Abstract
Several methods are used to measure lumbar lordosis. In adult scoliosis patients, the measurement is difficult due to degenerative changes in the vertebral endplate as well as the coronal and sagittal deformity. We did the observational study with three examiners to determine the reliability of six methods for measuring the global lumbar lordosis in adult scoliosis patients. Ninety lateral lumbar radiographs were collected for the study. The radiographs were divided into normal (Cobb < 10°), low-grade (Cobb 10°–19°), high-grade (Cobb ≥ 20°) group to determine the reliability of Cobb L1–S1, Cobb L1–L5, centroid, posterior tangent L1–S1, posterior tangent L1–L5 and TRALL method in adult scoliosis. The 90 lateral radiographs were measured twice by each of the three examiners using the six measurement methods. The data was analyzed to determine the inter- and intra-observer reliability. In general, for the six radiographic methods, the inter- and intra-class correlation coefficients (ICCs) were all ≥0.82. A comparison of the ICCs and 95% CI for the inter- and intra-observer reliability between the groups with varying degrees of scoliosis showed that, the reliability of the lordosis measurement decreased with increasing severity of scoliosis. In Cobb L1–S1, centroid and posterior tangent L1–S1 methods, the ICCs were relatively lower in the high-grade scoliosis group (≥0.60). And, the mean absolute difference (MAD) in these methods was high in the high-grade scoliosis group (≤7.17°). However, in the Cobb L1–L5 and posterior tangent L1–L5 method, the ICCs were ≥0.86 in all groups. And, in the TRALL method, the ICCs were ≥0.76 in all groups. In addition, in the Cobb L1–L5 and posterior tangent L1–L5 method, the MAD was ≤3.63°. And, in the TRALL method, the MAD was ≤3.84° in all groups. We concluded that the Cobb L1–L5 and the posterior tangent L1–L5 methods are reliable methods for measuring the global lumbar lordosis in adult scoliosis. And the TRALL method is more reliable method than other methods which include the L5–S1 joint in lordosis measurement.
Keywords: Adult scoliosis, Lumbar lordosis, Radiographic measurement
Introduction
The relationship between lumbar lordosis and low back disorders has received considerable attention and, several methods have been developed to measure the lumbar lordosis [1, 2, 4, 5, 7, 11, 18, 25, 26]. These include the Cobb, centroid, TRALL, and posterior tangent methods [4, 5, 7, 26]. And the interobserver and intraobserver reliability of several different types of lumbar curvature analysis have been reported [4, 19, 22, 26]. Harrison et al. [16] compared these four measurement methods in lumbar lordosis and demonstrated high reliability of all methods. Chen et al. [4] compared the reliability of the Cobb and centroid method and reported higher reliability in centroid method. However, there are no reports of lumbar lordosis measurement under specific conditions, such as a degenerative spine. The use of different radiographic analytical methods without proven reliability may account for the discrepancies between studies under specific conditions.
Recognition of the importance of reliability analysis for adult scoliosis measures has led to several studies and publications on this subject [3, 6, 9, 10, 12, 20]. Freedman et al. [12] reported the inter- and intra-observer reliability of measures in adult scoliosis and compared the three lateral listhesis measurement methods. In severe adult scoliosis, hypolordosis often occurs and might be an important factor in treatment of patients [21, 23]. However, to date the reliability of the lordosis angle measurements in adult scoliosis has not been reported. Global lumbar lordosis is an important value for adult scoliosis, the role of which in deformity progression, symptoms, and outcomes needs to be determined. And, adult scoliosis occurs in patients, who frequently show arthritic changes and osteoporosis. Therefore, the reliability of the lumbar lordosis measures in this patient population can be controversial. In addition to the degenerative changes in the vertebral endplate, a coronal and sagittal deformity could interfere with a precise measurement. Therefore, determining the appropriate methods for measuring the lumbar lordosis is important for clinical decisions in adult scoliosis. The aim of this study was to test the inter- and intra-observer reliability of six specific measures of global lumbar lordosis in patients with adult scoliosis, and suggest a better method in measures of lumbar lordosis.
Materials and methods
A delayed and repeated measurement design was used to evaluate the reliability of the three examiners [15–17]. All radiographs were measured twice by each of three examiners with 2 weeks delay between first and second measurement. Each examiner digitized 90 whole-spine standing anteroposterior and lateral radiographs, which had been taken at a 120 cm standard distance using the standard technique. According to the magnitude of the curve in the anteroposterior radiographs, the radiographs were divided into three groups: normal (Cobb angle < 10°), low grade (Cobb angle 10°–19°) and high grade (Cobb angle ≥20°). The radiographs were composed of 30 normal, 30 low- and 30 high-grade adult scoliosis. The lateral radiographs without markings were submitted randomly to each examiner with 1 week delay between readings. The subjects whose radiographs were used had an average age of 62.1 years, an average height of 168.8 cm and average weight of 64.3 kg. All measurement were carried out using a computer-based digital radiogram on a picture achieving computer system (PiViewSTAR, Infinitt 2004, Seoul, South Korea), which allowed easy and accurate determinations. A total of 540 measurements were taken for each of the six different radiographic methods. The only variables were the observer’s visibility and choice of vertebral body corners. The six methods included the Cobb L1–S1, Cobb L1–L5, centroid, posterior tangent L1–S1, posterior tangent L1–L5, and TRALL method.[4, 5, 7, 16, 26] These methods were defined as follows:
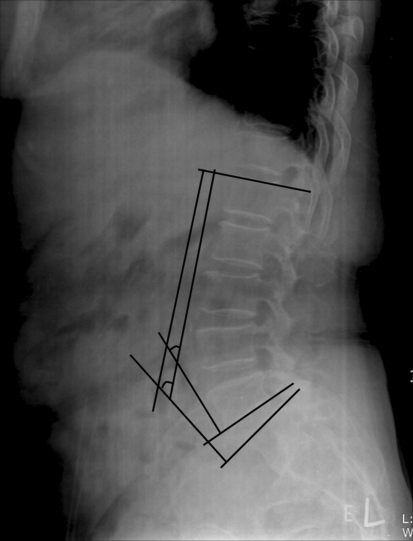
Cobb L1–S1 method (Fig. 1)
Fig. 1.
Cobb T12–S1 measured the angle between the inferior endplate of T12 and the superior endplate of S1. The Cobb L1–L5 method measured the angle between the superior endplate of L1 and the inferior endplate of L5. (Cobb method)
The angle between the superior endplate of L1 and the superior endplate of S1.
Cobb L1–L5 method
The angle between the superior endplate of L1 and the inferior endplate of L5.
Centroid method (Fig. 2).
Fig. 2.
The vertebral body centroids were approximated by the intersections of body diagonals using all four vertebral body corners (L1, L2, L5). The intersection of perpendicular lines drawn from the proximal line (connecting L1 and L2 centroid) and distal line (connecting L5 centroid and bisected sacral point) provide the lumbar lordosis angle. (centroid method)
The vertebral body centroids were approximated by the intersections of the body diagonals using all four vertebral body corners (L1, L2, L5). The intersection of the perpendicular lines drawn from the proximal line (connecting L1 and L2 centroid) and distal line (connecting L5 centroid and bisected sacral point) provided the lumbar lordosis angle [4].
Posterior tangent L1–S1 method (Fig. 3).
Fig. 3.
Posterior tangent lines were drawn through the posterior–superior and posterior–inferior body corners of T12 and S1, L1 and L5. The angles were constructed by intersecting tangents on the cranial and caudal segment of the curve. (posterior tangent method)
Posterior tangent lines are drawn through the posterior–superior and posterior–inferior body corners of L1 and S1. The angles were constructed by intersecting the tangents on the cranial and caudal segment of the curve [26].
Posterior tangent L1–L5 method.
Posterior tangent lines are drawn through the posterior–superior and posterior–inferior body corners of L1 and L5. The angles were constructed by intersecting the tangents on the cranial and caudal segment of the curve.
TRALL method (Fig. 4).
Fig. 4.
The largest perpendicular distance to the posterior longitudinal ligament from a line connecting the posterior–inferior of S1 and the superior–posterior body corner of L1 was used to locate the lumbar curve apex. This apex point was used as the vertex of the angle with the sides to L1 and S1. (TRALL method)
The largest perpendicular distance to the posterior longitudinal ligament from a line connecting the posterior–inferior of S1 and the superior–posterior body corner of L1, was used to locate the lumbar curve apex. This apex point was used for the vertex of the angle with the L1 and S1 sides [5].
Statistics
The means, standard deviations, interclass and intraclass correlation coefficients (ICCs), 95% confidence intervals (CI) between the three observers and between the two measurements of each observer were calculated. As an error analysis, we calculated for each angle the mean absolute differences (MAD) between the radiograph readings of a subject, where the mean is taken over all subjects and examiners. ICCs were considered by Shrout and Fleiss’s classifications (poor, <0.4; fair to good, 0.4–0.75; excellent, >0.75) [8, 24]. Using three-way analysis of variance (ANOVA), all statistical calculations for the reliability results of the outcome were performed with the assumptions that the measurement was crossed with the examiner and patient, and that the examiner is a random factor rather than a fixed factor. SPSS (version 13, Chicago, Illinois) was used for statistical analysis.
Results
Table 1 lists the overall means and standard deviations of the outcome measures covering the two readings of 90 radiographs by the three examiners. The ICCs, 95% CI and MAD are provided for the two Cobb methods, centroid method, two posterior tangent methods and TRALL method. Table 2 provides the data for each of the 30 radiographs, which was classified according to the severity of the coronal curves. In general, ICCs of all six methods were high. The ICCs were all ≥0.82 (excellent) for the six radiographic methods in the combined group (Table 1). However, a comparison of the ICCs and 95% CI between the groups with varying degrees of scoliosis showed that the reliability of the lordosis measurements decreased in proportion to the severity of scoliosis (Table 2). The intraclass correlation coefficient was ≥0.91 in all methods, but there was a difference in the interclass correlation coefficient between the scoliosis groups. The Cobb L1–L5 and posterior tangent L1–L5 methods consistently demonstrated higher ICCs for both inter- and intra-observer comparisons in all groups. In the Cobb L1–L5 and posterior tangent L1–L5 method, the interclass correlation coefficients were ≥0.86 (excellent) in all groups. And, in the TRALL method, the interclass correlation coefficients were ≥0.76 (excellent) in all groups. However, the other methods showed low ICCs when performed in the scoliosis radiograph. The interclass correlation coefficients in the Cobb L1–S1, centroid and posterior tangent L1–S1 method were low- in the high-grade scoliosis group (≥0.60, fair to good). For aspect of error analysis, in combined group, MAD was similar in all methods (2.53°–4.27°). A comparison of the MAD between the groups with varying degrees of scoliosis showed that the reliability of the lordosis measurements decreased in proportion to the severity of scoliosis. The intraobserver MAD was similar in all methods (2.22°–3.92°), but there was a difference in the interobserver MAD between the scoliosis groups. In the Cobb L1–L5 and posterior tangent L1–L5 method, the interobserver MAD was ≤3.63° in all groups. And, in the TRALL method, the MAD was ≤3.84° in all groups. However, the other methods showed higher MAD when performed in the scoliosis radiograph. The MAD in the Cobb L1–S1, centroid and posterior tangent L1–S1 method were high in the high-grade scoliosis group (≤7.69°).
Table 1.
The overall means, standard deviations and ICC values of the outcome measures covering the two readings by the three examiners for all 90 radiographs
| Methods | Mean and SD | Intraobserver reliability | Interobserver reliability | ||||
|---|---|---|---|---|---|---|---|
| ICC | 95% CI | MAD | ICC | 95% CI | MAD | ||
| C L1–S1 | 39.79 ± 15.50 | 0.97 | 0.96–0.97 | 3.07 | 0.90 | 0.88–0.94 | 4.14 |
| C L1–L5 | 35.29 ± 14.42 | 0.97 | 0.97–0.98 | 2.53 | 0.91 | 0.88–0.94 | 3.76 |
| Centroid | 35.66 ± 17.16 | 0.97 | 0.96–0.97 | 3.49 | 0.85 | 0.79–0.89 | 4.27 |
| P L1–S1 | 39.19 ± 16.10 | 0.96 | 0.95–0.97 | 3.59 | 0.84 | 0.79–0.89 | 4.14 |
| P L1–L5 | 34.91 ± 14.67 | 0.96 | 0.95–0.97 | 3.03 | 0.91 | 0.87–0.94 | 3.23 |
| TRALL | 32.96 ± 10.55 | 0.93 | 0.92–0.95 | 3.00 | 0.82 | 0.71–0.85 | 3.27 |
The measurement is crossed with the examiner and patient and examiner is a random factor
SD standard deviation, ICC inter- and intra-class correlation coefficient, CI confidence interval, MAD mean absolute difference
Table 2.
The overall means, standard deviations and ICC values of the outcome measures covering two readings by the three examiners for each group of 30 radiographs divided by the severity of scoliosis
| Methods | Mean and SD | Intraobserver reliability | Interobserver reliability | ||||
|---|---|---|---|---|---|---|---|
| ICC | 95% CI | MAD | ICC | 95% CI | MAD | ||
| Normal group | |||||||
| C L1–S1 | 39.88 ± 10.02 | 0.98 | 0.97–0.99 | 3.24 | 0.93 | 0.91–0.97 | 3.18 |
| C L1–L5 | 34.54 ± 11.09 | 0.98 | 0.97–0.99 | 2.22 | 0.94 | 0.90–0.97 | 3.03 |
| Centroid | 38.25 ± 11.61 | 0.97 | 0.96–0.98 | 3.46 | 0.90 | 0.83–0.95 | 5.81 |
| P L1–S1 | 40.68 ± 10.89 | 0.98 | 0.97–0.99 | 3.90 | 0.90 | 0.82–0.95 | 5.31 |
| P L1–L5 | 36.51 ± 10.62 | 0.98 | 0.96–0.98 | 2.91 | 0.92 | 0.87–0.96 | 3.54 |
| TRALL | 31.42 ± 8.64 | 0.96 | 0.93–0.97 | 3.33 | 0.91 | 0.84–0.95 | 2.96 |
| Low-grade group | |||||||
| C L1–S1 | 40.26 ± 13.36 | 0.95 | 0.92–0.96 | 3.11 | 0.88 | 0.84–0.96 | 4.31 |
| C L1–L5 | 34.10 ± 13.13 | 0.97 | 0.96–0.98 | 2.71 | 0.91 | 0.84–0.95 | 3.63 |
| Centroid | 35.73 ± 14.36 | 0.95 | 0.93–0.97 | 3.00 | 0.85 | 0.75–0.92 | 6.59 |
| P L1–S1 | 40.12 ± 12.47 | 0.91 | 0.86–0.94 | 3.71 | 0.81 | 0.68–0.90 | 6.33 |
| P L1–L5 | 37.49 ± 13.42 | 0.95 | 0.93–0.97 | 3.05 | 0.93 | 0.88–0.96 | 3.07 |
| TRALL | 35.50 ± 10.22 | 0.91 | 0.86–0.94 | 2.75 | 0.80 | 0.57–0.85 | 3.84 |
| High-grade group | |||||||
| C L1–S1 | 39.22 ± 18.35 | 0.93 | 0.89–0.95 | 2.85 | 0.66 | 0.48–0.81 | 6.93 |
| C L1–L5 | 37.23 ± 17.23 | 0.95 | 0.93–0.97 | 2.67 | 0.87 | 0.75–0.92 | 3.62 |
| Centroid | 33.00 ± 23.06 | 0.95 | 0.92–0.97 | 3.92 | 0.63 | 0.44–0.79 | 7.69 |
| P L1–S1 | 36.77 ± 20.39 | 0.91 | 0.87–0.94 | 2.97 | 0.60 | 0.40–0.76 | 7.17 |
| P L1–L5 | 30.74 ± 18.12 | 0.93 | 0.90–0.95 | 3.14 | 0.86 | 0.67–0.91 | 3.59 |
| TRALL | 31.97 ± 12.10 | 0.92 | 0.88–0.95 | 2.91 | 0.76 | 0.54–0.84 | 3.72 |
The measurement is crossed with the examiner and patient and the examiner is a random factor
SD standard deviation, CC inter- and intra-class correlation coefficient, CI confidence interval, MAD mean absolute difference
Discussion
Several investigators have developed a variety of methods for a radiographic evaluation of lumbar lordosis [4, 5, 7, 26]. However, measures that are not reproducible both internally and externally are not useful. Because, diagnosis and treatment of specific disease may depend on the measurement outcomes. The inter- and intra-observer reliability of several different measurement methods of lumbar lordosis in a normal population have been reported [4, 19, 22, 26]. Harrison et al. [16] compared the Cobb, centroid, posterior tangent, and TRALL methods for an analysis of segmental and global lumbar lordosis in a normal population. They reported that the inter- and intra-observer reliability of measuring all segmental and global angles were high (ICCs > 0.83). Chen et al. [4] compared the Cobb and centroid methods in measurement of global lordosis, and reported interobserver reliability coefficients for the vertebral centroid, Cobb L1–L5 and Cobb L1–S1 of 0.903, 0.826, and 0.784, respectively. They concluded that the vertebral centroid measurement is more reliable for assessing lumbar lordosis than the Cobb method. However, reliability might be different under specific conditions such as adult scoliosis. In this study, it was assumed that ICCs of the lumbar lordosis measurement method might be different in adult scoliosis radiographs. Edwards et al. [9] were the first to evaluate the reliability of the common scoliosis measures in adults. They demonstrated excellent intraobserver reliability for all parameters tested, except for curve differentiation. Good–excellent results of ICCs were obtained for all measures except for the sagittal and coronal Cobb angle and curve differentiation [9, 10]. However, they did not demonstrate the reliability in the lumbar lordosis measurement. Measurement of lumbar lordosis is important in diagnosis and treatment of adult scoliosis. Adult scoliosis patients often show lumbar hypolordosis [21, 23]. The global lumbar lordosis was lower in severe adult scoliosis, and lumbar hypolordosis is related to the spinopelvic orientation, which can rotate the pelvis and change the gross sagittal alignment of the spine. Glassman et al. [14] reported that restoration of a more normal sagittal balance is the critical goal for any reconstructive spine surgery in adult scoliosis. They mentioned that increased thoracic kyphosis and decreased global lumbar lordosis can break a sagittal balance in scoliosis. The global lordosis angle can be an important value in adult scoliosis, and accurate measurements of the lordosis angle are needed to examine adult scoliosis patients. However, measurements of the lumbar lordosis in adult scoliosis are difficult due to the degenerative changes in the vertebral body and endplate. In addition, axial, coronal and sagittal distortion of the spine often duplicates and blurs the vertebral silhouette. Therefore, the reliability of the lumbar lordosis measurement in adult scoliosis may be different from that in the normal population. If the measurement of lumbar lordosis is different between examiners in scoliosis, we cannot compare the pre- and post-operative global lumbar lordosis angle in the aspect of restoring the sagittal balance. And, if we want to treat adult scoliosis by fixation and fusion, it is important to establish the normal lumbar lordosis. In that case, we should calculate correct lordosis pre and post-operatively, so that we can obtain more aligned global lordosis and the sagittal balance. Therefore, in this study, we analyze the reliability of the global lordosis measurement method to suggest a better method in adult scoliosis patients. Clinically, segmental lumbar lordosis measurement is also important in the intervertebral cage insertion and segmental instability evaluation in scoliosis surgery. And, reliability of several segmental lordosis measurement methods in the normal population was reported [15–17]. However, in this study, we digitized the radiographs of aged degenerative spine (mean 62.1 years). It was very difficult drawing a multiple lines in a small segment which was obliterated by severe deformity and degeneration. And the ICCs of the segmental angles were lower than 0.38 in low- and high-grade scoliosis groups in this study. It was too low to compare the difference between measurement methods. Therefore, we could not compare the reliability of segmental lordosis measurement methods in scoliosis group and excluded segmental lordosis measurement in this study.
This study is the first to provide a reliability analysis of different global lumbar lordosis measurement methods in adult scoliosis, which can be implemented in a clinical evaluation. In the combined 90 radiographs, the ICCs were all high (ICCs ≥0.82, excellent) and MAD (2.53°–4.27°) was similar in all methods. However, in each of the scoliosis groups, the interobserver reliability decreased in proportion to the severity of the curve. The ICCs in Cobb L1–S1, the centroid and posterior tangent L1–S1 methods were ≥0.60 (fair to good) in the high-grade group. Only the Cobb L1–L5 and posterior tangent L1–L5 methods showed consistently high ICCs in the high-grade group (≥0.86, excellent). In addition, the Cobb L1–L5 and posterior tangent L1–L5 methods consistently demonstrated lower MAD for comparisons in all groups (≤3.63°). And, in the TRALL method, the ICCs were ≥0.76 (excellent) in all three groups, although these were lower than ICCs of Cobb L1–L5 and posterior tangent L1–L5 methods. And, in the TRALL method, the MAD was ≤3.84° in all groups. Between similar reliability of two methods, mean absolute difference (MAD) has been useful for determining the most reliable method. Chen et al. [4] reported that comparing the Cobb and his vertebral centroid method for lumbar lordosis in normal subjects, lower MAD of measurements (0.9°–1.7°) in centroid method. They conclude that centroid method is better than Cobb method with high ICCs and low MAD. Similarly, Harrison et al. concluded that all four methods are good in comparing of four lumbar lordosis method (centroid, Cobb, TRALL, posterior tangent), because they had high ICCs (>0.83) and very low MAD (0.6°–2.0°). And, they did not recommend the TRALL method despite the high reliability, because it lacks a segmental analysis [16]. They said that high ICCs and low MAD means high reliability of the methods, and proposed that MAD should be provided for an error analysis in the reliability studies. In another study, Harrison et al. [15] also reported that good to high ranges of ICCs and low MAD (0.9°–2.5°) means high reliability of the three methods, when comparing thoracic kyphosis measures (centroid, Cobb, posterior tangent). Therefore, the findings in this study demonstrate that the Cobb L1–5 and post tangent L1–5 methods are reliable global lumbar lordosis measurement methods regardless of the severity of scoliosis with higher ICCs and lower MAD, and the TRALL method can be a more reliable method than other methods which include the L5–S1 joint in lordosis measurement.
In this study, Cobb L1–5 and posterior tangent L1–5 method showed higher reliability. The posterior tangent can consider the slopes of the spinal curves at the midposterior body. It was assumed that the posterior tangent method had the highest average ICCs due to better radiographic visibility of the posterior vertebral body margins [26]. This is caused by the higher density of the posterior vertebral body compared with another corner of the vertebra. In this study, the L1–L5 posterior tangent method showed high inter- and intra-observer reliability in all groups (ICCs ≥0.86). Regardless of the degenerative changes, the posterior vertebral body margins of L1 and L5 were quite visible. Therefore, we can obtain higher ICCs and lower MAD. And, the Cobb method is the technique most commonly used by clinicians because it provides a simple and quick measurement of lumbar lordosis. Although, previous studies reported that the Cobb method is sensitive to contour changes, such as wedge, biconcave and brush, which resulted from degeneration [13, 22], and for the above reasons, several authors have included other radiographic measurement methods on the lateral radiographs, such as the posterior vertebral body tangents and the vertebral centroid methods [4, 26]. However, it might be different in scoliosis patients, as there is no report of scoliosis. In the present study, the interobserver and intraobserver reliability for the global L1–L5 Cobb angle was high with ICCs ≥0.87 in all groups. If the more prominent L1 and L5 vertebra body is chosen to evaluate the lumbar lordosis in scoliosis patients, Cobb’s method would be a reliable measurement method in adult scoliosis. And in this study, measurement from L1 to L5 resulted in better interobserver reliability than from L1 to S1 in Cobb and posterior tangent method. This result is compatible with the findings reported by Polly et al. [22], and explains why some authors believe that the superior endplate or posterior body of S1 is often difficult to visualize and hence choose L5. The S1 vertebra is often affected by degenerative changes and its contour usually invisible in arthritic patients. However, fixation in adult scoliosis often requires importance to L5–S1 joint and in that case we cannot ignore the methods that give reliability of L5–S1 joints. So reliable methods which include L5–S1 is also important. Cobb L1–S1, posterior tangent L1–S1, centroid and TRALL methods employ the S1 vertebra, which often affects the degenerative changes and smoothening effect. In this study, these methods showed lower ICCs than Cobb L1–L5 or posterior tangent L1–L5 method in the severe scoliosis group. However, in TRALL method, the ICCs were higher than 0.76 which was considered by Shrout and Fleiss to be ‘excellent’ and ‘substantial’ by Dunn [8, 24]. And, MAD was small (≤3.84°). Although TRALL method is labor intensive, requiring two times the number of reference line [16], we suggest that surgeons who routinely manage adult scoliosis including L5–S1 joint may choose the this method.
In conclusion, this study is the first to provide a reliability analysis of global lumbar lordosis measurement in adult scoliosis. The Cobb L1–L5 and posterior tangent L1–L5 methods are reliable methods for measuring the global lumbar lordosis in adult scoliosis. And the TRALL method is more reliable method than other methods which include the L5–S1 joint in lordosis measurement. Therefore, we suggest these methods for measures of global lordosis in adult scoliosis.
Acknowledgments
None.
References
- 1.Adams MA, Hutton WC. The effect of posture on the lumbar spine. J Bone Jt Surg [Br] 1985;67:625–629. doi: 10.1302/0301-620X.67B4.4030863. [DOI] [PubMed] [Google Scholar]
- 2.Bernhardt M, Bridwell KH. Segmental analysis of the sagittal plane alignment of the normal thoracic and lumbar spines and thoracolumbar junction. Spine. 1989;14:717–721. doi: 10.1097/00007632-198907000-00012. [DOI] [PubMed] [Google Scholar]
- 3.Carman DL, Browne RH, Birch JG. Measurement of scoliosis and kyphosis radiographs. Intraobserver and interobserver variation. J Bone Jt Surg [Am] 1990;72:328–333. [PubMed] [Google Scholar]
- 4.Chen YL. Vertebral centroid measurement of lumbar lordosis compared with the Cobb technique. Spine. 1999;24:1786–1790. doi: 10.1097/00007632-199909010-00007. [DOI] [PubMed] [Google Scholar]
- 5.Chernukha KV, Daffner RH, Reigel DH. Lumbar lordosis measurement. A new method versus Cobb technique. Spine. 1998;23:74–79. doi: 10.1097/00007632-199801010-00016. [DOI] [PubMed] [Google Scholar]
- 6.Cheung J, Wever DJ, Veldhuizen AG, Klein JP, Verdonck B, Nijlunsing R, Cool JC, Horn JR. The reliability of quantitative analysis on digital images of the scoliotic spine. Eur Spine J. 2002;11:535–542. doi: 10.1007/s00586-001-0381-7. [DOI] [PubMed] [Google Scholar]
- 7.Cobb J (1948) Outline for the study of scoliosis. Instructional course lectures. American Academy of Orthopaedic Surgeons, Ann Arbor, MI, pp 261–275
- 8.Dunn G. Design and analysis of reliability studies. Stat Methods Med Res. 1992;1:123–157. doi: 10.1177/096228029200100202. [DOI] [PubMed] [Google Scholar]
- 9.Edwards C, Hamill C, Baldus C (2007) Radiographic measurements in adult spinal deformity: what is the intra-observer reliability? In: 14th annual international meeting on advanced spinal techniques (IMAST). Paradise Island, Bahamas, 11–14 July
- 10.Edwards C, Wooten D, Baldus C (2007) Radiographic measurements in adult spinal deformity: what is the inter-observer reliability? In: 14th annual international meeting on advanced spinal techniques (IMAST). Paradise Island, Bahamas, 11–14 July
- 11.Fahrni WH, Trueman GE. Comparative radiological study of the spines of a primitive population with North Americans and northern Europeans. J Bone Jt Surg [Br] 1965;47:552–555. [PubMed] [Google Scholar]
- 12.Freedman BA, Horton WC, Rhee JM, Edwards CC, 2nd, Kuklo TR. Reliability analysis for manual radiographic measures of rotatory subluxation or lateral listhesis in adult scoliosis. Spine. 2009;34:603–608. doi: 10.1097/BRS.0b013e31819a841e. [DOI] [PubMed] [Google Scholar]
- 13.Genant HK, Li J, Wu CY, Shepherd JA. Vertebral fractures in osteoporosis: a new method for clinical assessment. J Clin Densitom. 2000;3:281–290. doi: 10.1385/JCD:3:3:281. [DOI] [PubMed] [Google Scholar]
- 14.Glassman SD, Berven S, Bridwell K, Horton W, Dimar JR. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine. 2005;30:682–688. doi: 10.1097/01.brs.0000155425.04536.f7. [DOI] [PubMed] [Google Scholar]
- 15.Harrison DE, Cailliet R, Harrison DD, Janik TJ, Holland B. Reliability of centroid, Cobb, and Harrison posterior tangent methods: which to choose for analysis of thoracic kyphosis. Spine. 2001;26:E227–E234. doi: 10.1097/00007632-200106010-00002. [DOI] [PubMed] [Google Scholar]
- 16.Harrison DE, Harrison DD, Cailliet R, Janik TJ, Holland B. Radiographic analysis of lumbar lordosis: centroid, Cobb, TRALL, and Harrison posterior tangent methods. Spine. 2001;26:E235–E242. doi: 10.1097/00007632-200106010-00003. [DOI] [PubMed] [Google Scholar]
- 17.Harrison DE, Harrison DD, Cailliet R, Troyanovich SJ, Janik TJ, Holland B. Cobb method or Harrison posterior tangent method: which to choose for lateral cervical radiographic analysis. Spine. 2000;25:2072–2078. doi: 10.1097/00007632-200008150-00011. [DOI] [PubMed] [Google Scholar]
- 18.Hedman TP, Fernie GR. Mechanical response of the lumbar spine to seated postural loads. Spine. 1997;22:734–743. doi: 10.1097/00007632-199704010-00004. [DOI] [PubMed] [Google Scholar]
- 19.Jackson RP, Kanemura T, Kawakami N, Hales C. Lumbopelvic lordosis and pelvic balance on repeated standing lateral radiographs of adult volunteers and untreated patients with constant low back pain. Spine. 2000;25:575–586. doi: 10.1097/00007632-200003010-00008. [DOI] [PubMed] [Google Scholar]
- 20.Morrissy RT, Goldsmith GS, Hall EC, Kehl D, Cowie GH. Measurement of the Cobb angle on radiographs of patients who have scoliosis. Evaluation of intrinsic error. J Bone Jt Surg Am. 1990;72:320–327. [PubMed] [Google Scholar]
- 21.Murata Y, Takahashi K, Hanaoka E, Utsumi T, Yamagata M, Moriya H. Changes in scoliotic curvature and lordotic angle during the early phase of degenerative lumbar scoliosis. Spine. 2002;27:2268–2273. doi: 10.1097/00007632-200210150-00016. [DOI] [PubMed] [Google Scholar]
- 22.Polly DW, Jr, Kilkelly FX, McHale KA, Asplund LM, Mulligan M, Chang AS. Measurement of lumbar lordosis. Evaluation of intraobserver, interobserver, and technique variability. Spine. 1996;21:1530–1535. doi: 10.1097/00007632-199607010-00008. [DOI] [PubMed] [Google Scholar]
- 23.Schwab FJ, Smith VA, Biserni M, Gamez L, Farcy JP, Pagala M. Adult scoliosis: a quantitative radiographic and clinical analysis. Spine. 2002;27:387–392. doi: 10.1097/00007632-200202150-00012. [DOI] [PubMed] [Google Scholar]
- 24.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420–428. doi: 10.1037/0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 25.Troyanovich SJ, Cailliet R, Janik TJ, Harrison DD, Harrison DE. Radiographic mensuration characteristics of the sagittal lumbar spine from a normal population with a method to synthesize prior studies of lordosis. J Spinal Disord. 1997;10:380–386. doi: 10.1097/00002517-199710000-00004. [DOI] [PubMed] [Google Scholar]
- 26.Troyanovich SJ, Harrison DE, Harrison DD, Holland B, Janik TJ. Further analysis of the reliability of the posterior tangent lateral lumbar radiographic mensuration procedure: concurrent validity of computer-aided X-ray digitization. J Manip Physiol Ther. 1998;21:460–467. [PubMed] [Google Scholar]