Abstract
The heart and the kidneys share responsibility for maintaining hemodynamic stability and end-organ perfusion. Connections between these organs ensure that subtle physiologic changes in one system are tempered by compensation in the other through a variety of pathways and mediators. In the setting of underlying heart disease or chronic kidney disease, the capacity of each organ to respond to perturbation caused by the other may become compromised. This has recently led to the characterization of the cardiorenal syndrome (CRS). This review will primarily focus on CRS type 1 where acute decompensated heart failure (ADHF) results in activation of hemodynamic and neurohormonal factors leading to an acute drop in the glomerular filtration rate and the development of acute kidney injury. We will examine the scope and impact of this problem, the pathophysiology associated with this relationship, including underperfuson and venous congestion, diagnostic tools for earlier detection, and therapeutic interventions to prevent and treat this complication.
1. Introduction
The heart and the kidneys share responsibility for maintaining hemodynamic stability and end-organ perfusion through a tight-knit relationship that controls cardiac output, volume status, and vascular tone. Connections between these organs ensure that subtle physiologic changes in one system are tempered by compensation in the other. As such, hemodynamic control remains stable through a wide range of physiologic conditions.
Communication between the heart and kidneys occurs through a variety of pathways. These include perfusion pressure, filling pressure, and neurohormonal activity. In particular, some of the key mediators include the sympathetic nervous system, the renin-angiotensin-aldosterone axis, and atrial natriuretic peptide. These agents have receptors in the heart, the kidneys, and the vasculature that affect volume status, vascular tone, cardiac output, and inotropy. A change in the performance of one of these organs elicits a cascade of mediators that affects the other.
In the setting of underlying heart disease or chronic kidney disease, the capacity of each organ to respond to perturbation caused by the other may become compromised. Acute or chronic heart failure may push the kidneys beyond their ability to maintain glomerular filtration, regulate fluid and electrolytes, and clear metabolic waste. Similarly, acute kidney injury or chronic kidney disease affects cardiac performance through electrolyte dysequilibration, volume overload, and negative inotropy. Clinical, cardiac, and renal parameters associated with dysfunction in the other organ are identified in Table 1.
Table 1.
Risk factors for the cardiorenal syndrome [1].
| Clinical |
| (i) Older age |
| (ii) Comorbid conditions (diabetes mellitus, uncontrolled hypertension, and anemia |
| (iii) Drugs |
| (a) Antiinflammatory agents |
| (b) Diuretics (thiazides, loop diuretics) |
| (c) Angiotensin converting enzyme inhibitors/angiotensin receptor blockers |
| (d) Aldosterone receptor antagonists |
| Heart |
| (i) History of heart failure or impaired left ventricular ejection fraction |
| (ii) Prior myocardial infection |
| (iii) New York Hear Association functional class |
| (iv) Elevated cardiac troponin |
| Kidney |
| (i) Chronic kidney disease (reduced eGFR, elevated BUN, creatinine, or cystatin) |
This special relationship and the interdependence of the kidneys and the heart is well recognized. The manner in which dysfunction of one organ affects the other has recently led to the characterization of the cardiorenal syndrome (CRS). At a consensus conference of the Acute Dialysis Quality Initiative (ADQI), the cardiorenal syndrome was subclassified into 5 types [2] based upon the organ that initiated the insult as well as the acuity or chronicity of the precipitating event. The classification system for the CRS is outlined in Table 2.
Table 2.
ADQI classification system of the cardiorenal syndrome [2].
| Inciting event | Secondary disturbance | |
|---|---|---|
| CRS type 1 | Acute decompensated heart failure | Acute kidney injury |
| CRS type 2 | Chronic heart failure | Chronic kidney disease |
| CRS type 3 | Acute kidney injury | Acute heart failure |
| CRS type 4 | Chronic kidney disease | Chronic heart failure |
| CRS type 5 | Codevelopment of heart failure and chronic kidney disease | |
This review will primarily focus on CRS type 1, where acute cardiac decompensation results in activation of hemodynamic and neurohormonal factors that lead to an acute drop in GFR and the development of AKI. We will examine the scope and impact of this problem, the pathophysiology associated with this relationship, diagnostic clues for earlier detection, and therapeutic interventions to prevent and treat this complication.
2. Epidemiology
Heart failure is a common chronic condition affecting 2% of the adult population [3] and resulting in over 1 million annual admissions [4], making it the leading cause of hospitalization in the United States among adults over the age of 65. Health expenditures for heart failure in 2008 exceeded $35 billion dollars [5]. Acute kidney injury may complicate one-third of these admissions, resulting in a three fold increase in length of stay, a greater likelihood for hospital readmission, and a 22% higher mortality rate [6–9]. This reduction in outcomes occurs with increases in serum creatinine of as little as 0.33 mg/dl, regardless of its presence at admission or its development during the course of heart failure treatment [10, 11].
In addition, approximately 25% of patients with chronic heart failure have been found to have reduced GFR [12], independent of their level of left ventricular function [13]. A prospective cohort of 754 patients with chronic heart failure found only 17% of patients had an eGFR > 90 ml/min [14]. In the large Acute Decompensated Heart Failure National Registry (ADHERE), reduced GFR affected 30% of the 107,362 individuals [15]. Furthermore, 21% of patients had serum creatinine concentrations > 2 mg/dl, and 9% had serum creatinine concentrations > 3 mg/dl [16]. This reduction in kidney function has significant impact on both morbidity and mortality [17, 18]. In a meta-analysis of 80,098 hospitalized and nonhospitalized patients, an eGFR < 53 ml/min was associated with a 51% 1-year mortality compared to a 38% 1-year mortality for an eGFR < 90 ml/min. Preserved kidney function with an eGFR > 90 ml/min was associated with a 24% 1-year mortality [19].
3. Physiology of the Cardiorenal Axis
The heart, by way of regulating the systemic circulation, and the kidneys, through their effect on extracellular fluid volume, share responsibility for the hemodynamic balance in the body. The kidneys produce a glomerular filtrate that is dependent upon perfusion pressure and afferent and efferent arteriolar tone. The arteriolar resistance is under intrinsic myogenic control, and responsive to several neurohormonal systems. The renin-angiotensin-aldosterone system (RAAS), the sympathetic nervous system (SNS), and local vasodilators such as nitric oxide (NO), adenosine, and prostaglandins contribute to maintaining the glomerular filtration rate (GFR) through conditions of increased or decreased perfusion pressure. When renal perfusion pressure decreases, angiotensin II (AII) preferentially increases the efferent arteriolar resistance to preserve intraglomerular hydrostatic pressure and maintain GFR. Simultaneously, the afferent arteriole, under control of tubuloglomerular feedback and prostaglandins, dilates to increase the transmission of perfusion pressure into the glomerulus. An elegant system senses decreased glomerular perfusion from hypovolemia or decreased cardiac output at the macula densa and the juxtaglomerular apparatus, then activates the RAAS, nitric oxide, adenosine, and prostaglandin production to prevent dramatic changes in kidney function.
We will now explore some of the mechanisms that effect kidney function during decompensated heart failure.
3.1. Underperfusion
Acute decompensated heart failure (ADHF) results in reduced effective arterial filling volume (EAFV) [20]. This decreased EAFV diminishes renal blood flow and subsequently renal perfusion pressure. Decreased tubular sodium and chloride delivery is sensed by the macula densa and the juxtaglomerular apparatus, activating the RAAS. RAAS enhances sodium and water retention to increase EAFV and stroke volume, but comes at the detrimental cost of volume overload. Furthermore, norepinephrine is released in response to systemic hypoperfusion sensed by baroreceptors. Whereas angiotensin causes efferent arteriole constriction, norepinephrine induces both afferent and efferent arteriole constriction and increases renal vascular resistance. In a setting of low cardiac output, both angiotensin and norepinephrine cause decreased renal blood flow (RBF), diverting blood to the coronary and cerebral circulations. When the normal compensatory mechanisms such as NO, bradykinin, adenosine, and prostaglandins are unable to maintain GFR in the setting of decreased RBF, the groundwork for renal ischemia is laid. It appears, therefore, that the cardiovascular effects on hemodynamics and the renal effects on extracellular fluid volume are in constant flux.
An imbalance in this relationship results in the CRS. In the setting of heart failure where low cardiac output and an overactive neurohormonal system push the compensatory limits, a simple insult such as NSAIDS or aggressive diuresis can precipitate acute kidney injury [21]. NSAIDs inhibit the protective effect of prostaglandins to dilate the afferent arteriole, while over diuresis might lead to further decreased EAFV. Diuretics are effective when properly dosed to allow reequilibration of fluid from the interstitial compartment into the intravascular compartment. If the rate of diuresis exceeds this shift, then kidney dysfunction occurs. Other observations have suggested that RBF is the most important determinant of GFR in patients with CHF [22].
3.2. Venous Congestion
While it is true that decreased forward flow as a result of decreased cardiac output in ADHF can cause acute deterioration in kidney function, there are several reasons why this mechanism fails to completely explain the development of the CRS. First, altered hemodynamics alone are inadequate to explain the mechanism of kidney injury in ADHF as redundant feedback mechanisms exist to prevent it. Second, the CRS has been observed in patients with diastolic dysfunction who have normal left ventricular systolic function [14]. In the ADHERE registry, acute kidney injury occurred at similar rates in patients with both systolic and diastolic dysfunction [23]. And finally, subgroup analysis of the ESCAPE trial showed evidence that poor forward flow alone was insufficient to explain worsening kidney function. In this trial, an improved cardiac index was not associated with improved renal outcomes, but increased CVP and atrial pressures were associated with decreased kidney function [24].
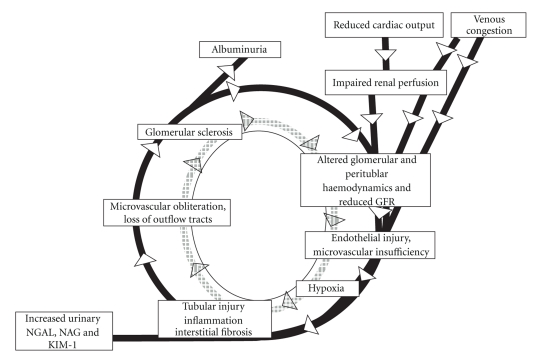
Observations dating back to the 1930s have suggested that renal venous congestion could also contribute to decreased glomerular filtration. Experiments conducted on canine models revealed that increased venous pressure in the kidneys caused changes in urinary sodium, chloride, and urea excretion similar to decreased arterial pressure. Urine flow decreased when renal venous pressures were increased to 20 mmHg. This also led to a drop in glomerular perfusion pressure, and a reduction in GFR [25]. It is hypothesized that increased venous pressure distends the venules surrounding the distal nephron. This leads to compression of the tubule, increased tubular fluid pressure, and backleak of filtrate into the interstitium. An increased interstitial pressure then results in venous congestion and interstitial hypoxia [26]. Furthermore, as hydrostatic pressure within the Bowman's capsule increases, GFR fails and the RAAS is activated and the SNS is triggered [27]. The sequence of events is shown in Figure 1.
Figure 1.
Pathophysiology of the relation between venous congestion and reduced glomerular filtration rate (GFR). Reprinted with modification from Damman et al. [28].
Studies in human subjects have also demonstrated that increased central venous and right atrial pressure are associated with worsening kidney function as well as increased mortality [29, 30]. Damman and colleagues have demonstrated that increased venous pressure is an independent determinant of glomerular filtration in patients with heart failure [28]. In this study the lowest glomerular filtration rate was observed in patients with lowest renal blood flow and highest right atrial pressures.
3.3. Intra-Abdominal Hypertension
Intraabdominal hypertension might be yet another mechanism contributing to the CRS. Elevated intraabdominal pressure from ascites and abdominal wall edema is also prevalent in patients with ADHF, and associated with worsening kidney function [31]. Several studies have suggested that the deterioration in the kidney function is not due to direct parenchymal pressure on the kidneys, but rather due to elevated central venous pressure, arterial underfilling, and renal venous congestion [32, 33]. The decline in kidney function from increased intraabdominal pressure is mechanistically related to the venous congestion described above.
4. Mediators of the Cardiorenal Syndrome
There are a variety of neurohormonal mediators associated with the deterioration of kidney function in ADHF. Understanding these-mediators and effectors yields insight into the diagnosis and therapy of CRS.
4.1. Renin-Angiotensin-Aldosterone System
The CRS occurs with both hypoperfusion associated with decreased cardiac output as well as venous congestion. The actions of the RAAS, beyond its role to maintain hemodynamics, may explain this cardiorenal connection.
Activation of RAAS by hypoperfusion activates the sympathetic nervous system (SNS) [34], and mediates the release of reactive oxygen species (ROS) and mediators of vascular inflammation [35]. Angiotensin II activates both NADH-oxidase and NADPH-oxidase [36], which then generates reactive oxygen species. Studies have demonstrated this activity in vascular smooth muscle cells, cardiac myocytes, and both renal tubular cells [37] and glomeruli in the kidneys. ROS, specifically superoxides, have been implicated in organ injury and inflammation. The ensuing oxidative stress results in a proinflammatory state activating chemokines such as IL-1, IL-6, and TNF alpha, and attracting leucocytes. Furthermore, studies have shown that the effect of NADPH-oxidase mediated ROS release can be attenuated by angiotensin converting enzyme (ACE) inhibition.
Angiotensin II also has a role in chemokine regulation and monocyte recruitment. Angiotensin II increases Monocyte Chemoattractant Protein-1 (MCP-1) in mesangial and mononuclear cells by a mechanism dependent on nuclear factor-κB (NF-κB) activation [38]. These monocytes and chemokines play a major role in the propagation of kidney injury [39]. Angiotensin II also activates the sympathetic nervous system through its effect on the vasomotor center in the brain. This was established by showing increased muscle sympathetic nerve activity (MSNA) in patients with kidney failure [40]. Studies using ACE inhibitors and angiotensin receptor blockers (ARB) have shown decreased MSNA and decreased sympathetic activity [41, 42]. Thus AII seems to play a direct role in renal injury [43] and direct damage to the glomerular filtration barrier [44, 45].
4.2. Nitric oxide and Reactive Oxygen Species Disequilibrium
Nitric oxide, an endothelium-derived relaxing factor, is a vasodilator that acts to regulate vascular tone, blood pressure, and smooth muscle hypertrophy through downregulation of ACE and the AII type 1 receptor. NO therefore represents a physiologic antagonist of AII at both the glomerular and tubular levels [46, 47]. It also plays a role in tubuloglomerular feedback through dilation of the afferent arteriole [48]. In decompensated heart failure, RAAS activation causes angiotensin mediated hypertension through increased systemic vascular resistance, greater renal perfusion pressure through preferential efferent arteriolar vasoconstriction, and renal oxidative stress through enhanced NADPH-oxidase activity in rats [49]. Reduced activity of superoxide dismutase (SOD) is thought to be involved in increased ROS generation. Subsequently, there is a shift in the NO/ROS system to the ROS side. Several factors contribute to this shift. In heart failure, asymmetric dimethyl arginine (ADMA) levels are increased. ADMA is a novel cardiovascular risk factor that decreases NO levels [50]. Even mild heart failure is associated with decreased renal perfusion by way of NO inhibition. Also, Endothelin I (ET 1) is implicated in vasoconstriction, causing mesangial cell contraction and mesangial cell mitogenesis [51]. Whereas AII stimulates the release of ET 1, NO inhibits ET 1 release from endothelial cells. An imbalance in favor of more ET 1 production causes endothelial dysfunction as well as glomerular and interstitial damage [52].
4.3. Other Mediators
Atrial natriuretic peptide (ANP) and brain natriuretic peptide (BNP) are released in response to stretch of the cardiac chambers, and play a role in regulation of ECFV by inducing sodium and water loss. They are elevated in both heart failure and reduced kidney function. Although they are an ideal therapeutic target, their role in the pathophysiology of CRS is not known.
Erythropoietin is purported to decrease apoptosis in renal cells and cardiac myocytes by decreasing oxidative stress [53]. Small trials have revealed that heart failure patients who received erythropoietin had improved kidney function [54], but their place in the treatment of CRS cannot be confirmed without long-term studies.
Antidiuretic hormone (ADH) levels are elevated in HF due to nonosmotic stimuli from baroreceptor stimulation [55]. Antagonism of ADH would seem to have a role in the CRS, but studies of vasopressin receptor 2 antagonists did not result in improvement in kidney function [56].
There is direct evidence to demonstrate that HF is associated with tubulointerstitial damage. A recent study by Damman and colleagues showed that congestive heart failure is associated with increased markers of tubulointerstitial damage such as N-acetyl-beta-D-glucosaminidase (NAG), kidney injury molecule 1 (KIM-1), and neutrophil gelatinase associated lipocalin (NGAL) [57]. Other studies have also demonstrated renal tubular and interstitial damage as well [58].
In summary, it appears that regardless of whether decreased perfusion occurs as a result of hypoperfusion or venous congestion, the consequent processes resulting in kidney injury are the same. RAAS activation results in increased AII which stimulates NADH and NADPH-oxidases. The resulting NADPH/NADH suppresses super-oxide dismutase, and increases reactive oxygen species. This results in the well known cascade of hypoxic ischemic injury, inflammation, apoptosis and cell death as shown in Figure 2.
Figure 2.
Hypothetical vicious circle of decreased glomerular function, endothelial injury, and tubular damage in heart failure. GFR: glomerular filtration rate. NGAL: neutrophil gelatinase associated lipocalin. NAG: N-acetyl-beta-D-glucosaminidase. KIM-1: kidney injury molecule 1. Adapted and reprinted with permission from Norman and Fine [59] and Damman et al. [60].
5. Diagnosis
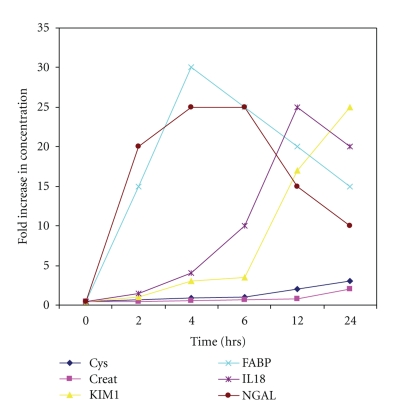
One of the cornerstones of CRS therapy is the early identification of worsening kidney function. This can be accomplished with the use of biomarkers that become detectable before the traditional tests for kidney function, including glomerular filtration rate or serum creatinine (Figure 3). Biomarkers such as NGAL, NAG, and KIM-1 have been implicated in tubulointerstitial damage and have been used to identify acute kidney injury [61–63]. Serum cystatin C is elevated earlier than creatinine. Furthermore, while cystatin C in the serum is a marker of reduced glomerular filtration, urinary cystatin C is a marker of tubular dysfunction [64]. Other biomarkers that have proven useful include BNP, IL-18, and Fatty Acid Binding Protein (FABP). Thus detection of these biomarkers might be used to diagnose CRS at an earlier time point, facilitate targeted therapy for CRS by modifying pharmacologic therapy, and monitor progression of disease. Nevertheless, a higher index of suspicion for identifying patients at CRS is needed as testing for biomarkers at this time is expensive.
Figure 3.
Urinary biomarker profiles in subjects who develop AKI after cardiopulmonary bypass (CPB) surgery. Abbreviations: AKI: acute kidney injury, defined as a 50% increase in serum creatinine from baseline; NGAL: neutrophil gelatinase associated lipocalin; IL-18: interleukin 18; KIM-1: kidney injury molecule 1; L-FABP: liver-type fatty acid binding protein; Cys: cystatin c; creat: creatinine. Adapted and modified with permission from Devarajan [65].
Tests for volume status and end-organ perfusion are also useful in the diagnosis of CRS. Bioimpedence vector analysis is effective at assessing hydration status and BNP measurement provides an assessment of cardiac filling, although it is often elevated in patients with AKI without overt fluid overload. Urine sediment examination should be performed in differentiating CRS from other causes of AKI by excluding pathologic cells, casts, or crystals. Hyponatremia, when present, may indicate excess ADH and portend an overall poor prognosis. Although patients with ADHF have a poor prognosis to begin with, ensuing AKI that accompanies the CRS confers an even more dire condition.
6. Therapies for the Cardiorenal Syndrome
In patients with ADHF who present with worsening kidney function, management is challenging and effective therapies are lacking [66]. This is in large part due to the exclusion of patients with kidney dysfunction in many of the trials analyzing treatment for heart failure. A rational approach would be multi-modal, focusing on the underlying pathophysiology of CRS with the goal of disrupting the cardiorenal connections. Ideally, therapy for CRS would prevent the fulminant decompensation that jeopardizes kidney function. This requires use of biomarkers in appropriate settings to detect early changes in kidney function, and represents an opportunity for initiation of immediate treatment.
6.1. Diuretics
Although diuretics have a major role in the symptomatic treatment of heart failure, their effectiveness is limited due to diuretic resistance in CRS. Although renal hypoperfusion may require a reduction in the dose of diuretics, venous congestion may necessitate additional diuresis. Thus, delicate fluid management may involve monitoring urine flow, central venous pressures, and possible cardiac output to optimize renal physiology. Nevertheless, CVP monitoring is cumbersome and costly. A forthcoming trial, “Determining Optimal Dose and Duration of Diuretic Treatment in People With Acute Heart Failure (DOSE-AHF) study,” is designed to answer these questions with regard to the role of diuretics in CRS [67].
6.2. Natriuretic Peptides
Several studies have explored the pharmacologic properties of natriuretic peptides in the treatment of heart failure. Nesiritide, a recombinant natriuretic peptide, decreases preload, after load, and pulmonary vascular resistance, while inducing diuresis. Because of its natriuretic and aquaretic properties, these agents seem to be an ideal candidate to relieve the venous congestion in CRS. Nevertheless, no studies have shown benefit on kidney function. In fact, a meta-analysis demonstrated poorer renal outcomes with nesiritide [68]. In one study, nesiritide when compared to placebo had no effect on glomerular filtration rate, renal plasma flow, urine output, and sodium excretion in patients with CRS [69]. To address these controversies, the “Acute Study of Clinical Effectiveness of Nesiritide in Decompensated Heart Failure Trial (ASCEND)” is underway [70].
6.3. Vasopressin Antagonists
By making use of their aquaretic properties, vasopressin (V2 receptor) antagonists have been used in severe heart failure. However, clinical trials such as the “Efficacy of Vasopressin Antagonism in Heart Failure Outcome Study With Tolvaptan (EVEREST)” trial showed no benefit of tolvaptan, a vasopressin antagonist, on all-cause mortality or the combined end point of cardiovascular mortality or hospitalization for ADHF [56]. Kidney function remained stable throughout this trial, and the use of vasopressin antagonists in the CRS conundrum may be limited to those patients complicated by hyponatremia. Although other studies showed there was some renal benefit [71], the cost of these medications would prohibit them from being used routinely.
6.4. Adenosine Antagonist
Adenosine is generated locally in the macula densa in response to diuretics that block sodium and chloride absorption, resulting in afferent arteriolar constriction and decreased GFR. Antagonizing adenosine might have a role in preserving kidney function in CRS. To this extent, KW-3902, an adenosine A1-receptor antagonist, was found to improve kidney function and decrease diuretic resistance in patients with ADHF and CRS [72].
6.5. Ultrafiltration
Ultrafiltration is usually reserved for diuretic resistance in patients with ADHF. However, in CRS it might have an early role by rapidly reducing venous pressure. In two trials of ultrafiltration in patients with ADHF, the “Relief for Acutely Fluid-Overloaded Patients With Decompensated Congestive Heart Failure (RAPIDCHF)” and “Ultrafiltration Versus Intravenous Diuretics for Patients Hospitalized for Acute Decompensated Congestive Heart Failure (UNLOAD),” there was marked weight loss and relief of heart failure symptoms [73, 74], but no improvement of kidney function. Nevertheless, published case reports have shown improved kidney function with ultrafiltration [75]. A final verdict might come with the much awaited “Cardiorenal Rescue Study in Acute Decompensated Heart Failure (CARRESS-HF)” study which will assess the effectiveness of ultrafiltration in ADHF and CRS [76].
6.6. Inotropes
Although the use of inotropes in systolic heart failure may improve the EAFV and cardiac output, the inherent adverse effects of these agents, including arrhythmias and myocardial ischemia, have limited their utility. In fact, the “Outcomes of a Prospective Trial of Intravenous Milrinone for Exacerbations of Chronic Heart Failure (OPTIME-CHF)” trial revealed increased mortality and poorer outcomes in the milrinone arm [77].
Levosimendan, a phosphodiesterase inhibitor, has been studied in CRS. In one study, levosimendan resulted in improved GFR when compared to dobutamine [78]. However, another study of levosimendan and dobutamine did not show any benefit [79]. At this time, the role of inotropic agents in CRS remains unknown.
6.7. Neurohormonal Blockade
The role of RAAS blockade with ACE inhibitors, ARB, direct renin inhibitors, or aldosterone antagonists in CRS is also unclear. While most of these medications cause an acute drop in GFR through the dilatory effect on the efferent arteriole, they have long-term reno- and cardioprotective effects. Therefore, patients who are prone to develop CRS yet able to tolerate a small reduction in GFR, up to 30% from the baseline, may benefit from these agents. As RAAS has been implicated in oxidative damage, its interruption though ACE inhibition or angiotensin blockade may prevent the development of CRS.
Similar to RAAS blockade, beta blockers through their effect on the SNS may have a role in the long-term prevention of adverse cardiac events and in remodeling. However in CRS, their role is limited by the altered hemodynamics. Unless the underlying etiology of ADHF is myocardial infarction, beta blockers are often held until the patients are hemodynamically stable.
7. Summary
Cardiorenal syndrome represents a disruption of the robust relationship between the kidneys and the heart to preserve hemodynamics and maintain organ function. Despite the ability to adjust filling pressures, afterload, inotropy, cardiac output, and volume status in order to compensate for a wide range of perturbations, dysfunction in either of these organs creates a susceptibility to dysfunction in the other. The mechanisms for worsening kidney function in ADHF are likely due to underperfusion from reduced cardiac output, venous congestion impairing tubular function and glomerular filtration, and activation of neurohormonal mediators that effect renal blood flow and glomerular autoregulation. The RAAS, SNS, and NO pathways are instrumental in preserving kidney function in compensated HF, but play an aggravating role once HF acutely worsens.
Measures to reverse kidney dysfunction in ADHF require the early recognition and immediate treatment of CRS. Agents that target the physiologic mechanisms of CRS may be effective in restoring kidney function. These include diuretics, natriuretic peptides, or ultrafiltration to reduce venous congestion, inotropes to augment cardiac output, and RAAS and SNS blockade. Despite these interventions, CRS identifies patients at the limits of hemodynamic compensation and most susceptible to increased morbidity and mortality.
References
- 1.Tang WHW, Mullens W. Cardiorenal syndrome in decompensated heart failure. Heart. 2010;96(4):255–260. doi: 10.1136/hrt.2009.166256. [DOI] [PubMed] [Google Scholar]
- 2.Ronco C, McCullough P, Anker SD, et al. Cardio-renal syndromes: Report from the consensus conference of the acute dialysis quality initiative. European Heart Journal. 2010;31(6):703–711. doi: 10.1093/eurheartj/ehp507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McMurray JJV, Pfeffer MA. Heart failure. Lancet. 2005;365(9474):1877–1889. doi: 10.1016/S0140-6736(05)66621-4. [DOI] [PubMed] [Google Scholar]
- 4.Haldeman GA, Croft JB, Giles WH, Rashidee A. Hospitalization of patients with heart failure: national hospital discharge survey, 1985 to 1995. American Heart Journal. 1999;137(2):352–360. doi: 10.1053/hj.1999.v137.95495. [DOI] [PubMed] [Google Scholar]
- 5.Rosamond W, Flegal K, Furie K, et al. Heart disease and stroke statistics—2008 update: a report from the American heart association statistics committee and stroke statistics subcommittee. Circulation. 2008;117(4):e25–e146. doi: 10.1161/CIRCULATIONAHA.107.187998. [DOI] [PubMed] [Google Scholar]
- 6.Forman DE, Butler J, Wang Y, et al. Incidence, predictors at admission, and impact of worsening renal function among patients hospitalized with heart failure. Journal of the American College of Cardiology. 2004;43(1):61–67. doi: 10.1016/j.jacc.2003.07.031. [DOI] [PubMed] [Google Scholar]
- 7.Wencker D. Acute cardio-renal syndrome: progression from congestive heart failure to congestive kidney failure. Current Heart Failure Reports. 2007;4(3):134–138. doi: 10.1007/s11897-007-0031-4. [DOI] [PubMed] [Google Scholar]
- 8.Hillege HL, Girbes ARJ, De Kam PJ, et al. Renal function, neurohormonal activation, and survival in patients with chronic heart failure. Circulation. 2000;102(2):203–210. doi: 10.1161/01.cir.102.2.203. [DOI] [PubMed] [Google Scholar]
- 9.Fonarow GC, Adams KF, Jr., Abraham WT, Yancy CW, Boscardin WJ. Risk stratification for in-hospital mortality in acutely decompensated heart failure: classification and regression tree analysis. Journal of the American Medical Association. 2005;293(5):572–580. doi: 10.1001/jama.293.5.572. [DOI] [PubMed] [Google Scholar]
- 10.Damman K, Navis G, Voors AA, et al. Worsening renal function and prognosis in heart failure: systematic review and meta-analysis. Journal of Cardiac Failure. 2007;13(8):599–608. doi: 10.1016/j.cardfail.2007.04.008. [DOI] [PubMed] [Google Scholar]
- 11.Gottlieb SS, Abraham W, Butler J, et al. The prognostic importance of different definitions of worsening renal function in congestive heart failure. Journal of Cardiac Failure. 2002;8(3):136–141. doi: 10.1054/jcaf.2002.125289. [DOI] [PubMed] [Google Scholar]
- 12.Hillege HL, Nitsch D, Pfeffer MA, et al. Renal function as a predictor of outcome in a broad spectrum of patients with heart failure. Circulation. 2006;113(5):671–678. doi: 10.1161/CIRCULATIONAHA.105.580506. [DOI] [PubMed] [Google Scholar]
- 13.Bhatia RS, Tu JV, Lee DS, et al. Outcome of heart failure with preserved ejection fraction in a population-based study. New England Journal of Medicine. 2006;355(3):260–269. doi: 10.1056/NEJMoa051530. [DOI] [PubMed] [Google Scholar]
- 14.McAlister FA, Ezekowitz J, Tonelli M, Armstrong PW. Renal insufficiency and heart failure: prognostic and therapeutic implications from a prospective cohort study. Circulation. 2004;109(8):1004–1009. doi: 10.1161/01.CIR.0000116764.53225.A9. [DOI] [PubMed] [Google Scholar]
- 15.Heywood JT, Fonarow GC, Costanzo MR, Mathur VS, Wigneswaran JR, Wynne J. High prevalence of renal dysfunction and its impact on outcome in 118,465 patients hospitalized with acute decompensated heart failure: a report from the ADHERE database. Journal of Cardiac Failure. 2007;13(6):422–430. doi: 10.1016/j.cardfail.2007.03.011. [DOI] [PubMed] [Google Scholar]
- 16.Adams KF, Jr., Fonarow GC, Emerman CL, et al. Characteristics and outcomes of patients hospitalized for heart failure in the United States: rationale, design, and preliminary observations from the first 100,000 cases in the Acute Decompensated Heart Failure National Registry (ADHERE) American Heart Journal. 2005;149(2):209–216. doi: 10.1016/j.ahj.2004.08.005. [DOI] [PubMed] [Google Scholar]
- 17.Dries DL, Exner DV, Domanski MJ, Greenberg B, Stevenson LW. The prognostic implications of renal insufficiency in asymptomatic and symptomatic patients with left ventricular systolic dysfunction. Journal of the American College of Cardiology. 2000;35(3):681–689. doi: 10.1016/s0735-1097(99)00608-7. [DOI] [PubMed] [Google Scholar]
- 18.Smilde TDJ, Hillege HL, Voors AA, Dunselman PHJ, Van Veldhuisen DJ. Prognostic importance of renal function in patients with early heart failure and mild left ventricular dysfunction. American Journal of Cardiology. 2004;94(2):240–243. doi: 10.1016/j.amjcard.2004.03.075. [DOI] [PubMed] [Google Scholar]
- 19.Smith GL, Lichtman JH, Bracken MB, et al. Renal impairment and outcomes in heart failure: systematic review and meta-analysis. Journal of the American College of Cardiology. 2006;47(10):1987–1996. doi: 10.1016/j.jacc.2005.11.084. [DOI] [PubMed] [Google Scholar]
- 20.Schrier RW, Abraham WT. Hormones and hemodynamics in heart failure. New England Journal of Medicine. 1999;341(8):577–585. doi: 10.1056/NEJM199908193410806. [DOI] [PubMed] [Google Scholar]
- 21.Brewster UC, Perazella MA. The renin-angiotensin-aldosterone system and the kidney: effects on kidney disease. American Journal of Medicine. 2004;116(4):263–272. doi: 10.1016/j.amjmed.2003.09.034. [DOI] [PubMed] [Google Scholar]
- 22.Smilde TD, Damman K, van der Harst P, et al. Differential associations between renal function and “modifiable” risk factors in patients with chronic heart failure. Clinical Research in Cardiology. 2009;98(2):121–129. doi: 10.1007/s00392-008-0732-z. [DOI] [PubMed] [Google Scholar]
- 23.Yancy CW, Lopatin M, Stevenson LW, De Marco T, Fonarow GC. Clinical presentation, management, and in-hospital outcomes of patients admitted with acute decompensated heart failure with preserved systolic function: a report from the Acute Decompensated Heart Failure National Registry (ADHERE) database. Journal of the American College of Cardiology. 2006;47(1):76–84. doi: 10.1016/j.jacc.2005.09.022. [DOI] [PubMed] [Google Scholar]
- 24.Nohria A, Hasselblad V, Stebbins A, et al. Cardiorenal interactions: insights from the ESCAPE trial. Journal of the American College of Cardiology. 2008;51(13):1268–1274. doi: 10.1016/j.jacc.2007.08.072. [DOI] [PubMed] [Google Scholar]
- 25.Firth JD, Raine AEG, Ledingham JGG. Raised venous pressure: a direct cause of renal sodium retention in oedema? Lancet. 1988;1(8593):1033–1036. doi: 10.1016/s0140-6736(88)91851-x. [DOI] [PubMed] [Google Scholar]
- 26.Maxwell MH, Breed ES, Schwartz IL. Renal venous pressure in chronic congestive heart failure. The Journal of Clinical Investigation. 1950;29(3):342–348. doi: 10.1172/JCI102263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kastner PR, Hall JE, Guyton AC. Renal hemodynamic responses to increased renal venous pressure: role of angiotensin II. The American Journal of Physiology. 1982;243(3):F260–F264. doi: 10.1152/ajprenal.1982.243.3.F260. [DOI] [PubMed] [Google Scholar]
- 28.Damman K, Navis G, Smilde TDJ, et al. Decreased cardiac output, venous congestion and the association with renal impairment in patients with cardiac dysfunction. European Journal of Heart Failure. 2007;9(9):872–878. doi: 10.1016/j.ejheart.2007.05.010. [DOI] [PubMed] [Google Scholar]
- 29.Mullens W, Abrahams Z, Francis GS, et al. Importance of venous congestion for worsening of renal function in advanced decompensated heart failure. Journal of the American College of Cardiology. 2009;53(7):589–596. doi: 10.1016/j.jacc.2008.05.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Damman K, van Deursen VM, Navis G, Voors AA, van Veldhuisen DJ, Hillege HL. Increased central venous pressure is associated with impaired renal function and mortality in a broad spectrum of patients with cardiovascular disease. Journal of the American College of Cardiology. 2009;53(7):582–588. doi: 10.1016/j.jacc.2008.08.080. [DOI] [PubMed] [Google Scholar]
- 31.Mullens W, Abrahams Z, Skouri HN, et al. Elevated intra-abdominal pressure in acute decompensated heart failure: a potential contributor to worsening renal function? Journal of the American College of Cardiology. 2008;51(3):300–306. doi: 10.1016/j.jacc.2007.09.043. [DOI] [PubMed] [Google Scholar]
- 32.Bradley SE, Bradley GP. The effect of increased intra-abdominal pressure on renal function in man. The Journal of Clinical Investigation. 1947;26(5):1010–1012. doi: 10.1172/JCI101867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Doty JM, Saggi BH, Sugerman HJ, et al. Effect of increased renal venous pressure on renal function. Journal of Trauma. 1999;47(6):1000–1003. doi: 10.1097/00005373-199912000-00002. [DOI] [PubMed] [Google Scholar]
- 34.Reid IA. Interactions between ANG II, sympathetic nervous system, and baroreceptor reflexes in regulation of blood pressure. American Journal of Physiology. 1992;262(6):E763–E778. doi: 10.1152/ajpendo.1992.262.6.E763. [DOI] [PubMed] [Google Scholar]
- 35.Ruiz-Ortega M, Lorenzo O, Egido J. Angiotensin III increases MCP-1 and activates NF-κB and AP-1 in cultured mesangial and mononuclear cells. Kidney International. 2000;57(6):2285–2298. doi: 10.1046/j.1523-1755.2000.00089.x. [DOI] [PubMed] [Google Scholar]
- 36.Griendling KK, Minieri CA, Ollerenshaw JD, Alexander RW. Angiotensin II stimulates NADH and NADPH oxidase activity in cultured vascular smooth muscle cells. Circulation Research. 1994;74(6):1141–1148. doi: 10.1161/01.res.74.6.1141. [DOI] [PubMed] [Google Scholar]
- 37.Chabrashvili T, Tojo A, Onozato ML, et al. Expression and cellular localization of classic NADPH oxidase subunits in the spontaneously hypertensive rat kidney. Hypertension. 2002;39(2):269–274. doi: 10.1161/hy0202.103264. [DOI] [PubMed] [Google Scholar]
- 38.Ruiz-Ortega M, Bustos C, Hernández-Presa MA, Lorenzo O, Plaza JJ, Egido J. Angiotensin II participates in mononuclear cell recruitment in experimental immune complex nephritis through nuclear factor-κB activation and monocyte chemoattractant protein-1 synthesis. Journal of Immunology. 1998;161(1):430–439. [PubMed] [Google Scholar]
- 39.Schlöndorff D, Nelson PJ, Luckow B, Banas B. Chemokines and renal disease. Kidney International. 1997;51(3):610–621. doi: 10.1038/ki.1997.90. [DOI] [PubMed] [Google Scholar]
- 40.Matsukawa T, Gotoh E, Minamisawa K, et al. Effects of intravenous infusions of angiotensin II on muscle sympathetic nerve activity in humans. American Journal of Physiology. 1991;261(3):R690–R696. doi: 10.1152/ajpregu.1991.261.3.R690. [DOI] [PubMed] [Google Scholar]
- 41.Ligtenberg G, Blankestijn PJ, Oey PL, et al. Reduction of sympathetic hyperactivity by enalapril in patients with chronic renal failure. New England Journal of Medicine. 1999;340(17):1321–1328. doi: 10.1056/NEJM199904293401704. [DOI] [PubMed] [Google Scholar]
- 42.Klein IHHT, Ligtenberg G, Oey PL, Koomans HA, Blankestijn PJ. Enalapril and losartan reduce sympathetic hyperactivity in patients with chronic renal failure. Journal of the American Society of Nephrology. 2003;14(2):425–430. doi: 10.1097/01.asn.0000045049.72965.b7. [DOI] [PubMed] [Google Scholar]
- 43.Kim S, Iwao H. Molecular and cellular mechanisms of angiotensin II-mediated cardiovascular and renal diseases. Pharmacological Reviews. 2000;52(1):11–34. [PubMed] [Google Scholar]
- 44.Kobori H, Nangaku M, Navar LG, Nishiyama A. The intrarenal renin-angiotensin system: from physiology to the pathobiology of hypertension and kidney disease. Pharmacological Reviews. 2007;59(3):251–287. doi: 10.1124/pr.59.3.3. [DOI] [PubMed] [Google Scholar]
- 45.Whaley-Connell AT, Chowdhury NA, Hayden MR, et al. Oxidative stress and glomerular filtration barrier injury: role of the renin-angiotensin system in the Ren2 transgenic rat. American Journal of Physiology. 2006;291(6):F1308–F1314. doi: 10.1152/ajprenal.00167.2006. [DOI] [PubMed] [Google Scholar]
- 46.Bataineh A, Raij L. Angiotensin II, nitric oxide, and end-organ damage in hypertension. Kidney International, Supplement. 1998;54(68):S14–S19. doi: 10.1046/j.1523-1755.1998.06806.x. [DOI] [PubMed] [Google Scholar]
- 47.De Nicola L, Blantz RC, Gabbai FB, Khang SJ. Nitric oxide and angiotensin II. Glomerular and tubular interaction in the rat. Journal of Clinical Investigation. 1992;89(4):1248–1256. doi: 10.1172/JCI115709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tolins JP, Palmer RMJ, Moncada S, Raij L. Role of endothelium-derived relaxing factor in regulation of renal hemodynamic responses. American Journal of Physiology. 1990;258(3):H655–H662. doi: 10.1152/ajpheart.1990.258.3.H655. [DOI] [PubMed] [Google Scholar]
- 49.Vallance P, Leone A, Calver A, Collier J, Moncada S. Accumulation of an endogenous inhibitor of nitric oxide synthesis in chronic renal failure. Lancet. 1992;339(8793):572–575. doi: 10.1016/0140-6736(92)90865-z. [DOI] [PubMed] [Google Scholar]
- 50.Kielstein JT, Bode-Böger SM, Klein G, Graf S, Haller H, Fliser D. Endogenous nitric oxide synthase inhibitors and renal perfusion in patients with heart failure. European Journal of Clinical Investigation. 2003;33(5):370–375. doi: 10.1046/j.1365-2362.2003.01149.x. [DOI] [PubMed] [Google Scholar]
- 51.Bakris GL, Re RN. Endothelin modulates angiotensin II-induced mitogenesis of human mesangial cells. American Journal of Physiology. 1993;264(6):F937–F942. doi: 10.1152/ajprenal.1993.264.6.F937. [DOI] [PubMed] [Google Scholar]
- 52.Hayakawa H, Raij L. Nitric oxide synthase activity and renal injury in genetic hypertension. Hypertension. 1998;31(1):266–270. doi: 10.1161/01.hyp.31.1.266. [DOI] [PubMed] [Google Scholar]
- 53.Jie KE, Verhaar MC, Cramer M-JM, et al. Erythropoietin and the cardiorenal syndrome: cellular mechanisms on the cardiorenal connectors. American Journal of Physiology. 2006;291(5):F932–F944. doi: 10.1152/ajprenal.00200.2006. [DOI] [PubMed] [Google Scholar]
- 54.Silverberg DS, Wexler D, Blum M, et al. The use of subcutaneous erythropoietin and intravenous iron for the treatment of the anemia of severe, resistant congestive heart failure improves cardiac and renal function and functional cardiac class, and markedly reduces hospitalizations. Journal of the American College of Cardiology. 2000;35(7):1737–1744. doi: 10.1016/s0735-1097(00)00613-6. [DOI] [PubMed] [Google Scholar]
- 55.Riegger GAJ, Liebau G, Kochsiek K. Antidiuretic hormone in congestive heart failure. American Journal of Medicine. 1982;72(1):49–52. doi: 10.1016/0002-9343(82)90576-9. [DOI] [PubMed] [Google Scholar]
- 56.Konstam MA, Gheorghiade M, Burnett JC, Jr., et al. Effects of oral tolvaptan in patients hospitalized for worsening heart failure: the EVEREST outcome trial. Journal of the American Medical Association. 2007;297(12):1319–1331. doi: 10.1001/jama.297.12.1319. [DOI] [PubMed] [Google Scholar]
- 57.Damman K, Van Veldhuisen DJ, Navis G, et al. Tubular damage in chronic systolic heart failure is associated with reduced survival independent of glomerular filtration rate. Heart. 2010;96(16):1297–1302. doi: 10.1136/hrt.2010.194878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Witko-Sarsat V, Friedlander M, Khoa TN, et al. Advanced oxidation protein products as novel mediators of inflammation and monocyte activation in chronic renal failure. Journal of Immunology. 1998;161(5):2524–2532. [PubMed] [Google Scholar]
- 59.Norman JT, Fine LG. Intrarenal oxygenation in chronic renal failure. Clinical and Experimental Pharmacology and Physiology. 2006;33(10):989–996. doi: 10.1111/j.1440-1681.2006.04476.x. [DOI] [PubMed] [Google Scholar]
- 60.Damman K, Kalra PR, Hillege H. Pathophysiological mechanisms contributing to renal dysfunction in chronic heart failure. Journal of Renal Care. 2010;36(supplement 1):18–26. doi: 10.1111/j.1755-6686.2010.00172.x. [DOI] [PubMed] [Google Scholar]
- 61.Haase M, Bellomo R, Devarajan P, Schlattmann P, Haase-Fielitz A. Accuracy of neutrophil gelatinase-associated lipocalin (NGAL) in diagnosis and prognosis in acute kidney injury: a systematic review and meta-analysis. American Journal of Kidney Diseases. 2009;54(6):1012–1024. doi: 10.1053/j.ajkd.2009.07.020. [DOI] [PubMed] [Google Scholar]
- 62.Han WK, Bailly V, Abichandani R, Thadhani R, Bonventre JV. Kidney Injury Molecule-1 (KIM-1): a novel biomarker for human renal proximal tubule injury. Kidney International. 2002;62(1):237–244. doi: 10.1046/j.1523-1755.2002.00433.x. [DOI] [PubMed] [Google Scholar]
- 63.Coca SG, Yalavarthy R, Concato J, Parikh CR. Biomarkers for the diagnosis and risk stratification of acute kidney injury: a systematic review. Kidney International. 2008;73(9):1008–1016. doi: 10.1038/sj.ki.5002729. [DOI] [PubMed] [Google Scholar]
- 64.Herget-Rosenthal S, van Wijk JAE, Bröcker-Preuss M, Bökenkamp A. Increased urinary cystatin C reflects structural and functional renal tubular impairment independent of glomerular filtration rate. Clinical Biochemistry. 2007;40(13-14):946–951. doi: 10.1016/j.clinbiochem.2007.04.013. [DOI] [PubMed] [Google Scholar]
- 65.Devarajan P. Emerging biomarkers for acute kidney injury. Clinical Laboratory International. April/ May 2009 [Google Scholar]
- 66.Leier CV. Renal roadblock in managing low output heart failure. Critical Care Medicine. 2004;32(5):1228–1229. doi: 10.1097/01.ccm.0000125510.02846.af. [DOI] [PubMed] [Google Scholar]
- 67.Determining Optimal Dose and Duration of Diuretic Treatment in People with Acute Heart Failure (The DOSE-AHF Study) August 2010, http://clinicaltrials.gov/ct2/show/NCT00577135.
- 68.Sackner-Bernstein JD, Skopicki HA, Aaronson KD. Risk of worsening renal function with nesiritide in patients with acutely decompensated heart failure. Circulation. 2005;111(12):1487–1491. doi: 10.1161/01.CIR.0000159340.93220.E4. [DOI] [PubMed] [Google Scholar]
- 69.Wang DJ, Dowling TC, Meadows D, et al. Nesiritide does not improve renal function in patients with chronic heart failure and worsening serum creatinine. Circulation. 2004;110(12):1620–1625. doi: 10.1161/01.CIR.0000141829.04031.25. [DOI] [PubMed] [Google Scholar]
- 70.Hernandez AF, O’Connor CM, Starling RC, et al. Rationale and design of the Acute Study of Clinical Effectiveness of Nesiritide in Decompensated Heart Failure Trial (ASCEND-HF) American Heart Journal. 2009;157(2):271–277. doi: 10.1016/j.ahj.2008.07.031. [DOI] [PubMed] [Google Scholar]
- 71.Costello-Boerrigter LC, Smith WB, Boerrigter G, et al. Vasopressin-2-receptor antagonism augments water excretion without changes in renal hemodynamics or sodium and potassium excretion in human heart failure. American Journal of Physiology. 2006;290(2):F273–F278. doi: 10.1152/ajprenal.00195.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Givertz MM, Massie BM, Fields TK, Pearson LL, Dittrich HC. The effects of KW-3902, an adenosine A1-receptor antagonist,on diuresis and renal function in patients with acute decompensated heart failure and renal impairment or diuretic resistance. Journal of the American College of Cardiology. 2007;50(16):1551–1560. doi: 10.1016/j.jacc.2007.07.019. [DOI] [PubMed] [Google Scholar]
- 73.Bart BA, Boyle A, Bank AJ, et al. Ultrafiltration versus usual care for hospitalized patients with heart failure: the relief for acutely fluid-overloaded patients with decompensated congestive heart failure (RAPID-CHF) trial. Journal of the American College of Cardiology. 2005;46(11):2043–2046. doi: 10.1016/j.jacc.2005.05.098. [DOI] [PubMed] [Google Scholar]
- 74.Costanzo MR, Guglin ME, Saltzberg MT, et al. Ultrafiltration versus intravenous diuretics for patients hospitalized for acute decompensated heart failure. Journal of the American College of Cardiology. 2007;49(6):675–683. doi: 10.1016/j.jacc.2006.07.073. [DOI] [PubMed] [Google Scholar]
- 75.Bart BA, Walsh MM, Blake D, Goldsmith SR. Ultrafiltration for cardiorenal syndrome. Journal of Cardiac Failure. 2008;14(6):531–532. doi: 10.1016/j.cardfail.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 76.Effectiveness of Ultrafiltration in Treating People With Acute Decompensated Heart Failure and Cardiorenal Syndrome (The CARRESS Study) August 2010, http://clinicaltrials.gov/ct2/show/NCT00608491.
- 77.Felker GM, Benza RL, Chandler AB, et al. Heart failure etiology and response to milrinone in decompensated heart failure: results from the OPTIME-CHF study. Journal of the American College of Cardiology. 2003;41(6):997–1003. doi: 10.1016/s0735-1097(02)02968-6. [DOI] [PubMed] [Google Scholar]
- 78.Yilmaz MB, Yalta K, Yontar C, et al. Levosimendan improves renal function in patients with acute decompensated heart failure: comparison with dobutamine. Cardiovascular Drugs and Therapy. 2007;21(6):431–435. doi: 10.1007/s10557-007-6066-7. [DOI] [PubMed] [Google Scholar]
- 79.Mebazaa A, Nieminen MS, Packer M, et al. Levosimendan vs dobutamine for patients with acute decompensated heart failure: the SURVIVE randomized trial. Journal of the American Medical Association. 2007;297(17):1883–1891. doi: 10.1001/jama.297.17.1883. [DOI] [PubMed] [Google Scholar]