Abstract
The impact of sagittal plane alignment on the treatment of spinal disorders is of critical importance. A failure to recognise malalignment in this plane can have significant consequences for the patient not only in terms of pain and deformity, but also social interaction due to deficient forward gaze. A good understanding of the principles of sagittal balance is vital to achieve optimum outcomes when treating spinal disorders. Even when addressing problems in the coronal plane, an awareness of sagittal balance is necessary to avoid future complications. The normal spine has lordotic curves in the cephalad and caudal regions with a kyphotic curve in between. Overall, there is a positive correlation between thoracic kyphosis and lumbar lordosis. There are variations on the degree of normal curvature but nevertheless this shape allows equal distribution of forces across the spinal column. It is the disruption of this equilibrium by pathological processes or, as in most cases, ageing that results in deformity. This leads to adaptive changes in the pelvis and lower limbs. The effects of limb alignment on spinal posture are well documented. We now also know that changes in pelvic posture also affect spinal alignment. Sagittal malalignment presents as an exaggeration or deficiency of normal lordosis or kyphosis. Most cases seen in clinical practise are due to kyphotic deformity secondary to inflammatory, degenerative or post-traumatic disorders. They may also be secondary to infection or tumours. There is usually pain and functional disability along with concerns about self-image and social interaction due to inability to maintain a horizontal gaze. The resultant pelvic and lower limb posture is an attempt to restore normal alignment. Addressing this complex problem requires detailed expertise and awareness of the potential pitfalls surrounding its treatment.
Keywords: Sagittal, Deformity, Alignment, Angles, Management
Introduction
The impact of sagittal plane alignment on the treatment of spinal disorders is of critical importance. A failure to recognise malalignment in this plane can have significant consequences for the patient not only in terms of pain and deformity but also social interaction due to deficient forward gaze. A good understanding of the principles of sagittal balance is vital to achieve optimum outcomes when treating spinal disorders. Even when addressing problems in the coronal plane, an awareness of sagittal balance is necessary to avoid future complications. The normal spine has lordotic curves in the cephalad and caudal regions with a kyphotic curve in between. Overall, there is a positive correlation between thoracic kyphosis and lumbar lordosis [50]. There are variations on the degree of normal curvature [4, 6, 22, 38] but nevertheless this shape allows equal distribution of forces across the spinal column. It is the disruption of this equilibrium by pathological processes or ageing that result in deformity. This leads to adaptive changes in the pelvis and lower limbs. The effects of limb alignment on spinal posture are well documented [1, 14, 17, 24, 37]. We now also know that changes in pelvic posture also affect spinal alignment [50].
Sagittal malalignment presents as an exaggeration or deficiency of normal lordosis or kyphosis. Most cases seen in clinical practise are due to kyphotic deformity secondary to inflammatory, degenerative or post traumatic disorders. They may also be secondary to infection or tumours. There is usually pain and functional disability along with concerns about self-image and social interaction due to inability to maintain a horizontal gaze. The resultant pelvic and lower limb posture is an attempt to restore normal alignment. Addressing this complex problem requires detailed expertise and awareness of the potential pitfalls surrounding its treatment.
The aim of this article is to incorporate the basic definitions of sagittal plane deformity with the multi-faceted issues associated with its diagnosis and treatment as well as challenge conventional thinking on what should constitute the normal sagittal profile.
Historical perspective
The Scoliosis research society (SRS) has previously described [41] normal sagittal balance as occurring when a plumb line drawn from the centre of the body of C7 lies within ±2 cm of the sacral promontory. Different authors have described numerous indices for measuring changes in sagittal balance [13, 17, 24, 37, 48, 50]. Suk et al. [45] described the importance of the chin-brow angle for cervical spine osteotomy, however, they did not take into account postural changes in the pelvis and lower limbs. Van Royen et al. [50] described radiological indices which take into consideration the angle of the sacral slope and its deviation from the norm. Hahn et al. [20] presented the concept of whole body kyphosis angle which does accommodate limb and pelvic changes. However, the thoracic kyphosis angle was measured from T4 to T12 which is not always fully representative of the total amount of kyphosis. Duval-Beaupere and Legaye [31] introduced the concept of ‘optimal lordotic positioning’ and ‘correctly oriented pelvis’ values. They compared a control group of 49 asymptomatic adults to a group of 66 adult females with scoliosis and were able to show, using regression coefficients, a close relationship between pelvic and spinal parameters. During [14] had earlier reported a constant pelvic measurement for morphology on standing lateral radiographs called the pelvisacral angle. Both of these studies had a limiting factor of methodology. Jackson [25, 26] more recently described pelvic morphology using the pelvic radius technique and subsequently compared the reliability of each of these three measurements. An earlier study by Fisher et al. [18] identified the centre of pelvic rotation to be along an axis through the centre of the femoral head. In a recent paper, Schwab et al. [40] stressed the important role played by pelvic parameters in regulating standing balance.
Nomenclature
Sagittal plane deformity can be assessed clinically and radiographically. The advantage of the radiographic markers is that they provide an objective evaluation of the magnitude of the deformity and degree of correction required to restore balance.
These markers document the position of the head, orientation of gaze, characteristics of the thoracic and lumbar profiles and the orientation of the pelvis. Deformity correction results in changes to both coronal and sagittal planes, and thus the accurate measurement of these markers is dependent on obtaining the correct imaging with careful positioning of the patient.
Each of the relevant radiographic markers are described below.
Sagittal vertical axis (SVA) (Fig. 1)
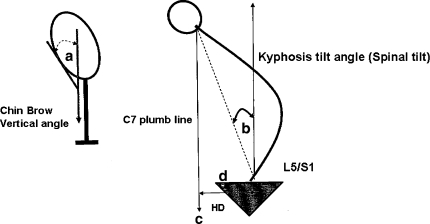
Fig. 1.
a Chin-brow vertical angle, b Kyphosis tilt angle, c C7 plumb line (sagittal vertical axis), d Horizontal distance (HD) of displaced sagittal vertical axis from reference point on sacral end plate
This is used to document the location of the head with respect to the normal centre of gravity (offset of the head from the sacral promontory). This is identified by a plumb line dropped from C7 to the sacral end plate. There is controversy as to the distal boundaries of this line as it has been described as central, anteroposterior or anterosuperior by different authors. This only influences the reciprocal distance to the SVA but not the principle of measurement [50].
Chin-brow vertical angle (Fig. 1)
This angle is measured between a line from the brow to the chin and the vertical axis, when the patient stands with hips and knees extended and the neck in a neutral or fixed position [6]. In kyphosis, this axis tilts forward resulting in poor horizontal gaze. This is a postural angle.
C7 plumb line (Fig. 1)
This is a vertical line drawn from the vertebral body of C7. It should normally intersect the superior endplate of S1.
Kyphosis tilt angle and Spinal tilt angle (Fig. 1)
The kyphosis tilt angle is the angle between the vertical axis and a line drawn from the centre of C7 to the centre of the inferior kyphotic vertebral body. This angle describes the tilt induced by global kyphosis. When the lowermost vertebra in the curve is L5, the kyphosis tilt angle is equivalent to the spinal tilt angle (T1–S1 angle). Both these angles are postural and will vary with lower limb position.
Pelvic incidence (Fig 2)
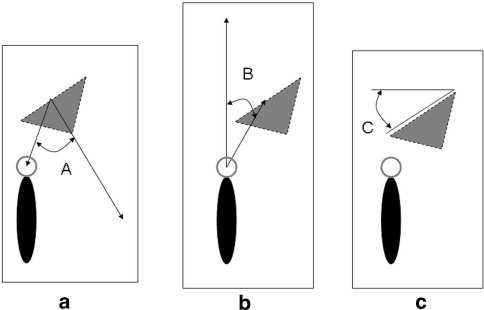
Fig. 2.
The 3 main pelvic parameters. When measuring pelvic incidence, the reference point is the centre of the femoral head (if the femoral heads superimpose) or the mid point of the line connecting the femoral heads (if they do not superimpose)
This is the angle subtended by the perpendicular to the sacral plate at its mid-point and a line from the mid-point of the sacral plate to the centre of the femoral head.
Pelvic tilt (Fig. 2)
This is the angle between a vertical line originating at the centre of the femoral head and a line starting from the centre of the femoral head to the midpoint of the endplate of S1. In simple terms, this angle describes the rotation of the pelvis around the femoral heads.
Sacral slope (Fig. 2)
This is the angle between the superior endplate of S1 and a horizontal axis.
Spino-pelvic angle (Fig. 3)
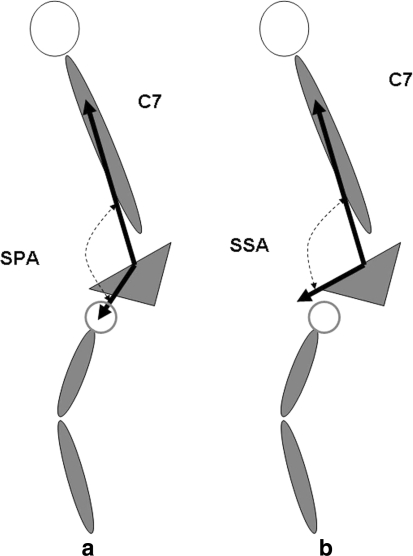
Fig. 3.
a Spino-pelvic angle and b Spino-sacral angle
This is the angle between a line from the centre of C7 to the centre of the sacral endplate and a line from the centre of the sacral endplate to the centre of the femoral head. This angle increases in kyphosis and is therefore a postural angle.
Spino-sacral angle (Fig. 3)
This is the angle between a line from the centre of C7 to the centre of the sacral endplate and the surface of the sacral endplate. In a healthy population, this angle strongly correlates with the sacral slope (Pearson correlation coefficient) and does not change. It is therefore a fixed angle.
The descriptive nomenclature of alignment angles can be seen to be divided largely into two groups: The postural group, which varies with compensatory changes in alignment and the fixed group, which does not vary. There is a third group described as the mixed group, which are usually the cases where surgical fusion has altered the overall shape of the spine.
Normal values for spinal alignment
In normal individuals, the Chin-brow vertical angle is close to zero. The pelvic incidence angle measures approximately 52° with a range from 34° to 84° [48, 50]. After skeletal maturity, this angle is fixed. The pelvic tilt angle measures 12° with a range of 5°–30° [50]. This angle changes with compensatory posture and is therefore a postural angle. Sacral slope is approximately 40° with a range of 20°–65° [48, 50]. This angle also changes with compensatory posture and is therefore a postural angle. There is a geometrical relationship between the pelvic angles and sacral slope such that Pelvic incidence is equal to the sum of the angles of sacral slope and pelvic tilt (PI = SS + PT).
There are varying reports in the literature on normal values for acceptable kyphosis or lordosis in the spine [4, 6, 22]. In the cervical spine, acceptable lordosis is 40° ± 9.7°. Thoracic kyphosis is between 20° and 50°. Due to radiographic constraints in obtaining suitable exposure of T1–T3 levels, it is often difficult to assess the full extent of thoracic kyphosis as estimations are frequently made from lower levels. To obtain an accurate measurement, the upper and lower maximally angulated vertebrae must be included. The thoracolumbar junction is relatively flat. Normal lumbar lordosis ranges from 31° to 79° from L1 to S1. This range may vary depending on the inclusion of the lumbosacral junction in the measurement. The L5–S1 motion segment has a large degree of lordosis.
Spinopelvic relationship
Many studies have highlighted the relationship of the spine and pelvis in the standing balance in normal adults and children particularly through the effect of lumbar lordosis [51, 52]. Schwab et al. [40] described the gravitational line to remain fairly constant with age, however, the degree of thoracic kyphosis associated with age would shift the plumb line anteriorly with a compensatory retroversion of the pelvis increasing the pelvic tilt to keep the gravitational line constant and maintain adequate sagittal balance. A prospective study conducted by Mac-Thiong et al. [33] found a positive correlation between PI and age during childhood and adolescence before stabilising in adult life. They hypothesised that this would maintain an adequate sagittal balance through the physical and physiological changes during growth and puberty. It should be noted that Pelvic tilt also increased with age with the sacral slope remaining fairly constant. Furthermore, it has been proved that the relationship of one anatomical portion of the spine is interdependent on its adjacent structure particularly at the lumbar-pelvic level. Compensatory mechanisms will maintain an adequate sagittal balance whilst minimising energy expenditure which has been shown in both children and adults.
Spine and age
Vendatam et al. [55] demonstrated that the mean sagittal vertical axis (SVA) shifts forward in the ageing population from −5.6 cm in adolescents to −3.2 cm in the middle aged and elderly population. A strong correlation exists between a positive shift in the SVA and a loss of lumbar lordosis and the onset of symptoms in patients, such as back pain and fatigue. Moreover, Glassman et al. [15, 19] demonstrated that a positive sagittal imbalance was the most reliable radiographic predictor and indicator of clinical health status. It was shown in 352 patients that a mildly positive sagittal imbalance is detrimental with a linear fashion increase in symptoms with progressive sagittal imbalance. It is of note that disability was worse amongst those with a degree of kyphosis in their lumbar spine in comparison to the normal and lordotic lumbar spines. The causes of sagittal spine imbalance are multi-factorial and these range from iatrogenic causes to genetic and metabolic causes.
Variations of spinal alignment
The aim of treatment of sagittal malalignment is to restore normal balance. From the figures presented in the previous section, it is obvious that there are wide variations on what is considered normal. To this effect, the senior author [38] studying a group of 160 asymptomatic individuals has identified four patterns of variation of normal sagittal alignment (see below). This was done using a computer generated 3 dimensional model. The conventional method of delineating thoracic kyphosis from lumbar lordosis based on anatomical landmarks such as the thoraco-lumbar junction is overly simplistic. The advantage of this new method is that the segments are defined by the change in spatial relationship between the vertebral bodies. The point at which this occurs is called the inflection point. The distal extent of the lumbar curve is defined by the antero-superior aspect of S1. This mirrors the Cobb method in the coronal plane. It gives a more accurate definition of each sagittal curve and the number of vertebral bodies in kyphosis and lordosis. The four groups in this classification system are based on the observation that there are characteristic sagittal profiles that occur subsequent to the orientation of the pelvis, lumbosacral junction and sacrum.
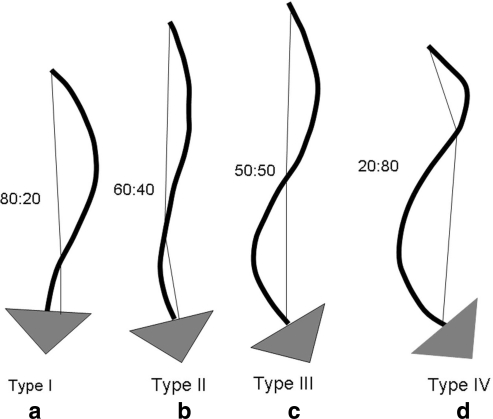
Type 1 lordosis (Fig. 4): The inflection point, i.e. the point at which the orientation of the vertebral bodies changes is at the L3/L4 level. The sacral slope is less than 35° and the pelvic incidence is small. Note the thoracolumbar kyphosis. Also, note the long kyphotic curve and short lordotic curve using this classification compared to conventional delineation between thoracic and lumbar segments. There is an 80:20 split of the total thoracolumbar length.
Fig. 4.
Variations of spinal alignment. Types I–IV. Note the thoracolumbar split (as a measure of length ratio of the thoracic and lumbar curves) in each type: a Type I 80:20, b type II 60:40 c type III 50:50, d 20:80
Type 2 lordosis (Fig. 4): The inflection point is higher at the L1–L2 level. The sacral slope is less than 35° and the pelvic incidence is small. The length of the kyphotic curve is shorter and the lordotic curve is longer, i.e. contains more vertebral bodies. There is a 60:40 split of the total thoracolumbar length. Despite the longer lordotic curve, the lumbar spine has a flat back appearance.
Type 3 lordosis (Fig. 4): The inflection point is at T12–L1. The sacral slope is between 35° and 45°. Pelvic incidence is high. The length of the kyphotic and lumbar curves is almost equal, i.e. 50:50 split. The spine is well balanced.
Type 4 lordosis (Fig. 4): The inflection point is at T9–T10. The sacral slope is greater than 45°. There is a high pelvic incidence. The lordotic curve is longer than the kyphotic curve. There is a reversed 20:80 split of the thoracolumbar column.
Clinical presentation
There is a tri-modal age distribution of sagittal plane deformities. The first group is found in the latter part of teenage years, usually secondary to Scheuermann’s kyphosis. Although Scheuermann’s Kyphosis is predominant in adolescence, undiagnosed patients often present in adulthood with an exaggerated kyphosis. The second group occurs in the 40–50 year age range, commonly due to inflammatory disorders such as ankylosing spondylitis. The last group is in the over 60s, where the commonest problem is degenerative arthritis of the spine. The centre of gravity line in the standing position lies just in front of the thoracic spine. There is therefore a natural tendency for the upper trunk to move forwards but this is counterbalanced by the lordotic lumbar spine. The integrity of the intervertebral discs is important in maintaining this profile. In pathological states, there is collapse of the disc height which leads to a loss of the normal sagittal curves and a straighter profile which is not biomechanically efficient. This is similarly found in physiological ageing of the spine.
This means that the centre of gravity line moves more anteriorly in relation to the spinal column [19]. The lack of ability of the pelvis to compensate for this along with the increased lumbar lordosis leads to constant strain on the patient trying to maintain an erect posture. Affected individuals will often report deformity, fatigue and pain in the spine, buttocks and thighs which is often made worse by prolonged activity.
The reasons for presentation are pain, deformity, functional disability and loss of horizontal gaze, all of which contribute to diminishing social independence. The problems are two-fold: the primary deformity caused by sagittal imbalance and the compensatory changes in the position of the pelvis (Fig. 5) and lower extremities. The deformity results in a downward tilt of the head with consequent inability to see above the horizon. The centre of gravity (C7 plumb line) moves anteriorly giving rise to a stooped posture. In an attempt to correct this socially inept position, the patient tilts the pelvis backwards, extends the hips, flexes the knees and dorsiflexes the ankles to try and shift the entire rigid spine backwards in order to maintain an upright posture (Fig. 6). In simplistic terms, this situation can be likened to a circus ringmaster with a whip, in order to effectively attain a cracking sound, first, by straightening and then curling the whip, the wrist needs to be cocked backwards with the elbow flexed to get the full length of the whip straight. If we were to imagine the flexible end of the whip as the spine drooping forwards, the hand as the pelvis, the extensor surface of the arm as the front of the lower limb, with the elbow in place of the knee, this compensatory mechanism becomes easier to understand. However, if we were to walk around all day with a cocked wrist and flexed elbow the comfort and social implications would not be favourable to say the least! By the same token, the compensated position of the pelvis and lower limbs is biomechanically inefficient and painful causing early fatigue and poor exercise tolerance. The ability of the spine to compensate for this deformity is governed by the patients’ intrinsic pelvic morphology as defined by the pelvic incidence. By tilting the pelvis backwards, the sacral slope is decreased. As discussed previously, SS + PT = PI. The importance of this equation is that the ability of the individual to vary the SS or PT to compensate for sagittal imbalance depends on the size of PI. Those with a large pelvic incidence are able to compensate for a kyphotic deformity by inducing a large posterior tilt and reducing the sacral slope. Conversely, those with a small pelvic incidence do not have adequate capacity to induce the amount of pelvic tilt required to restore balance (Fig. 7). This interpretation can be taken a step further to imply that patients with low pelvic incidence and sagittal plane deformities are likely to present earlier due to lack of or deficiency of this compensatory mechanism.
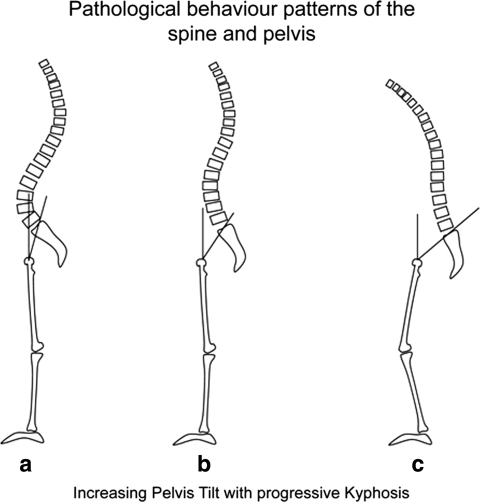
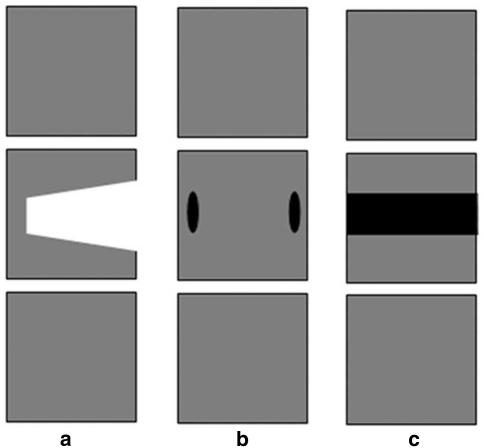
Fig. 5.
Pathological behaviour pattern of pelvis in presence of kyphosis shows a normal posture, b abnormal posture, and c compensatory posture. Pelvic tilt increases in order to maintain an upright posture
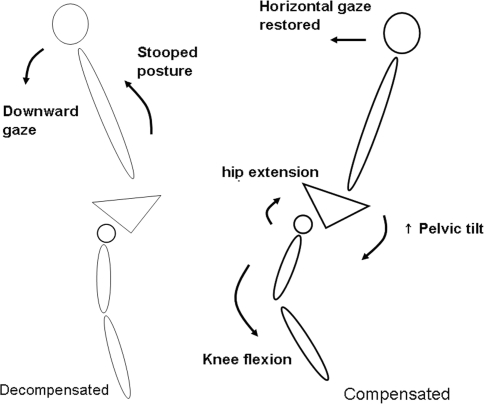
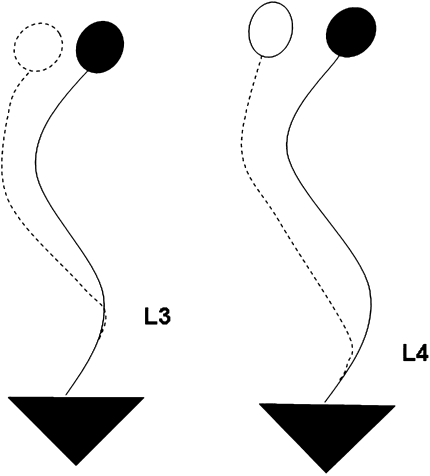
Fig. 6.
Sagittal plane imbalance. Decompensated posture on the left versus compensated posture on the right. Note change in lower limb profile with extension of hip joints and flexion of knees
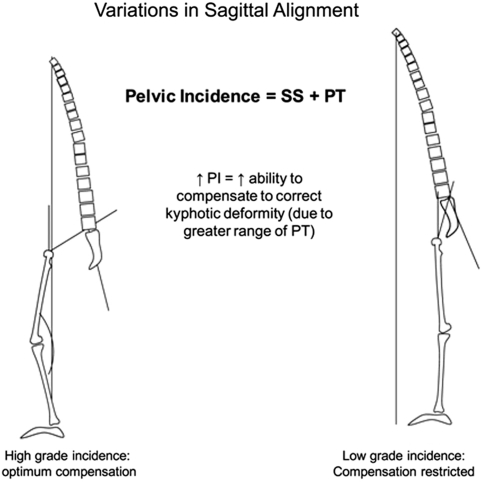
Fig. 7.
Demonstration of relationship between pelvic incidence and pelvic tilt in compensatory adjustment for kyphosis. Smaller pelvic incidence indicates less compensatory ability
Investigations
The mainstay of investigation apart from clinical evaluation is radiological imaging. This requires full length 36 inch standing postero-anterior (PA) and lateral radiographs of the spine. The PA views should show C0 to the femoral heads and the entire rib cage from right to left. The knees are locked and shoulder width apart. If a leg length discrepancy of greater than 2 cm is present, a standing block should be used. The lateral view should include C0 to the femoral head as a minimum. On plain standing lateral xrays, sagittal balance is measured with the patient ideally standing fully erect with knees and hips in full extension to counteract all compensatory mechanisms with attention to upper limb posture. This is because the position of the arms at the time of x-ray can have a bearing on sagittal alignment. Horton et al. [24] describe the “fist on Clavicle” approach as the optimal position for radiographic acquisition of key vertebral landmarks. This is a routine practise in the second author’s institution. In the senior author’s institution, the arms are rested on a specially designed support to optimise the sagittal assessment.
Optional views to help with surgical decision making to determine the flexibility of the deformity include fulcrum bend and hyperextension cross table lateral views for the thoracic spine and knee to chest position for the lumbar spine. In the coronal plane, traction views can be used.
Treatment options
Most of these patients will present to tertiary centres following a period of conservative management. These patients complain of a significantly diminished quality of life with pain and severe functional restrictions as well as cosmetic deformity. Those with flexible deformities may respond to a period of intensive physiotherapy, but this is unlikely in patients with a fixed deformity. Both groups with careful counselling can be considered for surgery if conservative measures fail.
Operative considerations
Some of these patients will have existing co-morbidities which must be optimised prior to any surgery. Multi-disciplinary input is therefore required. Many techniques have been described [2, 3, 5, 7, 11–13, 21, 34, 36, 43, 45–47] for surgical correction of sagittal plane deformity. The choice of method depends on the degree of rigidity or flexibility of the deformity. Bridwell [9] classified patients deformities into three categories based on the assessment of flexibility. (1) Totally flexible, (2) partially correctable deformity through its mobile segments, and (3) totally inflexible spinal deformity with no correction (this is termed a fixed deformity). The flexibility is imperative in deciding which surgical approach will best restore the surgical balance.
Types of deformity and correction techniques
Flexible deformity
Flexible deformities are primarily disc-based. To improve sagittal balance, the anterior column can be reconstructed through an anterior or posterior approach using bone graft or interbody cages. Polysegmental wedge osteotomies (PWO) (Fig. 8) are used for a posteriorly based correction.
Fig. 8.
Polysegmental wedge osteotomies showing resection of the lamina and facets. This leaves segmental gaps posteriorly at each level which are closed with compression to shorten the posterior column and correct deformity
Fixed deformity
With a fixed deformity, the surgical technique is determined by the degree of correction required. Options include pedicle subtraction osteotomy (PSO) and more recently, the posterior vertebral column resection technique (PVCR).
Each of these techniques will now be discussed in further detail:
Polysegmental wedge osteotomy (Fig. 8): This is a modification of the Smith Peterson technique. It is used for less severe deformities. This technique involves creating wedge shaped osteotomies of the posterior arches of adjacent vertebra with bilateral facetectomies and ligamentum flavum excision. The osteotomy gap is about 1 cm. Correction is attained by closing down the gap with the aid of instrumentation to shorten the posterior column. In contrast to the Smith Peterson technique, the anterior column is left intact. This technique relies on the mobility of the discs. This is because closing the posterior osteotomies is potentiated by the extra degrees of freedom present in the mobile discs. In other words, the global angular correction of the osteotomies depends on the number of levels involved whilst the local angular potential depends on the ability of the anterior column discs to open up. The mobility of the anterior column in these cases does lead to concern about the prospect of later loss of correction, and it is therefore the senior authors practise to reconstruct the anterior column with interbody cages at a second stage. Approximately 10°–15° of sagittal correction can be obtained with a PWO [29, 44], and it is usually performed at two or more levels. For a patient requiring 10°–20° of lordosis to achieve 4–7 cm of correction of the C7 plumb line, it is more appropriate to do a limited number of WO’s.
Pedicle subtraction osteotomy (Fig. 9): This has been described by numerous authors [2, 8, 12, 13, 27, 34, 39, 47, 49]. The PSO technique is commonly performed in cases in which there is a rigid anterior and posterior column such as in ankylosing spondylitis. The principle is to remove a wedge of bone from the anterior and posterior columns followed by a reapposition of the residual upper and lower segments of the vertebra i.e. ‘close the wedge’ to effect a correction. The apex of the wedge is centred on the vertebral body anteriorly and the base overlies the facet joints and laminae posteriorly. The area of the base runs from the foraminal space above to the foraminal space below in the sagittal plane and in the coronal plane runs from the inferior laminae of the adjacent superior vertebra to the inferior laminae below. The size of the wedge is determined by the angular correction necessary to restore C7 over the sacral end plate. Using the spino-sacral angle, the amount of correction required is calculated. If this is less than 45°, then a single level posteriorly based PSO can be performed in the lumbar spine. The level of osteotomy when performed in the lumbar spine using the PSO technique will determine the new position of the apex of lordosis. An ostoeomy at L3 will induce a greater lordotic curve than a more distal correction at L4 which is more likely to give rise to a short lordotic lumbar curve (Fig. 10). The second issue is that the closer this osteotomy is to the apex of the kyphosis the greater the angular correction required for the same degree of deformity due to the short lever arm. This runs the risk of overcorrection and subsequent vertical gaze. A more distal osteotomy has a longer lever arm and therefore requires less angular correction (Fig. 11). This type of surgical intervention is useful in correcting large fixed sagittal plane deformities. It can achieve up to 40° of sagittal correction [7, 11, 35]. During surgery, multiple screws are placed bilaterally at a minimum of three levels on either side of the proposed osteotomy site. A working rod is placed on the contralateral side. After posterior decompression with removal of the posterior arch and pedicular resection, decancellation of the vertebral body is then performed stopping short of the anterior wall. The lateral and posterior wall inner surfaces are cleared of cancellous bone. This has the effect of weakening these walls in readiness for the reduction manoeuvre. It also has the added advantage of avoiding dissection on the outer lateral wall with the inherent risk of bleeding from the segmental vessels. The weakened posterior wall is then resected at its margins with care to avoid damage to the dura and then pushed anteriorly with an angled curette into the hollow cavity within the vertebral body. At this point, the reduction manoeuvre can begin with elevation of the distal part of the table to re-orientate the pelvis and distal part of the spine. A rough guide is to line up the plane of the back of the occiput with that of the buttocks. At the same time, there is sequential tightening of the screw rod construct. This follows application of rods which have been contoured to match the angle of desired correction. Compression of the osteotomy gap continues until further movement is stopped by the margins of the previous laminotomies. It is important to note that the primary stability of the correction using both techniques depends on the contact between the opposing laminotomy surfaces and is then supplemented with the rod-screw construct.
Asymmetrical pedicle subtraction osteotomy (Fig. 12): In cases of combined rigid sagittal and coronal plane deformities, correction in both planes is needed. An asymmetrical osteotomy which is still centred on the pedicles is carried out. The laminotomy lines are no longer parallel and the decancellation manoeuvre mirrors this asymmetry. A simple pedicular resection will suffice unilaterally.
Posterior vertebral column resection (Fig. 13): This is a more recently described technique and is useful in rigid deformities which require correction by angulation as well as translation. It is performed through a posterior approach and involves resection of the vertebral body and posterior arch. The anterior longitudinal ligament acts as a restraint to overcorrection. An interbody cage or strut graft is used to bridge the defect created by removal of the vertebra [9]
Smith Peterson osteotomy (Fig. 14): This procedure is rarely performed nowadays due to its associated vascular complications. The correction forcibly opens up the anterior column and hinges on the middle and posterior columns.
Fig. 9.
Pedicle subtraction osteotomy. a Lateral view of vertebra with wedge removed, b posterior vertebral wall with posterior arch and pedicles removed, c posterior view of vertebra after wedge excision. Re-alignment is effected by apposition of the remaining upper and lower portions of the vertebra by compression
Fig. 10.
Change in lordotic profile of lumbar spine with shift in apex when osteotomy performed at different levels (L3 vs. L4). Note the shorter lumbar curve when the osteotomy is performed at L4
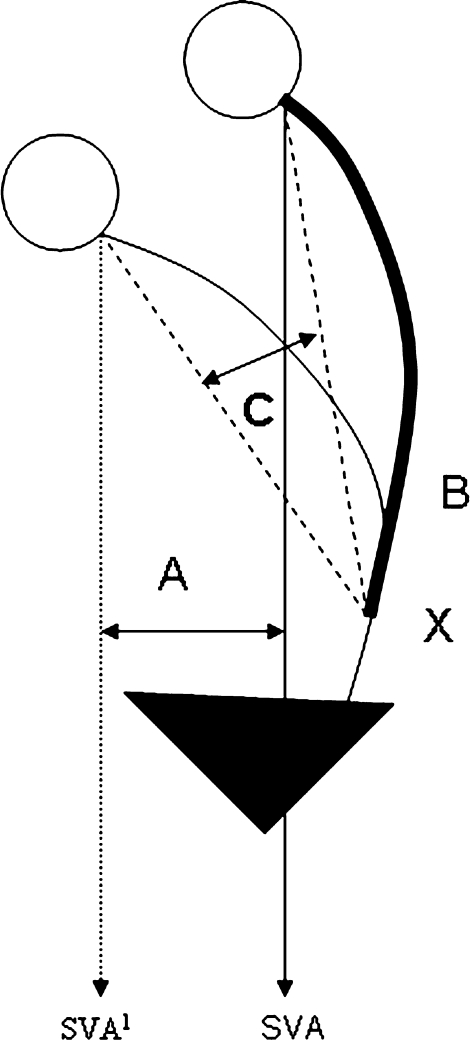
Fig. 11.
Restoration of sagittal alignment is measured by the distance between the plumb lines (A) when the osteotomy is performed at B which is further away and distal to the apex of the deformity therefore requiring a smaller angle of correction C
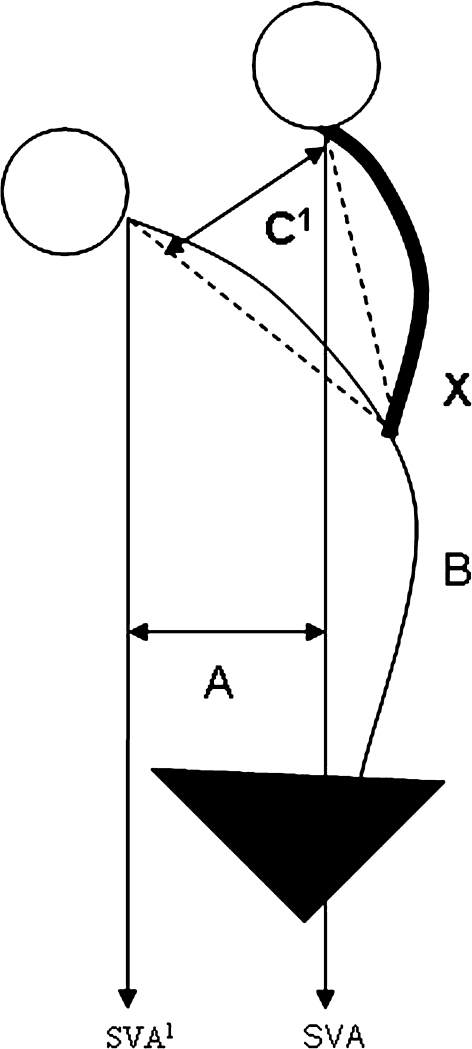
Fig. 12.
Restoration of sagittal alignment with osteotomy (X) closer to apex of deformity. Angle of correction C1 required to give same amount of improvement in sagittal correction (A) is greater. In both cases, the plumb line (sagittal vertical axis, SVA1) shifts posteriorly (SVA) with restoration of alignment
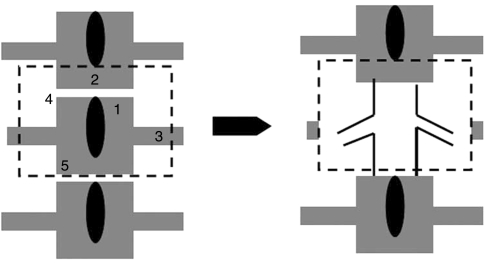
Fig. 13.
Posterior vertebral column resection diagram to demonstrate margins of resection: 1 Posterior arch, 2 Adjacent lamina, 3 Transverse processes/ribs, 4 Discs, 5 Vertebral body. The anterior longitudinal ligament is left intact to act as a restraint to overcorrection
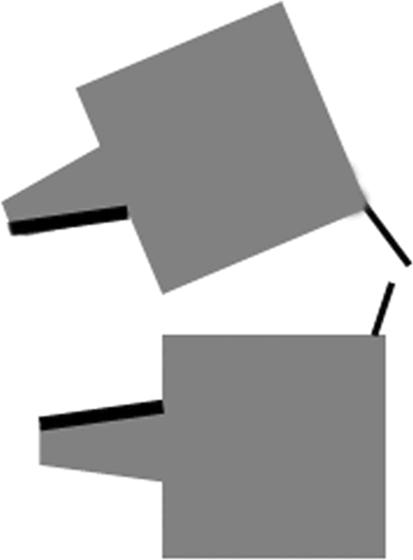
Fig. 14.
Smith Petersen osteotomy: Posterior osteotomies (black lines) with deformity correction through disc space and anterior longitudinal ligament. The correction hinges on the middle and posterior columns. There is a risk of great vessel rupture with this method
In some cases, it has been noted postoperatively that despite a reasonable thoracolumbar correction, patients maintain a compensatory lower limb profile suggesting incomplete realignment. This may be due to a residual excessive pelvic tilt in the presence of a small sacral slope. Referring to earlier discussions, the pelvic tilt (PT) and sacral slope (SS) are variable. Pelvic incidence is constant. Normal PT (NPT) is 12°. The excess Pelvic tilt = NPT − PT. This difference should be added to the amount of correction required to bring C7 over the sacral endplate. For example, if 30° of correction is necessary to bring C7 over S1 but a reduction of 10° pelvic tilt is desirable, then the osteotomy must accomplish 40° of sagittal correction.
Complications
Van Royen et al. [39] carried out a comprehensive review of three techniques of lumbar osteotomy in patients with Ankylosing Spondylitis. They looked at outcomes of SPO, PWO and PSO using technical grading criteria and complication rates [16].
Technical grading was classified as (1) Good, if fusion was complete with loss of correction of less than 10°; (2) Fair, with pseudoarthrosis and loss of correction of greater than 10° with complications; (3) Poor, with no correction and major complications including fatality. Good results were reported in 78% of the PSO group, 73% of the SPO group and 69% of the PWO group. There was no statistical difference between the groups. Transient neurological complications were reported in all the three groups, but no permanent neurological injury was reported in the PSO group. Buchowski et al. [10] reported on a 10-year review of lumbar pedicle subtraction osteotomies. They found that the incidence of intraoperative and post-operative neurological deficits was 11% but permanent neurologic deficit was 2.8%. Bridwell reported no permanent neurological deficit. However, a recent cohort study by Willems et al. [54] reports a complication rate of 7.8% with permanent neurological damage.
Bleeding : Significant blood loss can occur. Kim et al. [27] reported on comparison of blood loss in SPO versus PSO. They found a substantially greater blood loss in the PSO group (P < 0.001). Most of the bleeding occurs from bone and therefore, installation of all instrumentation prior to bony osteotomy is to be recommended. As a general rule, closure of the osteotomy reduces bleeding.
Infection: Deep and superficial infection rates of up to 43% have been reported. Willems et al. report a rate of 9.6% for deep wound infections.
Mortality: In his review, Van Royen [48] described an overall peri-operative mortality rate of 4%. This was mainly due to pulmonary and bowel conditions, cardiac failure and sepsis. A sub-group analysis showed the incidence of peri-operative mortality in SPO was 5.8, 2.4% in WO and 1.4% in PSO. The risk of vascular complications [32, 42, 53] was 0.9% in the SPO group. This risk increased if the SPO was between L1 and L3.
Inadequate correction [30] or loss of correction: This may be caused by over or under resection of bone or poor technique. In the thoracic spine, reduction can be restricted by stiff costovertebral joints or contracted anterior musculature. Loss of correction can occur with pseudoarthrosis or failure of instrumentation and is less likely to occur in PSO probably due to the stability afforded by bony surface apposition.
Despite these risks, there appears to be a general improvement in functional outcomes on the whole. Bridwell [7] performed an outcome analysis on 27 patients who had undergone lumbar pedicle subtraction osteotomies for sagittal plane deformity with a minimum 2-year follow-up. Using the SRS questionnaire, twenty patients reported a reduction in pain while three reported an increase in pain with no change in the remaining patients. Nineteen patients reported an improvement in self-image, and 24 of 26 patients felt that they looked better after surgery than before. The overall satisfaction scores were high. It is not stated whether there is a statistically significant difference between preoperative and post-operative scores. In the same paper using the Oswestry questionnaire, they report a significant difference between preoperative and postoperative scores (P < 0.0001). In a more recent study, [28] the same author reported on a cohort of 35 patients with a minimum 5-year follow-up. The Oswestry questionnaire score again demonstrated a significant decrease after surgery. The SRS questionnaire did not show any significant differences. However, the satisfaction sub-scale rated highest at 87% but the pain score rated lowest at 66%. The authors state that associated co-morbidities affected the pain score. SVA > 8 cm demonstrated a strong negative trend toward the SRS score.
Discussion
Until recently, a lot of attention has been focused on coronal plane deformities. Emphasis has been placed on the ability to make the spine straight or balanced when interpreting post-operative AP radiographs. The downside of this principle is that as is now widely acknowledged, destabilisation of the sagittal profile may occur following treatment. A sagittal plane deformity can be very disabling for the patient and must be addressed. To correct any deformity, however, requires an understanding of what is normal for the individual patient. The clinical outcomes for joint arthroplasty improved with a better understanding of joint mechanics, soft tissue tension and bone preservation techniques. This was tempered by an awareness of the patient specific variation of these parameters.
With the sagittal profile of the spine, conventional thinking has been to categorise it into different segments based on the anatomical differentiation of the vertebrae. This delineation does not take into account the true surface contour of the spine. The disadvantage of this overly simplistic categorisation is that when attempting to restore what is perceived as a ‘normal thoracolumbar spine’, we are applying a ‘one size fits all’ approach. This is at odds with the principles of joint reconstruction where, so often, surgical choices are governed by preoperative templating. The authors believe that it is important to be aware of the expected individual sagittal profile for each patient in order to have a template upon which to plan treatment. The restoration of alignment to equalise force distribution and avoid future loss of correction or junctional failure should be a major aim of treatment. A better understanding of sagittal plane alignment should influence the treating spinal surgeon when deciding on the length of the construct as well as the fixation points.
Our increased understanding of sagittal plane deformity means that our case load will increase due to earlier identification. Also as the life expectancy of the population increases along with the patients desire to lead more active lives well into advanced years, so will the demand for appropriate expertise and skill in dealing with this complex problem. Spinal osteotomies remain complicated procedures. This treatment strategy must be the subject of specific training and must be practised by specialist surgeons for the best outcomes.
Acknowledgment
The authors would like to thank Mr. Sanjay Purushothamdas and Dr Akash Sharma of the Spinal Surgery Unit, Nuffield Orthopaedic Centre, Oxford for proof reading and organisation of the manuscript.
References
- 1.Berthonnaud E, Dimner J, Roussouly P, Labelle H. Analysis of the sagittal balance of the spine and pelvis using shape and orientation parameters. J Spine Disord. 2004;18(1):40–47. doi: 10.1097/01.bsd.0000117542.88865.77. [DOI] [PubMed] [Google Scholar]
- 2.Berven SH, Deviren V, Smith JA, Emami A, Hu SS, Bradford DS. Management of fixed sagittal plane deformity: results of the transpedicular wedge resection osteotomy. Spine. 2001;26(18):2036–2043. doi: 10.1097/00007632-200109150-00020. [DOI] [PubMed] [Google Scholar]
- 3.Boachie-Adjei O, Bradford DS. Vertebral column resection and arthrodesis for complex spinal deformities. J Spinal Disord. 1991;4(2):193–202. doi: 10.1097/00002517-199106000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Boesker EH, Moe JH, Winter RB, Koop SE. A determination of the normal thoracic kyphosis: a roentgenographic study of 121 normal children. J Pediatr Orthop. 2000;20:796–798. doi: 10.1097/00004694-200011000-00019. [DOI] [PubMed] [Google Scholar]
- 5.Bradford DS, Schumacher WL, Lonstein JE. Ankylosing spondylitis: experience in surgical management of 21 patients. Spine. 1987;12:238–243. doi: 10.1097/00007632-198704000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Bridwell KH, Bernhardt M. Segmental Analysis of the sagittal plane alignment of the normal thoracic and lumbar spines and thoracolumbar junction. Spine. 1989;14:717–721. doi: 10.1097/00007632-198907000-00012. [DOI] [PubMed] [Google Scholar]
- 7.Bridwell KH, Lewis SJ, Edwards C, Lenke LG, Iffrig TM, Berra A. Complications and outcomes of pedicle subtraction osteotomies for fixed sagittal imbalance. Spine. 2003;28(18):2093–2101. doi: 10.1097/01.BRS.0000090891.60232.70. [DOI] [PubMed] [Google Scholar]
- 8.Bridwell KH, Lewis SJ, Lenke LG, Baldus C, Blanke K. Pedicle subtraction osteotomy for the treatment of fixed sagittal imbalance. J Bone Joint Surg Am. 2003;85-A(3):454–463. doi: 10.2106/00004623-200303000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Bridwell KH. Decision making regarding Smith-Petersen vs pedicle subtraction osteotomy vs vertebral column resection for spinal deformity. Spine. 2006;31(19 suppl):S171–S178. doi: 10.1097/01.brs.0000231963.72810.38. [DOI] [PubMed] [Google Scholar]
- 10.Buchowski JM, Bridwell KH, Lenke LG, Kuhns CA. Neurologic complications of lumbar pedicle subtraction osteotomy. Spine. 2007;32(20):2245–2252. doi: 10.1097/BRS.0b013e31814b2d52. [DOI] [PubMed] [Google Scholar]
- 11.Camargo FP, Cordeiro EN, Napoli MM. Corrective osteotomy of the spine in ankylosing spondylitis. Experience with 66 cases. Clin Orthop. 1986;208:157–167. [PubMed] [Google Scholar]
- 12.Chen IH, Chien JT, Yu TC. Transpedicular wedge osteotomy for correction of thoracolumbar kyphosis in ankylosing spondylitis. Spine. 2001;26(16):354–360. doi: 10.1097/00007632-200108150-00010. [DOI] [PubMed] [Google Scholar]
- 13.Danisa OA, Turner D, Richardson WJ. Surgical correction of lumbar kyphotic deformity: posterior reduction ‘eggshell’ osteotomy. J Neurosurg. 2000;92(1 suppl):50–56. doi: 10.3171/spi.2000.92.1.0050. [DOI] [PubMed] [Google Scholar]
- 14.During J, Goudfrooij H, Keesen W, Beeker TW, Crowe A. Toward standards for posture: postural characteristics of the lower back system in normal and pathologic conditions. Spine. 1985;10(1):83–87. doi: 10.1097/00007632-198501000-00013. [DOI] [PubMed] [Google Scholar]
- 15.Djurasovic M, Glassman SD. Correlation of radiographic and clinical findings in spinal deformities. Neurosurg Clin N Am. 2007;18(2):223–227. doi: 10.1016/j.nec.2007.01.006. [DOI] [PubMed] [Google Scholar]
- 16.Fox MW, Onofrio BM, Kilgore JE. Neurosurgical complications of ankylosing spondylitis. J Neurosurgery. 1993;78(6):871–878. doi: 10.3171/jns.1993.78.6.0871. [DOI] [PubMed] [Google Scholar]
- 17.Farcy JP, Schwab FJ. Management of flatback and related kyphotic decompensation syndromes. Spine. 1997;22:2452–2457. doi: 10.1097/00007632-199710150-00025. [DOI] [PubMed] [Google Scholar]
- 18.Fisher PE, John JF. Radiographic determination of the anatomic hip centre. a cadaver study. Acta Orthop Scand. 1994;65:509–510. doi: 10.3109/17453679409000901. [DOI] [PubMed] [Google Scholar]
- 19.Glassman SD, Bridwell K, Dimar JR, Horton W, et al. The impact of positive sagittal balance on adult spinal deformity. Spine. 2005;30(18):2024–2029. doi: 10.1097/01.brs.0000179086.30449.96. [DOI] [PubMed] [Google Scholar]
- 20.Hahn F, MD Min, Kan MD, Leonardi Massimo MD. Lumbar spinal osteotomy for kyphosis in ankylosing spondylitis: the significance of the whole body kyphosis angle. J Spinal Disord Tech. 2007;20(2):149–153. doi: 10.1097/01.bsd.0000211252.67576.d9. [DOI] [PubMed] [Google Scholar]
- 21.Halm H, Metz-Stavenhagen P, Zielke K. Results of surgical correction of kyphotic deformities of the spine in ankylosing spondylitis on the basis of the modified arthritis impact measurement scales. Spine. 1995;20(14):1612–1619. doi: 10.1097/00007632-199507150-00010. [DOI] [PubMed] [Google Scholar]
- 22.Hardacker JW, Shuford RF, Capicotto RN, Pryor PW. Radiographic standing cervical segmental alignment in adult volunteers without neck symptoms. Spine. 1997;22:1472–1480. doi: 10.1097/00007632-199707010-00009. [DOI] [PubMed] [Google Scholar]
- 23.Hehne HJ, Zielke K, Bohm H. Polysegmental lumbar osteotomies and transpedicular fixation for correction of long-curved kyphotic deformities in ankylosing spondylitis. Report on 177 cases. Clin Orthop. 1990;258:49–55. [PubMed] [Google Scholar]
- 24.Horton WC, Brown CW, Bridwell KH. The effect of arm position on sagittal plane alignment. Spine. 2005;30:427–433. doi: 10.1097/01.brs.0000153698.94091.f8. [DOI] [PubMed] [Google Scholar]
- 25.Jackson RP, Peterson MD, McManus AC, Hales C. Compensatory spinopelvic balance over the “hip axis” and better reliability in measuring lordosis to the pelvic radius on standing lateral radiographs of adult volunteers and patients. Spine. 1998;23:1750–1767. doi: 10.1097/00007632-199808150-00008. [DOI] [PubMed] [Google Scholar]
- 26.Jackson RP MD, Phipps T, Hales C, Suber J. Pelvic lordosis and alignment in spondylolisthesis. Spine. 2003;28(2):151–160. doi: 10.1097/00007632-200301150-00011. [DOI] [PubMed] [Google Scholar]
- 27.Kim KT, Suk KS, Cho YJ, Hong GP, Park BJ. Clinical outcome results of pedicle subtraction osteotomy in ankylosing spondylitis with kyphotic deformity. Spine. 2002;27(6):612–618. doi: 10.1097/00007632-200203150-00010. [DOI] [PubMed] [Google Scholar]
- 28.Kim YJ, Bridwell KH, Lenke LG, Cheh G, Baldus C. Results of lumbar pedicle subtraction osteotomies for fixed sagittal imbalance: a minimum 5-year follow-up study. Spine. 2007;32(20):2189–2197. doi: 10.1097/BRS.0b013e31814b8371. [DOI] [PubMed] [Google Scholar]
- 29.Kyn-Jung Cho MD, Keith Bridwell H, Lawrence G, Lenke MD, Annette Berra BA, Christy Baldus RN. Comparison of Smith-Petersen versus pedicle subtraction osteotomy for the correction of fixed sagittal imbalance. Spine. 2005;30(18):2030–2037. doi: 10.1097/01.brs.0000179085.92998.ee. [DOI] [PubMed] [Google Scholar]
- 30.La Grone MO, Loss of lumbar lordosis A complication of spinal fusion for scoliosis. Orthop Clin North Am. 1988;19:383–393. [PubMed] [Google Scholar]
- 31.Legaye J, Duval-Beaupere G, Hecquet J, Marty C. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 1998;7(2):99–103. doi: 10.1007/s005860050038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lichtblau PO, Wilson PD. Possible mechanism of aortic rupture in orthopaedic correction of rheumatoid spondylitis. J Bone Joint Surg Am. 1956;38(1):123–127. [PubMed] [Google Scholar]
- 33.Mac-Thiong JM, Labelle H, Berthonnaud E, Betz RR, Roussouly P. Sagittal spinopelvic balance in normal children and adolescents. Eur Spine J Feb. 2007;16(2):227–234. doi: 10.1007/s00586-005-0013-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McMaster MJ. A technique for lumbar spinal osteotomy in ankylosing spondylitis. J Bone Joint Surg Br. 1985;67(2):204–210. doi: 10.1302/0301-620X.67B2.3980526. [DOI] [PubMed] [Google Scholar]
- 35.McMaster MJ, Coventry MB. Spinal osteotomy in ankylosing spondylitis. Technique, complications, and long-term results. Mayo Clin Proc. 1973;48(7):476–486. [PubMed] [Google Scholar]
- 36.Noun Z, Lapresle P, Missenard G. Posterior lumbar osteotomy for flatback in adults. J Spinal Disord. 2000;14:311–316. doi: 10.1097/00002517-200108000-00005. [DOI] [PubMed] [Google Scholar]
- 37.Pile KD, Laurent MR, Salmond CE, Best MJ, Pyle EA, Moloney RO. Clinical assessment of ankylosing spondylitis: a study of observer variation in spinal measurements. Br J Rheumatol. 1991;30(1):29–34. doi: 10.1093/rheumatology/30.1.29. [DOI] [PubMed] [Google Scholar]
- 38.Roussouly P, Gollogly S, Berthonnaud E, Dimnet J. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine. 2005;30(3):346–353. doi: 10.1097/01.brs.0000152379.54463.65. [DOI] [PubMed] [Google Scholar]
- 39.Roussouly P, Richard A, Vallese P, Berthonnaud E (2000) Compared effect of eggshell transpedicular lumbar osteotomy and pelvic osteotomy in correction of great sagittal imbalance. 9th International Meeting on Advanced Spine Techniques, Montreux, Switzerland
- 40.Schwab F, Lafage V, Patel A, Farcy JP. Sagittal plane considerations and the pelvis in the adult patient. Spine. 2009;34(17):1828–1833. doi: 10.1097/BRS.0b013e3181a13c08. [DOI] [PubMed] [Google Scholar]
- 41.Scoliosis Research Society. White paper on sagittal plane alignment
- 42.Simmons EH (1994) Relation of vascular complications to the level of lumbar extension osteotomy in ankylosing spondylitis. 61st Annual meeting of the American academy of Orthopaedic Surgeons, New Orleans
- 43.Simmons EH. Kyphotic deformity of the spine in ankylosing spondylitis. Clin Orthop. 1977;128:65–77. [PubMed] [Google Scholar]
- 44.Smith-Petersen MN, Larson CB, Aufranc OE. Osteotomy of the spine for correction of flexion deformity in rheumatoid arthritis. J Bone Joint Surg Am. 1945;27:1–11. [PubMed] [Google Scholar]
- 45.Suk KS, Kim KT, Lee SH, Kim JM. Significance of chin-brow vertical angle in correction of kyphotic deformity of ankylosing spondylitis patients. Spine. 2003;28(17):2001–2005. doi: 10.1097/01.BRS.0000083239.06023.78. [DOI] [PubMed] [Google Scholar]
- 46.Thomasen E. Vertebral osteotomy for correction of kyphosis in ankylosing spondylitis. Clin Orthop. 1985;194:142–152. [PubMed] [Google Scholar]
- 47.Royen BJ, Gast A. Lumbar osteotomy for correction of thoracolumbar kyphotic deformity in ankylosing spondylitis. A structured review of three methods of treatment. Ann Rheum Dis. 1999;58(7):399–406. doi: 10.1136/ard.58.7.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Royen BJ, Gast A, Smit TH. Deformity planning for sagittal plane corrective osteotomies of the spine in ankylosing spondylitis. Eur Spine J. 2000;9(6):492–498. doi: 10.1007/s005860000183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Royen BJ, Slot GH. Closing-wedge posterior osteotomy for ankylosing spondylitis. Partial corpectomy and transpedicular fixation in 22 cases. J Bone Joint Surg Br. 1995;77(1):117–121. [PubMed] [Google Scholar]
- 50.Royen BJ, Toussaint HM, Kingma I, Bot SD, Caspers M, Harlaar J, Wuisman PI. Accuracy of the sagittal vertical axis in a standing lateral radiograph as a measurement of balance in spinal deformities. Eur Spine J. 1998;7(5):408–412. doi: 10.1007/s005860050098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Vaz G, Roussouly P, Berthonnaud E, Dimnet J. Sagittal morphology and equilibrium of pelvis and spine. Eur Spine J. 2000;11:80–87. doi: 10.1007/s005860000224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Voutsinas SA, MacEwen GD. Sagittal profiles of the spine. Clinical Orthopaedics and related research. 1986;210:235–242. [PubMed] [Google Scholar]
- 53.Weatherley C, Jaffray D, Terry A. Vascular complications associated with osteotomy in ankylosing spondylitis: a report of two cases. Spine. 1988;13(1):43–46. doi: 10.1097/00007632-198801000-00010. [DOI] [PubMed] [Google Scholar]
- 54.Willems KF, Slot GH, Anderson PG, Pavlov PW, Kleuver M. Spinal osteotomy in patients with ankylosing spondylitis: complications during first post operative year. Spine. 2005;30(1):101–107. doi: 10.1097/00007632-200501010-00018. [DOI] [PubMed] [Google Scholar]
- 55.Vendatam R, Lenke LG, Keeney JA, Bridwell KH. Comparison of standing sagittal spinal alignment in asymptomatic adolescents and adults. Spine. 1998;23(2):211–215. doi: 10.1097/00007632-199801150-00012. [DOI] [PubMed] [Google Scholar]