Abstract
Researchers and clinicians have long hypothesized that there are temperamental vulnerabilities to depressive disorders. Despite the fact that individual differences in temperament should be evident in early childhood, most studies have focused on older youth and adults. We hypothesized that if early childhood temperament is a risk factor for depressive disorders, it should be associated with better-established risk markers, such parental depression. Hence, we examined the associations of laboratory-assessed positive emotionality (PE), negative emotionality (NE), and behavioral inhibition (BI) with semi-structured interview-based diagnoses of parental depressive disorders in a community sample of 536 three-year old children. Children with higher levels of NE and BI had higher probabilities of having a depressed parent. However, both main effects were qualified by interactions with child PE. At high and moderate, but not low, levels of child PE, greater NE and BI were associated with higher rates of parental depression. Conversely, at low, but not high and moderate, levels of child NE, low PE was associated with a higher rate of parental depression. Child temperament was not associated with parental anxiety and substance use disorders. These findings indicate that laboratory-assessed temperament in young children is associated with parental depressive disorders, however the relations are complex and it is important to consider interactions between temperament dimensions rather than focusing exclusively on main effects.
Keywords: Child temperament, depression, parents, vulnerability, risk
Researchers have long hypothesized that temperament is a precursor or predisposing factor for mood disorders (Clark, 2005; Compas, Connor-Smith, & Jaser, 2004; Klein, Durbin, & Shankman, 2009). Currently, the leading temperament model of depressive disorders, proposed by Clark and Watson (e.g., Clark & Watson, 1999), posits that depression develops from low positive emotionality (PE) and high negative emotionality (NE). PE and NE are higher-order factors included in most structural models of temperament/personality in children and adults (Caspi & Shiner, 2006; Clark & Watson, 1999; Rothbart & Bates, 2006). PE has a number of facets, including positive affect, reward sensitivity, and sociability, although recent studies indicate that sociability may be less central than the affective and motivational components (Lucas, Diener, Grob, Suh, & Shao, 2000). NE refers to high negative mood reactivity, including fear, sadness, and anger. Clark and Watson (1999) hypothesized that low PE has a relatively specific association with depression, although it may also play a role in several other disorders, such as social phobia and schizophrenia. In contrast, high NE is a non-specific risk factor that plays a major role in anxiety disorders and a significant, but somewhat smaller, role in externalizing conditions such as substance use, antisocial personality, and conduct disorders (Clark, 2005).
Another temperament construct that may be related to risk for depressive disorders is behavioral inhibition (BI; Kagan, 1989). BI refers to a disposition for wariness, reticence, and decreased exploration in unfamiliar contexts and with unfamiliar people. Although BI is primarily viewed as predisposing to anxiety disorders, it may also play a role in depression (Fox, Henderson, Marshall, Nichols, & Ghera, 2005; Hirshfeld-Becker et al., 2008). BI overlaps with NE in that both include a substantial fear component (Muris & Dietvorst, 2006).
Many cross-sectional studies have reported that youth and adults with depressive disorders or symptoms exhibit diminished levels of PE and elevated levels of NE (e.g., Brown, Chorpita, & Barlow, 1998; Lonigan, Hooe, David, & Kirstner, 1999). In addition, prospective studies have found that low PE and high NE predict the onset of depressive episodes and increases in depressive symptoms (e.g., Kendler, Gatz, Gardner, & Pederson, 2006; Krueger, 1999; Lonigan, Phillips, & Hooe, 2003). However, the role of temperament in depressive disorders cannot be regarded as established due to three critical limitations in the literature.
First, most studies have used adults, and studies of youth have generally focused on older children and adolescents. As temperament is generally defined as individual differences in emotional reactivity and regulation that are evident by early childhood (Caspi & Shiner, 2006; Rothbart & Bates, 2006), it is critical to determine whether associations with risk for mood disorders are present in young children.
Second, with some notable exceptions (Hirschfeld et al., 1989; Kendler, Neale, Kessler, Heath, & Eaves, 1993; Kendler et al., 2006; Ormel, Oldehinkel, & Vollebergh, 2004), most studies have not excluded participants with a current or past history of depression. Thus, they cannot determine whether temperament predicts the onset of disorder as the assessment of temperament may have been influenced by current or prior depression. Moreover, excluding participants with current or past depression is also problematic if the sample has entered the risk period for depression, as it may remove the individuals at highest risk from the sample (Klein et al., 2009). Hence, a better approach is to study children before the age of risk for depression.
Third, almost all studies have used self-report measures of temperament. As virtually all of these studies have also assessed depression via self-report (either with questionnaires or interviews), this raises the possibility that associations are inflated by shared method variance. In addition, most self-report measures of NE, and to a lesser extent PE, have items that overlap with depressive symptoms (Ormel, Rosmalen, & Farmer, 2004), potentially creating a problem with measurement confounding.
Thus, research is needed to determine whether temperament in early childhood is associated with risk for depressive disorders. As the prevalence of depressive disorders in early childhood is extremely low (Lavigne, LeBailly, Hopkins, Gouze, & Binns, 2009), and young children cannot complete self-report inventories, studying this population also avoids the other problems discussed above. However, research on temperament in young children and risk for depression poses at least two significant challenges of its own. First, prospective studies of risk for depressive disorders in young children require 20–30 years to complete, as the incidence of mood disorders does not peak until young adulthood (Kessler et al., 2005). While long-term follow-up studies are ultimately necessary, in the short term a useful and informative strategy is to determine whether early child temperament is associated with known risk factors for depressive disorders. The best-established risk factor is parental history of depressive disorder (Hammen, 2009). Indeed, many investigators have hypothesized that the nature of the diathesis in the intergenerational transmission of depression involves a temperamental vulnerability (e.g., Silberg & Rutter, 2002).
Second, temperament in young children cannot be assessed with self-report. Hence, informants, such as parents, or behavioral observations must be used. Parent-reports have several strengths, including low cost and capitalizing on the parent’s observations of the child over time and across multiple contexts. However, parent reports can be influenced by the parent’s experience, frame of reference, and expectations (Kagan, 1998). This is particularly problematic in studies of the association between child temperament and parental depression, as the parent contributes information on both variables. In addition to the question of shared method variance, there is evidence that being depressed biases parents’ reports of child temperament, in that it is associated with greater discrepancies between parents’ reports and both other informants’ reports and laboratory measures of temperament (Leerkes & Crockenberg, 2003; Whiffen, 1990).
Observational measures, although time-consuming and limited to a single context and relatively brief time-frame, provide a more objective and controlled approach to assessing temperament in young children. However, few studies have examined the association between observational measures of early childhood temperament and risk for depressive disorders. In a seminal paper, Caspi, Moffitt, Newman, and Silva (1996) examined the associations between examiners’ global ratings collected when a large birth cohort of children was three years old and psychopathology at age 21. They found that a cluster of behaviors labeled as “inhibited”, which included a mixture of items tapping aspects of BI, NE, and low PE, predicted the development of major depressive disorder (MDD), but not anxiety and substance use disorders. Unfortunately, the assessment procedures were not specifically designed to assess temperament and the rating scales were not developed to reflect contemporary temperament models.
Four studies have examined the association between observational assessments of early childhood temperament and parental depressive disorders. Three of these studies focused exclusively on BI. In a sample of 88 2–3½ year olds, Kochanska (1991) found that the children of parents with bipolar disorder exhibited greater BI than children of non-depressed parents, but neither group differed from children of parents with MDD. In a pilot study (N = 56) and subsequent study (N = 284), Rosenbaum et al. (1988, 2000) reported that the 2–7 year old children of parents with a history of both panic disorder and MDD exhibited greater BI than children of healthy controls. However, children of parents with MDD alone and children of parents with panic disorder alone did not differ from any of the other groups. Finally, in a community sample of 100 three-year old children, Durbin, Klein, Hayden, Buckley, and Moerk (2005) found that child low PE, but not NE or BI, was associated with an increased risk of maternal depressive disorders. None of the three temperament dimensions were associated with risk for paternal depressive disorders.
Thus, data on the association between observational measures of temperament in young children and parental mood disorders are quite limited. Samples have generally been small; only one study examined PE and NE; and while more data are available for BI, the results are equivocal. We sought to provide a more conclusive test by conducting a family study of a large community sample of three-year old children to determine whether observational measures of child PE, NE, and BI are associated with a lifetime history of depressive disorder in their parents. We hypothesized that higher levels of child NE and BI and lower levels of child PE would be associated with parental depression. In addition, we examined two additional issues.
First, although Clark and Watson’s (1999) model emphasizes the roles of both low PE and high NE in risk for depression, they have not explicitly addressed the nature of the relation between the two dimensions (Shankman & Klein, 2003). One possibility is that they are additive, and the sum of the two dimensions determines risk. A second possibility is that they interact, reflecting a non-additive effect on risk. Although an interaction could take several forms (see Morris, Giesla, and Garber [2008]’s discussion in the context of cognitive vulnerability to depression), the most plausible is that the combination of high NE and low PE confers greater risk than the sum of the risks associated with each dimension alone. Only a handful of studies, all using adolescents or adults and self-report measures, have tested the interaction of PE and NE in predicting depression. Several studies found that the combination of low PE and high NE was associated with greater depression (Gershuny & Sher, 1998; Joiner & Lonigan, 2000; Wetter & Hankin, 2009), but others failed to find an interaction (Jorm et al., 2000; Kendler et al., 2006; Verstraeten, Vasey, Raes, & Bijttebier, 2009). To our knowledge, no studies have examined the relation between these two temperament dimensions in young children using observational measures, or with respect to their association with parental depression. Hence, we investigated whether the interaction between child PE and NE was associated with parental depressive disorders. Given the close conceptual and empirical association between BI and NE, we also explored the interaction of child PE and BI with parental depression, but we did not test the interaction of BI and NE due to the overlap between these constructs.
Second, to explore the specificity of the relationship between child temperament and parental psychopathology, we examined the associations of child PE, NE, and BI with parental anxiety and substance use disorders. We chose these broad groups for two reasons: (1) the existing literature provides a basis for clear hypotheses regarding their associations with PE and NE; and (2) along with depressive disorders, they are the most prevalent groups of disorders in community samples (e.g., Kessler et al., 2005). Based on Clark and Watson’s original model, we hypothesized that child NE would be associated with both parental anxiety and substance use disorders, whereas child PE would be unrelated to both groups of disorders in parents. However, as a number of studies have found that low PE is also associated with social phobia (e.g., Brown et al., 1998; Naragon-Gainey, Watson, & Markon, 2009), and some studies suggest that BI may be specifically associated with social phobia, rather than with a broader spectrum of anxiety disorders (Fox, Henderson et al., 2005; Hirshfeld-Becker et al., 2008), we conducted secondary analyses examining the associations between child temperament and parental social phobia.
Method
The sample consisted of 559 families from a suburban community. Potential participants were identified using a commercial mailing list and screened by telephone. Families with a child between three and four years of age who lived with an English-speaking biological parent and did not have significant medical conditions or developmental disabilities were included. Of eligible families, 66.4% entered the study. Families who agreed and declined to participate did not differ significantly on child sex and race/ethnicity and parental marital status, education, and employment status. Eighteen families without parental diagnostic data, three families in which one parent had bipolar disorder and the co-parent did not have a history of depressive disorder, and two families in which the child had already developed a mood disorder were excluded from the present analyses, leaving a final sample of 536.
The mean age of the children was 42.2 months (SD=3.1), and 289 (53.9%) were male. Mothers were 36.0 years (SD=4.5) and fathers were 38.3 years (SD=5.4) old. Most participants (86.9%) were White and middle class, as measured by Hollingshead’s Four Factor Index of Social Status (M=45.1; SD=10.9). Approximately half the mothers (54.7%) and fathers (45.7%) had at least a four-year college degree. Most children (95.0%) lived with both biological parents, and 51.9% of the mothers worked outside the home part- or full-time. Children were of average cognitive ability on the Peabody Picture Vocabulary Test (Dunn & Dunn, 1997; M=102.9, SD=13.9). The parent with primary caretaking responsibilities (generally the mother) was interviewed about the child with the Preschool Age Psychiatric Assessment (PAPA; Egger, Ascher, & Angold, 1999), which assesses psychopathology within the past three months. The two children with PAPA diagnoses of MDD or dysthymic disorder were excluded from the analyses.
Child Temperament
Each child and a parent (95.0% mothers) visited the laboratory for a 2-hour observational assessment of temperament that included a standardized set of 12 episodes selected to elicit a range of temperament-relevant behaviors. Eleven episodes were from the Laboratory Temperament Assessment Battery (Lab-TAB; Goldsmith, Reilly, Lemery, Longley, & Prescott, 1995) and one was adapted from a Lab-TAB episode. Using an independent sample, we previously reported moderate stability of laboratory ratings of temperament from ages 3 to 7 (r=.46 and .45 for PE and NE, respectively), and moderate concurrent and longitudinal associations between Lab-TAB ratings and home observations (Durbin, Hayden, Klein, & Olino, 2007). Each task was videotaped through a one-way mirror and later coded. To prevent carry-over effects, no episodes presumed to evoke similar affective responses occurred consecutively and each episode was followed by a brief play break to allow the child to return to a baseline affective state. The parent remained in the room with the child for all episodes except Stranger and Box Empty (see below), but was instructed not to interact with the child (except in Pop-Up Snakes), and was seated facing at a right angle from the experimenter and child and given questionnaires to complete.
The episodes, in order of presentation, were: (1) Risk Room. Child explored a set of novel and ambiguous stimuli, including a Halloween mask, balance beam, and black box; (2) Tower of Patience. Child and experimenter alternated turns in building a tower. The experimenter took increasing amounts of time before placing her block on the tower during each turn; (3) Arc of Toys. Child played independently with toys for five minutes before the experimenter asked the child to clean up the toys; (4) Stranger Approach. Child was left alone briefly in the room before a male accomplice entered, speaking to the child while slowly walking closer; (5) Make that Car Go. Child and experimenter raced remote-controlled cars; (6) Transparent Box. Experimenter locked an attractive toy in a transparent box, leaving the child alone with a set of non-working keys. After a few minutes, the experimenter returned and told the child that she had left the wrong set of keys. The child used the new keys to open the box and play with the toy; (7) Exploring New Objects. Child was given the opportunity to explore a set of novel and ambiguous stimuli, including a mechanical spider, a mechanical bird, and sticky soft gel balls; (8) Pop-up Snakes. Child and experimenter surprised the parent with a can of potato chips that actually contained coiled snakes; (9) Impossibly Perfect Green Circles. Experimenter repeatedly asked the child to draw a circle on a large piece of paper, mildly criticizing each attempt; (10) Popping Bubbles. Child and experimenter played with a bubble-shooting toy; (11) Snack Delay. Child was instructed to wait for the experimenter to ring a bell before eating a snack. The experimenter systematically increased the delay before ringing the bell; and (12) Box Empty. Child was given an elaborately wrapped box to open under the impression that a toy was inside. After the child discovered the box was empty, the experimenter returned with several toys for the child to keep.
Coding Procedures
Each display of facial, bodily and vocal positive affect, fear, sadness, and anger in each episode was rated on a three-point scale (low, moderate, high). Ratings were summed separately within each channel (facial, bodily, vocal) across the 12 episodes, standardized, and summed across the three channels to derive total scores for positive affect, fear, sadness, and anger. Interest was rated on a single four-point scale (none, low, moderate, and high) for each episode based on the child’s comments about the activity and how engaged the child was in play. Interest ratings were then summed across the 12 episodes. PE consisted of the sum of the standardized total positive affect and interest variables. NE was the sum of the standardized total sadness, fear, and anger variables.
BI was coded using an approach that was similar to most previous studies (e.g., Kagan, 1989; Pfeifer, Goldsmith, Davidson, & Rickman, 2002). The three episodes specifically designed to assess BI (Risk Room, Stranger Approach, Exploring New Objects) were divided into 20 or 30 second epochs, and a series of affective and behavioral codes were rated for each epoch (Goldsmith et al., 1995). Within each epoch, a maximum intensity rating of facial, bodily, and vocal fear was coded on a scale of 0 (absent) to 3 (highly present and salient). Based on previous studies using the Lab-TAB (Durbin et al., 2005; Pfeiffer et al., 2002), BI was computed as the average standardized ratings of latency to fear (reversed); and facial, vocal, and bodily fear (Risk Room, Stranger Approach, and Exploring New Objects); latency to touch objects; total number of objects touched (reversed); tentative play; referencing the parent; proximity to parent; referencing the experimenter; and time spent playing (reversed) (Risk Room and Exploring New Objects); startle (Exploring New Objects); sad facial affect (Exploring New Objects and Stranger Approach); and latency to vocalize; approach towards the stranger (reversed); avoidance of the stranger; gaze aversion; and verbal/nonverbal interaction with the stranger (reversed; Stranger Approach).
For each participant, different raters coded PE/NE and BI. Most episodes were coded by different raters. Coders were unaware of information on parental psychopathology. PE and NE had adequate internal consistency (α=.82 and .74, respectively) and inter-rater reliability (ICC=.89 and .82, respectively; N=35). BI exhibited good internal consistency (α=.80) and inter-rater reliability (ICC=.88; N=28). NE correlated −.12 (p<.01) with PE and .40 (p<.001) with BI; the correlation between PE and BI was −.22 (p<.001).
Parental Psychopathology
Children’s biological parents were interviewed using the Structured Clinical Interview for DSM-IV, Non-patient version (SCID-NP; First, Spitzer, Gibbon, & Williams, 1996). Interviews were conducted by telephone, which yields similar results as face-to-face interviews (Rohde, Lewinsohn, & Seeley, 1997), by two Masters-level raters with no knowledge of the temperament ratings. SCIDs were obtained from 535 (99.8%) mothers and 443 (82.6%) fathers. When parents were unavailable, family history interviews were conducted with the co-parent. Diagnoses based on family history data were obtained for an additional one (0.2%) mother and 83 (15.5%) fathers. Based on audiotapes of 30 SCID interviews, kappas for inter-rater reliability of lifetime diagnoses were .93 for mood disorder; .91 for anxiety disorder (.87 for social phobia); and 1.00 for substance abuse/dependence.
Of the children, 219 (40.9%) had at least one parent with a lifetime depressive disorder (35.3% MDD; 14.6% dysthymic disorder); 32.3% of mothers and 17.3% of fathers had a lifetime depressive disorder. Only 5.2% of children had a parent with current MDD or dysthymia. There were 237 children (44.2%) with a parent with a lifetime anxiety disorder (10.6% panic; 1.7% agoraphobia without panic; 20.7% social phobia; 18.5% specific phobia; 6.5% posttraumatic stress; 8.2% generalized anxiety; and 4.9% obsessive-compulsive disorder); 34.0% of mothers and 19.0% of fathers had a lifetime anxiety disorder. Finally, 264 children (49.3%) had a parent with a lifetime substance use disorder (44.6% alcohol abuse/dependence; 17.2% cannabis abuse/dependence; 9.5% hard drug abuse/dependence); 22.0% of mothers and 36.9% of fathers had a lifetime substance use disorder.
The clinical characteristics of the depressed parents who were directly interviewed were as follows (when both parents had SCID-diagnosed depression, we selected the more severe value): severity of worst lifetime MDD episode (28.4% mild; 46.4% moderate; 25.2% severe); onset of earliest depressive disorder (M=21.5 years; SD=8.6); and history of recurrent MDD episodes (32.5%).
Data Analyses
Preliminary analyses revealed significant gender differences in PE (t[534] 2.21, p<.05) and BI (t[534 3.56, p<.001). Girls exhibited greater PE (M=.11, SD=1.01) and BI (M=.16, SD=1.04) than boys (M=−.09, SD=.99; M=−.14, SD=.95; respectively). Gender was not associated with NE. There were no substantive differences in results when analyses included gender and temperament by gender interactions, so we do not consider child gender further.
Our primary analyses focused on the associations of child PE, NE, and BI with lifetime parental psychopathology. Secondary analyses examined associations with the three NE facets (sadness, fear, anger) and with maternal and paternal disorders separately. Analyses consisted of hierarchical multiple logistic regression models. Consistent with traditional bottom-up family study designs, and to facilitate testing interactions between temperament dimensions, child temperament variables were treated as independent variables (IVs) and parental psychopathology was the dependent variable. As these analyses are intended to test cross-sectional associations, we do not make any assumptions regarding direction of causality. IVs were centered, and cross-product terms were created by multiplying the relevant IVs to represent the interaction. Main effects were entered on the first step and interactions were entered on the second step. To interpret significant interactions, one temperament dimension was plotted against the predicted probability of parental depression at one SD above the mean, the mean, and one SD below the mean of the second dimension, and the significance of the simple slopes were tested (Jaccard, 2001). In interpreting these analyses, it is important to bear in mind that high and low levels of the moderator reflect participants’ relative standing in the sample, rather than the clinical significance of the trait.
Results
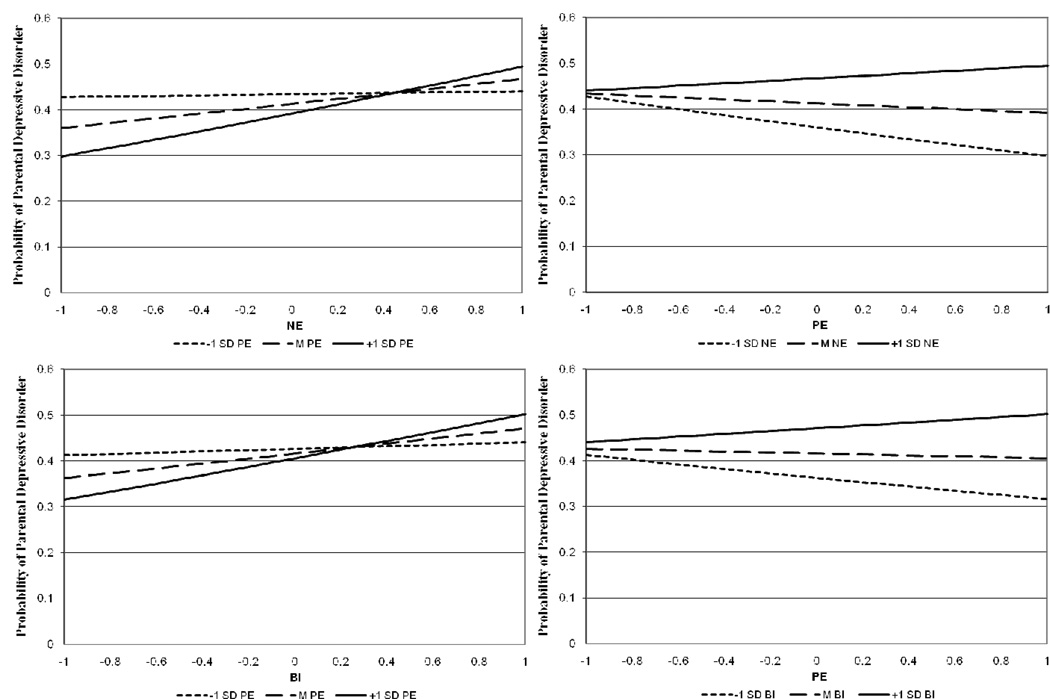
First, we examined the associations of child PE and NE with parental depressive disorders using hierarchical logistic regression (Table 1). The main effect for NE was significant; higher levels of child NE were associated with a greater predicted probability of parental depression. However, this was qualified by a significant PE X NE interaction. Interestingly, the interaction did not take the anticipated form of a synergistic effect of low PE and high NE. Instead, simple slopes tests indicated that at high (+1 SD) (B=.42, SE=.13; p<.01) and moderate (mean) (B=.22, SE=.09; p<.05) levels of child PE, increases in child NE were associated with a greater predicted probability of parental depressive disorder. In contrast, at low (−1 SD) levels of child PE, there was no association between child NE and parental depression (B=.03, SE=.11; p=.82) (Figure 1, top left).
Table 1.
Multiple logistic regression models of associations between child temperament and parental depressive disorder.
| Depressive Disorder | Depressive Disorder | ||
|---|---|---|---|
| OR (95% CI) | OR (95% CI) | ||
| Model 1 | Model 4 | ||
| PE | .92 (.76–1.09) | PE | .96 (.81–1.14) |
| NE | 1.25 (1.04–1.49)* | Fear | 1.26 (1.06–1.50)* |
| PE X NE | 1.22 (1.03–1.43)* | PE X Fear | [1.13 (.94–.136)] |
| Model 2 | Model 5 | ||
| PE | .96 (.79–1.15) | PE | .95 (.79–1.12) |
| BI | 1.25 (1.04–1.50)* | Anger | 1.04 (.88–1.24) |
| PE X BI | 1.18 (1.00–1.38)* | PE X Anger | [1.16 (.97–.138)] |
| Model 3 | |||
| PE | .92 (.77–1.10) | ||
| Sad | 1.19 (.98–1.44)+ | ||
| PE X Sad | 1.14 (1.00–1.29)* |
p<.10
p≤.05.
PE=positive emotionality; NE=negative emotionality; BI=behavioral inhibition. Bracketed ORs/CIs were dropped from the final models that included only main effects, the results of which appear in the table.
Figure 1.
Top: Relation between predicted probability of parental depressive disorder and child negative emotionality (NE) as a function of child positive emotionality (PE). Left panel: PE as moderator; right panel: NE as moderator. Bottom: Relation between predicted probability of parental depressive disorder and child behavioral inhibition (BI) as a function of child PE. Left panel: PE as moderator; right panel: BI as moderator.
As the choice of which temperament dimension to use as moderator is arbitrary, we also examined the association of child PE with parental depression at different levels of child NE (Figure 1, top right). Simple slopes tests indicated that at high and moderate levels of NE, child PE was not associated with parental depression (B=.11, SE=.11; p=.32 and B=−.09, SE=.09; p=.35, respectively). However, at low levels of NE, low child PE was associated with a greater probability of parental depression (B=−.28, SE=.14; p<.02).
We also examined the associations between each of the three facets of child NE (fear, sadness, and anger), child PE, and parental depressive disorder (Table 1). There was a significant main effect for fear, indicating that higher levels of child fearfulness were associated with a greater probability of parental depressive disorder. In addition, there was a marginally significant (p=.05) interaction between sadness and PE. The form of the interaction was similar to that described above for NE as a whole (figure available upon request). At high (B=.30, SE=.14; p<.05) and moderate (B=.17, SE=.10; p=.07) levels of child PE, increasing child sadness was associated with a greater predicted probability of parental depressive disorder. In contrast, at low levels of child PE, child sadness was not associated with the probability of parental depression (B=.05, SE=.10; p=.65). Reversing the moderator, at high and moderate levels of sadness, child PE was not associated with parental depression (B=.05, SE=.10; p=.66 and B=−.09, SE=.09; p=.36, respectively). However, at low levels of sadness, there was a trend for PE to be inversely associated with rates of parental depression (B=−.22, SE=.13; p<.09). There were no significant main or interaction effects for child anger.
Next, we examined the associations of child PE and BI with parental depression (Table 1). There was a significant main effect for BI, which was qualified by a significant PE X BI interaction. The form of the interaction was fairly similar to the PE X NE interaction described above. Simple slopes tests indicated that at high (B=.39, SE=.13; p<.01), and moderate (B=.22, SE=.09; p<.05), levels of child PE, increases in child BI were associated with a greater predicted probability of parental depressive disorder. However, at low levels of child PE, there was no association between BI and the probability of parental depression (B=.06, SE=.11; p=.60) (Figure 1, bottom left). Reversing the moderator (Figure 1, bottom right), at high and moderate levels of BI, PE was not associated with parental depression (B=.12, SE=.12; p=.29 and B=−.04, SE=.09; p=.69, respectively). At low levels of BI, there was a non-significant tendency for lower child PE to be associated with higher rates of parental depression (B=−.21, SE=.13; p=.11).
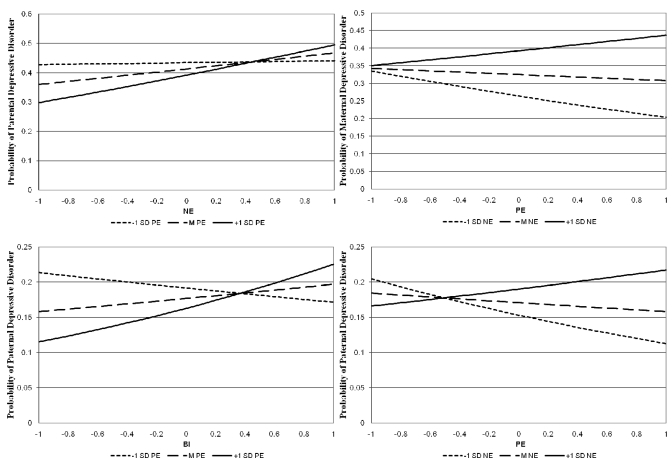
In the next set of analyses, we examined associations of child NE, PE, and BI with maternal and paternal depressive disorders separately. In the model examining child NE and PE and maternal depression, there was a non-significant main effect of PE (OR=.92, 95% CI=.761.12, p=.43), a significant main effect for NE (OR=1.34, 95% CI=1.11–1.62, p<.01), and a significant NE X PE interaction (OR=1.29, 95% CI=1.08–1.56, p<.01). Similar to the results for the sample as a whole, simple slopes tests indicated that at high (B=.55, SE=.14; p<.001) and moderate (B=.29, SE=.09; p<.01) levels of child PE, increasing child NE was associated with a greater probability of maternal depressive disorder. In contrast, at low levels of child PE, NE was not associated with maternal depression (B=.03, SE=.12; p=.08) (Figure 2, top left). When NE was used as the moderator, the results were also similar to those for both parents considered together. At high and moderate levels of NE, PE was not associated with maternal depression (B=.18, SE=.12; p=.13 and B=−.08, SE=.10; p=.43, respectively). However, at low levels of NE, PE was inversely associated with maternal depression (B=−.34, SE=.15; p<.03) (Figure 2, top right).
Figure 2.
Top: Relation between predicted probability of maternal depressive disorder and child negative emotionality (NE) as a function of child positive emotionality (PE). Left panel: PE as moderator; right panel: NE as moderator. Bottom: Relation between predicted probability of paternal depressive disorder and child behavioral inhibition (BI) as a function of child PE. Left panel: PE as moderator; right panel: BI as moderator.
In the model examining child BI and PE and maternal depression, there was a trend for a main effect for BI (OR=1.20, 95% CI=.99–1.44, p=.06). However, the main effect for PE (OR=.99, 95% CI=.81–1.19, p=.88) and the BI X PE interaction (OR=1.10, 95% CI=.94–1.29, p=.22) were not significant.
In the model for child PE and NE and paternal depression, the main effects for PE (OR=.95, 95% CI=.75–1.21, p=.68) and NE (OR=1.12, 95% CI=.89–1.41, p=.32) and the PE X NE interaction (OR=1.00, 95% CI=.83–1.21, p=.95) were all non-significant. However in the model examining child BI and PE and paternal depression, although the main effect for PE was non-significant (OR=.91, 95% CI=.71–1.16, p=.46), there was a trend for a main effect for BI (OR=1.14, 95% CI=.90–1.44, p=.06) and a significant PE X BI interaction (OR=1.31, 95% CI=1.04–1.63, p<.05). Simple slopes tests indicated that at high levels of child PE, BI was associated with a greater predicted probability of paternal depressive disorder (B=.40, SE=.17; p<.05). However, at moderate (B=.13, SE=.12; p=.27) and low (B=−.14, SE=.16; p=.43), levels of child PE, BI was not associated with the probability of paternal depression (Figure 2, bottom left). Reversing the moderator (Figure 2, bottom right), at high and moderate levels of child BI, PE was not associated with paternal depression (B=.17, SE=.16; p=.30 and B=−.09, SE=.13; p=.46, respectively). However, at low levels of BI, child PE was inversely associated with paternal depression (B=−.35, SE=.18; p=.05).
Next, we examined bivariate associations of child PE, NE, and BI with three clinical characteristics of parental depression (severity of worst MDD episode, age of onset of earliest depressive disorder, history of recurrent MDD) among children with a depressed parent. If both parents had histories of depression, the more severe value was used. None of these associations approached significance (available upon request).
Finally, we conducted hierarchical logistic regression analyses examining the associations of child temperament with parental anxiety and substance use disorders, as well as with parental social phobia specifically. No significant main or interaction effects were observed (Table 2).
Table 2.
Multiple logistic regression models of associations between child temperament and parental anxiety disorder, social phobia, and substance use disorder.
| Anxiety Disorders | Social Phobia | Substance Use | |
|---|---|---|---|
| Disorders | |||
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Model 1 | |||
| PE | 1.05 (.88–1.25) | .94 (.76–1.17) | 1.03 (.87–1.23) |
| NE | 1.00 (.84–1.19) | .87 (.69–1.08) | 1.11 (.94–1.32) |
| PE X NE | [1.03 (.89–1.20)] | [.96 (.75–1.23)] | [.99 (.85–1.14)] |
| Model 2 | |||
| PE | 1.04 (.87–1.24) | .93 (.75–1.15) | 1.06 (.89–1.26) |
| BI | .97 (.81–1.16) | .86 (.63–1.09) | 1.16 (.98–1.39) |
| PE X BI | [1.04 (.90–1.21)] | [1.13 (.86–1.50)] | [1.06 (.92–1.23)] |
p≤.05.
PE = positive emotionality; NE = negative emotionality; BI = behavioral inhibition. Bracketed ORs/CIs were dropped from the final models that included only main effects, the results of which appear in the table.
Discussion
We conducted a bottom-up family study of the associations between laboratory-assessed PE, NE, and BI in three-year old children and a history of depressive disorders in their parents using a large community sample. While some results were consistent with our hypotheses, others were unexpected. In accord with Clark and Watson’s (1999) tripartite model, higher levels of child NE were associated with a higher probability of parental depressive disorder. However, in contrast to the tripartite model and our prior findings with a smaller sample (Durbin et al., 2005), child PE was not directly associated with parental depression.1
These results were qualified by a significant interaction between child PE and NE. We had expected that if there was an interaction, greater levels of putative risk on both temperament dimensions (low PE and high NE) would be associated with a multiplicative increase in the probability of parental depression. Instead, we found that each temperament dimension was associated with parental depression only when the other temperament dimension was in the lower risk range. Thus, NE was positively associated with parental depressive disorders among children with moderate and high levels of PE, and child PE was inversely associated with parental depression among those with lower NE.
These findings are suggestive of the “dual vulnerability model” described by Morris et al. (2008), in which each of two risk factors is sufficient but neither is necessary to predict psychopathology. Thus, Morris et al. found that among adolescent girls with low (but not high) levels of stress, cognitive vulnerability predicted depressive symptoms, whereas among girls with low (but not high) levels of cognitive vulnerability, life stress predicted depressive symptoms.
It is unclear why our findings differed from our previous study (Durbin et al., 2005), which used largely similar methods. However, the current sample was over five times larger, providing greater power to detect main effects for NE and BI and PE X NE and PE X BI interactions. It is more difficult to explain the failure to find a main effect for PE in the present study. However, one possibility is that while the levels of PE were similar in both samples, the current sample exhibited a higher level of NE.2 As the present findings indicate that low PE is associated with higher rates of parental depression only at low levels of NE, the lower NE in the Durbin et al. sample may have obscured the interaction and created the appearance of a PE main effect.
The nature of the PE X NE interaction was also unexpected, although admittedly, Clark and Watson have not addressed the issue of an interaction between these dimensions (Shankman & Klein, 2003) and the few studies that have reported testing this interaction have yielded inconsistent findings (e.g., Verstraeten et al., 2009; Wetter & Hankin, 2009). Our sample consisted of young children, and it is conceivable that the nature of the associations between NE, PE, and parental depression could change over the course of development. It is increasingly recognized that temperament is only moderately stable and changes over time (Caspi & Shiner, 2006; Roberts, Walton, & Viechtbauer, 2006). This may, in part, be due to environmental influences, such as life stressors. Stress is, almost by definition, associated with NE and it appears to attenuate PE (Berenbaum & Connelly, 1993; Bogdan & Pizzagalli, 2006). At the same time, PE has been shown to buffer the effects of stress, which could, in turn, reduce levels of NE (Tugade & Fredrickson, 2004; Wichers et al., 2007). As parental depression is a marker of a chronically stressful environment (Hammen, 2009), it is conceivable that, over time, the combination of these processes could lead to both increasingly lower PE and higher NE in children with a depressed parent.
Analyses at the facet level revealed interesting differences in the associations of child fear, sadness, and anger with parental depressive disorders. Child fear was directly associated with parental depression, whereas the association of child sadness with parental depression was moderated by child PE. The former finding is consistent with studies reporting elevated levels of fear-related psychopathology in older offspring of depressed parents (Warner, Wickramaratne, & Weissman, 2008). Finally, child anger was not associated with parental depression in any analyses. These data support the importance of going beyond the superfactor level and examining associations at the facet level (Klein et al., 2009).
Previous studies of child BI and parental depression have yielded ambiguous findings (Kochanska, 1991; Rosenbaum et al., 1988, 2000), but used small samples or focused primarily on parental anxiety disorders. In the present study, the results for BI were fairly similar to those for NE. Thus, there was a significant main effect indicating that higher levels of child BI were associated with higher rates of parental depressive disorders. However, this was qualified by a BI X PE interaction. At moderate and high levels of PE, children with higher levels of BI had higher probabilities of parental depression, whereas at low levels of PE, child BI was not associated with parental depression. Although the simple slope for the inverse association of PE with parental depression at low levels of BI was not statistically significant, it was in the same direction as the corresponding association for NE and this effect was significant in the analyses for paternal depression.
We observed some differences in associations between temperament and maternal, as opposed to paternal, depression. Maternal depressive disorder was associated with the interaction between child PE and NE, whereas paternal depressive disorder was associated with the interaction between child PE and BI. While this could suggest that the gender of the depressed parent is associated with different temperamental vulnerabilities in children, there was considerable overlap between the confidence intervals of the odds ratios, indicating that these are probably not reliable differences.3
Interestingly, the associations between child temperament and parental psychopathology were specific to depressive disorders. Based on the larger literature, we had expected child NE and BI to be associated with parental anxiety disorders. However, consistent with Durbin et al. (2005), these associations were not significant. In addition, we examined parental social phobia separately, as a number of studies have reported that social phobia is characterized by both low PE as well as high NE (Narragon-Gainey et al., 2009), and BI appears to predict the development of social phobia more strongly than other anxiety disorders (Hirshfeld-Becker et al., 2008). However, child temperament was also unrelated to parental social phobia.
We were also somewhat surprised that child NE was not associated with parental substance use disorders. However, other temperament dimensions not examined in this report, such as non-affective constraint/effortful control appear to play a greater role in externalizing disorders (Clark, 2005; Krueger, Markon, Patrick, Benning, & Kramer, 2007; Rothbart & Bates, 2006).
In this paper, we focused on the associations between child temperament and parental depressive disorders, rather than elucidating the underlying causal processes. A variety of plausible mechanisms may be involved. For example, if particular temperament traits predispose to depression, parents with those traits are more likely to have a history of depression and to transmit the traits to their children. Alternatively, the genetic factors influencing temperament and depression may overlap, hence the liabilities to both would be transmitted together. Indeed, there is evidence for shared genetic factors in the transmission of NE and MDD (e.g., Kendler et al., 2006). Finally, as suggested above, depressed parents may provide an environment that amplifies NE and BI, and/or suppresses PE (e.g., Yap, Allen, & Ladouceur, 2008).
The present study had a number of strengths. Children were three years old, the age at which temperament begins to exhibit greater stability (Caspi & Shiner, 2006) and prior to the age of risk for even pediatric depression. Only two children had already developed a depressive disorder, and they were excluded. The sample was large, particularly given the time-intensive nature of the temperament assessments. We used an unselected community sample, avoiding the biases associated with clinical samples. Our measures of child temperament and parental psychopathology were independent, consisting of laboratory observations and semi-structured diagnostic interviews with both parents, respectively. Finally, we had sufficient power to examine temperament by temperament interactions.
However, the study also had limitations. First, the design was cross-sectional. It will be necessary to follow the children over time to determine whether temperamental emotionality predicts the onset of depressive disorders. Second, the laboratory observation of temperament was limited to a single session, hence it was influenced by situational, as well as trait factors, and may not provide a representative sample of behavior. However, as noted above, previous studies have demonstrated that laboratory temperament assessments are associated with home observations and exhibit moderate stability over time (Durbin et al., 2007; Pfeifer et al., 2002; Stifter, Putnam, & Jahromi, 2008). Third, in order to examine interactions between temperament traits, we treated temperament as the independent variable and parental psychopathology as the dependent variable. This is counterintuitive, as the direction of the effect probably runs from parent to child. Future studies might deal with this by exploring person-centered approaches within a longitudinal framework. Fourth, we may have included a few children who had recovered from a depressive episode more than three months before the assessment (the assessment period for the PAPA; Egger et al., 1999). However, the number of such cases would have been very small given the extremely low prevalence of depression in early childhood (Lavigne et al., 2009). Finally, the sample was primarily middle-class and Caucasian, which may limit generalizability.
In conclusion, this study adds to the nomological net linking early childhood temperament and risk for depression. Specifically, observational measures of child PE, NE, and BI were associated with the best-established risk marker for depressive disorders: parental depression. However, the associations were complex, involving interactions between PE and NE/BI. Further work is needed to understand the mechanisms responsible for these associations, determine whether early temperament actually predicts later depressive disorders, and delineate the processes and pathways that lead from early temperament to later mood disorders.
Acknowledgments
This work was supported by NIMH RO1-MH069942 (DNK) and GCRC Grant M01-RR10710 to Stony Brook University from the National Center for Research Resources.
The authors thank H. Hill Goldsmith for consultation on the Lab-TAB and James Jaccard for consultation on data analysis.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/ABN
In the analyses presented in Table 1, the main effects for PE and NE or BI were entered simultaneously. However, the non-significant main effects for PE are not due to partialling the effects of NE and BI, as the univariate association between PE and parental depression was not significant.
As the scoring system was extensively revised between the two studies, we cannot directly compare the temperament ratings from the videotaped episodes. However, in both studies, the experimenter completed a global rating scale after the laboratory visit that included identical sets of items for PE and NE (three items each; each item scored on a scale of 1–4). The mean PE scores in Durbin et al. and present studies were 9.86 (SD=2.44) and 10.01 (SD=2.30), respectively, t(635)=0.56, p=.58; the mean NE scores in the two studies were 7.69 (SD=1.89) and 9.49 (SD=2.10), respectively, t(635)=8.09, p<.001. The reason for the difference on NE is unclear, but it may be due to differences in recruitment methods (half the participants in Durbin et al. were recruited using ads and fliers and half were recruited with mailing lists whereas all participants in this study were recruited through mailing lists; it is conceivable that parents of high NE children are less likely to respond to ads for studies) and/or the laboratory battery (the current battery substituted an episode designed to elicit NE [Exploring New Objects] for an episode designed to elicit contentment [painting a picture]).
The ORs and 95% CIs for the associations of maternal and paternal depression with the child PE X NE interaction were 1.29 (1.08–1.56) and 1.03 (.85–1.23), respectively. The ORs and 95% CIs for the associations of maternal and paternal depression with the child PE X BI interaction were 1.10 (.94–1.29) and 1.31 (1.04–1.64), respectively.
Contributor Information
Thomas M. Olino, Western Psychiatric Institute and Clinic
Daniel N. Klein, Stony Brook University
Margaret W. Dyson, Stony Brook University
Suzanne A. Rose, Stony Brook University
C. Emily Durbin, Northwestern University.
References
- Berenbaum H, Connelly J. The effect of stress on hedonic capacity. Journal of Abnormal Psychology. 1993;102:474–481. doi: 10.1037//0021-843x.102.3.474. [DOI] [PubMed] [Google Scholar]
- Bogdan R, Pizzagalli DA. Acute stress reduces reward responsiveness: Implications for depression. Biological Psychiatry. 2006;60:1147–1154. doi: 10.1016/j.biopsych.2006.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TA, Chorpita BF, Barlow DH. Structural relationships among dimensions of the DSM-IV anxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. Journal of Abnormal Psychology. 1998;107:179–192. doi: 10.1037//0021-843x.107.2.179. [DOI] [PubMed] [Google Scholar]
- Caspi A, Moffitt TE, Newman DL, Silva PA. Behavioral observations at age 3 years predict adult psychiatric disorders. Archives of General Psychiatry. 1996;53:1033–1039. doi: 10.1001/archpsyc.1996.01830110071009. [DOI] [PubMed] [Google Scholar]
- Caspi A, Shiner RL. Personality Development. In: Eisenberg N, Damon W, Lerner RM, editors. Handbook of child psychology: Vol. 3, Social, emotional, and personality development. Hoboken, NJ: John Wiley & Sons Inc.; 2006. pp. 300–365. [Google Scholar]
- Clark LA. Temperament as a unifying basis for personality and psychopathology. Journal of Abnormal Psychology. 2005;114:505–521. doi: 10.1037/0021-843X.114.4.505. [DOI] [PubMed] [Google Scholar]
- Clark LA, Watson D. Temperament: A new paradigm for trait psychology. In: Pervin LA, John OP, editors. Handbook of personality. 2nd. ed. New York: Guilford Press; 1999. pp. 399–423. [Google Scholar]
- Compas BE, Connor-Smith J, Jaser SS. Temperament, stress reactivity, and coping: Implications for depression in childhood and adolescence. Journal of Clinical Child and Adolescent Psychology. 2004;33:21–31. doi: 10.1207/S15374424JCCP3301_3. [DOI] [PubMed] [Google Scholar]
- Dunn LM, Dunn LM. Peabody Picture Vocabulary Test. 3rd edition. Circle Pines, Minnesota: American Guidance Service; 1997. [Google Scholar]
- Durbin CE, Hayden EP, Klein DN, Olino TM. Stability of laboratory assessed temperament traits from ages 3 to 7. Emotion. 2007;7:388–399. doi: 10.1037/1528-3542.7.2.388. [DOI] [PubMed] [Google Scholar]
- Durbin CE, Klein DN, Hayden EP, Buckley ME, Moerk KC. Temperamental emotionality in preschoolers and parental mood disorders. Journal of Abnormal Psychology. 2005;114:28–37. doi: 10.1037/0021-843X.114.1.28. [DOI] [PubMed] [Google Scholar]
- Egger HL, Ascher BH, Angold A. The Preschool Age Psychiatric Assessment: Version 1.1. Durham, NC: Center for Developmental Epidemiology, Department of Psychiatry and Behavioral Sciences, Duke University Medical Center; 1999. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. The Structured Clinical Interview for DSM-IV Axis I Disorders – Non-patient edition. New York: Biometrics Research Department, New York State Psychiatric Institute; 1996. [Google Scholar]
- Fox NA, Henderson HA, Marshall PJ, Nichols KE, Ghera MM. Behavioral Inhibition: Linking biology and behavior within a developmental framework. Annual Review of Psychology. 2005;56:235–262. doi: 10.1146/annurev.psych.55.090902.141532. [DOI] [PubMed] [Google Scholar]
- Gershuny BS, Sher KJ. The relation between personality and anxiety: Findings from a 3-year prospective study. Journal of Abnormal Psychology. 1998;107:252–262. doi: 10.1037//0021-843x.107.2.252. [DOI] [PubMed] [Google Scholar]
- Goldsmith HH, Reilly J, Lemery K, Longley S, Prescott A. Laboratory Temperament Assessment Battery: Preschool Version. 1995 Unpublished manuscript. [Google Scholar]
- Hammen CL. Children of depressed parents. In: Gotlib IH, Hammen CL, editors. Handbook of Depression and Its Treatment. 2nd ed. New York: Guilford Press; 2009. pp. 275–297. [Google Scholar]
- Hirschfeld RMA, Klerman GL, Lavori P, Keller MB, Griffith P, Coryell W. Premorbid personality assessments of first onset of major depression. Archives of General Psychiatry. 1989;46:345–350. doi: 10.1001/archpsyc.1989.01810040051008. [DOI] [PubMed] [Google Scholar]
- Hirshfeld-Becker D, Micco J, Henin A, Bloomfield A, Biederman J, Rosenbaum J. Behavioral inhibition. Depression and Anxiety. 2008;25:357–367. doi: 10.1002/da.20490. [DOI] [PubMed] [Google Scholar]
- Jaccard J. Interaction Effects in Logistic Regression. Newbury Park: Sage; 2001. [Google Scholar]
- Joiner TE, Jr, Lonigan CJ. Tripartite model of depression and anxiety in youth psychiatric inpatients: Relations with diagnostic status and future symptoms. Journal of Clinical Child Psychology. 2000;29:372–382. doi: 10.1207/S15374424JCCP2903_8. [DOI] [PubMed] [Google Scholar]
- Jorm AF, Christensen H, Henderson AS, Jacomb PA, Korten AE, Rodgers B. Predicting anxiety and depression from personality: Is there a synergistic effect of neuroticism and extraversion? Journal of Abnormal Psychology. 2000;109:145–149. doi: 10.1037//0021-843x.109.1.145. [DOI] [PubMed] [Google Scholar]
- Kagan J. Temperamental contributions to social behavior. American Psychologist. 1989;44:668–674. [Google Scholar]
- Kagan J. Biology and the child. In: Eisenberg N, editor. Handbook of child psychology: Vol. 3: Social, emotional and personality development. 5th ed. New York: John Wiley; 1998. pp. 177–235. [Google Scholar]
- Kendler K, Gatz M, Gardner C, Pedersen N. Personality and major depression: A Swedish longitudinal, population-based twin study. Archives of General Psychiatry. 2006;63:1113–1120. doi: 10.1001/archpsyc.63.10.1113. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ. A longitudinal twin study of personality and major depression in women. Archives of General Psychiatry. 1993;50:853–862. doi: 10.1001/archpsyc.1993.01820230023002. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Klein DN, Durbin CE, Shankman SA. Depression and personality. In: Gotlib IH, Hammen CL, editors. Handbook of Depression. 2nd Ed. New York: Guilford Press; 2009. [Google Scholar]
- Kochanska G. Patterns of inhibition to the unfamiliar in children of normal and affectively ill mothers. Child Development. 1991;62:250–263. doi: 10.1111/j.1467-8624.1991.tb01529.x. [DOI] [PubMed] [Google Scholar]
- Krueger RF. Personality traits in late adolescence predict mental disorders in early adulthood: A prospective-epidemiological study. Journal of Personality. 1999;67:39–65. doi: 10.1111/1467-6494.00047. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Markon KE, Patrick CJ, Benning SD, Kramer MD. Linking antisocial behavior, substance use, and personality: An integrative quantitative model of the adult externalizing spectrum. Journal of Abnormal Psychology. 2007;116:645–666. doi: 10.1037/0021-843X.116.4.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavigne JV, LeBailly SA, Hopkins J, Gouze KR, Binns HJ. The prevalence of ADHD, ODD, depression, and anxiety in a community sample of 4-year-olds. Journal of Clinical Child & Adolescent Psychology. 2009;38:315–328. doi: 10.1080/15374410902851382. [DOI] [PubMed] [Google Scholar]
- Leerkes EM, Crockenberg SC. The impact of maternal characteristics and sensitivity on the concordance between maternal reports and laboratory observations of infant negative emotionality. Infancy. 2003;4:517–539. [Google Scholar]
- Lonigan CJ, Hooe ES, David CF, Kistner JA. Positive and negative affectivity in children: Confirmatory factor analysis of a two-factor model and its relation to symptoms of anxiety and depression. Journal of Consulting and Clinical Psychology. 1999;67:374–386. doi: 10.1037//0022-006x.67.3.374. [DOI] [PubMed] [Google Scholar]
- Lonigan CJ, Phillips BM, Hooe ES. Relations of positive and negative affectivity to anxiety and depression in children: Evidence from a latent-variable longitudinal study. Journal of Consulting and Clinical Psychology. 2003;71:465–481. doi: 10.1037/0022-006x.71.3.465. [DOI] [PubMed] [Google Scholar]
- Lucas RE, Diener E, Grob A, Suh EM, Shao L. Cross-cultural evidence for the fundamental features of extraversion. Journal of Personality and Social Psychology. 2000;79:452–468. doi: 10.1037//0022-3514.79.3.452. [DOI] [PubMed] [Google Scholar]
- Morris MC, Ciesla JA, Garber J. A prospective study of the cognitive diathesis-stress model of depressive symptoms in adolescents. Journal of Abnormal Psychology. 2008;117:719–734. doi: 10.1037/a0013741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muris P, Dietvorst R. Underlying personality characteristics of behavioral inhibition in children. Child Psychiatry & Human Development. 2006;36:437–445. doi: 10.1007/s10578-006-0014-9. [DOI] [PubMed] [Google Scholar]
- Narragon-Gainey K, Watson D, Markon KE. Differential relations of depression and social anxiety symptoms to the facets of extraversion/positive emotionality. Journal of Abnormal Psychology. 2009;118:299–310. doi: 10.1037/a0015637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ormel J, Oldehinkel AJ, Vollebergh W. Vulnerability before, during, and after a major depressive episode. Archives of General Psychiatry. 2004;61:990–996. doi: 10.1001/archpsyc.61.10.990. [DOI] [PubMed] [Google Scholar]
- Ormel J, Rosmalen A, Farmer A. Neuroticism: A non-informative marker of vulnerability to psychopathology. Social Psychiatry and Psychiatric Epidemiology. 2004;39:906–912. doi: 10.1007/s00127-004-0873-y. [DOI] [PubMed] [Google Scholar]
- Pfeifer M, Goldsmith HH, Davidson RJ, Rickman M. Continuity and change in inhibited an uninhibited children. Child Development. 2002;73:1474–1485. doi: 10.1111/1467-8624.00484. [DOI] [PubMed] [Google Scholar]
- Roberts BW, Walton KE, Viechtbauer W. Patterns of mean-level change in personality traits across the life course: A meta-analysis of longitudinal studies. Psychological Bulletin. 2006;132:1–25. doi: 10.1037/0033-2909.132.1.1. [DOI] [PubMed] [Google Scholar]
- Rohde P, Lewinsohn PM, Seeley JR. Comparability of telephone and face-to-face interviews assessing Axis I and II disorders. American Journal of Psychiatry. 1997;154:1593–1598. doi: 10.1176/ajp.154.11.1593. [DOI] [PubMed] [Google Scholar]
- Rosenbaum JF, Biederman J, Gersten M, Hirshfeld DR, Meminger SR, Herman JB, et al. Behavioral inhibition in children of parents with panic disorder and agoraphobia: A controlled study. Archives of General Psychiatry. 1988;45:463–470. doi: 10.1001/archpsyc.1988.01800290083010. [DOI] [PubMed] [Google Scholar]
- Rosenbaum JF, Biederman J, Hirshfeld-Becker DR, Kagan J, Friedman D, Nineberg A, Gallery DJ, Faraone SV. A controlled study of behavioral inhibition in children of parents with panic disorder and depression. American Journal of Psychiatry. 2000;157:2002–2010. doi: 10.1176/appi.ajp.157.12.2002. [DOI] [PubMed] [Google Scholar]
- Rothbart MK, Bates JE. Temperament in children’s development. In: Damon W, Lerner R, Eisenberg N, editors. Handbook of child psychology, sixth edition: Social, emotional, and personality development. Vol. 3. New York: John Wiley; 2006. pp. 99–166. [Google Scholar]
- Shankman SA, Klein DN. The comorbidity between depression and anxiety: An evaluation of the tripartite, approach-withdrawal, and valence-arousal models. Clinical Psychology Review. 2003;23:605–637. doi: 10.1016/s0272-7358(03)00038-2. [DOI] [PubMed] [Google Scholar]
- Stifter CA, Putnam S, Jahromi L. Exuberant and inhibited toddlers: Stability of temperament and prediction to behavior problems. Development and Psychopathology. 2008;20:401–421. doi: 10.1017/S0954579408000199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silberg J, Rutter M. Nature-nurture interplay in the risks associated with parental depression. In: Goodman SH, Gotlib IH, editors. Children of depressed parents: Alternative pathways to risk for psychopathology. Washington, D.C: American Psychological Association Press; 2002. pp. 13–36. [Google Scholar]
- Tugade MM, Fredrickson BL. Resilient individuals use positive emotions to bounce back from negative emotional experiences. Journal of Personality and Social Psychology. 2004;86:320–333. doi: 10.1037/0022-3514.86.2.320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verstraeten K, Vasey MW, Raes F, Bijttebier P. Temperament and risk for depressive symptoms in adolescence: Mediation by rumination and moderation by effortful control. Journal of Abnormal Child Psychology. 2009;37:349–361. doi: 10.1007/s10802-008-9293-x. [DOI] [PubMed] [Google Scholar]
- Warner V, Wickramaratne P, Weissman M. The role of fear and anxiety in the familial risk for major depression: A three-generation study. Psychological Medicine. 2008;38:1–14. doi: 10.1017/S0033291708002894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wetter EK, Hankin BL. Mediational pathways through which positive and negative emotionality contribute to anhedonic symptoms of depression: A prospective study of adolescents. Journal of Abnormal Child Psychology. 2009;37:507–520. doi: 10.1007/s10802-009-9299-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whiffen VE. Maternal depressed mood and perceptions of child temperament. Journal of Genetic Psychology. 1990;151:329–339. doi: 10.1080/00221325.1990.9914621. [DOI] [PubMed] [Google Scholar]
- Wichers MC, Myin-Germeys I, Jacobs N, Peeters F, Kenis G, Derom C, et al. Evidence that moment-to-moment variation in positive emotions buffer genetic risk for depression: A Momentary assessment twin study. Acta Psychiatrica Scandinavica. 2007;115:451–457. doi: 10.1111/j.1600-0447.2006.00924.x. [DOI] [PubMed] [Google Scholar]
- Yap MBH, Allen NB, Ladouceur CD. Maternal socialization of positive affect: The impact of invalidation on adolescent emotion regulation and depressive symptomatology. Child Development. 2008;79:1415–1431. doi: 10.1111/j.1467-8624.2008.01196.x. [DOI] [PubMed] [Google Scholar]