Abstract
Women going through menopause experience bone loss and increased musculoskeletal pain, including low back pain. This study explored the relationships between bone mineral density (BMD) and body mass index (BMI), postmenopausal period and outcomes of treatment for low back pain in postmenopausal Korean women. On examining the medical records of 78 postmenopausal women hospitalized for low back pain, investigators found that women with low BMD were older and had been postmenopausal for longer periods than women with normal BMD. Postmenopausal length was positively correlated with pain scores at day 15 and 20 post-admission (P = 0.011 and 0.006) and negatively correlated with T-scores (P = 0.002). BMI was positively correlated with T-scores (r = 0.283, P = 0.022). In conclusion, age, postmenopausal length and BMI correlate with BMD in Korean women suffering from LBP. Larger studies investigating the associations between menopause, BMD, BMI and LBP seem desirable. Moreover, evidence-based therapeutic approaches should be explored for BMD and LBP management.
Keywords: Bone mineral density, Menopause, Low back pain
Introduction
Menopause is commonly associated with rapid bone loss, beginning 2–3 years before and continuing for up to 3–4 years after menopause [1]. This bone loss manifests as a significant decrease in bone mineral density (BMD) measured by dual energy X-ray absorptiometry [2]. BMD is an important clinical measure of bone strength and health, and an association between reduced BMD and musculoskeletal pain is plausible [3, 4]. Musculoskeletal pain [5], and specifically LBP [6–9], is also one of the most commonly and consistently reported symptoms of women going through menopause.
Although postmenopausal women are recognized as a population of particular concern for low back pain (LBP) because of the effects of decreased estrogen level on bone mineral density (BMD) [10], limited and inconsistent data are available on postmenopausal women who suffer from chronic LBP. A study of community-dwelling middle-aged women in the USA found that postmenopausal women reported experiencing significantly greater LBP symptoms than pre- or perimenopausal women [7]. Moreover, a study of Japanese women 25–85 years of age reported that the prevalence of LBP increased in groups of older and perimenopausal women [8]. Age was also a predictor of back pain in Mexican women of menopausal age (90% between 40 and 60, mean age 50.1 years), whereas menopausal status was not [9]. However, back pain was one of the most common everyday symptoms reported by these women.
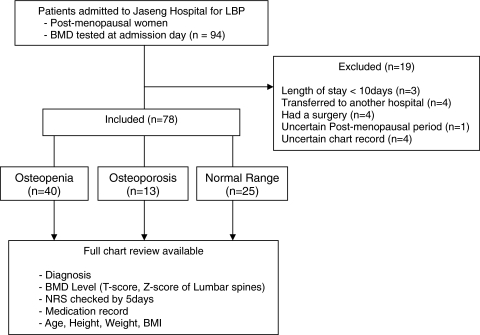
Similarly, the relationship between bone mineral density (BMD) and LBP has not been widely investigated. Compared to a normal population, patients with chronic LBP have been shown to have a lower bone density at the lumbar spine and an increased incidence of osteopenia and osteoporosis [3]. In addition, a review of data on sex and gender differences in the General Practice Research Database in England and Wales found that the incidence of radiographic vertebral fractures in women increased sharply after the age of 65 years [10]. However, limited and inconsistent data are available on risk factors for chronic LBP in postmenopausal women, including age, menopausal status and symptoms, and BMD [8]. Therefore, the relationship between BMD and LBP in postmenopausal women remains unclear. The current study aims at exploring the relationships among bone mineral density (BMD), body mass index (BMI), postmenopausal period and outcomes of treatment for low back pain in postmenopausal Korean women by analyzing the correlations between BMD and these variables (Fig. 1).
Fig. 1.
Flow chart of BMD study
Methods
This retrospective review was conducted at Jaseng Hospital in Seoul, Korea, which specializes in nonsurgical treatment of LBP, spine and joint disorders [11]. The study was approved by the hospital institutional review boards (IRB) at both Jaseng Hospital and at the University of North Carolina in Chapel Hill due to the nature of international collaboration. The medical records of women who had been treated for LBP at the Jaseng Hospital between May 2007 and February 2008 were screened for inclusion in the chart review according to the following criteria. Included were postmenopausal women with LBP symptoms, who had documented pathological, diagnostic and radiological data, BMD measured at admission, and who stayed as an inpatient for more than 10 days. The excluded women were those: who were premenopausal, perimenopausal or of uncertain menopausal status; who had osteoporotic fractures; who had a lumbar surgery previously; who were transferred to a different hospital or did not complete the treatment; or whose chart record was incomplete.
Data extracted from the participants’ charts included demographic data, medical history, LBP and osteopathic diagnoses, measures of BMD at admission, treatment modalities for LBP and postmenopausal symptoms, and routine measures of pain. Bone mineral density (BMD) was measured by dual energy X-ray absorptiometry, using a Lunar DPX Bravo Densitometer, (GE medical system, USA) at the lumbar vertebrae L1, L2, L3 and L4 [4, 12]. Average BMD values of all four vertebrae as well as computer-generated T and Z-scores were included. T-score (Z-score) is the number of standard deviations above or below the mean for a healthy 30-year-old adult (patient’s age) of the same sex and ethnicity as the patient. For the purpose of the analyses conducted in this study, women with T-scores lower than −1 were classified as having low BMD.
Outcome measures extracted from the study participants’ charts included pain NRS scores at 15 and 20 days post-admission, proportions of participants with pain NRS scores of 3 or less at the same days, length of hospital stay and all available routine pain NRS scores [13–16] at admission and every 5 days up to 50 days post-admission. The 15 and 20-day post-admission markers were chosen for this study, since such a time frame allows a sufficiently long duration to observe treatment outcomes while providing the largest hospitalized patient population possible for this review.
Data were analyzed using Stata software version 9 (StataCorp LP, College Station, TX). Participants’ characteristics, treatment modalities and outcomes for the whole sample and the two groups of osteopathic categories were described using frequencies and descriptive statistics. Differences between groups of osteopathic categories were evaluated by t test, Fisher’s test for treatment modalities and Mann–Whitney tests for pain NRS scores. Exploratory correlation analyses were performed to evaluate associations between measures of pain and other variables (Spearman’s correlations) and between measures of bone mineral density and other variables (Pearson’s correlations). A P value <0.05 represented a significant statistical difference.
Results
Participants
A total of 78 postmenopausal women with LBP met the inclusion/exclusion criteria, and their medical records were included in this study. Women included in the study were between 50 and 82 years old at admission (mean ± SD = 63.9 ± 7.5 years) and had been postmenopausal for a mean of 13.2 years (SD = 8.8). Their mean weight and height were 59.1 kg (SD = 8.3) and 156.6 cm (SD = 4.4), respectively, and their mean body mass index (BMI) was 24.1 (SD = 3.1). Most women (83.3%) complained of both leg and back pain and only 13 (16.7%) complained of LBP alone. Median length of LBP was 5 months. Several women had serious spinal pathologies, including protrusions (n = 35), extrusions (n = 14), bulging disks (n = 7), stenosis (n = 20) and spondylolisthesis (n = 13). The mean calculated overall L1–L4 BMD value was 1.02 g/cm2 (SD = 0.17), and the mean T and Z-score values were −0.85 (SD = 1.42) and 0.28 (SD = 1.22), respectively. Of the 78 participants, 52.6% (n = 41) had low BMD values (T-score < −1) and the remainder had normal BMD.
Compared to women with normal BMD, women with low BMD were significantly older and had been postmenopausal for a longer time (P = 0.003 and 0.031, respectively, Student’s t test; Table 1). Women with low BMD also had significantly lower weight and height than those with normal BMD (P = 0.033 and 0.020, respectively, Student’s t test). The two groups of women had similar treatment outcome measures (Table 1), though women with low BMD tended to have longer hospital stays and higher pain NRS scores than women with normal BMD. The proportions of women with pain NRS scores of 3 or less at 15 or 20 days post-admission were similar for the two BMD groups (Table 1).
Table 1.
Clinical characteristics, bone densitometry measurements and pain scores of participants according to categories of lumbar bone mineral density levels (mean ± SD)
| All (n = 78) | Low BMD (n = 41) | Normal BMD (n = 37) | |
|---|---|---|---|
| Age (years) | 63.9 ± 7.5 | 66.3 ± 6.9** | 61.3 ± 7.4 |
| Postmenopausal length (years) | 13.2 ± 8.8 | 15.2 ± 8.3* | 10.9 ± 9.0 |
| Weight (kg) | 59.1 ± 8.3 | 56.9 ± 7.6* | 61.2 ± 8.5 |
| Height (cm) | 156.6 ± 4.4 | 155.3 ± 4.2* | 157.8 ± 4.2 |
| Body mass index (kg/m2) | 24.1 ± 3.1 | 23.6 ± 2.8 | 24.6 ± 3.3 |
| Proportion overweight (%, n) | 39.4 (26) | 39.4 (13) | 39.4 (13) |
| Proportion obese (%, n) | 16.7 (11) | 9.1 (3) | 24.2 (8) |
| Bone mineral density L1–L4 (g/cm2) | 1.02 ± 0.17 | 0.889 ± 0.076 | 1.160 ± 0.135 |
| T-score L1–L4 | −0.85 ± 1.42 | −1.89 ± 0.61 | 0.34 ± 1.10 |
| Z-score L1–L4 | 0.28 ± 1.22 | −0.46 ± 0.71 | 1.12 ± 1.12 |
| Pain NRS score at admission | 7.4 ± 2.0 | 7.4 ± 2.0 | 7.3 ± 2.0 |
| Length of hospital stay (days) | 29.7 ± 12.6 | 30.9 ± 13.9 | 28.3 ± 11.2 |
| Proportion discharged before day 15 | 12.8 (10) | 9.8 (4) | 16.2 (6) |
| Proportion discharged before day 20 | 26.9 (21) | 22.0 (9) | 32.4 (12) |
| Last recorded pain NRS score at day 15 | 4.5 ± 2.1 | 4.6 ± 2.5 | 4.3 ± 1.8 |
| Last recorded pain NRS score at day 20 | 4.0 ± 2.0 | 4.1 ± 2.2 | 3.8 ± 1.6 |
| Proportion with pain NRS score of 3 or less | |||
| At day 15 | 32.5 (25) | 34.2 (14) | 30.6 (11) |
| At day 20 | 41.6 (32) | 41.5 (17) | 41.7 (15) |
Z-score: the number of standard deviations above or below the mean for the patient’s age, sex and ethnicity
T-score: the number of standard deviations above or below the mean for a healthy 30-year-old adult of the same sex and ethnicity as the patient
* P < 0.05, Student’s t test
** P < 0.005, Student’s t test
BMD bone mineral density;
NRS numeric rating scale
Association analyses
Age, postmenopausal length and BMI were all significantly correlated with T-scores (Table 2). In the case of age and postmenopausal length, the correlations were negative, suggesting that BMD decreased as these women aged, or as the time since their menopause increased. Interestingly, BMI was positively correlated with T-scores, indicating that women with higher BMI in this population also had higher BMD. There were no significant correlations between T-scores and pain NRS scores recorded at 15 or 20 days post-admission (Table 2). Neither BMI nor age was correlated with pain NRS scores, though postmenopausal length was.
Table 2.
Pearson’s correlations between measures of pain or bone mineral density levels and other variables (NRS numeric rating scale; r correlation coefficient)
| Last recorded pain NRS score at | ||||||
|---|---|---|---|---|---|---|
| Day 15 | Day 20 | T-score L1–L4 | ||||
| r | P | r | P | r | P | |
| Bone mineral density L1–L4 (g/cm2) | −0.220 | 0.056 | −0.197 | 0.089 | N/A | N/A |
| T-score L1–L4 | −0.214 | 0.063 | −0.192 | 0.096 | ||
| Z-score L1–L4 | −0.156 | 0.178 | −0.134 | 0.248 | ||
| Age (years) | 0.202 | 0.078 | 0.254 | 0.026 | −0.432 | <0.001 |
| Postmenopausal length (years) | 0.288 | 0.011 | 0.313 | 0.006 | −0.351 | 0.002 |
| Weight (kg) | 0.021 | 0.867 | 0.105 | 0.405 | 0.407 | 0.001 |
| Height (cm) | −0.043 | 0.735 | 0.020 | 0.877 | 0.365 | 0.003 |
| Body mass index (kg/m2) | 0.040 | 0.750 | 0.113 | 0.372 | 0.283 | 0.022 |
| Pain NRS score at admission | 0.454 | <0.001 | 0.386 | <0.001 | −0.097 | 0.401 |
| Length of hospital stay (days) | 0.407 | <0.001 | 0.365 | 0.001 | −0.156 | 0.176 |
| Last recorded pain NRS score | ||||||
| At day 15 | 1.000 | N/A | −0.214 | 0.063 | ||
| At day 20 | 0.908 | <0.001 | 1.000 | N/A | −0.192 | 0.096 |
Bold values indicate statistical significance
There were no statistically significant correlations between measures of bone mineral density (T or Z-score) and pain at day 15 and 20 (Pearson’s correlations, Table 2) in this group of postmenopausal women.
Discussion
This study found several meaningful correlations and trends involving BMD, menopause and pain: women with low BMD had longer postmenopausal length, which was positively correlated with pain NRS scores at 15 and 20 days post-admission, although there was no correlation between BMD and recorded pain scores. It was also found that BMI was positively correlated with T-scores, and a negative correlation between T-scores and pain NRS scores at 15 days post-admission was almost significant.
These findings support a number of previous studies on BMD, menopause and LBP. Several reports similarly displayed that the time since menopause was negatively correlated with BMD [17, 18]. The longer the postmenopausal period, the more likely was the participant to have a lower BMD, probably due to the increased bone loss suffered during the longer postmenopausal period. However, in contrast to the above studies, this retrospective review also found age to be correlated with lower BMD, which was consistent with another large population-based Korean study [19]. While postmenopausal length and age are not necessarily synonymous, this study shows that both are significant factors to consider in studies on BMD. More importantly, this study’s findings that postmenopausal period was positively correlated with pain scores supports previous arguments,that physicians should address BMD changes [18] and quality of life measures[20] in postmenopausal women with LBP regardless of the presence of fractures.
There are conflicting claims in literature about the relationship of BMI with BMD and LBP. A recent study of Australian community-dwelling women reported a positive association between high BMI and both high LBP intensity and disability [21]. An Italian study found that patients with high BMI were at greater risk of fractures regardless of high BMD [22]. In contrast, other studies note that those with high BMI are not at risk for fractures [23]. Our findings further shed light on both sides of the discussion in that, while there was a positive correlation between BMI and BMD T-scores, indicating that mild high BMI would be protective in maintaining higher BMD, BMI was not significantly associated with LBP intensity at admission or with efficiency of pain reduction. However, these findings could be specific to our Korean population in that most women in the current study were of normal weight (43.8% with BMI between 18.5 and 23, n = 29), 25.8% were slightly overweight (BMI between 25 and 30, n = 17) and only 3 had a BMI over 30. Moreover, there was a trend in BMI values decreasing from the normal, to the lower BMD group, though BMI values did not significantly differ between the two BMD categories. This interesting observation is in accordance with a previous study [24] and should be investigated further, especially looking for the role of fat-soluble vitamins, such as vitamins A, D and K, in a potential association between adiposity and BMD.
Considering the previous body of literature, this study exhibits several strengths. Given that LBP and the factors affecting LBP manifest themselves differently for different populations, this study provides a Korean case study to add to the body of knowledge. While this is a Korean women-specific study, it also poses broader implications: it is one of the few to incorporate treatment outcomes and efficiency of pain reduction into the analysis of factors of LBP in postmenopausal women. Furthermore, this study evidenced that postmenopausal women with a longer duration of menopause are an at-risk population not only for osteoporosis, osteopenia, fractures and other risks related to low BMD, but also to the reduced efficiency of LBP treatment.
However, there are also limitations: one is that the measured lumbar spine BMD might have increased due to calcifications related to the spinal pathologies present in this study’s population. This may explain why the trends identified did not reach statistical significance. While exclusion of patients with these serious spinal pathologies is one option in a future study, further research into a specific spinal pathology and its correlation to BMD, BMI, menopausal period and LBP treatment outcome is another potential direction for future research. In a recent survey of healthy postmenopausal Korean women, fracture risk based on lumbar BMD was not found to be associated with self-reported LBP status [25]. Therefore, additional BMD measures taken at non-spinal sites, such as the hip, might be helpful to investigate the relationship between BMD and LBP in this population. Moreover, our relatively small sample size and the nature of a retrospective study where variable factors could not be controlled are also weaknesses to consider and areas where future research could expand.
In summary, age, postmenopausal length and BMI correlate with BMD in Korean women suffering from LBP. Larger studies investigating the associations between menopause, BMD, BMI and LBP seem desirable. Moreover, evidence-based therapeutic approaches should be explored for BMD and in LBP management.
Acknowledgments
The authors thank Margeaux Akazawa, Julie Omohundro and Katie Smith for their assistance in the preparation of this manuscript. This study was supported by the Jaseng Medical foundation (JP).
Conflict of interest Drs. Joonshik Shin, Yousuk Youn, Eunseok Jin, Soonsung Hong, Sangho Lee and Sunkyu Yeom were employed at the Jaseng Hospital during the period of the study.
References
- 1.Recker R, Lappe J, Davies K, Heaney R. Characterization of peri-menopausal bone loss: a prospective study. J Bone Miner Res. 2000;15:1965–1973. doi: 10.1359/jbmr.2000.15.10.1965. [DOI] [PubMed] [Google Scholar]
- 2.Gallager JC. Effect of early menopause on bone mineral density and fractures. Menopause. 2007;14:567–571. doi: 10.1097/gme.0b013e31804c793d. [DOI] [PubMed] [Google Scholar]
- 3.Gaber TA-ZK, McGlashan KA, Love S, Jenner JR, Crisp AJ. Bone density in chronic low back pain: a pilot study. Clin Rehabil. 2002;16:867–870. doi: 10.1191/0269215502cr558oa. [DOI] [PubMed] [Google Scholar]
- 4.Briggs AM, Straker LM, Wark JD. Bone health and back pain: what do we know and where should we go? Osteoporos Int. 2009;20:209–219. doi: 10.1007/s00198-008-0719-7. [DOI] [PubMed] [Google Scholar]
- 5.Freeman EW, Sammuel MD, Lin H, Gracia CR, Pien GW, Nelson DB, Sheng L. Symptoms associated with menopausal transition and reproductive hormones in midlife women. Obstet Gynecol. 2007;110:230–240. doi: 10.1097/01.AOG.0000270153.59102.40. [DOI] [PubMed] [Google Scholar]
- 6.Adera T, Deyo RA, Donatelle RJ. Premature menopause and low back pain. A population-based study. Ann Epidemiol. 1994;4:416–422. doi: 10.1016/1047-2797(94)90077-9. [DOI] [PubMed] [Google Scholar]
- 7.Dugan SA, Powell LH, Kravitz HM, Everson Rose SA, Karavolos K, Luborsky J. Musculoskeletal pain and menopausal status. Clin J Pain. 2006;22:325–331. doi: 10.1097/01.ajp.0000208249.07949.d5. [DOI] [PubMed] [Google Scholar]
- 8.Manabe T, Takasugi SI, Iwamoto Y. Positive relationship between bone mineral density and low back pain in middle-aged women. Eur Spine J. 2003;12:596–601. doi: 10.1007/s00586-003-0585-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sievert LL, Goode-Null SK. Musculoskeletal pain among women of menopausal age in Puebla, Mexico. J Cross Cult Gerontol. 2005;20:127–140. doi: 10.1007/s10823-005-9087-3. [DOI] [PubMed] [Google Scholar]
- 10.Geusens P, Dinant G. Integrating a gender dimension into osteoporosis and fracture risk research. Gene Med. 2007;4:S147–S161. doi: 10.1016/s1550-8579(07)80055-6. [DOI] [PubMed] [Google Scholar]
- 11.Stevens L, Duarte H, Park J. Promising implications for integrative medicine for back pain: a profile of a Korean hospital. J Altern Complement Med. 2007;13(5):481–484. doi: 10.1089/acm.2007.6263. [DOI] [PubMed] [Google Scholar]
- 12.Prakash LV, Prabhu VV, Saralaya MM, Pai AV, Singh G, Madhyastha S. Vertebral body integrity: a review of various anatomical factors involved in the lumbar region. Osteoporos Int. 2007;18:891–903. doi: 10.1007/s00198-007-0373-5. [DOI] [PubMed] [Google Scholar]
- 13.Downie WW, Leatham PA, Rhind VM, et al. Studies with pain rating scales. Ann Rheum Dis. 1978;37:382–384. doi: 10.1136/ard.37.4.382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jensen MP, Turner JA, Romano JM. What is the maximum number of levels needed in pain intensity measurement? Pain. 1994;58:387–392. doi: 10.1016/0304-3959(94)90133-3. [DOI] [PubMed] [Google Scholar]
- 15.Price DD, Bush FM, Long S, Harkins SW. A comparison of pain measurement characteristics of mechanical visual analogue and simple numerical rating scales. Pain. 1994;56:217–226. doi: 10.1016/0304-3959(94)90097-3. [DOI] [PubMed] [Google Scholar]
- 16.Katz J, Melzack R. Measurement of pain. Surg Clin North Am. 1999;79:231–252. doi: 10.1016/S0039-6109(05)70381-9. [DOI] [PubMed] [Google Scholar]
- 17.Francucci CM, Romagni P, Camilletti A, Fiscaletti P, Amoroso L, Cenci G, Morbidelli C, Boscaro M. Effect of natural early menopause on bone mineral density. Maturitas. 2008;59(4):323–328. doi: 10.1016/j.maturitas.2008.03.008. [DOI] [PubMed] [Google Scholar]
- 18.Hassa H, Tanir HM, Senses T, Oge T, Sahin-Mutlu F. Related factors in bone mineral density of lumbal and femur in natural postmenopausal women. Arch Gynecol Obstet. 2005;273(2):86–89. doi: 10.1007/s00404-005-0015-0. [DOI] [PubMed] [Google Scholar]
- 19.Cui LH, Choi JS, Shin MH, Kweon SS, Park KS, Lee YH, Nam HS, Jeong SK, Im JS. Prevalence of osteoporosis and reference data for lumbar spine and hip bone mineral density in a Korean population. J Bone Miner Metab. 2008;26(6):609–617. doi: 10.1007/s00774-007-0847-8. [DOI] [PubMed] [Google Scholar]
- 20.Bianchi ML, Orsini MR, Saraifoger S, Ortolani S, Radaelli G, Betti S. Quality of life in post-menopausal osteoporosis. Health Qual Life Outcomes. 2005;1:3–78. doi: 10.1186/1477-7525-3-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Urquhart DM, Bell R, Cicuttini FM, Cui J, Forbes A, Davis SR. Low back pain and disability in community-based women: prevalence and associated factors. Menopause. 2009;16:24–29. doi: 10.1097/gme.0b013e31817e5ce0. [DOI] [PubMed] [Google Scholar]
- 22.Pirro M, Fabbriciani G, Leli C, Callarelli L, Manfredelli MR, Fioroni C, Mannarino MR, Scarponi AM, Mannarino E. High weight or body mass index increase the risk of vertebral fractures in postmenopausal osteoporotic women. J Bone Miner Metab. 2010;28(1):88–93. doi: 10.1007/s00774-009-0108-0. [DOI] [PubMed] [Google Scholar]
- 23.Pesonen J, Sirola J, Tuppurainen M, Jurvelin J, Alhava E, Honkanen R, Kroger H. High bone mineral density among perimenopausal women. Osteoporos Int. 2005;16(12):1899–1906. doi: 10.1007/s00198-005-1958-5. [DOI] [PubMed] [Google Scholar]
- 24.Gnudi S, Sitta E, Fiumi N. Relationship between body composition and bone mineral density in women with and without osteoporosis: relative contribution of lean and fat mass. J Bone Miner Metab. 2007;25(5):326–332. doi: 10.1007/s00774-007-0758-8. [DOI] [PubMed] [Google Scholar]
- 25.Ahn S, Song R. Bone mineral density and perceived menopausal symptoms: factors influencing low back pain in postmenopausal women. J Adv Nurs. 2009;65:1228–1236. doi: 10.1111/j.1365-2648.2009.04983.x. [DOI] [PubMed] [Google Scholar]