Abstract
The aim of our study was twofold: firstly, to compare the preoperative and postoperative results at mid-term follow-up periods along with the data of the control group. Secondly, to evaluate the effectiveness among open-discectomy and microdiscectomy surgical groups. In the present study, we investigated a cohort of 100 patients with the lumbar disc herniation causing low back pain compared to 100 subjects of the control group with the non-specific low back pain by applying physical activity, pain scale, Short Form 36 General Health Questionnaire and additional postoperative records of patient’s satisfaction and complications level, consumption of analgesics, and return to work status. The quantitative analysis of all questionnaires showed substantial differences in the preoperative and postoperative groups. The best results were achieved at the second year follow-up period. However, there were no statistically significant differences in both the examined surgical subgroups (p > 0.05). In addition, we estimated from moderate to great statistical significance (p < 0.01–0.05) among preoperative and overall postoperative results: PHC and MHC in the SF-36, Oswestry and VAS. The total increased satisfaction, reherniation rate and return to work frequency comprised 40, 9 and 64%, respectively. The analgesics were still indicated for 21% of the patients. The results of the present study suggest of sufficient decompression in both surgical groups, as the health-related quality of life parameters (Oswestry, VAS and SF-36) were defined as clinically improved. Regardless of persisted minor pain in both areas, it remained greater in the low back than in the leg, which should be held for beneficial to decompressive surgery.
Keywords: Lumbar disc herniation disease, Physical health component, Mental health component, Microdiscectomy, Open-discectomy
Introduction
According to the recent studies [31, 34, 35], the degenerative disc disease (DDD) occurs even in asymptomatic patients, but for about 10% of the population it results in permanent chronic pain and disability. The frequency of lumbar disc herniation (LDH) amounts from 5.1 to 3.7% with the male and female population, respectively, with the majority of 90–97% displaying at L4–L5 and L5–S1 levels [1, 25, 48]. Therefore, long lasting pain and functional impairments undergone by the patients as well as the varied treatment opportunities have led to situation, when the operation of the ruptured lumbar intervertebral disc represents a special challenge.
Lumbar microdiscectomy (MD) and open-discectomy (OD) are commonly performed surgical procedures for that type of patients. Mixter et al. were the first to describe pitfalls of laminectomies [38] and later in 1978 Caspar and Williams [29, 56] initially reported the technique of lumbar MD, which slightly contributes to a relatively smaller incision, less soft tissue damage, therefore reduced postoperative pain, early discharge from hospital and return to work compared to OD.
Despite various underlying factors, the success rate depends commonly on the appropriate screening for those treatment modalities, because pain and disability may persist regardless of positive radiological changes, consequently it should not be restricted only to radiological diagnostic techniques [2]. The cost of unsatisfactory outcomes is crucial both for the patient in terms of health-related life quality and to providers of health service in terms of financial costs and further treatment [11, 18].
Along with the clinical examinations, computed tomography (CT) and magnetic resonance imaging (MRI), the paraclinical diagnostic techniques are frequently applied due to the additional standardized screening of patients for those surgical interventions [4, 16, 21]. The generic measurements are broadly applicable and therefore employed across patient population, as they could be cheaply and lightly used for the additional screening. However, the SF-36 [52, 58] is recommended for the assessment of general health status, and more spine-specific measures are further recommended. The accomplished study of the Short Form Health Survey (SF-36), Oswestry disability and visual analogue scale (VAS) for pain was performed due to their effectiveness in preoperative screening of the patients with LDH disease in comparison with data of the control group (CG) as well as in postoperative follow-up assessment with two operating techniques.
Patients and methods
Patient population
Within the prospective observational cohort study, there were two populations of the clinical subjects complaining of low back pain and sciatica at the Kaunas University of Medicine, Department of Neurosurgery reviewed. The study sample examination was done between June 2003 and May 2007, under permission from our local ethics committee (No.BE-2-31). The patients’ group predisposed to surgery was divided into two quantitatively equal subgroups (MD and OD). There were no special criteria for that sampling provided.
Inclusion and exclusion criteria
One hundred patients with the LDH disease were recruited for the present study guiding to the following criteria: (1) chronic pain, occurring daily, for at least 3 months, and at least 20 h a day, refractory to >6 weeks of conservative treatment; (2) chief complaint of pain and/or numbness in the lumbar spine, buttock, and/or lower extremity; (3) age >21 years and <76 years; (4) duration of current episode <16 days (judged from the patient’s self-report); (5) symptoms extending distal to the knee (judged from the pain diagram); (6) stiffness in the lumbar spine (judged from segmental mobility testing); (7) signs consistent with nerve root compression, including any one of the following: (a) reproduction of low back or leg pain with straight leg raise <45°; (b) muscle weakness involving a major muscle group of the lower extremity; (c) diminished lower extremity muscle stretch reflex (quadriceps and Achilles tendon); (d) diminished or absence of sensation to pinprick in any lower extremity dermatome; (8) MRI or CT demonstrating anatomical unilateral LDH correlating with the patient’s symptoms.
The next hundred of the CG’s subjects, the majority of which belonged to the Kaunas University of Medicine Hospital nursing personnel experiencing milder low back pain symptoms, were involved into the present study according to the following criteria: (1) chronic pain, occurring after physical chores, for at least 3 months, susceptible to conservative treatment; (2) chief complaint of pain and/or numbness in the lumbar spine; (3) age >20 years and <65 years; (4) no symptoms extending distal to the knee (judged from the pain diagram); (5) reproduction of low back and/or leg pain with straight leg raise >45°.
The patients were ineligible if they met further specification: prior lumbar surgery, segmental instability, vertebral fractures and spinal infections, other types of DDD, tumors, and pregnancy.
Outcome measures
Subjects were asked to complete a screening questionnaire that combined demographic characteristics with information about previous, present history and current medication. Physical examinations of the preoperative patients included motor, sensation, reflexes, degree of pain-onset by the straight leg raising test (Laseque symptom), and CT or MRI. The motor function was determined using a manual muscle test and results were classified as normal, good, fair, poor, trace and zero. Sensation was judged according to whether or not there were some hypaesthesic or hypalgesic changes. Consumption of analgesics was classified into several categories: simple analgesics, NSAIDs, mild opioids, major opioids, antidepressive, and antianxiety drugs.
Specific outcome tools at the baseline and follow-up examination periods
One of the most frequently applied questionnaires for the health-related quality of life evaluation in spinal pathology is SF-36 [47, 59]. The SF-36 questionnaire is a multipurpose, short-form health survey with 36 questions and it yields an 8-scale profile, representing functional health: physical health component (PCH) and psychological status: mental health component (MCH) equally.
The more specific measure—degree of disability, expressed as Oswestry Disability Index (ODI), was assessed guiding to the Oswestry Low Back Pain Disability Questionnaire [14, 15].
Intensity of low back pain and sciatica was scored on the visual analogue scale (VAS) and obtained in a standard fashion. Relevance, validity, and reliability of the VAS are commonly accepted in the area of low back and leg pain [5, 22].
The postoperative evaluation was conducted in nearly the same manner as the preoperative examination. In that part of the survey, patients were asked to rate their satisfaction as positive, satisfactory and negative. In these subsets were consumption of analgesics, specific health-related quality of life questionnaires for the disability and pain intensity measurement included.
Follow-up examinations on the MD and OD patients with one level LDH disease were performed at 1/2, 1, 2, 3, and 4 years after surgery. The imaging examination was carried out whether the patient had any pathological conditions agreeably to accurate functional and neurological evaluation. The essential data were collected by postal questionnaire. Non-responders received reminders, contrarily they were telephoned.
Surgical procedures
Fifty percent of patients underwent conventional OD [38]. The large majority of consecutive patients were surgical candidates for a limited posterior discectomy approach. Due to the lumbar disc localization type, the procedure has been done through the interlaminar space, whereas medial facetectomy was performed rarely, when the medial facet was clearly impinging on the nerve root.
Another fifty patients were scheduled for the MD surgical procedure following the Caspar’s technique [29, 56]. During the study period, only two spinal surgeons with adequate training and expertise in performing OD and MD participated and the preoperative diagnosis was confirmed in all cases.
Statistical methods
According to the one-way ANOVA test, normal and patient population groups concerning their age and sex were proved homogenous. Data were expressed as means ± SE. Statistical significance of the difference between the means was performed with Student’s independent test, and due to assumption of abnormal distribution of variables, there were applied non-parametric tests (Mann–Whitney). Significance accepted at p < 0.05. The statistical analysis was performed using SPSS version 10.0.
Results
At the baseline, the 200 participants consisted of 100 LDH cases and 100 of CG’s subjects. The age of patients was 43 ± 1 years (range 21–76), whereas in the control group it made up 41 ± 1 years (range 20–65). Due to our study patients with lumbar disc medial and lateral herniations were included. The lower two segments composed 94.2% of the majority (Table 1).
Table 1.
Initial data of the patient population
| Initial data of patients | Number of patients |
|---|---|
| Sex | |
| Male | 53 |
| Female | 47 |
| Age | 43 ± 1 (min 21–max 76) |
| Diagnosis | |
| L2–L3 disc herniation disease | |
| Left sided | 2.4% |
| L3–L4 disc herniation disease | |
| Right sided | 3.4% |
| L4–L5 disc herniation disease | |
| Right sided | 12.6% |
| Left sided | 23% |
| Medial | 9.2% |
| L5–S1 disc herniation disease | |
| Right sided | 21.8% |
| Left sided | 27.6% |
| Duration (months) | |
| Low back pain | 83 ± 11 (min 0.25–max 360) |
| Leg pain | 7 ± 1 (min 0.25–max 84) |
The objective examination of the preoperative patients showed weak lower extremity muscle function. For example, the moderate muscle dysfunction as well as reduction of sensory and reflex function was typical for the vast majority (75–83% of patients).
A trend toward increased satisfaction levels in means of the entire patients (40%), combining MD (45%) and OD (36%) groups was observed. Less favorable mean results were reported by 50% of all, 45% in MD and 52% in OD group patients, negative by overall, and MD subjects rated 10% while OD group rated 12%.
Evaluating the return-to-work status: 64% of overall, 60% of MD and 64% of OD patients returned to work; 10% of all, 10% of MD and 6% OD patients were retired; 26% of all, 30% in OD, likewise in the MD group have changed their qualification or work.
Thus, the consumption of analgesics for all patients drew up 21%, 43% for the MD and 57% for the OD group, accordingly. The opioids were administered for the 5% of patients and slightly increased in the OD group.
By the first 2 years of follow-up period, the failed back surgery syndrome (FBSS) along with reherniation comprised 9%: 5% in adjacent and 4% in the same level as before the treatment alone in the OD group.
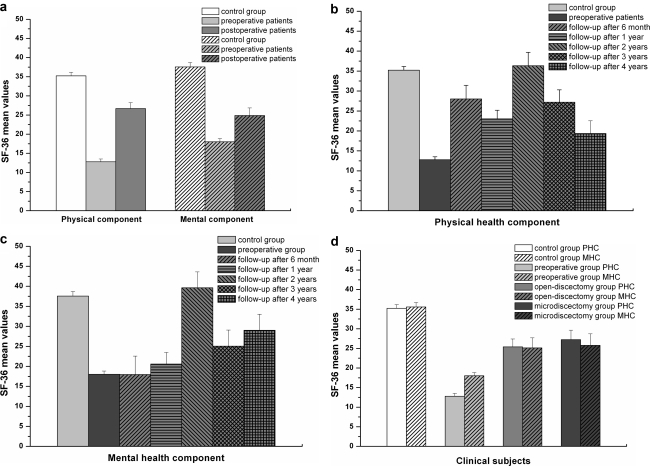
According to the SF-36 questionnaire the PHC varied as follows: in the CG it made up 35.23 ± 1, preoperative 12.8 ± 1 and postoperative patients 26.21 ± 1.54. Change among pre- and post-treatment groups was 51.2% (Fig. 1a). The results of MHC differed closely in the same manner. In the CG it made up 35.57 ± 1, preoperative 18 ± 1 and postoperative patients 25.42 ± 2. Change among pre- and post-treatment groups comprised 30%.
Fig. 1.
a Statistically significant differences (p < 0.02) in CG of PHC and MHC scores compared with pre- and postoperative assessments among all subgroups. b, c Bar graphs of norm-based PHC and MHC scores compared with pre- and postoperative assessments at ½, 1, 2, 3, 4 years of follow-up time points. Compared post- to preoperative scores—p < 0.05 with exception to ½ and 1 year assessment (p > 0.05). Compared postoperative to the CG—p > 0.05 at all follow-up time periods, with exception to PHC by the first and fourth year (p < 0.05), as well as to MHC by the second year of follow-up (p = 0.03). d The SF-36 PHC and MHC profiles (means ± SE) for both surgical treatment modalities (bars) compared with CG values and preoperative ones. Except among OD and MD patients (p > 0.05), the statistically significant differences were found in all subgroups (p < 0.05)
Further, the postoperative patients were grouped due to follow-up periods. A trend toward improvement in the PHC and MHC comprised the positive changes by all follow-up time points (Fig. 1b). The same positive mutual tendency was observed by the second year of study. However, the lower values of MHC were rated at ½ and 1-year periods (Fig. 1c).
Statistically insignificant results of two standard operating techniques with advantage to MD were defined (Fig. 1d). The PHC’s mean values among preoperative and patients after OD comprised positive change of 50% and after MD 53%. The MHC’s mean values among preoperative and patients after OD comprised positive mean change of 28.4% and after MD 30.2%.
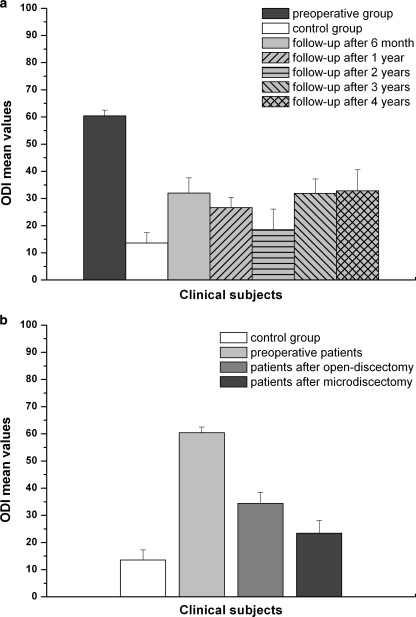
Due to the Oswestry Disability Questionnaire in patients grouped by follow-up period, the greatest mend was noted by the second year (Fig. 2a). Comparing the statistically significant results of both operative methods with the preoperative, the positive changes made up 62% for the OD and 65% for MD (Fig. 2b).
Fig. 2.
a Statistically significant differences (p < 0.05) showing the ODI scores (means ± SE) in the CG compared to pre- and postoperative assessments at ½, 1, 2, 3, 4 years of follow-up periods, except among the postoperative and CG (p > 0.05) by the second year. b Comparison of postoperative statistically significant Oswestry results (means ± SE) in MD and OD versus preoperative and CG subjects (p < 0.05)
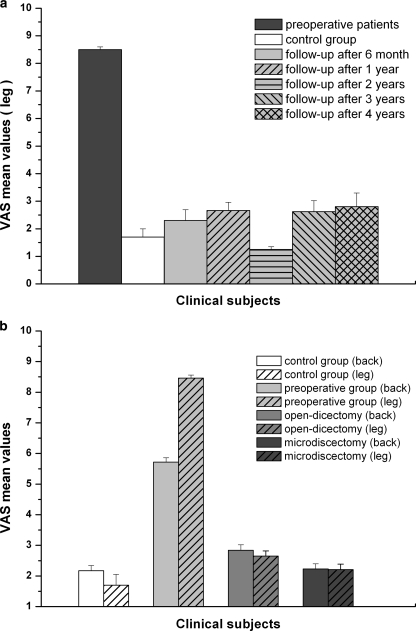
The preoperative pain according to the VAS self-reporting scale showed to be stronger in the leg (Fig. 3a, b) and conversely postoperatively. In addition, the pain intensity in both areas was tested for correlation between variables in the Oswestry and the SF-36 questionnaires. The moderate correlations were observed among ODI in the low back (R = 0.42, p = 0.022) and leg (R = 0.46, p = 0.015), likewise VAS pain intensity in the leg correlated moderately with PHC (R = 0.52, p = 0.015). A strong correlation was received from ODI and PHC and MHC at the second year of follow-up time (R = 0.98, R = 0.77, R = 0.72, p < 0.02). The poor correlation, however, statistically significant (p < 0.05) was obtained from the rest variables.
Fig. 3.
a, b The statistically significant (p < 0.05) VAS changes (means ± SE) in the low back and leg compared between the pre- and postoperative ones at all follow-up assessment time points. Statistically insignificant (p > 0.05) changes in both pain areas compared to the CG. c Bar graph delineating CG, pre- and postoperative (MD and OD methods) VAS pain outcomes (means ± SE) in both pain areas. Statistically significant differences were found in all variables (p < 0.05), except among MD and OD subgroups (p > 0.05)
Ultimately, the data of both operating methods were compared with preoperative and CG ones. The significant results among pre- and postoperative patients after OD involved the change of 50.2% in the low back and 68.8% in the leg. Slightly higher values were observed between pre- and postoperative patients after MD amounting 60.9% in the low back and 74% in the leg (Fig. 3c).
The minimum clinically important difference (MCID) for the PHC in the OD patients was 12.6 and MHC was 7.2 points. In the MD patients, it made up 14.4 for the PHC and 7.7 for the MHC. The MCID for the ODI in the OD group was 20 points and 23.4 in the MD group. Finally, the MCID for the VAS in the low back and leg in the OD patients composed 2.8 and 5.8, whereas in the MD subjects 3.5 and 6.3, respectively.
Discussion
Despite the multitude debates on the optimal treatment for LDH disease, the effectiveness of surgery varies from 49 to 90% [24, 42, 57], the results of which are observed mostly in short-term study samples with the lack of mid-term and long-term clinical data.
The aim of our study was twofold: firstly, to compare the pre- and postoperative results at mid-term follow-up periods along with data of the CG; secondly, we evaluated the effectiveness among OD and MD surgical subgroups, as it was expected the OD to be more muscle damaging.
Comparing some other randomized controlled studies [27, 28, 32, 45] dealing with the outcomes of patients underwent the standard OD and minimally invasive approaches with mid-term follow-up. The strong evidence of OD providing faster relief than conservative treatment for carefully selected LDH patients with sciatica should be amplified. However, it remained broadly similar in OD and MD subgroups.
However, design of the Weinstein’s SPORT [54] provides an opportunity to compare over time the randomized trial results to the simultaneously involved observational cohort, with small absolute differences. The latter was relatively more symptomatic and functionally impaired.
Analyzing the SF-36 and Oswestry data in the observational cohort compared to our surgical candidates, the physical function and ODI tend mostly to improve during the first 6 months postoperatively and the achieved mutual outgrowth stability during the next 4 years.
Judged by the secondary outcomes, the mutually analyzed satisfaction level and return-to-work status in the SPORT were ascendant in favor of surgery, which combined to our study exhibited almost the same tendency, with exception to return-to-work of 84.4% against our 64%.
In general, comparing the SF-36 data with other studies, almost similar results of the PHC (from 47 to 52% of positive change) were reported by Gerszten et al. [19, 55] in chronic low back pain patients undergoing intradiscal electrothermy procedure at 1–2-year follow-up time points. The total mean change of 42.2% at ½–1-year study periods amounted by Thomas et al. [50].
Application of more spine-specific tool—the Oswestry Disability Questionnaire—revealed more stable changes after desired ½, 3 and 4-year time periods, where most of means remained at a 1/2 lower than preoperatively with exception to 1 and 2 years of follow-up with a slightly better improvement of ODI means appending to the SF-36 and VAS outcomes. Though all the postoperative ODI means never reached the level of the CG population, for the majority of patients moderate disability was estimated. Our mid-term results suggest of substantial improvement in 1–2 years of observation attributed to studies [17, 37, 45], however, coincide with those short-term ones [6, 7, 41].
The goal of surgical treatment of LDH is sufficient decompression and minimization of pain intensity measured by the VAS. The measurements were performed pre- and postoperatively as described in the “Methods”. Accordingly to Zanoli et al. [59], the preoperative pain was intrinsic in population of the LDH analyzed, where the leg pain was the mostly prominent, likewise it reduced strikingly at all follow-up periods especially at the second year postoperatively and correlated highly with other questionnaires, therefore suggestive of effectiveness of the procedures performed.
A more or less remarkable postoperative pain was thought to be the consequence of peridural fibrosis, however, due to several findings [3, 30, 39, 40], the correct relation among radiological and clinical symptoms was not found. The free fat graft concluded as useful in reduction of scar tissue formation after surgery, did not result in clinically better outcomes [20].
Due to our study, pain alleviation over 50% was considered to be a positive response. In respective data, the obtained VAS scores indicated stability in change especially at 3 and 4 years of follow-up in both pain areas, thus highly correlating with the adequate ODI rates of other trials [10, 20]. However, the follow-up results by 3–4 years showed to be poorer than we expected and were not attributed to positive response. This could be explained by higher reherniation frequency, possible muscle injury during operation period or by insufficient and/or premature rehabilitation program, and/or by the scar tissue formation at these time periods [13].
Interpretation of clinical significance of changes in quality of life questionnaires becomes important in the evidence-based methods in terms of MCID, involvement of various instruments and underlying pathologies. Based on published SPORT study [54], it is reasonable to estimate MCID for the scales used: 10 points for the SF-36 subscales, 8–10 points for the Oswetry [23, 36]. The MCID in pain on VAS for lumbar surgery patients is considered to be 20 mm [23, 43].
The improved optical conditions serve for better differentiation of the anatomical structures with milder manipulation of the nerve root and dural sac [9]. It should be added that, by comparing the overall results of the questionnaires (Figs. 1d, 2a, 3b) among both golden standard surgical procedures, slightly better findings but statistically insignificant were in the MD group and maintained these unique surveys [33, 46, 51].
The reherniation rate along with other entities: segmental instability, facet joint disease, epidural fibrosis, incomplete or wrong level decompression, and poor patient selection could be attributed to the relatively frequent manifesting FBSS, comprising from 5 to 10% of lumbosacral spine surgery cases [16, 49]. In our series it did not overwhelm the results of these studies [12, 53]. Moreover, the complication rates reported by Waguespack and Ebeling were higher and could be explained by different referral patterns and categories provided.
Since LDH disease became a sore point of the working population, there is a demand to set the risk factors for work disability days after concrete surgery, where the most predicting ODI > 20, considerable degree of pain, poor motivation to work are among other confounding agents making the prognosis more complicated [44]. The early return to vigorous activities and daily work with the mean sick leave of 1.7 weeks seems likely not increasing the complication rate [8]. In present case, for 26% of rest population the disability level limited the return to job rate, which may contribute to increased consumption of analgesics.
Finally, patient satisfaction with both operating procedures was not as boosting, as it was claimed by Hersht et al. [26], where the overall experience was satisfactory for 90% of patients and several other factors such as adequate quality and amount of patient education, trust in one’s surgeon were taken into account. Based on our study, patients’ opinion on the effect of surgery associated with more subjective experience influenced by much more confusing factors compared to applied health-related life quality instruments have represented objective findings.
Conclusions
The results of present study suggest of predictably sufficient decompression in both operative techniques. Though quality of life parameters were defined as clinically improved, they had not reached preferred values of the CG. The remained minor low back pain should be held beneficial to demonstrate the effectiveness of the decompressive surgery alone. Despite slightly better values in the MD group, the technical superiority has not been proven, however, it could probably be the key to faster recovery and diminished complication rate. The secondary outcomes did not follow improvement in pain, function or satisfaction with treatment.
The provided methodology could be used in population-based studies or clinical samples that focus on specific impairments and seek to control for pain frequency, intensity or follow-up assessments testing the effectiveness of performed surgical procedures, and elicit the pathways leading to other impairments: functional limitations, disability, etc.
Contributor Information
Kotryna Veresciagina, Phone: +370-618-15180, Email: cotryna@gmail.com.
Bronius Spakauskas, Email: spak@takas.lt.
Kazys Vytautas Ambrozaitis, Email: ambrozaitis@kmu.lt.
References
- 1.Albert TJ, Balderston RA, Heller JG, Herkowitz HN, Garfin SR, Tomany K, et al. Upper lumbar disc herniations. J Spinal Disord. 1993;6(4):351–359. doi: 10.1097/00002517-199306040-00009. [DOI] [PubMed] [Google Scholar]
- 2.Atlas SJ, Keller RB, Wu YA, Deyo RA, Singer DE. Long-term outcomes of surgical and nonsurgical management of sciatica secondary to a lumbar disc herniation: 10 year results from the maine lumbar spine study. Spine. 2005;30(8):927–935. doi: 10.1097/01.brs.0000158954.68522.2a. [DOI] [PubMed] [Google Scholar]
- 3.Bernsmann K, Kramer J, Ziozios I, Wehmeier J, Wiese M. Lumbar micro disc surgery with and without autologous fat graft. A prospective randomized trial evaluated with reference to clinical and social factors. Arch Orthop Trauma Surg. 2001;121(8):476–480. doi: 10.1007/s004020100277. [DOI] [PubMed] [Google Scholar]
- 4.Bombardier C. Outcome assessments in the evaluation of treatment of spinal disorders: summary and general recommendations. Spine. 2000;25(24):3100–3103. doi: 10.1097/00007632-200012150-00003. [DOI] [PubMed] [Google Scholar]
- 5.Buttermann GR. Treatment of lumbar disc herniation: epidural steroid injection compared with discectomy. A prospective, randomized study. J Bone Joint Surg Am. 2004;86-A(4):670–679. [PubMed] [Google Scholar]
- 6.Carlsson AM. Assessment of chronic pain. I. Aspects of the reliability and validity of the visual analogue scale. Pain. 1983;16(1):87–101. doi: 10.1016/0304-3959(83)90088-X. [DOI] [PubMed] [Google Scholar]
- 7.Carragee EJ, Han MY, Suen PW, Kim D. Clinical outcomes after lumbar discectomy for sciatica: the effects of fragment type and anular competence. J Bone Joint Surg Am. 2003;85-A(1):102–108. [PubMed] [Google Scholar]
- 8.Carragee EJ, Han MY, Yang B, Kim DH, Kraemer H, Billys J. Activity restrictions after posterior lumbar discectomy. A prospective study of outcomes in 152 cases with no postoperative restrictions. Spine. 1999;24(22):2346–2351. doi: 10.1097/00007632-199911150-00010. [DOI] [PubMed] [Google Scholar]
- 9.Caspar W, Campbell B, Barbier DD, Kretschmmer R, Gotfried Y. The Caspar microsurgical discectomy and comparison with a conventional standard lumbar disc procedure. Neurosurgery. 1991;28(1):78–86. doi: 10.1097/00006123-199101000-00013. [DOI] [PubMed] [Google Scholar]
- 10.Cho DY, Lin HL, Lee WY, Lee HC. Split-spinous process laminotomy and discectomy for degenerative lumbar spinal stenosis: a preliminary report. J Neurosurg Spine. 2007;6(3):229–239. doi: 10.3171/spi.2007.6.3.229. [DOI] [PubMed] [Google Scholar]
- 11.Dolan P, Greenfield K, Nelson RJ, Nelson IW. Can exercise therapy improve the outcome of microdiscectomy? Spine. 2000;25(12):1523–1532. doi: 10.1097/00007632-200006150-00011. [DOI] [PubMed] [Google Scholar]
- 12.Ebeling U, Reichenberg W, Reulen HJ. Results of microsurgical lumbar discectomy. Review on 485 patients. Acta Neurochir (Wien) 1986;81(1–2):45–52. doi: 10.1007/BF01456264. [DOI] [PubMed] [Google Scholar]
- 13.Epstein JA, Lavine LS, Epstein BS. Recurrent herniation of the lumbar intervertebral disk. Clin Orthop Relat Res. 1967;52:169–178. doi: 10.1097/00003086-196700520-00013. [DOI] [PubMed] [Google Scholar]
- 14.Fairbank JC, Couper J, Davies JB, O’Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66(8):271–273. [PubMed] [Google Scholar]
- 15.Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine. 2000;25(22):2940–2952. doi: 10.1097/00007632-200011150-00017. [DOI] [PubMed] [Google Scholar]
- 16.Fiume D, Sherkat S, Callovini GM, Parziale G, Gazzeri G. Treatment of the failed back surgery syndrome due to lumbo-sacral epidural fibrosis. Acta Neurochir Suppl. 1995;64:116–118. doi: 10.1007/978-3-7091-9419-5_25. [DOI] [PubMed] [Google Scholar]
- 17.Floman Y, Millgram MA, Smorgick Y, Rand N, Ashkenazi E. Failure of the Wallis interspinous implant to lower the incidence of recurrent lumbar disc herniations in patients undergoing primary disc excision. J Spinal Disord Tech. 2007;20(5):337–341. doi: 10.1097/BSD.0b013e318030a81d. [DOI] [PubMed] [Google Scholar]
- 18.Gatchel RJ, Mayer T, Dersh J, Robinson R, Polatin P. The association of the SF-36 health status survey with 1-year socioeconomic outcomes in a chronically disabled spinal disorder population. Spine. 1999;24(20):2162–2170. doi: 10.1097/00007632-199910150-00017. [DOI] [PubMed] [Google Scholar]
- 19.Gerszten PC, Welch WC, McGrath PM, Willis SL. A prospective outcomes study of patients undergoing intradiscal electrothermy (IDET) for chronic low back pain. Pain Physician. 2002;5(4):360–364. [PubMed] [Google Scholar]
- 20.Gorgulu A, Simsek O, Cobanoglu S, Imer M, Parsak T. The effect of epidural free fat graft on the outcome of lumbar disc surgery. Neurosurg Rev. 2004;27(3):181–184. doi: 10.1007/s10143-003-0310-9. [DOI] [PubMed] [Google Scholar]
- 21.Graham RC, Hughes RA. A modified peripheral neuropathy scale: the Overall Neuropathy Limitations Scale. J Neurol Neurosurg Psychiatry. 2006;77(8):973–976. doi: 10.1136/jnnp.2005.081547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guyatt GH, Townsend M, Berman LB, Keller JL. A comparison of Likert and visual analogue scales for measuring change in function. J Chronic Dis. 1987;40(12):1129–1133. doi: 10.1016/0021-9681(87)90080-4. [DOI] [PubMed] [Google Scholar]
- 23.Hagg O, Fritzell P, Nordwall A. The clinical importance of changes in outcome scores after treatment for chronic low back pain. Eur Spine J. 2003;12(1):12–20. doi: 10.1007/s00586-002-0464-0. [DOI] [PubMed] [Google Scholar]
- 24.Hakkinen A, Kautiainen H, Jarvenpaa S, Arkela-Kautiainen M, Ylinen J. Changes in the total Oswestry Index and its ten items in females and males pre- and post-surgery for lumbar disc herniation: a 1-year follow-up. Eur Spine J. 2007;16(3):347–352. doi: 10.1007/s00586-006-0187-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Heliovaara M, Impivaara O, Sievers K, Melkas T, Knekt P, Korpi J, et al. Lumbar disc syndrome in Finland. J Epidemiol Community Health. 1987;41(3):251–258. doi: 10.1136/jech.41.3.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hersht M, Massicotte EM, Bernstein M. Patient satisfaction with outpatient lumbar microsurgical discectomy: a qualitative study. Can J Surg. 2007;50(6):445–449. [PMC free article] [PubMed] [Google Scholar]
- 27.Hoogland T, Schubert M, Miklitz B, Ramirez A. Transforaminal posterolateral endoscopic discectomy with or without the combination of a low-dose chymopapain: a prospective randomized study in 280 consecutive cases. Spine (Phila Pa 1976) 2006;31(24):E890–E897. doi: 10.1097/01.brs.0000245955.22358.3a. [DOI] [PubMed] [Google Scholar]
- 28.Hoogland T, Brekel-Dijkstra K, Schubert M, Miklitz B. Endoscopic transforaminal discectomy for recurrent lumbar disc herniation: a prospective, cohort evaluation of 262 consecutive cases. Spine (Phila Pa 1976) 2008;33(9):973–978. doi: 10.1097/BRS.0b013e31816c8ade. [DOI] [PubMed] [Google Scholar]
- 29.Iwa H, Caspar W. A microsurgery operation for lumbar disc herniation (author’s transl) No Shinkei Geka. 1978;6(7):657–662. [PubMed] [Google Scholar]
- 30.Jensen TT, Asmussen K, Berg-Hansen EM, Lauritsen B, Manniche C, Vinterberg H, et al. First-time operation for lumbar disc herniation with or without free fat transplantation. Prospective triple-blind randomized study with reference to clinical factors and enhanced computed tomographic scan 1 year after operation. Spine. 1996;21(9):1072–1076. doi: 10.1097/00007632-199605010-00016. [DOI] [PubMed] [Google Scholar]
- 31.Jonsson E, Nachemson A. Collected knowledge about back pain and neck pain. What we know–and what we don’t know. Lakartidningen. 2000;97(44):4974–4980. [PubMed] [Google Scholar]
- 32.Katayama Y, Matsuyama Y, Yoshihara H, Sakai Y, Nakamura H, Nakashima S, et al. Comparison of surgical outcomes between macro discectomy and micro discectomy for lumbar disc herniation: a prospective randomized study with surgery performed by the same spine surgeon. J Spinal Disord Tech. 2006;19(5):344–347. doi: 10.1097/01.bsd.0000211201.93125.1c. [DOI] [PubMed] [Google Scholar]
- 33.Lagarrigue J, Chaynes P. Comparative study of disk surgery with or without microscopy. A prospective study of 80 cases. Neurochirurgie. 1994;40(2):116–120. [PubMed] [Google Scholar]
- 34.Luoma K, Riihimaki H, Luukkonen R, Raininko R, Viikari-Juntura E, Lamminen A. Low back pain in relation to lumbar disc degeneration. Spine. 2000;25(4):487–492. doi: 10.1097/00007632-200002150-00016. [DOI] [PubMed] [Google Scholar]
- 35.Maniadakis N, Gray A. The economic burden of back pain in the UK. Pain. 2000;84(1):95–103. doi: 10.1016/S0304-3959(99)00187-6. [DOI] [PubMed] [Google Scholar]
- 36.Mannion AF, Junge A, Grob D, Dvorak J, Fairbank JC. Development of a German version of the Oswestry Disability Index. Part 2: sensitivity to change after spinal surgery. Eur Spine J. 2006;15(1):66–73. doi: 10.1007/s00586-004-0816-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mariconda M, Galasso O, Secondulfo V, Rotonda GD, Milano C. Minimum 25-year outcome and functional assessment of lumbar discectomy. Spine. 2006;31(22):2593–2599. doi: 10.1097/01.brs.0000240726.26096.be. [DOI] [PubMed] [Google Scholar]
- 38.Mixter WJ. Pitfalls in the surgery of the ruptured intervertebral disk. J Fla Med Assoc. 1952;39(3):159–167. [PubMed] [Google Scholar]
- 39.Nygaard OP, Jacobsen EA, Solberg T, Kloster R, Dullerud R. Nerve root signs on postoperative lumbar MR imaging. A prospective cohort study with contrast enhanced MRI in symptomatic and asymptomatic patients one year after microdiscectomy. Acta Neurochir (Wien) 1999;141(6):619–622. doi: 10.1007/s007010050351. [DOI] [PubMed] [Google Scholar]
- 40.Nygaard OP, Kloster R, Dullerud R, Jacobsen EA, Mellgren SI. No association between peridural scar and outcome after lumbar microdiscectomy. Acta Neurochir (Wien) 1997;139(12):1095–1100. doi: 10.1007/BF01410967. [DOI] [PubMed] [Google Scholar]
- 41.Osterman H, Seitsalo S, Karppinen J, Malmivaara A. Effectiveness of microdiscectomy for lumbar disc herniation: a randomized controlled trial with 2 years of follow-up. Spine. 2006;31(21):2409–2414. doi: 10.1097/01.brs.0000239178.08796.52. [DOI] [PubMed] [Google Scholar]
- 42.Padua R, Padua S, Romanini E, Padua L, Santis E. Ten- to 15-year outcome of surgery for lumbar disc herniation: radiographic instability and clinical findings. Eur Spine J. 1999;8(1):70–74. doi: 10.1007/s005860050129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Peul WC, Houwelingen HC, Hout WB, Brand R, Eekhof JA, Tans JT, et al. Surgery versus prolonged conservative treatment for sciatica. N Engl J Med. 2007;356(22):2245–2256. doi: 10.1056/NEJMoa064039. [DOI] [PubMed] [Google Scholar]
- 44.Puolakka K, Ylinen J, Neva MH, Kautiainen H, Hakkinen A. Risk factors for back pain-related loss of working time after surgery for lumbar disc herniation: a 5-year follow-up study. Eur Spine J. 2008;17(3):386–392. doi: 10.1007/s00586-007-0552-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Righesso O, Falavigna A, Avanzi O. Comparison of open discectomy with microendoscopic discectomy in lumbar disc herniations: results of a randomized controlled trial. Neurosurgery. 2007;61(3):545–549. doi: 10.1227/01.NEU.0000290901.00320.F5. [DOI] [PubMed] [Google Scholar]
- 46.Ruetten S, Komp M, Merk H, Godolias G. Use of newly developed instruments and endoscopes: full-endoscopic resection of lumbar disc herniations via the interlaminar and lateral transforaminal approach. J Neurosurg Spine. 2007;6(6):521–530. doi: 10.3171/spi.2007.6.6.2. [DOI] [PubMed] [Google Scholar]
- 47.Rugiene R, Dadoniene J, Venalis A. Adaptation of health-related quality of life (“SF-36”) questionnaire, its validation and assessment of performance for control group and patients with rheumatoid arthritis. Medicina (Kaunas) 2005;41(3):232–239. [PubMed] [Google Scholar]
- 48.Schwetlick G. Microsurgery in lumbar disk operations. Possibilities, methods and results. Orthopade. 1998;27(7):457–465. doi: 10.1007/s001320050256. [DOI] [PubMed] [Google Scholar]
- 49.Spakauskas B, Dambrauskas Z, Krikscionaitiene A. Pain in failed back surgery syndrome. Medicina (Kaunas) 2002;38(8):808–815. [PubMed] [Google Scholar]
- 50.Thomas KC, Fisher CG, Boyd M, Bishop P, Wing P, Dvorak MF. Outcome evaluation of surgical and nonsurgical management of lumbar disc protrusion causing radiculopathy. Spine. 2007;32(13):1414–1422. doi: 10.1097/BRS.0b013e318060a5d1. [DOI] [PubMed] [Google Scholar]
- 51.Tullberg T, Isacson J, Weidenhielm L. Does microscopic removal of lumbar disc herniation lead to better results than the standard procedure? Results of a one-year randomized study. Spine. 1993;18(1):24–27. doi: 10.1097/00007632-199301000-00005. [DOI] [PubMed] [Google Scholar]
- 52.Veresciagina K, Ambrozaitis KV, Spakauskas B. Health-related quality-of-life assessment in patients with low back pain using SF-36 questionnaire. Medicina (Kaunas) 2007;43(8):607–613. [PubMed] [Google Scholar]
- 53.Waguespack A, Schofferman J, Slosar P, Reynolds J. Etiology of long-term failures of lumbar spine surgery. Pain Med. 2002;3(1):18–22. doi: 10.1046/j.1526-4637.2002.02007.x. [DOI] [PubMed] [Google Scholar]
- 54.Weinstein JN, Tosteson TD, Lurie JD, Tosteson AN, Hanscom B, Skinner JS, et al. Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT): a randomized trial. JAMA. 2006;296(20):2441–2450. doi: 10.1001/jama.296.20.2441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Welch WC, Gerszten PC. Alternative strategies for lumbar discectomy: intradiscal electrothermy and nucleoplasty. Neurosurg Focus. 2002;13(2):E7. doi: 10.3171/foc.2002.13.2.8. [DOI] [PubMed] [Google Scholar]
- 56.Williams RW. Microlumbar discectomy: a conservative surgical approach to the virgin herniated lumbar disc. Spine. 1978;3(2):175–182. doi: 10.1097/00007632-197806000-00015. [DOI] [PubMed] [Google Scholar]
- 57.Yorimitsu E, Chiba K, Toyama Y, Hirabayashi K. Long-term outcomes of standard discectomy for lumbar disc herniation: a follow-up study of more than 10 years. Spine. 2001;26(6):652–657. doi: 10.1097/00007632-200103150-00019. [DOI] [PubMed] [Google Scholar]
- 58.Zanoli G, Jonsson B, Stromqvist B. SF-36 scores in degenerative lumbar spine disorders: analysis of prospective data from 451 patients. Acta Orthop. 2006;77(2):298–306. doi: 10.1080/17453670610046064. [DOI] [PubMed] [Google Scholar]
- 59.Zanoli G, Stromqvist B, Jonsson B. Visual analog scales for interpretation of back and leg pain intensity in patients operated for degenerative lumbar spine disorders. Spine. 2001;26(21):2375–2380. doi: 10.1097/00007632-200111010-00015. [DOI] [PubMed] [Google Scholar]