Abstract
Objective:
Rheumatoid arthritis (RA) differs depending on the age of disease onset. The differences between EORA and YORA are important because they have clinical and therapeutic implications.
Method:
1185 patients were ranked after classification according to age at onset of the disease into YORA I (16–40 years), YORA II (41–60 years) and EORA >60 years. All patients groups were compared, based on disease duration, disease activity, severity parameters and drug history.
Results:
YORA I included 298 patients, 28.85% were males, with mean age of 29.4 ± 6 years and disease duration 4 ± 3.3 y, YORA II included 539 patients, 33.77% males, age 49.7 ± 6.1 y and disease duration 6.5 ± 5.6 y. EORA included 348 RA patients 40.5% males, age 67.1 ± 6.6 y, disease duration 9.95 ± 7.2 y. Activity was increased in EORA compared to YORA I and YORA II, while severity decreased in EORA. ESR, CRP and degree of anemia were higher in EORA. RF titer was higher in YORA. Small joints of the hands and feet were more involved in YORA, while, large joints in EORA.
Rheumatoid nodules were increased in YORA I than EORA P = 0.04. Polymyalgia rheumatica was exclusively present in EORA group 25 patients 7.2%.
Methotrexate was used in both YORA and EORA, with a higher mean of dosage in YORA than EORA. Multiple DMARDs in EORA was 57.9%, and biologics in 0.8% was which was significantly lower compared with YORA I, 86.3% and 1.7%, with P = 0.001.
Conclusion:
EORA has more active and less disabling and affects more males than YORA. The use of biologic therapy and combination DMARD therapy was less in EORA.
Keywords: EORA, YORA, Egypt. Age of onset elderly patients, young onset, DMARDs, Methotrexate, DAS 28, HAQ, rheumatoid arthritis, treatment, biological treatment, registry
Introduction
Rheumatoid arthritis (RA) is a chronic destructive inflammatory disease characterized especially by the involvement of small joints.1 RA usually develops in middle aged adults; however, it may occur at childhood or old age, too.2 RA is known to increase in incidence and prevalence up to approximately age of 85 years. The presentation, severity and prognosis of RA differ depending on the age of disease onset. The prevalence of RA in 60 years of age and older persons is reported to be around 2%.1 The issue of whether RA arising in the elderly population (EORA) is a distinct disease from younger onset RA (YORA) is not settled yet. A major concern is that arthritic disorders and functional status may diminish elderly patients’ independence. Despite several cross-sectional studies, it has not been clearly established if there are important clinical differences between elderly onset rheumatoid arthritis (EORA) and younger onset rheumatoid arthritis (YORA).3
This study was conducted to analyze and compare the demographic data, clinical profiles, disease activity and different treatment modalities in patients with elderly onset RA (EORA) and younger onset rheumatoid arthritis (YORA). We conducted this study utilizing the registry, and database generated by rheumatologist investigators of the rheumatology service at Minia University hospital (a hospital serving a whole region of Minia governorate), Egypt.
Patients and method
Data of 1185 RA patients who fulfill the ACR classification criteria of RA,4 were reviewed, in a retrospective study including clinical, functional, laboratory and radiological assessments. All RA patients were classified according to the age at onset of the RA disease into:
YORA I: with onset between 16–40 years.
YORA II: with disease onset between 41–60 years.
EORA: with disease onset >60 years.
All patients were compared, based on disease duration, disease activity and severity parameters and the proportion of patients on methotrexate, multiple disease modifying anti-rheumatic drugs (DMARDs), and biologic agents in each group. The Ritchie articular index (RAI),5 tender joint count (TJC), swollen joint count (SJC), and disease activity score (DAS 28) were used as a parameters of disease activity.6 Joint erosions were used as markers of disease severity and damage. Disability was assessed using the Stanford Health Assessment Questionnaire disability index (HAQ DI).7
Statistical analysis
Data were expressed as the mean ± SD for baseline measurement. The Data were analyzed by the Statistical Package for the Social Sciences (SPSS, version 11.0 under windows).8 One-way analysis of variance was used. A two-tailed P value less than 0.05 was considered significant.
Results
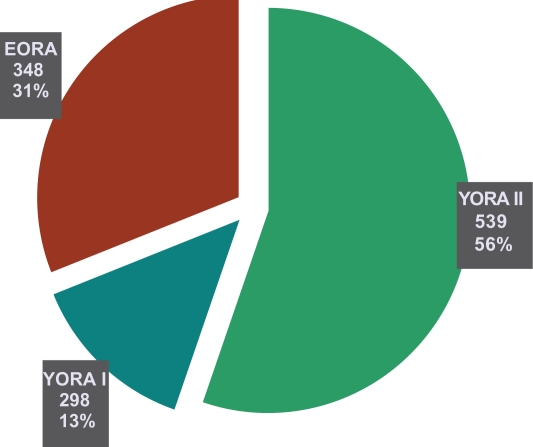
The number of RA patients in YORA I was 298, 28.85% of them were males, mean (age 29.4 ± 6 and disease duration 4 ± 3.3 years),YORA II were 539 patients with 33.77% males, mean (age 49.7 ± 6.1 y and disease duration 6.5 ± 5.6 y) and EORA were 348 patients with 40.5% males, mean (age 67.1 ± 6.6 y and disease duration 9.95 ± 7.2 y) are shown in (Table 1 and Fig. 1). Frequency and pattern of joint involvement in YORA and EORA groups are shown in Table 2 in which peripheral small joints of the hands and feet were mainly involved in YORA groups while large joints were involved in EORA group more than in YORA groups (Table 2). Extra-articular features of YORA and EORA are shown in Table 3a, where rheumatoid nodules were present in 15% of YORA I, 14% of YORA II and 6.8% of EORA with a significant increase in YORA I compared with EORA where P value = 0.04, where Polymyalgia rheumatica like symptoms (PMR) was exclusively present in EORA group 25 patients (7.2%). Comorbidities and common joint deformities in both EORA and YORA groups are shown in Table 3b.
Table 1.
Patient characteristics.
| Parameters | YORA I N = 298 | YORA II N = 539 | EORA N = 348 | Pvalue |
|---|---|---|---|---|
| Age: range | 16–40 Y | 41–60 Y | >60 Y | XX |
| M ± SD | 29.4 ± 6 | 49.7 ± 6.1 | 67.1 ± 6.6 | |
| Sex: ♂% | 86 (28.85%) | 182 (33.77%) | 141 (40.5%) | 0.02* & 0.004** |
| ♀% | 212 (71.15%) | 357 (66.23%) | 207 (59.5%) | |
| ♂/♀ | 1:2.5 | 1:2 | 1:1.5 | |
| Disease duration | 4 ± 3.3 Y | 6.5 ± 5.6 Y | 9.95 ± 3.2 Y | 0.003** & 0.01* |
Figure 1.
Number and percentage of patients in different RA groups.
Table 2.
Frequency of joint involvement in YORA and EORA.
| Parameters | YORA I (16–40) Y N = 298 | YORA II (41–60) Y N = 539 | EORA >60 Y N = 348 | Pvalue |
|---|---|---|---|---|
| PIP | 224 (75.1) | 346 (64.2) | 152 (43.7) | <0.001 & 0.02 |
| MCP | 266 (89.3) | 391 (72.6) | 189 (54.4) | <0.001 & 0.01 |
| Wrist | 223 (74.7) | 371 (68.9) | 227 (65.3) | 0.04 & NS |
| Elbow | 115 (38.5) | 168 (31.2) | 97 (27.8) | 0.005 & 0.04 |
| Shoulder | 11 (3.7) | 46 (8.6) | 65 (18.7) | <0.001 & 0.006 |
| MTP | 50 (16.7) | 51 (9.4) | 29 (8.4) | 0.022 & NS |
| Ankle | 159 (53.3) | 232 (43) | 98 (28.1) | <0.01 & 0.03 |
| Knee | 190 (63.8) | 340 (63.1) | 253 (72.6) | NS |
| Hip | 2 (0.8) | 17 (3.1) | 14 (3.9) | NS |
Table 3a.
Extra-articular features in YORA and EORA.
| Parameters | YORA I N = 298 | YORA II N = 539 | EORA > N = 348 | Pvalue |
|---|---|---|---|---|
| Loss of weight | 60 (20.0) | 149 (27.6) | 136 (39) | 0.01 & 0.04 |
| Fever | 33 (11) | 809 (15) | 59 (17) | NS |
| Myalgia | 11 (3.8) | 29 (5.4) | 37 (10.5) | 0.003 & NS |
| Fatigue | 217 (72.9) | 433 (80.4) | 295 (84.7) | NS |
| Lymphadenopathy | 17 (5.6) | 25 (4.7) | 73 (21) | 0.02 & 0.003 |
| Hepatomegaly | 19 (6.3) | 48 (8.9) | 35 (10.1) | NS |
| Splenomegaly | 15 (5) | 32 (6) | 24 (7) | NS |
| Neuropathy | 18 (5.9) | 97 (18) | 87 (25.0) | <0.001 & 0.05 |
| Rheumatoid nodules | 45 (15) | 75 (14) | 24 (6.8) | 0.04 & 0.05 |
| PMR-like symptoms | 0 | 0 | 25 (7.2) | 0.001 |
Table 3b.
Common co-morbidities and join deformities in YORA and EORA.
| Parameters | YORA I N = 298 | YORA II N = 539 | EORA > N = 348 | Pvalue |
|---|---|---|---|---|
| Sjogren’s syndrome | 27 (9.0) | 65 (12) | 15 (4.3) | <0.04 & 0.01 |
| Interstitial lung disease | 39 (13) | 43 (8) | 21 (6) | 0.01 & 0.03 |
| Malignancy | 3 (0.9) | 11 (2.1) | 13 (3.6) | 0.03 & NS |
| Swan-neck | 158 (53.2) | 127 (23.5) | 64 (18.3) | <0.001 & NS |
| Ulnar deviation | 270 (90.6) | 403 (74.8) | 191 (54.8) | <0.001 & 0.04 |
| Boutonniere | 140 (46.9) | 156 (28.9) | 62 (17.7) | <0.001 & 0.02 |
Disease activity and severity differed slightly between YORA I and YORA II, but disease activity was increased in EORA compared to both YORA I and YORA II, The mean of tender joint count (TJC) was 6.2 ± 2.8 in YORA I, 8.3 ± 4.1 in YORA II and 9.2 ± 3.9 in EORA with a significant statistical difference between YORA I and EORA where P value = 0.01. Ritchie articular index (RAI) mean was 16 ± 5 in YORA I, 20.4 ± 3.8 in YORA II and 21.8 ± 4.1 in EORA with a significant statistical difference between YORA I and EORA where P value = 0.04. Swollen joint count (SJC) was 5.7 ± 3.9 in YORA I, 6.8 ± 4.6 in YORA II and 8.1 ± 3.7 in EORA with a significant statistical difference between YORA I and EORA where P value = 0.01. DAS-28 was 3.6 ± 2.6 in YORA I, 3.9 ± 1.8 in YORA II; and 4.3 ± 2.3 in EORA with a significant statistical difference between YORA I vs. YORA II and EORA where P value was 0.03 and 0.05 respectively. Patient visual analogue scale for pain (VAS) was 26.8 ± 9.3 in YORA I, 28.12 ± 7.1 in YORA II; and 36.0 ± 13.2 in EORA with a significant statistical difference between YORA I vs. EORA where P value was 0.04. Patient Global Assessment was 15.7 ± 18.3 in YORA I, 20.9 ± 13.6 in YORA II; and 32.5 ± 14. 8 in EORA with a significant statistical difference between YORA I vs. YORA II and EORA where P value was 0.001 and 0.007 respectively. Physician Global assessment was 16.5 ± 11.2 in YORA I, 23.7 ± 9.3 in YORA II; and 29.5 ± 14.6 in EORA with a significant statistical difference between YORA I vs. YORA II and EORA where P value was 0.002 and 0.04 respectively (Table 4).
Table 4.
Disease activity characteristics in RA patients sub groups.
| Parameters | YORA I N = 298 | YORA II N = 539 | EORA N = 348 | Pvalue |
|---|---|---|---|---|
| M ± SD | M ± SD | M ± SD | ||
| Physician global assessment | 16.5 ± 11.2 | 23.7 ± 9.3 | 29.5 ± 14.6 | 0.002 & 0.04 |
| Patient global assessment | 15.7 ± 18.3 | 20.9 ± 13.6 | 32.5 ± 14.8 | 0.001 & 0.007 |
| Patient VAS (pain) | 26.8 ± 9.3 | 28.12 ± 7.1 | 36.0 ± 13.2 | 0.04 & 0.06 |
| SJC | 5.7 ± 3.9 | 6.8 ± 4.6 | 8.1 ± 3.7 | 0.07 & 0.1 |
| RAI | 16 ± 5 | 20.4 ± 3.8 | 21.8 ± 4.1 | 0.04 & 0.07 |
| TJC | 6.2 ± 2.8 | 8.3 ± 4.1 | 9.2 ± 3.9 | 0.01 & 0.06 |
| DAS 28 | 3.6 ± 2.6 | 3. 9 ± 1.8 | 4.3 ± 2.3 | 0.03 & 0.05 |
While disease severity decreased in EORA compared to Both YORA I and II for example: Joint erosions were present in 94 (39.6%) of YORA I, 193 (35.8%) in YORA II and in 118 (27.01%) of EORA patients (Table 5). HAQ disability index (HAQ DI) was 0.34 in YORA I, 0.28 in YORA II, and 0.26 in EORA, with a significant statistical difference between YORA I vs. YORA II and EORA groups where P value = 0.003 and 0.01 respectively (Table 6).
Table 5.
Disease severity characteristics in patients sub groups.
| Parameter | YORA I (16–40) Y N = 298 | YORA II (41–60) Y N = 539 | EORA >60 Y N = 348 |
|---|---|---|---|
| Number and % | Number and % | Number and % | |
| X-ray bone erosions | (118) 39.6% | 193 (35.8%) | 94 (27.01%) |
Table 6.
Disability assessment in RA patients sub groups.
|
Age at onset of RA | ||||
|---|---|---|---|---|
| Parameter | YORA I (16–40) Y N = 298 | YORA II (41–60) Y N = 539 | EORA >60 Y N = 348 | Pvalue |
| M ± SD | M ± SD | M ± SD | ||
| HAQ DI | 0.34 | 0.28 | 0.26 | 0.003 & 0.01 |
Laboratory parameters including ESR, CRP and degree of anemia were significantly increased in EORA group compared to both YORA I and II, IgM Rheumatoid factor titer was significantly increased in YORA group compared to EORA group (Table 7).
Table 7.
The laboratory features of YORA I and II and EORA patients.
| Parameters | YORA I (16–40) Y N = 298 | YORA II (41–60) Y N = 539 | EORA >60 Y N = 348 | Pvalue |
|---|---|---|---|---|
| ESR | 53.3 ± 9.5 | 73.8 ± 16.6 | 94 ± 32.3 | 0.004 & 0.02 |
| CRP | 18.5 ± 3.6 | 24.5 ± 12.7 | 48.12 ± 6.7 | 0.001 & 0.01 |
| HB | 9.6 ± 3.6 | 10.4 ± 2.9 | 11.3 ± 3.7 | 0.01 & 0.06 |
| IG M RF | 72.7 ± 8.4 | 56.9 ± 16.5 | 32.13 ± 8.5 | 0.002 & 0.03 |
| ANA | 157 ± 90.8 | 90.5 ± 60.3 | 70.6 ± 34.7 | 0.04 & 0.2 |
Regarding therapy, methotrexate use was slightly more common among YORA patients (89.3% YORA I vs. 83.6% YORA II vs. 58.4% EORA), although the mean methotrexate dose among both YORA I and II was higher than EORA. The percentage of EORA patients who were on multiple DMARD therapy (57.9%) or on biologic agents (0.8%) was significantly lower compared with YORA I patients (86.3% and 1.7%, where P value = 0.001), (Table 8). Toxicity related to therapy was very minimal in both groups, while toxicities related to methotrexate and anti malarial drugs were more common in EORA group.
Table 8.
Types-of treatment in RA sub groups.
|
Age at onset of RA | |||
|---|---|---|---|
| Parameter | YORA I (16–40) Y N = 298 | YORA II (41–60) Y N = 539 | EORA >60 Y N = 348 |
| METXOTREXATE | 266 (89.3%) | 451 (83.6%) | 203 (58.4%) |
| Mean dose in mg | 17.5 ± 7.5 | 15 ± 6.3 | 12.5 ± 7.4 |
| Multiple DMARDS | 257 (86.3%) | 427 (79.3%) | 201 (57.9%) |
| Steroids | 78 (26.2%) | 123 (22.8%) | 112 (32.2%) |
| Biologic therapy | 5 (1.7%) | 12 (2.3%) | 3 (0.8%) |
Discussion
Rheumatoid arthritis is the most prevalent inflammatory synovitis affecting 2%–2.3% of the geriatric population.9 Differential diagnostic possibilities for EORA are PMR, pseudo gout, reflex sympathetic dystrophy and osteoarthritis which must be excluded before definite diagnosis of EORA.10 Since EORA is difficult to diagnose exactly, it takes a long time to be sure of the definite diagnosis. Meanwhile, we found that the disease duration was longer in EORA than in YORA (9.95 ± 3.2 y in EORA, 4 ± 3.3 y in YORA I, and 6.5 ± 5.6 y in YORA II, P = 0.003 and 0.01.
A striking female preponderance characterizes many autoimmune diseases and estrogen activated humoral immunity. Sex steroids contribute to the expression of autoimmune diseases.11 It is well known that women are affected approximately three times as often as men, but gender differences have been diminishing in the studies of the older age group.2,12 In our study, the gender ratio in EORA was similar to that in literature male:female (♂/♀) (1/4.8) (♂/♀ in EORA was 1/1.5, YORA I 1/2.5 and in YORA II 1/2), but there was more preponderance of female involvement in YORA groups in comparison to EORA group with P value = 0.02 and 0.004. With regard to morning stiffness duration, Deal and his colleagues13 emphasized that there were no differences between EORA and YORA. However, Pease and his colleagues14 found that EORA patients had longer morning stiffness than that in YORA patients, and we found that EORA group had increase morning stiffness duration and increase in the disease activity parameters in comparison to the YORA groups.
In some papers, shoulder involvements in EORA are reported in 48%–64%; however, it was found in 18.7% in our study, which was statistically higher than that in YORA 3.7% with P = 0.001. More significant and frequent shoulder joint involvements in EORA group may testify to the concomitant degenerative-destructive changes of non-rheumatoid nature and other large joints are involved in the EORA group frequently. Although PIP, MCP (89.3% in YORA I and 54.4% in EORA with P value = 0.001), elbow, MTP and ankle joints were more commonly involved in YORA than in EORA. Classical rheumatoid hand deformities, interstitial lung disease and SS were significantly lower in EORA patients than in YORA patients, whereas EORA patients had more common constitutional features such as weight loss and Myalgia, Lymphadenopathy, rheumatoid nodules and neuropathy, this was similar to that of Turkcapar et al.15
A substantial proportion of EORA patients had a PMR like symptoms including bilateral aching and prolonged morning stiffness involving neck or torso, shoulders or arms, hips or thighs, that occur in episodic attacks at different times during the patients follow up. The occurrence of peripheral arthritis particularly in both hands may lead to some difficulties in the differential diagnosis between PMR and EORA. They had a different clinical condition from classical RA to a closely similar condition of PMR. A diagnosis of PMR or RA could therefore be made in the same patient at a different time depending on the clinical expression of the disease.16,17 Moreover, in other studies the patients were considered to have PMR, manifesting the broader clinical spectrum of this disease at the end of the period of observation. 18,19 In our study episodic attack of PMR-like symptoms, (that do not fulfill a complete picture of PMR) were found in 7.2% of EORA patients and it is similar to other studies.17,19,20 The large joint involvements especially of the shoulders are common in EORA patients. It is reported that older patients had an acute onset, in both small and large joint involvements and PMR-like symptoms more frequently.21
There are controversial results about RF seropositivity in EORA. It was found to be higher in EORA than in YORA (89% versus 78%) by Van der Heijde et al21 but we found RF seropositivities higher in YORA than in EORA, similar to that reported by other investigators.22–24 In our study, the frequencies of RF, ANA, anti-SSA/Ro and anti-SSB/La seropositivities were lower in EORA than in YORA, but anemia-associated chronic diseases, elevated ESR and CRP were more common in EORA patients and these results are similar to the literature.14,22,25
Regarding therapy; (in Table 8), methotrexate use was slightly more common among YORA patients (89.3% YORA I vs. 83.6.6% YORA II vs. 58.4% EORA), although the mean methotrexate dose among both YORA I and II was higher than EORA. The percentage of EORA patients who were on multiple DMARD therapy (57.9%) or on biologic agents (0.8%) was significantly lower compared with YORA I patients (86.3% and 1.7%, where P value = 0.001). Toxicity related to therapy was very minimal in both groups, while toxicities related to methotrexate and anti malarial drugs were more common in EORA group.
This study demonstrates that EORA group has more active and less disabling disease course and affects more males than YORA groups. Erosions were more prevalent in YORA groups than EORA and also HAQ disability index increased in YORA compared to EORA. Peripheral small joints of the hands and feet were significantly involved in YORA I and II compared to EORA, which decrease the self care activities of the YORA groups, hence increase the HAQ score, while Para axial large joints were involved more frequently in EORA than YORA. IgM Rheumatoid factor titer was increased in YORA group and associated with poor remission in EORA group. PMR-like symptoms were exclusively present in EORA not in YORA groups, However, some cases with negative rheumatoid factor and polymyalgia-like symptoms appear to be a distinct subset with a different genetic basis and a more benign course.26 Joint deformities were significantly high in YORA groups than EORA. The aging process is associated with important changes in drug pharmacokinetics and pharmacodynamics. It appears that the former, mainly through decreased renal clearance, is responsible for an increased incidence of adverse effects with some DMARDs.27 In our patients the use of biologic therapy and combination DMARD therapy were less frequently used in EORA than in YORA patients because of the presence of co-morbidities and financial aspects in this group of patients. Taking the age at onset into consideration, these differences must be kept in mind while making RA diagnosis which may be of benefit not only in providing the correct diagnosis but also of its prognostic and therapeutic implications.
Footnotes
Disclosures
This manuscript has been read and approved by all authors. This paper is unique and is not under consideration by any other publication and has not been published elsewhere. The authors and peer reviewers of this paper report no conflicts of interest. The authors confirm that they have permission to reproduce any copyrighted material.
References
- 1.Lopez-Hoyos M, Ruiz de Alegria C, Blanco R, et al. Clinical utility of anti-CCP antibodies in the differential diagnosis of elderly-onset rheumatoid arthritis and polymyalgia rheumatica. Rheumatology. 2004;43:655–7. doi: 10.1093/rheumatology/keh143. [DOI] [PubMed] [Google Scholar]
- 2.Goronzy JJ, Weyand CM.Rheumatoid arthritis. Epidemiology, Pathology and pathogenesis Klippel JH, Primer on the Rheumatic Disease. 12th edArthritis Foundation Atlanta GA 2001209–17. [Google Scholar]
- 3.Tutuncu Z, Reed G, Kremer J, Kavanaugh A.Do Patients With Older Onset Rheumatoid Arthritis Receive Less Aggressive Treatment Than Younger Patients? Ann Rheum Dis. published online 2006 Jan 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arnett FC, Edworthy SM, Bloch DA, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988;31:315–24. doi: 10.1002/art.1780310302. [DOI] [PubMed] [Google Scholar]
- 5.Jones SM, Armas JB, Cohen MG, et al. Psoriatic arthritis: Outcome of disease subsets and relationship of joint disease to nail and skin disease. Br J Rheumatol. 1994;33:834–40. doi: 10.1093/rheumatology/33.9.834. [DOI] [PubMed] [Google Scholar]
- 6.Prevoo ML, van t’Hof MA, Kuper HH, van Leeuwen MA, van de Putte LB, van Reil PL. Modified disease activity scores that include twenty-eight joint counts. Development and validation in a prospective longtidinal study of patients with rheumatoid arthritis. Arthritis Rheum. 1995;38:44–8. doi: 10.1002/art.1780380107. [DOI] [PubMed] [Google Scholar]
- 7.Fries JF, Spitz P, Krainer RG, et al. Measurement of patients outcome in arthritis. Arthritis Rheum. 1980;23:137–45. doi: 10.1002/art.1780230202. [DOI] [PubMed] [Google Scholar]
- 8.SPSS Inc (2001): Statistical Package for Social Sciences Incorporation for windows, version 11.
- 9.Rasch EK, Hirsch R, Paulose-Ram R, Hochberg MC. Prevalence of rheumatoid arthritis in persons 60 years of age and older in the United States: effect of different methods of case classification. Arthritis Rheum. 2003;48:917–26. doi: 10.1002/art.10897. [DOI] [PubMed] [Google Scholar]
- 10.Kerr LD. Inflammatory arthropathy. A review of rheumatoid arthritis in older patients. Geriatrics. 2004;59:32–5. [PubMed] [Google Scholar]
- 11.Masi AT, Crofford LJ.Immunity. Neuroendocrine influences Klippel JH, Primer on the Rheumatic Disease. 12th edArthritis Foundation, Atlanta, GA 2001100–3. [Google Scholar]
- 12.Yazici Y, Paget SA. Elderly onset rheumatoid arthritis. Rheum Dis North Am. 2000;26:518–9. doi: 10.1016/s0889-857x(05)70154-x. [DOI] [PubMed] [Google Scholar]
- 13.Deal CL, Meenan RF, Goldenbert DL, et al. The clinical features of elderly onset rheumatoid arthritis. A comparison with younger onset disease of similar duration. Arthritis Rheum. 1985;28:987–94. doi: 10.1002/art.1780280905. [DOI] [PubMed] [Google Scholar]
- 14.Pease CT, Bhakta BB, Devlin J, Emery P. Does the age of onset of rheumatoid arthritis influence phenotype? A prospective study of outcome and prognostic factors. Rheumatology. 1999;38:228–34. doi: 10.1093/rheumatology/38.3.228. [DOI] [PubMed] [Google Scholar]
- 15.Turkcapar N, Demir O, Atli T.Late onset rheumatoid arthritis: Clinical and laboratory comparisons with younger onset patients Archives of Gerontology and Geriatrics 2006;42 230225–31. [DOI] [PubMed] [Google Scholar]
- 16.Healey LA, Sheets PK. The relation of Polymyalgia rheumatica to rheumatoid arthritis. J Rheumatol. 1988;15:750–2. [PubMed] [Google Scholar]
- 17.Healey LA. Polymyalgia rheumatica and seronegative rheumatoid arthritis may be the same entity. J Rheumatol. 1992;19:270–2. [PubMed] [Google Scholar]
- 18.Salvarani C, Hunder GG. Musculoskeletal manifestations in a population-based cohort of patients with giant cell arteritis. Arthritis Rheum. 1999;42:1259–266. doi: 10.1002/1529-0131(199906)42:6<1259::AID-ANR24>3.0.CO;2-I. [DOI] [PubMed] [Google Scholar]
- 19.Salvarani C, Cantini F, Boiardi L, Hunder GG. Polymyalgia rheumatica. Best Pract. Res. Clin Rheumatol. 2004;18:705–22. doi: 10.1016/j.berh.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 20.Gonzalez-Gay MA, Hajeer AH, Dababneh A, et al. Seronegative rheumatoid arthritis in elderly and polymyalgia rheumatica have similar patterns of HLA association. J Rheumatol. 2001;28:122–5. [PubMed] [Google Scholar]
- 21.Van der Heijde DMFM, Van Riel PLCM, Van Leeuwen MA, Van’t Hof MA, Van Rijswijk MH, Van de Putte LBA. Older versus younger onset rheumatoid arthritis: results at onset and after 2 years of prospective follow-up study of early rheumatoid arthritis. J Rheumatol. 1991;181:1285–289. [PubMed] [Google Scholar]
- 22.Ehrlich GE, Katz WA, Cohen SA. Rheumatoid arthritis in the aged. Geriatrics. 1970;25:103–13. [PubMed] [Google Scholar]
- 23.Ferraccioli GF, Cavalieri F, Mercandati M, Conti G, Viviano P, Ambanelli U. Clinical features, scintiscan characteristics and X-ray progression of late onset rheumatoid arthritis. Clin Exp Rheumatol. 1984;2:157–61. [PubMed] [Google Scholar]
- 24.Inoue K, Shichikawa K, Nishioka J, Hirota S. Older age onset rheumatoid arthritis. Ann Rheum Dis. 1987;46:908–11. doi: 10.1136/ard.46.12.908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tishler M, Yaron I, Shirazi I, Yaron M. Clinical and immunological characteristics of elderly onset Sjogren’s syndrome: a comparison with younger onset disease. J Rheumatol. 2001;28:795–97. [PubMed] [Google Scholar]
- 26.Villa-Blanco JI, Calvo-Alen J. Elderly onset rheumatoid arthritis: differential diagnosis and choice of first-line and subsequent therapy. Drugs Aging. 2009;26(9):739–50. doi: 10.2165/11316740-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 27.Diaz-Borjon A. Guidelines for the use of conventional and newer disease-modifying antirheumatic drugs in elderly patients with rheumatoid arthritis. Drugs Aging. 2009;26(4):273–93. doi: 10.2165/00002512-200926040-00001. [DOI] [PubMed] [Google Scholar]