Abstract
Purpose
Most studies have reported the effects of short-term double-J ureteral stenting on patient symptoms. We reviewed the changes in symptoms and the factors associated with tolerance due to long-term stenting.
Materials and Methods
We investigated 20 patients (mean age±SD, 58.3±11.8 years). The patients consisted of those with cervical cancer (n=12), retroperitoneal fibrosis (n=5), colon cancer (n=1), rectal cancer (n=1), and endometrial cancer (n=1). A questionnaire that included domains for urinary symptoms and quality of life (QoL) scores for evaluation of urinary symptoms (International Prostate Symptom Score, or IPSS), a 10-cm linear visual analogue scale (VAS) score rated from 0 (no pain) to 10 (unendurable pain) for tolerance, and uroflowmetry were performed at every replacement.
Results
Frequency and urgency on the storage symptom score, residual urine sensations, and intermittency on the voiding symptom score were significantly aggravated at the initial stenting (p<0.05), but the sum of the storage symptom score and urgency improved with time (p<0.05). The quality of life score and total IPSS score also changed significantly (p<0.05). However, although the QoL score and the total IPSS score after stenting were not decreased to less than before stenting, the QoL score was significantly decreased at 9 months (p<0.05), and the total IPSS score was significantly decreased at 12 months (p<0.05).
Conclusions
The symptoms were acutely aggravated at first, but the results showed increased tolerance with time. Adaptation of the bladder and desensitization of the patients may be important factors in the increased tolerance.
Keywords: Stent, Symptom, Quality of life, Tolerance
Introduction
Insertion of a ureteral stent is one of the most common procedures in urology. Self-retaining ureteral stents have been commonly used to relieve obstruction of the upper urinary tract since Finney et al. initially introduced them [1]. In addition, ureteral stents are often inserted prophylactically if patients are at risk for upper urinary tract obstruction following various procedures, such as ureteroscopy, percutaneous nephrolithotomy, pyeloplasty, ureterolithotomy, and ureteral end-to-end anastomosis; moreover, they can be inserted for relieving ureteral obstruction due to extrinsic causes.
Unfortunately, discomfort associated with ureteral stents is a complaint of a high proportion of patients (up to 80%); stents have a negative impact on health-related QoL [2,3]. Storage bladder symptoms, incontinence, hematuria, and dysuria are the most common problems [2,3]. However, the underlying pathophysiology associated with the urinary symptoms caused by ureteral stents remains unknown. In reported studies, several factors have been investigated for their effects on symptoms related to stent insertion; the factors that have been previously studied include the stent length, diameter, material, softness, position, and loop completeness [4-7]. However, only a few studies on the urinary symptoms associated with stents have been reported, and reports on changes in voiding symptoms and the ability to tolerate long-term stenting are rare.
Consequently, we conducted a retrospective study on the changes in symptoms and the factors associated with tolerance of double-J ureteral stents over time.
Materials and Methods
We investigated 20 patients (mean age±SD, 58.3±11.8 years) who changed double-J ureteral stents between December 2002 and June 2008. The double-J ureteral stents were kept in place for long periods of time, over 12 months (mean period of time, 21.1 months range, 12-38 months), in all patients. The mean age of the 5 male patients was 69±8.12 years (range, 58-79 years), and the mean age of the 15 female patients was 54.7±10.69 years (range, 36-73 years).
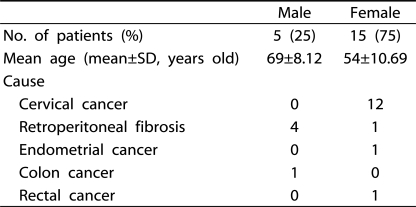
The criteria for inclusion in this study were as follows: patients with ureteral obstruction that could not be cured by surgery and who were not good candidates for surgery, especially patients with a short life expectancy such as those with an advanced non-urological malignancy, and who consequently required long-term stents. Patients with urogenital malignancies and the presence of bilateral obstruction and those who had additional procedures and were taking medication such as alpha blockers and anticholinergics before the initial double-J ureteral stenting were excluded from this study to avoid patient heterogeneity. Patients who had malignancies with bladder invasion or other urogenital organic metastases were also excluded. Table 1 lists the characteristics of the patients.
Table 1.
characteristics of the patients
SD: standard deviation
The stents were placed as either an outpatient or an inpatient procedure with the use of local anesthesia. At the time of placement of the stent, C-arm fluoroscopy was always used for exact placement of the stents. Then, a plain abdominal radiograph (kidney ureter and bladder; KUB) was routinely obtained to confirm correct placement of the stents. Two types of polyurethane double-J ureteral stents (Cook®, USA, 6 Fr, 24-26 cm) were used in all patients, and the length of the stent was selected on the basis of the height of the patient.
The double-J stents were mostly replaced every three months; the timing of replacement varied according to the patients' condition (degree of ureteral stricture, encrustation of stents, and discomfort due to the stent). Microscopic and microbiological examination of the urine and standard radiological studies (kidney ureter and bladder; KUB) were performed at the time of every replacement.
Assessment of stent-related urinary symptoms and patient tolerance was performed by collecting information from a questionnaire that included a quality of life (QoL) score (International Prostate Symptom Score, IPSS) and a 10 cm linear visual analogue scale (VAS) score rated from 0 (no pain) to 10 (unendurable pain) at every replacement. Although the IPSS questionnaire did not completely cover the urinary symptoms, and other questionnaires related to ureteral stenting were introduced, we used the IPSS questionnaire because of its greater popularity and precise description. At the same time, patients underwent uroflowmetry evaluation (CUBE Flow, Mcube Technology, Korea), and postvoid residual urine was determined by using an automated bladder scan (Biocon-500™, Mcube Technology, Korea).
The data were analyzed by using non-parametric tests, including the Friedman test, Bonferroni correction, and Mann-Whitney U test, because of sample size. The Friedman test showed only whether there was a significant change between pre-stenting and 12 months, and then Bonferroni correction, which is a multiple-comparison test, showed whether there was a significant difference between each 3 month period from pre-stenting to 12 months. Multiple regression analysis was used to determine whether gender, catheter length, history of intrapelvic radiotherapy, or bacteriuria influenced urinary symptoms, VAS score, and QoL. The results were considered significant at a p<0.05. All statistical analyses were performed by using the Statistical Package for the Social Sciences for Windows version 17.0 (SPSS Inc. Chicago, USA).
Results
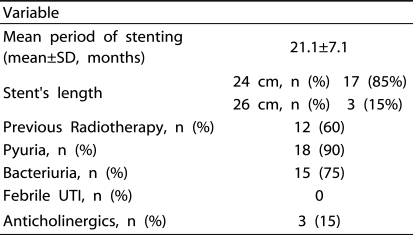
Twelve patients (60%) had undergone previous intrapelvic radiotherapy. No patients had urinarytract infection before double-J ureteral stenting. However, microscopic examination of the urine during the stenting revealed significant pyuria (>5 pus cells/high-power field) in 18 patients (90%), and 15 of them had positive urine cultures (Enterobacter, Staphylococcus, Proteus, Klebsiella, and especially Escherichia coli). However, no patient had febrile urinary tract infection. The 24 cm and 26 cm double-J catheter were used in 13 and 7 patients, respectively (Table 2).
Table 2.
Baseline characteristics of patients that underwent placement of stents for over 12 months
SD: standard deviation, UTI: urinary tract infection
All patients experienced discomfort from the double-J ureteral stent and reported one or more of the following symptoms: frequency, urgency, nocturia, sense of residual urine, intermittency, weak stream, and hesitancy.
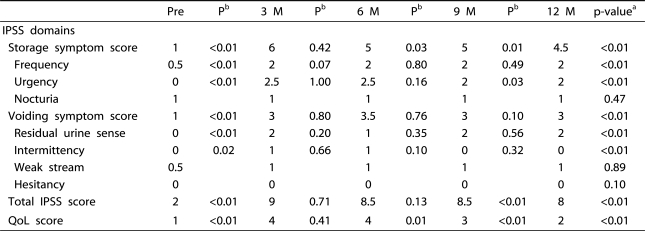
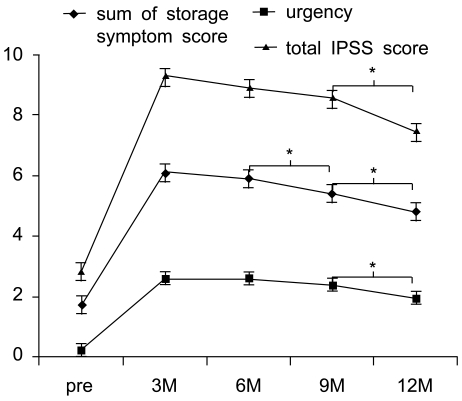
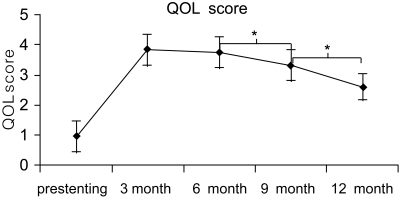
The changes in the urinary symptoms with time are shown in Table 3. Frequency and urgency on the storage symptom score, residual urine sensations, and intermittency on the voiding symptom score were all significantly aggravated at the initial stenting (Friedman test. p<0.05), but the sum of the storage symptom score and urgency were improved with time (Bonferroni correction, p<0.05) (Figure 1). The QoL score and total IPSS score also changed significantly due to double-J ureteral stenting (Friedman test, p<0.05). Although the total IPSS score and the QoL score after stenting were not decreased to less than before stenting, the total IPSS score was significantly decreased at 12 months (Bonferroni correction. p<0.05), and the QoL score was significantly decreased at 9 months (Bonferroni correction. p<0.05) (Figure 2).
Table 3.
Types of stent related urinary symptoms over time (Data presented as median score)
P-valuea: Friedman test (only showed whether there was significant change between pre-stenting and 12 months)
Pb: p-value = Bonferroni correction (multiple comparison test, showed whether there was significant difference between each 3 months from pre-stenting to 12 months)
Pre: pre-stenting, IPSS: International Prostate Symptom Score, QoL: Quality of Life, M: months
Figure 1.
Changes of urinary symptoms showing significant improvement. The bar indicates the standard deviation. The Friedman test showed significant differences among five measures (p=0.000). *: The Bonferroni correction showed significant decrease
Figure 2.
Change of QOL score, preoperative, 3, 6, 9, 12 months. The bar indicates the standard deviation. The Friedman test showed significant differences among five measures (p=0.000). *: The Bonferroni correction showed significant decrease QOL: quality of life
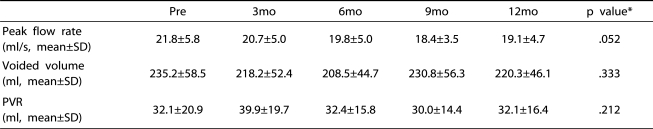
On the uroflowmetry testing, the peak flow rate, voided volume, and postvoid residual urine volume were not significantly changed (Table 4).
Table 4.
Results of uroflowmetry testing in 20 patients, pre-stenting, 3, 6, 9, 12 months after indwelling double J ureteral stents were placed
*: p value :Friedman test (This test used to investigate whether change of score with time was significant.)
SD: standard deviation, Pre: pre-stenting, PVR: postvoided residual volume
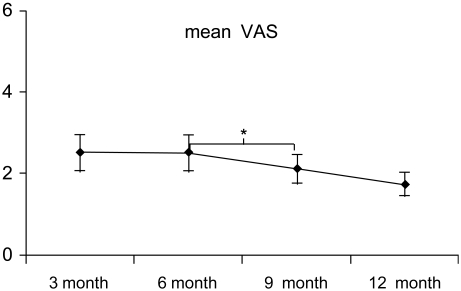
The VAS score was significantly decreased at 9 months (Bonferroni correction. p=0.002) (Figure 3). In addition, the multiple regression analysis showed that there were no statistically significant effects of gender, catheter length, history of intrapelvic radiotherapy, or bacteriuria on the VAS score.
Figure 3.
Change of the VAS score, pre-operative, 3, 6, 9, 12 months: The bar indicates the standard deviation. The Friedman test showed a significant difference. (p=0.001) *: The Bonferroni correction showed significant decrease VAS: visual analogue scale
Discussion
Double-J ureteral stents are widely used for the management of upper urinary tract obstruction and for preventing complications after ureteral surgery. The use of ureteral stents continues to increase with ureteroscopy procedures [8,9]. Many patients with urinary obstruction from nonurological malignancies that affect the urinary tract are not candidates for surgery and have a relatively short-term survival; these patients are candidates for ureteral stenting. Such stenting is associated with unfavorable symptoms including flank pain, frequency, urgency, dysuria, and hematuria [10-13].
The etiology of the discomfort associated with symptoms is not completely understood. Some have suggested that high pressure transmitted to the renal pelvis with urine in the bladder and trigonal irritation by the intravesical part of the stent could be irritating factors. In addition, Deliveliotis et al. suggested that stent-related pain and urinary frequency could be related to lower ureteral spasm or local trigone sensitivity [14]. These symptoms usually continue until removal of the ureteral stents. In cases with long-term placement, encrustation or fragmentation might occur [3,10,13].
Damiano et al. reported that early complications of a double pigtail stent appeared during the first 4 weeks after stent insertion and included discomfort, irritative bladder symptoms, hematuria, bacteriuria with or without clinical urinary tract infection, fever, and flank pain for reflux also, the late complications resulted in hydronephrosis, upward and downward stent migration, fragmentation, and breakage [15]. They argued that morbidity was minimal with indwelling polyurethane stenting for up to 3 months, but that longer times are associated with increased frequency of encrustation, infection, secondary stone formation, and obstruction of the stented tract. However, they surveyed the voiding symptoms during only the early phase and thus could not determine changes in the voiding symptoms.
Established studies of the symptoms associated with ureteral stents have mainly been comparisons of the kinds of stents or materials used for the stents and do not provide enough help for precise information for each patient about tolerance and changes in voiding symptoms due to indwelling ureteral stents with time.
Irani et al. also reported improved tolerance of symptoms with time and that dysuria and hematuria also improved with time [16]. They found no significant gender differences. The men reported more severe symptoms than did the woman. This might be explained by the differences in instrumentation; however, the men did not adjust to the irritation, which was relieved only after the stent was removed. Similarly, in our study, there were no gender differences. Lee et al. reported on a comparison of patients with ureteral stents placed after ureteroscopic lithotripsy for 3 days and for 2 weeks; 84% of the patients reported urgency, lower abdominal discomfort, and other urinary symptoms, and there was no difference in the symptoms over time [17].
Among the stent-related symptoms, urgency, frequency, and suprapubic discomfort are similar to the symptoms associated with an overactive bladder (OAB), which is caused by involuntary contraction of the bladder mediated by muscarinic receptors. The symptoms such as storage symptoms, incontinence, and dysuria are examples of the significant impact of stents on patients' QoL. Agarwal et al. reported a significant reduction in the incidence and severity of bladder catheter-related discomfort during the postoperative period in patients who had received either oxybutynin or tolterodine before surgery [18]. However, Norris et al. reported that neither oxybutynin nor phenazopyridine was different from placebo in providing relief of stent-related symptoms [19]. Recently, Park et al. reported that tolterodine ER significantly improved urinary symptoms and reduced stent-related pain [20]. Therefore, physicians can consider prescribing anticholinergics for patients with severe urinary symptoms due to ureter stenting, but more studies of the effects of anticholinergics must be performed. Also, in another study by Damiano et al., tamsulosin proved to be efficacious in improving stent-related morbidity [21]. Because of such effects, we excluded patients taking a-blocker medication in this study design. The data showed that flank pain and urinary symptoms decreased at 1 week and the general health index score increased.
The purpose of our study was to show how urinary symptoms changed naturally with time. Our results showed a type and rate of complications similar to that in other studies. Also, the results of this study showed that most voiding symptoms, the quality of life, and the VAS score changed significantly with time, and the results did not show a gender difference. As our results showed, all patients with double-J ureteral stenting showed significantly aggravated urinary symptoms and pain after stenting. However, the VAS score and QoL score significantly decreased at 9 months, and the total IPSS score significantly decreased at 12 months, which represented an improvement in patient tolerance over time. The explanation for this is unclear; adaptation of the bladder and desensitization of the patients might be important factors. Thus, we determined that the QoL score improved as several urinary symptoms and the VAS score improved with time.
The limitations of this study include the small sample size and the collection of information from questionnaires. In addition, the urinary symptoms studied were not a complete list of possible symptoms. However, the changes in urinary symptoms, quality of life, and pain due to long-term ureteral stenting that we studied showed significant improvement after 9 months. Thus, physicians should consider active medication with anti-cholinergics for patients suffering long-term stenting until 9 months and can expect natural improvement of urinary symptoms, quality of life, and pain without treatment after 9 months.
Nevertheless, a prospective, randomized study with more detailed symptom assessment and a larger sample size will be performed.
Conclusions
The stent-related symptoms were mostly aggravated at the time of stenting. However, the stent-related urinary symptoms, quality of life, and pain improved over time. We suggest that adaptation of the bladder and desensitization of the patients might be important factors in this improvement.
References
- 1.Finney RP. Experience with new double J ureteral catheter stent. J Urol. 1978;120:678–681. doi: 10.1016/s0022-5347(17)57326-7. [DOI] [PubMed] [Google Scholar]
- 2.Joshi HB, Stainthorpe A, McDonagh RP, Keeley FX, Jr, Timoney AG, Barry MJ. Indwelling ureteral stents: evaluation of symptoms, quality of life and utility. J Urol. 2003;169:1065–1069. doi: 10.1097/01.ju.0000048980.33855.90. [DOI] [PubMed] [Google Scholar]
- 3.Pollard SG, Macfarlane R. Symptoms arising from Double-J ureteral stents. J Urol. 1988;139:37–38. doi: 10.1016/s0022-5347(17)42282-8. [DOI] [PubMed] [Google Scholar]
- 4.Rane A, Saleemi A, Cahill D, Sriprasad S, Shrotri N, Tiptaft R. Have stent-related symptoms anything to do with placement technique? J Endourol. 2001;15:741–745. doi: 10.1089/08927790152596352. [DOI] [PubMed] [Google Scholar]
- 5.Erturk E, Sessions A, Joseph JV. Impact of ureteral stent diameter on symptoms and tolerability. J Endourol. 2003;17:59–62. doi: 10.1089/08927790360587342. [DOI] [PubMed] [Google Scholar]
- 6.Lennon GM, Thornhill JA, Sweeney PA, Grainger R, Mc-Dermott TE, Butler MR. 'Firm' versus 'soft' double pigtail ureteric stents: A randomised blind comparative trial. Eur Urol. 1995;28:1–5. doi: 10.1159/000475010. [DOI] [PubMed] [Google Scholar]
- 7.Liatsikos EN, Gershbaum D, Kapoor R, Fogarty J, Dinlenc CZ, Bernardo NO, et al. Comparison of symptoms related to positioning of double-pigtail stent in upper pole versus renal pelvis. J Endourol. 2001;15:299–302. doi: 10.1089/089277901750161854. [DOI] [PubMed] [Google Scholar]
- 8.Harmon WJ, Sershon PD, Blute ML, Patterson DE, Segura JW. Ureteroscopy: current practice and long-term complications. J Urol. 1997;157:28–32. doi: 10.1016/s0022-5347(01)65272-8. [DOI] [PubMed] [Google Scholar]
- 9.Netto Júnior NR, Claro Jde A, Esteves SC, Andrade EF. Ureteroscopic stone removal in the distal ureter. Why change? J Urol. 1997;157:2081–2081. doi: 10.1097/00005392-199706000-00012. [DOI] [PubMed] [Google Scholar]
- 10.Pryor JL, Langley MJ, Jenkins AD. Comparison of symptom characteristics of indwelling ureteral catheters. J Urol. 1991;145:719–722. doi: 10.1016/s0022-5347(17)38433-1. [DOI] [PubMed] [Google Scholar]
- 11.Thomas R. Indwelling ureteral stents; impact of material and shape on patient comfort. J Endourol. 1993;7:137–140. doi: 10.1089/end.1993.7.137. [DOI] [PubMed] [Google Scholar]
- 12.Stoller ML, Wolf JS, Jr, Hofmann R, Marc B. Ureteroscopy without routine balloon dilation: an outcome assessment. J Urol. 1992;147:1238–1242. doi: 10.1016/s0022-5347(17)37527-4. [DOI] [PubMed] [Google Scholar]
- 13.Bregg K, Riehle RA., Jr Morbidity associated with indwelling internal ureteral stents after shock wave lithotripsy. J Urol. 1989;141:510–512. doi: 10.1016/s0022-5347(17)40875-5. [DOI] [PubMed] [Google Scholar]
- 14.Deliveliotis C, Chrisofos M, Gougousis E, Papatsoris A, Dellis A, Varkarakis IM. Is there a role for alpha1-blockers in treating double-J stent-related symptoms? Urology. 2006;67:35–39. doi: 10.1016/j.urology.2005.07.038. [DOI] [PubMed] [Google Scholar]
- 15.Damiano R, Oliva A, Esposito C, De Sio M, Autorino R, D'Armiento M. Early and late complications of double pigtail ureteral stent. Urol Int. 2002;69:136–140. doi: 10.1159/000065563. [DOI] [PubMed] [Google Scholar]
- 16.Irani J, Siquier J, Pires C, Lefebvre O, Dore B, Aubert J. Symptom characteristics and the development of tolerance with time in patients with indwelling double-pigtail ureteric stents. BJU Int. 1999;84:276–279. doi: 10.1046/j.1464-410x.1999.00154.x. [DOI] [PubMed] [Google Scholar]
- 17.Lee JH, Park HJ, Cho JM, Han KH, Kang JY, Jeong JY, et al. Is the 3-day stenting sufficient for ureteroscopic lithotripsy? Korean J Urol. 2003;44:1011–1014. [Google Scholar]
- 18.Agarwal A, Dhiraaj S, Singhal V, Kapoor R, Tandon M. Comparison of efficacy of oxybutynin and tolterodine for prevention of catheter related bladder discomfort: a prospective, randomized, placebo-controlled, double-blind study. Br J Anaesth. 2006;96:377–380. doi: 10.1093/bja/ael003. [DOI] [PubMed] [Google Scholar]
- 19.Norris RD, Sur RL, Springhart WP, Marguet CG, Mathias BJ, Pietrow PK, et al. A prospective, randomized, double-blinded placebo-controlled comparison of extended release oxybutynin versus phenazopyridine for the management of postoperative ureteral stent discomfort. Urology. 2008;71:792–795. doi: 10.1016/j.urology.2007.11.004. [DOI] [PubMed] [Google Scholar]
- 20.Park SC, Jung SW, Lee JW, Rim JS. The effects of tolterodine extended Release and alfuzosin for the treatment of Double-J stent-related symptoms. J Endourol. 2009;23:1913–1917. doi: 10.1089/end.2009.0173. [DOI] [PubMed] [Google Scholar]
- 21.Damiano R, Autorino R, De Sio M, Giacobbe A, Palumbo IM, D'Armiento M. Effect of tamsulosin in preventing ureteral stent-related morbidity: a prospective study. J Endourol. 2008;22:651–655. doi: 10.1089/end.2007.0257. [DOI] [PubMed] [Google Scholar]