A 32-year-old man presented to our hospital on July 5, 2006, after the onset of headache, paresthesias of the left upper limb for 10 days, and weakness for 7 days before admission. He had eaten an inadequately cooked Pomacea canaliculata 20 days previously. Laboratory testing indicated a normal white blood cell count of 6,700/mm3 with mild eosinophilia of 7.8% (523/mm3). A lumbar puncture test showed an opening pressure of 220 mm H2O and 160 cells with 23% eosinophils, and cerebrospinal fluid (CSF) cultures were negative. We detected the circulating antigens (CAg) of Angiostrongylus cantonensis by double antibody sandwich enzyme-linked immunosorbent assay (ELISA), and they tested positive. This method had a high sensitivity (86.4%), and no cross-reactions with sera from patients with many other parasites were observed.1 Therefore, the result was helpful for diagnosis. Spinal magnetic resonance imaging (MRI) showed a lesion with high signal intensity in the cervical spinal cord on both sagittal and transverse T2-weighted imaging (T2WI) (Figures 1 and 2) at 9 days after admission.
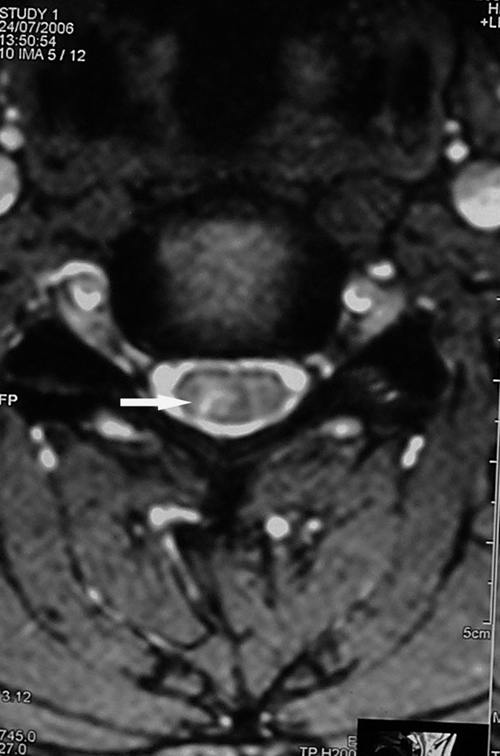
Figure 1.

A lesion in the cervical spinal cord presented as hyperintense on a sagittal T2WI.
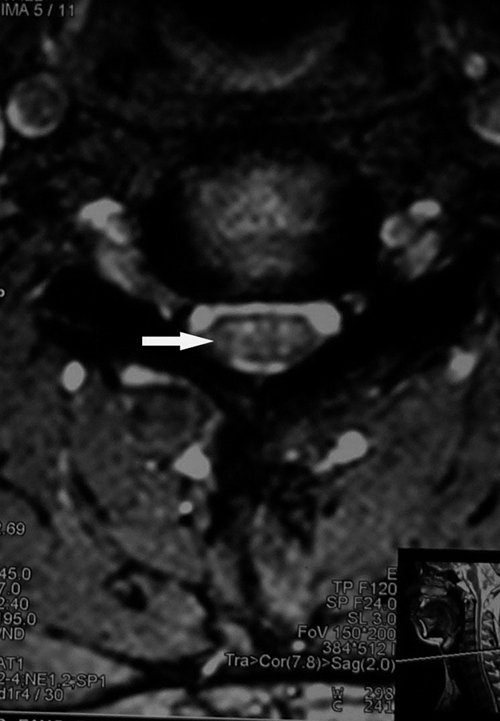
Figure 2.
A lesion in the cervical spinal cord presented as hyperintense on a transverse T2WI.
On the basis of history, clinical presentation, and examinations, a diagnosis of angiostrongyliasis was made,2 and the patient was treated with a combination of albendazole and dexamethasone. Symptoms of headache and paresthesia resolved within 14 days, and spinal-cord lesions completely resolved by a 1-month follow-up (Figures 3 and 4).
Figure 3.
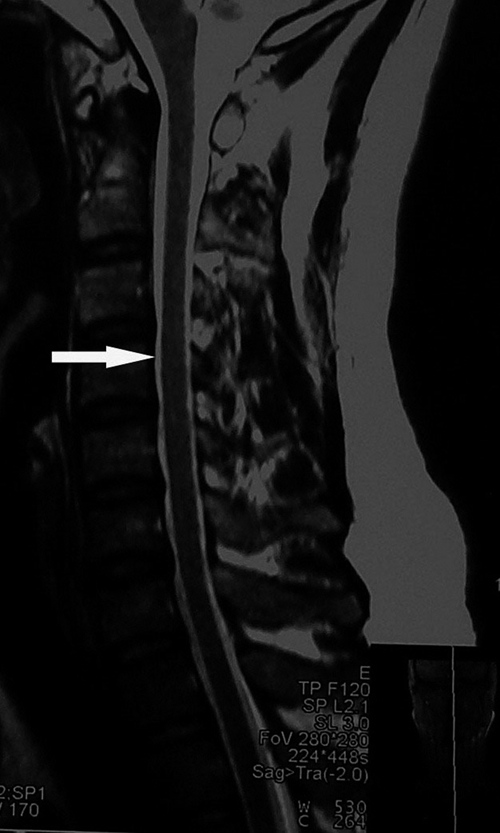
The abnormally high signal on a sagittal T2WI completely disappeared.
Figure 4.
The abnormally high signal on a sagittal T2WI completely disappeared.
Footnotes
Authors' addresses: Zongli Diao and Chenghong Yin, Beijing Tropical Medicine Research Institute, Beijing Friendship Hospital, Capital Medical University, Beijing, China, E-mails: diaozongli@yahoo.com.cn and modscn@yahoo.com.cn. Erhu Jin, Department of Radiology, Beijing Friendship Hospital, Capital Medical University, Beijing, China, E-mail: erhujin@hotmail.com.
References
- 1.Liang SH, Huang HC, Pan CW, Tan F. Detection of Angiostrongylus cantonensis circulating antigen by monoclonal antibodies. Zhonghua Yi Xue Za Zhi. 2005;85:3057–3061. [PubMed] [Google Scholar]
- 2.Wang QP, Lai DH, Zhu XQ, Chen XG, Lun ZR. Human angiostrongyliasis. Lancet Infect Dis. 2008;8:621–630. doi: 10.1016/S1473-3099(08)70229-9. [DOI] [PubMed] [Google Scholar]


