion has the potential risk of causing neurovascular injury [12]. Several authors have attempted to identify suitable bony landmarks to guide the placement of screws with a view to minimize these injuries [5, 10]. Owing to the large individual variation morphometric landmarks are not reliable. The present study confirms the anatomic variability of the C7 vertebra as reported in other studies [1, 2, 4, 5, 9]. We observed that the combined transverse pedicle inclination angle to be 27° (26.1°–27.9°) with no significant difference between right and left. Panjabi et al. [9] reported similar values of left 26.7° ± 2.69° and right 33.1° ± 2.23°. Other researchers measured a transverse pedicle angulation ranging from 33.4° ± 6.6° to 45° [1, 2, 4]. The differences obtained in these studies may be related to the method of measuring the transverse pedicle angle. In our study, we measured the transverse pedicle angle from the axial image obtained from the disarticulated C7 vertebra. A specially designed morphometer with a three-dimensional coordinating system and computed tomography scans of articulated C7 vertebra have also been used to measure this angle [2, 4, 9].
We recognize the presence of a sagittal pedicle angle of the C7 vertebra; however, this angle was not measured in this study. As reported by other morphometry studies, there is normal anatomic variability of the sagittal pedicle angle [4, 9, 11]. The technique evaluated in this study obviates the need to know the exact angulation by accounting for this when obtaining the initial true A/P image of the pedicles. When adjusting the C-arm to obtain the best true A/P image, the beam of the image intensifier is parallel to the angle of the pedicles in the sagittal plane. By following the path of the beam, one remains in line with the sagittal pedicle angle.
The results of the anatomic study also confirm that the waist of the pedicle is the narrowest region of the pedicle which progressively enlarges anteriorly and posteriorly. When preparing the specimens, a gross examination of the pedicles revealed that the width of the pedicle is lesser than the height. The markers were subsequently placed along the pedicle width. Most previous anatomic studies that measured both height and width showed a slight difference favoring height [4, 9, 11]; however, Barrey et al. [2] in their study on 15 C7 specimens reported that this ratio was reversed with the width slightly greater than its height. The measurements of the pedicle width obtained in our study were comparable to previous reported values. Although we did see a significant difference between right and left middle pedicle width, we are aware of the low power of this study and the high probability of committing a type I error. A larger number of specimens would need to be examined before any final conclusion can be made between right and left differences.
Further, we have shown that the bilateral elliptical densities seen on the A/P image represent the pedicle and more specifically correlated with the mid-pedicle width. The most lateral point of this fluoroscopic density correlates with the anatomic outer cortex of the pedicle at its narrowest point which is at the middle of the pedicle. It also correlates with the perfect starting point on the posterior surface of the C7 vertebra because it falls in the middle of the pedicle at its posterior border in all of the 20 pedicles we examined. The ability to consistently locate the starting point of the C7 pedicle screw is probably the key point of this paper. By remaining within this radiographic ellipse, the surgeon remains within the pedicle itself. In addition, by obtaining a true A/P image of the pedicle prior to placement of screws, the trajectory for placement in the sagittal plane is known and is parallel to the fluoroscopic beam. The trajectory in the transverse plane should have a 25°–30° lateral to medial angulation to enable placement of the screw within the cortical confines of the pedicle. Finally, the starting point of the pedicle screw should be at the lateral border of the elliptical densities representing the pedicles on a true A/P image. Intra-operative radiographic localization of entry point is a superior technique since it considers variations in individual anatomy. In a recent article, the technique of pedicle screw application using fluoroscopic pedicle axis view has been described [12]. In the 620 cervical pedicle screws placed, perforation of the pedicle (>50% screw outside the pedicle) and exposure of the screw (<50% screw outside the pedicle) were noted in 3.9 and 9.2% screws, respectively. Although the technique used in the present study is also based on intra-operative radiographic localization we used a true AP view to guide our insertion. As stated above, the elliptical pedicle density seen in this view corresponds to the waist of the pedicle and screw placement within this density minimizes the chances of pedicular perforation. Further, we used a drill to prepare the trajectory of the pedicle screw since we felt comfortable with the end point of hard bone having placed several hundred pedicle screws using this technique in the lumbar spine. However, this procedure may be performed manually for greater tactile feedback.
The initial results of this prospective study demonstrate that the described technique is a suitable alternative for placement of pedicle screws in the C7 vertebrae. Although we reported four post-operative complications, these were not directly related to the C7 pedicle screw or the technique itself. We did have 2 clinically silent cortical wall perforations in this study (lateral pedicle wall and anterior vertebral body) in the 20 CT scans that were obtained. CT scans were only obtained on patients who agreed to undergo evaluation or if there appeared to be post-op complications due to hardware placement. This number could be higher, if CT scans were obtained on all study patients.
Preliminary data from this study shows that C7 pedicle screw placement can be safely performed in patients where a true A/P of the pedicle can be obtained. One patient with hyperparathyroidism and multiple revision surgeries was excluded from this study due to our inability to obtain an acceptable true A/P image. This technique was abandoned and the pedicle screws were placed using lamino-foraminotomies and lateral fluoroscopic imaging. A true A/P image may not always be possible due to anatomic differences between patients. When a true A/P of the pedicle cannot be obtained, we recommend abandoning this technique and using the traditional methods.
Conclusion
The biomechanical advantage of pedicle screw fixation of the cervicothoracic junction is widely accepted. However, pedicle screw fixation of the cervical spine is technically challenging, and potential intra-operative complications can have disastrous results. By adhering to the above principles, complications can be minimized with superior placement of pedicle screws. We do not advocate replacing traditional methods of C7 pedicle screw placement; but recommend this technique as an adjunct in a surgical armamentarium. Further studies of this technique on a larger cohort are required to verify the safety and efficacy of this method of screw placement. Studies that compare surgical time and radiation exposure have yet to be investigated. Nonetheless, it is our premise that this is a potentially useful technique.
Footnotes
Investigation performed at Henry Ford Hospital and Detroit Receiving Hospital, Detroit, MI, USA.
References
- 1.An HS, Gordin R, Renner K. Anatomic considerations for plate-screw fixation of the cervical spine. Spine. 1991;16:S548–S551. doi: 10.1097/00007632-199110001-00019. [DOI] [PubMed] [Google Scholar]
- 2.Barrey C, Cotton F, Jund J, Mertens P, Perrin G. Transpedicular screwing of the seventh cervical vertebra: anatomical considerations and surgical technique. Surg Radiol Anat. 2003;25:354–360. doi: 10.1007/s00276-003-0163-5. [DOI] [PubMed] [Google Scholar]
- 3.Boyle J, Singer KP, Milne N. Morphological survey of the cervicothoracic junctional region. Spine. 1996;21:544–548. doi: 10.1097/00007632-199603010-00003. [DOI] [PubMed] [Google Scholar]
- 4.Jones LE, Heller J, Silcox HD, Hutton WC. Cervical pedicle screw versus lateral mass screws: anatomic feasibility and biomechanical comparison. Spine. 1997;22(9):977–982. doi: 10.1097/00007632-199705010-00009. [DOI] [PubMed] [Google Scholar]
- 5.Karaikovic EE, Kunakornsawat S, Daubs MD, Madsen TW, Gaines RW., Jr Surgical anatomy of the cervical pedicles: landmarks for posterior cervical pedicle entrance localization. J Spinal Disord. 2000;13(1):63–72. doi: 10.1097/00002517-200002000-00013. [DOI] [PubMed] [Google Scholar]
- 6.Lee GYF, Massicotte EM, Rampersaud YR. A comparison of the “open” lamino-foraminotomy and computer-assisted techniques. J Spinal Disord Tech. 2007;20:25–32. doi: 10.1097/01.bsd.0000211239.21835.ad. [DOI] [PubMed] [Google Scholar]
- 7.Ludwig SC, Kowalski JM, Edwards CC, Heller JG. Cervical pedicle screws: comparative accuracy of two insertion techniques. Spine. 2000;25:2675–2681. doi: 10.1097/00007632-200010150-00022. [DOI] [PubMed] [Google Scholar]
- 8.Ludwig SC, Kramer DL, Balderstone RA, Vaccaro AR, Foley KF, Albert TJ. Placement of pedicle screws in the human cadaveric cervical spine: comparative accuracy of three techniques. Spine. 2000;25:1655–1667. doi: 10.1097/00007632-200007010-00009. [DOI] [PubMed] [Google Scholar]
- 9.Panjabi M, Duranceau J, Goel V, Oxland T, Takata K. Cervical human vertebra: quantitative three-dimensional anatomy of the middle and lower regions. Spine. 1991;16:861–869. doi: 10.1097/00007632-199108000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Reinhold M, Magerl F, Rieger M, Blauth M. Cervical pedicle screw placement: feasibility and accuracy of two insertion techniques based on morphometric data. Eur Spine J. 2007;16:47–56. doi: 10.1007/s00586-006-0104-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xu R, Ebraheim NA, Yeasting R, Wong F, Jackson WT. Anatomy of C7 lateral mass and projection of pedicle axis on its posterior aspect. J Spinal Disord. 1995;8:116–120. [PubMed] [Google Scholar]
- 12.Yukawa Y, Kato F, Ito K, Horie Y, Hida T, Nakashima H, Machino M. Placement and complications of cervical pedicle screws in 144 cervical trauma patients using pedicle axis view techniques by fluoroscope. Eur Spine J. 2009;18(9):1293–1299. doi: 10.1007/s00586-009-1032-7. [DOI] [PMC free article] [PubMed] [Google Scholar]