Abstract
Purpose
To evaluate the outcome and efficacy of transobturator adjustable (TOA) tape sling operations on women with intrinsic sphincter deficiency (ISD) and/or detrusor underactivity (DU) combined with stress urinary incontinence (SUI).
Materials and Methods
This retrospective analysis comprised 60 TOA patients. 30 patients hadDU (Qmax < 15ml/s) and/or ISD (Valsalva leak point pressure;VLPP < 60cmH20) on the preoperative UDS and the rest only had SUI. I-QoL, visual analog scale (VAS), Patient's Perception of Urgency Severity (PPUS), and Self-Assessment/Sandvik Questions were performed before and 1 year after surgery. The mesh tension was controlled at 1 day after surgery. The objective cure rate was defined as no leakage using the cough test with a full bladder.
Results
Patients were divided into two groups: Group A:SUI with ISD and/or DU, n=30; Group B:only SUI without ISD and DU, n=30. The two groups showed a difference in Qmax and VLPP preoperatively. Objective success rates were 18 (60.0%) completely cured, 10 (33.3%) improved in Group A, and 23 (76.7%) completely cured, 7 (23.3%) improved in Group B. Three cases needed tape-tension adjustment due to urinary leakage one-day after surgery (2 in Group A, 1 in Group B). There was no postoperative urinary retention.
Conclusions
After TOA for SUI with ISD and/or DU, 3 cases were needed tension adjustment after surgery. TOA procedures seem to be effective and safe, more clinical studies with long-term follow up are required for a definite conclusion.
Keywords: Transobturator tape, Urodynamics, Stress urinary incontinence
Introduction
Stress urinary incontinence (SUI) is the most common form of urinary incontinence in women, and about 21% of middle-aged Korean women suffer from SUI [1]. SUI consists of involuntary leakage of urine with increased intra-abdominal pressure caused by the weakness of the pelvic floor musculature, including the bladder neck and proximal urethra, or intrinsic sphincter deficiency (ISD) [2].
Recently, as quality of life has improved, interest in the treatment of SUI has increased, with more attempts at noninvasive treatment with definite effects and with low side effects and recurrence. Tension-free vaginal tape (TVT) was introduced by Ulmsten et al. [3] in 1996 and has shown good treatment results and has been performed worldwide since its presentation. Since then, Delorme et al. [4] developed trans-obturator vaginal tape (TOT) by using a tape passing the obturator foramen in 1994. TVT and TOT are the techniques most used recently.
When urinary retention occurs, however, the tape must be cut or released. On the other hand, when urinary leakage continues, the tape needs to be pulled to both sides to control the leakage after cutting or folding with ligation or suture. However, this kind of tension control is not easy and is inconvenient. Hence, methods that areable to control the tension after surgery were introduced, such as TVA, the External Mechanical Regulator (REMEEX) system, and transobturator adjustable tape (TOA) [4]. There is little domestic research on the efficacy of these methods or their treatment indications [5].
Thus, we evaluated the efficacy and stability of TOA in women with ISD or Detrusor underactivity (DU) or both combined with SUI.
Materials and methods
This retrospective study comprised 30 patients who had ISD or DU or both (Group A) and 30 patients who had SUI only (Group B) from March 2007 until March 2008 who were able to be followed up for at least 1 year. Every patient who participated in the research underwent history taking physical examination, including measurement of height and weight and a pelvic examination urinalysis urine culture three-day voiding diary questionnaires one-hour Pad test Q-tip test and urodynamic studies including uroflowmetry before surgery. For the urodynamic study, Qmax below 15 ml/s was defined as DU, and Valsalva leak point pressure (VLPP) below 60 cmH20 was defined as ISD. A questionnaire was filled out before and 1 year after surgery about Incontinence Quality of Life (I-QOL), Visual Analog Scale (VAS), Patient's Perception of Urgency Severity (PPUS), and Ssf-Assessment/Sandvik Questions and uroflowmetry and post-void residual urine were determined to assess the cure rate and the complication rate. The full bladder standing stress test by coughing was carried out to assess the objective cure rate.
All patients received preventive antibiotics by IV, by one operator, and were given Mobinul 0.2 mg and Vascam 3 mg for IV anesthetics. The operation method was no different from TOT except that the string was exposed for tension control, and the tape was positioned where there was no tension on the urethra. The tape material was monofilament polypropylene. The string exposed at the obturator foramen was used to increase the tension when urinary leakage occurred, and the tape exposed at the vagina was used todecrease the tension when urinary retention occurred. The tension was adjusted after confirming urinary retentionor urinary leakage after the Foley catheter was removed 1 day after surgery.
To evaluate the surgery success objectively, the Stamey standard [6] was used: the full bladder standing stress test with no urine leakage was defined as cure, significant reduction in urine leakage was defined as improvement, and no change in the SUI or dissatisfaction was defined as failure. The success rate included cure and improvement.
Student's t-test and the chi-square test of PC-SPSS version 12.0 were used for statistical analysis, and p values below 0.05 were considered to be statistically significant.
Results
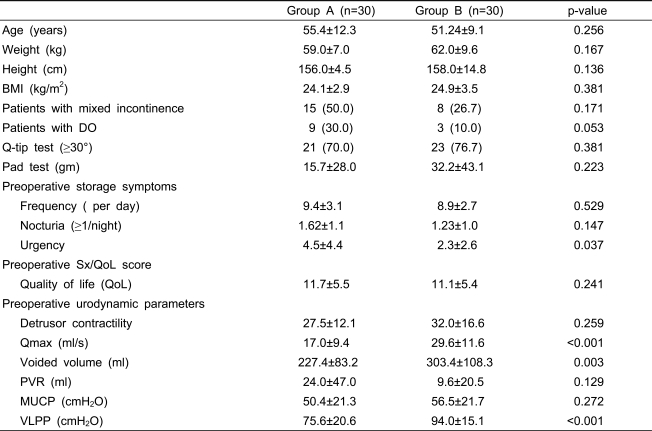
There were no significant differences in age, weight, height, BMI, Q-tip test, or pad test before surgery between the two groups, but group A complained of urgency more and the urodynamic study performed before surgery showed significant differences in VLPP (p<0.001), Q-max (p<0.001), and voided volume (p<0.001) between the two groups (Table 1).
Table 1.
Clinical characteristics of patients treated with TOAprocedure.
BMI: body mass index, DO: detrusor overactivity, Qmax: maximal flow rate, PVR: post void residual, MUCP: maximal urethral closure pressure, VLPP: Valsalva leak point pressure, Values are given as mean±SD or number (%).
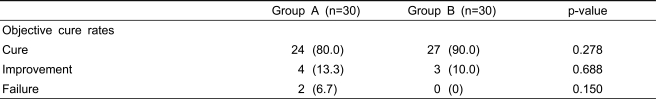
At 1 year after surgery, a total of 24 of 30 patients were cured completely and 4 were improved in group A, and 27 patients were cured and 3 were improved in group B, showing no significant difference in the success rate (Table 2).
Table 2.
Comparison of the clinical outcomes
Values are given as number (%).
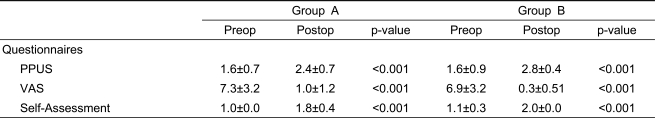
The survey of PPUS before and after surgery, the VAS of SUI, and the treatment target achievement filled out by the patients showed significant improvement in both groups (Table 3).
Table 3.
Changes in scores of several questionnaires following surgery to treat female stress urinary incontinence
PPUS: patient's perception of urgency severity, VAS: visual analog scale
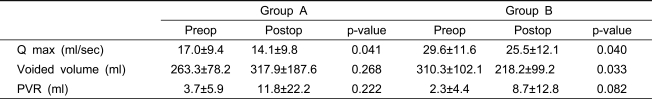
There was no difference in the post-void residual urine in the urodynamic study performed after surgery, but the Qmax decreased from 17.0±9.4l ml/s to 14.1±9.8 ml/s in group A and from 29.6±11.6 ml/s to 25.5±12.1 ml/s in group B. Two patients in group A and 1 patient in group B showed urinary leakage on the full bladder standing stress test carried out after the study, but after the tension was adjusted by the string, no urinary leakage was confirmed.
In group A, the voided volume was 26.3±78.2 before surgery and 317.9±187.9 after surgery, showing no difference (p=0.286), but in group B it was 310.3±102.1 before surgery and 218.2±99.2 after surgery, showing a significant decrease. Neither group showed urinary retention.
Discussion
Treatments such as preservative, pharmaceutical, and surgical treatements have been introduced for the purpose of treating SUI, which is the most common form of female urinary incontinence. In terms of surgical treatment, bladder neck suspension and sling operations exist, and of them, the sling operation is the most frequently used method. The TVT method presented by Ulmsten et al. [3] in 1996 is a representative sling operation, and has its basis in the Integral theory [7] that the midurethra serves a significant role in urinary continence. The TVT type surgery is simple and easy to learn and has a short surgery time and short hospitalization period. In addition, it has few side effects and thus has become a standard treatment until now. Recently, however, there have been reports of complications of bladder perforation, major bleeding, and damage of the internal organs, veins, and nerves [8]. Delome et al. [9] in 2004 reported that the TOT method, which uses an obturator foramen to pass through the tape, is more convenient and efficient than the TVT and shows similar levels of recovery and improvement while abolishing the need for a cystoscope, because it does not carry the risk of developing a bladder perforation. It also has fewer complications. Since then, De Laval et al. [10] further improved the TOT method, which still had a small possibility of damaging the urethra or bladder. They utilized both the TOT method, which inserts the tape from outside of the obturator foramen within, and the inside-out TVT obturator, which conversely passes the needle from the inside of the vagina through the thigh and into the tape. Both the TOT and the inside-out TVT obturator (TVT-O) method have now become the new way of performing the sling operation.
To date, various surgical methods that allow adjustment of the tension, which in turn corrects complications of urinary leakage or retention, have been introduced. These include the REMEEX system, the TVA (Adjustable Transvaginal Tape), and the TOA (transobturator adjustable tape) methods. These methods work more effectively in SUI patients who have ISD or DU and who therefore have a high possibility of developing urinary leakage or retention after surgery. One survey reported that of 38 patients with ISD who underwent the REMEEX surgery, all of the surgeries remained successful after 1 year [11]. According to another survey, 40.6% of patients with SUI who underwent TVA resolved their complications of urinary leakage or retention by adjustment of the tension [12]. Delome et al. reported that after conducting the TOT method, patients showed a cure rate of 90.6% and an improvement rate of 9.4% [4]. They also reported that after conducting both the TOT and the TVT-O method, the cure rate for each after 1 year was 90% and 87% [13]. In the case of our study, of the 30 patients who had ISD or DU or both, 24 of them (80.0%) were cured and 4 of them (19.1%) were improved. Of the 30 patients who did not have ISD or DU, 17 of them (90.0%) were cured and 3 (10.0%) were improved, thus showing success rates of 93.3% and 100%, respectively. However, in regard to the long-term success rate, more study and observation must be done.
One study stated that compared with the TVT method, after the TOT method, due to its larger angle and parallel direction of the tape under the urethra, the pressure around the urethra suffers less and shows less urinary retention [14]. However, out of the 183 patients who had TOT surgery done, 7 of them (3.8%) developed a urinary obstruction right after surgery [15]. In our subjects, no patients were in need of tension adjustment in the two groups who underwent TOA.
Before surgery, the two groups showed a significant difference in Qmax but not in post-void residual urine. Other research comparing the TOT and TVT-O methods in 2008 had the same result [16]. Our research showed urinary leakage in 2 patients in group A and 1 patient in group B, which was not significantly different. All patients were confirmed to have no leakage after tension adjustment.
The limitations of this study were that the follow-up period was short and the long-term success rates were not defined. The patient number was small, so there was no way to proverare side effects and there were not many other TOA studies available with which to compare our results.
Conclusions
After TOA for SUI with ISD or DU, 3 cases needed tension adjustment after surgery. TOA procedures seem to be effective and safe however, more clinical studies with long-term follow-up are required for a definite conclusion.
Table 4.
Changes in uroflowmetric parameters following surgery to treat female stress urinary incontinence.
Q max: maximal flow rate, PVR: postvoided residual urine
References
- 1.Abrams P, Andersson KE, Birder L, Brubaker L, Cardozo L, Chapple C, et al. Fourth International Consultation on Incontinence Recommendations of the International Scientific Committee: Evaluation and treatment of urinary incontinence, pelvic organ prolapse, and fecal incontinence. Neurourol Urodyn. 2010;29:213–240. doi: 10.1002/nau.20870. [DOI] [PubMed] [Google Scholar]
- 2.Nitti VW, Blaivas JG. Urinary incontinence: epidemiology, pathophysiology, evaluation, and management overview. In: Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Campbell's urology. 9th ed. Philadelphia: Saunders; 2007. pp. 2046–2078. [Google Scholar]
- 3.Ulmsten U, Henriksson L, Johnson P, Varhos G. An ambulatory surgical procedure under local anesthesia for treatment of female urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 1996;7:81–85. doi: 10.1007/BF01902378. [DOI] [PubMed] [Google Scholar]
- 4.Delorme E, Droupy S, de Tayrac R, Delmas V. Transobturator tape (Uratape): a new minimally-invasive procedure to treat female urinary incontinence. Eur Urol. 2004;45:203–207. doi: 10.1016/j.eururo.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 5.Maroto JR, Gorraiz MO, Bueno JJ, Perez LG, Bru JJ, Chaparro LP. Transobturator adjustable tape (TOA) permits to correct postoperatively the tension applied in stress incontinence surgery. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20:797–805. doi: 10.1007/s00192-009-0872-3. [DOI] [PubMed] [Google Scholar]
- 6.Stamey TA. Endoscopic suspension of the vesical neck for urinary incontinence in females. Report on 203 consecutive patients. Ann Surg. 1980;192:465–471. doi: 10.1097/00000658-198010000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Petros PE, Ulmsten UI. An integral theory and its method for the diagnosis and management of female urinary incontinence. Scand J Urol Nephrol Suppl. 1993;153:1–93. [PubMed] [Google Scholar]
- 8.Choi SK, Yun JM, Lee YS. Early clinical outcome and complications of tension freevaginal tape procedure in stress incontinent women. Korean J Urol. 2001;42:589–593. [Google Scholar]
- 9.Seok NS, Suh HJ, Lee DH. Clinical outcome of transobturator monarc procedures for treating of women with stress urinary incontinence: the 2-year follow up. Korean J Urol. 2006;47:835–840. [Google Scholar]
- 10.de Leval J. Novel surgical technique for the treatment of female stress urinary incontinence: transobturator vaginal tape inside-out. Eur Urol. 2003;44:724–730. doi: 10.1016/j.eururo.2003.09.003. [DOI] [PubMed] [Google Scholar]
- 11.Araco F, Gravante G, Dati S, Bulzomi' V, Sesti F, Piccione E. Results 1 year after the Reemex system was applied for the treatment of stress urinary incontinence caused by intrinsic sphincter deficiency. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19:783–786. doi: 10.1007/s00192-007-0523-5. [DOI] [PubMed] [Google Scholar]
- 12.Romero Maroto J, Ortiz GM, Prieto CL, Pacheco Bru, JJ, Miralles Bueno JJ, Lopez LC. Transvaginal adjustable tape: an adjustable mesh for surgical treatment of female stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19:1109–1116. doi: 10.1007/s00192-008-0590-2. [DOI] [PubMed] [Google Scholar]
- 13.Liapis A, Bakas P, Creatsas G. Monarc vs TVT-O for the treatment of primary stress incontinence: a randomized study. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19:185–190. doi: 10.1007/s00192-007-0432-7. [DOI] [PubMed] [Google Scholar]
- 14.Davila GW, Johnson JD, Serels S. Multicenter experience with the Monarc transobturator sling system to treat stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2006;17:460–465. doi: 10.1007/s00192-005-0039-9. [DOI] [PubMed] [Google Scholar]
- 15.Costa P, Grise P, Droupy S, Monneins F, Assenmacher C, Ballanger P, et al. Surgical treatment of female stress urinary incontinence with a trans-obturator-tape (T.O.T.) Uratape: short term results of a prospective multicentric study. Eur Urol. 2004;46:102–106. doi: 10.1016/j.eururo.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 16.Lee KS, Choo MS, Lee YS, Han JY, Kim JY, Jung BJ, et al. Prospective comparison of the 'inside-out' and 'outside-in' transobturator-tape procedures for the treatment of female stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19:577–582. doi: 10.1007/s00192-007-0487-5. [DOI] [PubMed] [Google Scholar]