Upper-abdominal exenteration (resection of the liver, pancreas, spleen, stomach, duodenum, and usually part of the colon) has been proposed for treatment of otherwise unresectable tumors (1). Replacement of the removed organs was originally with a liver homograft in continuity with the donor pancreas and a segment of duodenum. With a simplified version of this operation, only the liver is replaced, accepting the penalty of diabetes mellitus (2). The longest survivor following upper-abdominal exenteration now is approaching 2 years. We report here a follow-up on all 37 patients treated with these procedures through the end of 1989.
The actuarial survival at 1 year for the group is slightly better than 50% and is not significantly different with the two procedures (Fig. 1). Twenty-two of the 37 survivors have no evidence of recurrent tumor after 5–21 months. Six of the deaths were caused by technical complications. Four of these complications were after the more-complex cluster replacements and were derivative from the pancreas (pancreatitis and pancreatic abscess: 2 cases; and pancreatitis and rupture of arterial pseudoaneurysm: 2 cases). Technical deaths with the liver replacement alone accounted for only 2 of the losses (postoperative bleeding: 1 case; and biliary leak: 1 case).
FIGURE 1.
Survival of cluster Tx recipients, Pittsburgh, PA.
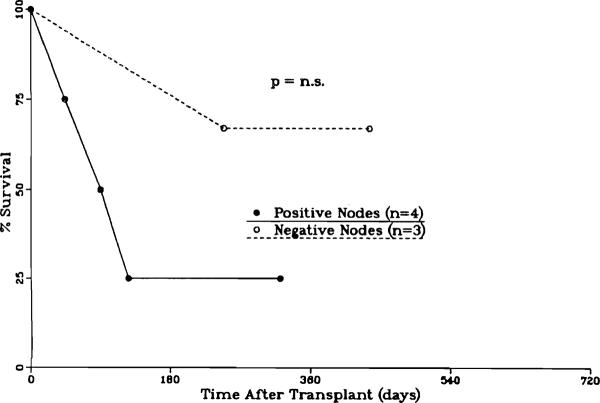
Apart from technical problems, the principal factors influencing survival were the type and extent of the primary tumor. Eight of the 11 patients operating on for neuroendocrine tumors or sarcomas are alive, after a mean follow-up of 12.5 months (follow-up ranging from 4.5 to 21 months); none of the 8 survivors have evidence of recurrence. Patients with the more common hepatocellular carcinomas (Fig. 2) and cholangiocarcinomas (Fig. 3) have fared less well, particularly if the lymph nodes were positive in the surgical specimen. Of 4 patients with hepatocellular carcinomas and positive lymph nodes, only one is currently alive and thought to be tumor free, approaching 1 year postoperative. The exceptional patient had hepatocellular carcinoma of the fibrolamellar variety that is known to carry a better prognosis. Nine patients with cholangiocarcinoma had positive lymph nodes; 3 are still alive and without evidence of recurrence after 11 (2 cases) and 9 months.
FIGURE 2.
Survival of HCC cluster Tx recipients, Pittsburgh, PA.
FIGURE 3.
Survival of cholangio CA Tx recipients, Pittsburgh, PA.
As previously emphasized (1), these patients suffer significant nutritional consequences as a result of the surgery. The patients approach a point of emaciation at about 3 months after successful surgery and then maintain a body weight usually 30% lower than preoperatively. Interestingly, their level of activity has not been commensurately reduced. Their energy level has been sufficient to support full-time employment for most of the survivors.
Current efforts are directed toward identifying the groups of patients who can benefit from the exenteration procedure, determining whether or not adjuvant chemotherapy or irradiation is beneficial, and ascertaining means of improving the quality of life postoperatively.
Acknowledgments
This work was supported by research grants from the Veterans Administration and Project Grant No. DK 29961 from the National Institutes of Health, Bethesda, MD.
REFERENCES
- 1.Starzl TE, Todo S, Tzakis A, et al. Abdominal organ cluster transplantation for the treatment of upper abdominal malignancies. Ann Surg. 1989;210:374. doi: 10.1097/00000658-198909000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tzakis AG, Todo S, Starzl TE. Upper abdominal exenteration with liver replacement: a modification of the “cluster” procedure. Transplant Proc. 1990;22:273. [PMC free article] [PubMed] [Google Scholar]