Abstract
This paper is a review article that collects and synthesizes up-to-date information about the complex etiological theories and treatment regimens associated with Fibromyalgia. The authors have written the paper in an evidence-based model in order to show the reader where adequate data exist in regards to these pharmacological, psychological, and physical strategies. A thorough MEDLINE search was utilized to collect many papers dedicated to this topic spanning 1970-2005. Measurements: The relevant papers were divided, based upon intervention used for the treatment of FM (pharmacological vs. non-pharmacological). They were also divided based on their scientific merit; randomized controlled trials were given the most evidence-based weight and the case studies the least. Results: The authors first review current epidemiologic and etiologic theories regarding fibromyalgia. A formal literature review is next presented to allow the reader to understand the evidence base that supports treatment of this disorder. In conclusion, a commentary regarding the treatment of this disorder in psychiatric practice occurs where pharmacodynamics and management strategy is discussed. Conclusion: There is much literature available regarding treatment of fibromyalgia. This complex illness has reasonable controlled studies for monotherapy treatments; however, multimodal treatments are the usual norm.
Keywords: Fibromyalgia, Pharmacotherapy, Psychotherapy, Physical therapy, Polypharmacy
Introduction
Fibromyalgia (FM) is a complex disorder with many associated symptoms. It affects two percent of the US population, approximately 3.7 million people in the US.1 The establishment of FM as a diagnosis has been an evolving process with the absence of definitive criteria until 1990. In 1990, the American College of Rheumatology published their research-based criteria, which is now the standard when diagnosing FM.2
There are four main components in FM: Pain, fatigue, mood, and function. FM occurs seven times more frequently in women than in men, and it occurs most frequently in women of childbearing age. Prevalence is 3.5 percent in women as compared to 0.5 percent in men.3 In outpatient rheumatology settings, 10 to 20 percent of patients seeking care have FM, while in outpatient, non-rheumatology settings, the prevalence is lower at 2.1 to 5.7 percent. In women between the ages of 60 and 79, the prevalence tends to be lower than expected at seven percent.3 Ninety percent of FM patients will have jaw and facial tenderness, especially pain on opening and closing their mouth, and the jaws having a “tight” sensation. These symptoms are similar to those seen with temporomandibular joint disease. In patients with fibromyalgia, 50 percent suffer from sensitivities to various elements in the environment, such as odors, noise, and bright lights. Some may have sensitivities to medications and various foods.
The treatment of FM is also important because of the deleterious impact it has on the economic condition and productivity of society. In one study, 26 percent of FM patients surveyed received some form of disability payment. The average cost of treating an FM patient was $2,274 per year. Despite a variety of treatments employed, patients tended to show no clear, sustained response over a seven-year follow-up period. Over 20 billion dollars per year are spent on FM patients because physicians are unable to provide them with clear, single therapies that work. Multimodal treatment is the norm. Despite this huge socioeconomic burden and frustrating attempts by clinicians to treat the pain, the quality of life for a person with FM remains poor.4
Given the impact of this illness and the overlap in care between primary care, rheumatology, neurology, and psychiatry, we have compiled a comprehensive review of treatment options available for the treatment of FM. As we are practicing psychiatrists, this paper is written from a psychiatric point of view. The paper also utilizes an evidence-based approach through which the reader will not only receive a comprehensive review of FM treatments, but gain some understanding in regards to the most well-studied treatments versus more anecdotal options. Finally, we will suggest some clinical options for the psychopharmacologist to consider if FM patients are encountered in psychiatric practice. We will discuss the etiology, clinical presentation, and nonpharmacological and pharmacological treatment options for FM throughout the paper. A listing of FM literature is provided in an extensive table at the end of the article.
Etiology
FM is a controversial syndrome due to the presence of a wide range of symptoms affecting multiple systems in the body and the difficulty in characterizing it into a specific systemic category. It is characterized by persistent widespread pain, abnormal pain sensitivity, and additional symptoms, such as fatigue, sleep disturbance, and mood symptoms. Although the exact etiology and pathogenesis of FM are still unknown, it has been suggested that stress or psychological factors may play a key role in the syndrome.
From 1904 to 1976, FM was known as fibrositis, an inflammatory disease, then the term fibromyalgia was coined due to the predominant pain symptoms seen in patients suffering from this illness.5 It was often noted that FM is associated with depression, stress, and anxiety. It is often felt that these psychiatric co-morbid disorders are more a result than the cause of FM.6–8
Multiple etiological theories have been proposed to explain the pathophysiology of FM. Studies suggest that the symptom of pain is present due to damage in various soft tissue organs of the body, such as the muscles; however, this was disproven by the absence of any damage noted in muscle biopsies of patients with FM.9
Abnormalities in the serotonin and epinephrine pathways have been suspected as a possible etiology for FM as both tricyclic antidepressants and selective serotonin antidepressants are sometimes useful in treatment, but the exact relationship and the role of serotonin in the etiology of FM remains unclear. It is possible that the abnormalities in these pathways prevent the dampening of afferent pain signals, causing an increase in perception of pain.
The increased concentration of a pain modulator Substance P may suggest an increased peripheral sensitivity to pain for patients with FM, but this was disproven by the lack of correlation between the level of substance P and the tenderness present in patients.10
An autoimmune process was suggested to be a probable etiology of FM due to the presence of cytokines, such as Interleukin 2 in patients with FM.11 It has not been distinguished whether the presence of this cytokine is a result or the cause of FM, leaving this theory in question.
Other studies found abnormalities in sleep patterns in patients with FM, including abnormal amounts of alpha activity and decreased delta sleep on the electroencephalogram,12 and a response to aerobic exercise programs, leading to an improvement in sleep abnormalities,13 which suggests that alteration in sleep patterns may be a possible etiology for FM.
Some other neuroendocrine abnormalities have been identified in FM patients,14,15 such as impairment in activation of the hypothalamic-pituitary-adrenal (HPA) axis and low, 24-hour, urinary free cortisol with normal peak and elevated trough plasma cortisol levels compared with normal subjects. This suggests an overall hyporesponsiveness at the HPA axis in patients with FM. The significance of these findings in terms of the etiology of FM is still unknown.
Due to the inability of the above purely biological theories to explain the exact pathophysiology of FM, a biopsychosocial etiology is the most practical model for the understanding of FM. Increased incidence in relatives of affected patients has been noted, which implies that inheritance may be a variable.16 Precipitating factors, such as trauma, infection, stress, or sleep deprivation, may help precipitate some of the biological changes mentioned above, leading to the onset of FM syndrome.
Clinical Presentation and Diagnosis
The diagnostic feature of FM is the prevalence of widespread bilateral pain. Pain is considered widespread when it is in both sides of the body and/or pain is above and below the waist. In addition, axial skeletal pain (cervical spine, anterior chest, thoracic spine, or low back pain) must be present.
Pain should be reproducible in 11 of 18 tender point sites upon digital palpation. The 18 tender point sites are as follows:
Occiput or suboccipital muscle insertions
Low cervical or anterior aspects of the intertransverse spaces at C5–C7
Trapezius or midpoint of the upper border
Supraspinatus or origins above the scapula spine near the medial border
Second rib or upper lateral to the second costochondral junction
Lateral epicondyle or at 2cm distal to the epicondyles
Gluteal or in upper, outer quadrants of buttocks in anterior fold of muscle
Greater trochanter or posterior to the trochanteric prominence
Knee or at the medial fat pad proximal to the joint line.
Digital palpation cannot be light and must be performed with an approximate force of 4kg. A moderate amount of pressure must be applied by the clinician to fully illicit a painful tenderpoint response. A tender point has to be painful at palpation, not just “tender” or uncomfortable.17
The following symptoms are often reported in descending order of occurrence: Muscular pain 100 percent, fatigue 96 percent, insomnia 86 percent, joint pain 72 percent, headaches 60 percent, restless legs 56 percent, numbness and tingling 52 percent, impaired memory 46 percent, leg cramps 42 percent, impaired concentration 41 percent, nervousness 32 percent, and major depression 20 percent.17
As understood by the data above, muscle pain remains the cardinal feature of FM, with fatigue and insomnia following it. Although depressive symptoms are felt to be common, the presence of a major depressive episode is prevalent in only 20 percent of FM patients. There is a significant overlap between the symptomatology of FM, depression, dysthymia, and generalized anxiety. The implication in regards to etiology and potential treatment is that perhaps common neural pathways both mediate and treat psychiatric and FM syndromes.
Most of the studies conducted on the correlation of comorbidity with FM suggest that the prevalence of depression and anxiety disorders is significant in patients with FM. In one study, 73 subjects with FM were found to have a high lifetime and current prevalence of major depression and panic disorder. The most common disorders were major depression (lifetime [L] = 68%, current [C] = 22%); dysthymia (10% [C only]); panic disorder (L = 16%, C = 7%); and simple phobia (L = 16%, C = 12%). Functional impairment on all measures of the Social Functioning -36 scale was severe (e.g., physical functioning = 45.5 and role limitations due to physical problems = 20.0).18 A study of 115 patients that looked at the functionality of FM patients with respect to coping mechanisms for pain divided the patients into three groups based on responses to the Multidimensional Pain Inventory (MPI): The dysfunctional group (DYS), the interpersonally distressed(ID) group, and the adaptive copers (AC). Overall, Axis I diagnoses were present in 74.8 percent of the participants with the DYS subgroup mainly reporting anxiety and the ID group reporting mood disorders. The AC group showed little comorbidity. Axis II diagnoses were present in only 8.7 percent of the FM sample. This suggested that FM is not a homogeneous syndrome and shows varying proportions of comorbid anxiety and depression disorders, which are dependent on psychosocial characteristics of the patients. Therefore, treatment should focus both on physical and psychological dysfunction.19 The research completed on the impact of comorbid conditions on FM has shown varied results. A Swiss study has shown the highest rate of comorbidity. In this study of 180 women, FM had 90-percent comorbidity with psychiatric disorders.20
Although multiple instruments have been used for the measurement of symptoms of FM, the Fibromyalgia Impact Questionnaire (FIQ) is the most standardized and widely used. It is an instrument designed to quantitate the overall impact of FM over many dimensions (e.g., function, pain level, fatigue, sleep disturbance, psychological distress). It is scored from 0 to 100 with 100 being the most severe. The average score for patients seen in tertiary care settings is about 50. The FIQ is widely used to assess change in FM status as well.21,22
The FIQ is a patient self-rated questionnaire that consists of 20 separate questions. Of these questions, 11 address the functionality and ask about the various activities and instrumental activities of daily living, such as shopping, laundry, and household work. Some questions address the impairment in number of days and the extent that symptoms of FM interfered with the ability to do household work. Other questions address the pain, stiffness, anxiety, and depression accompanied with the cardinal symptom of pain. Overall it measures physical functioning, work status, depression, anxiety, morning tiredness, pain, stiffness, fatigue, and wellbeing during the preceding week.
Management
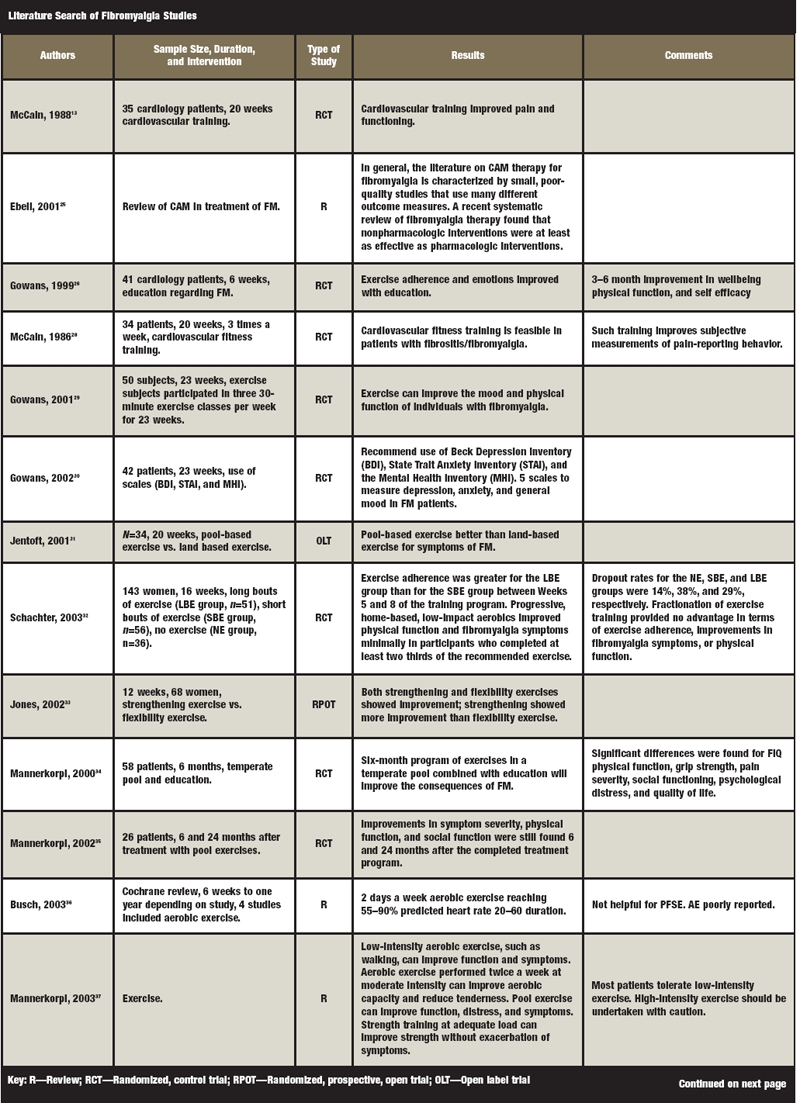
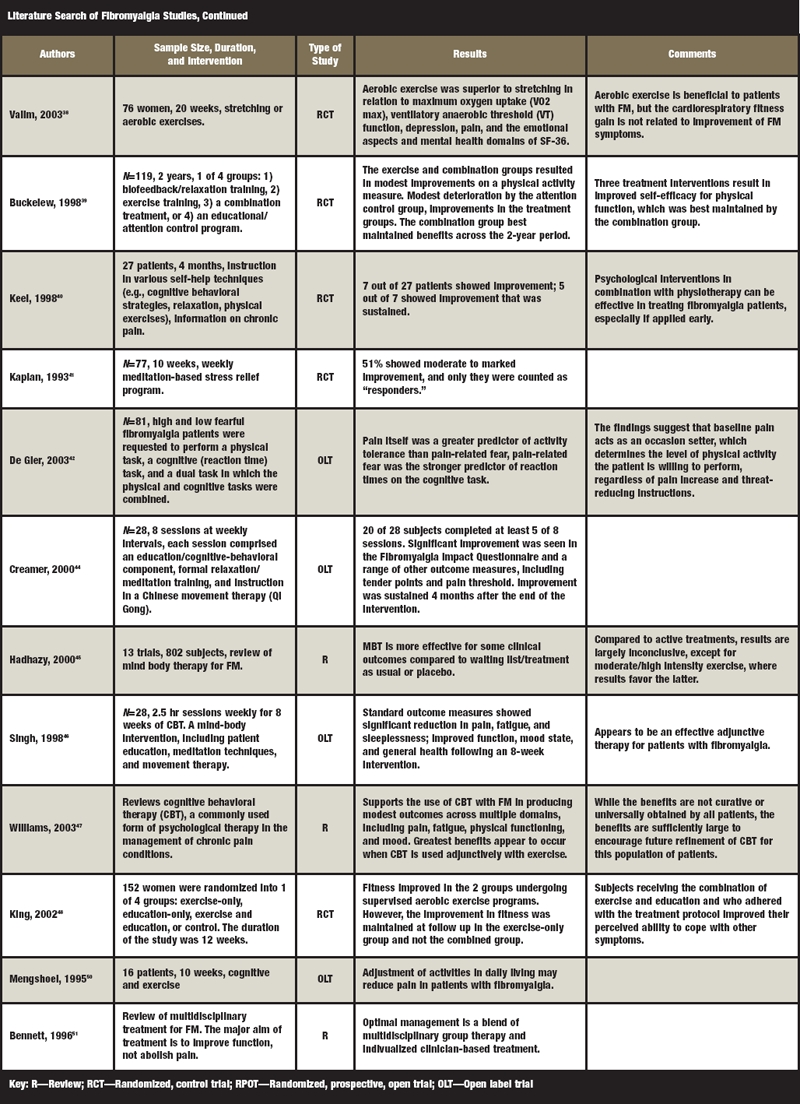
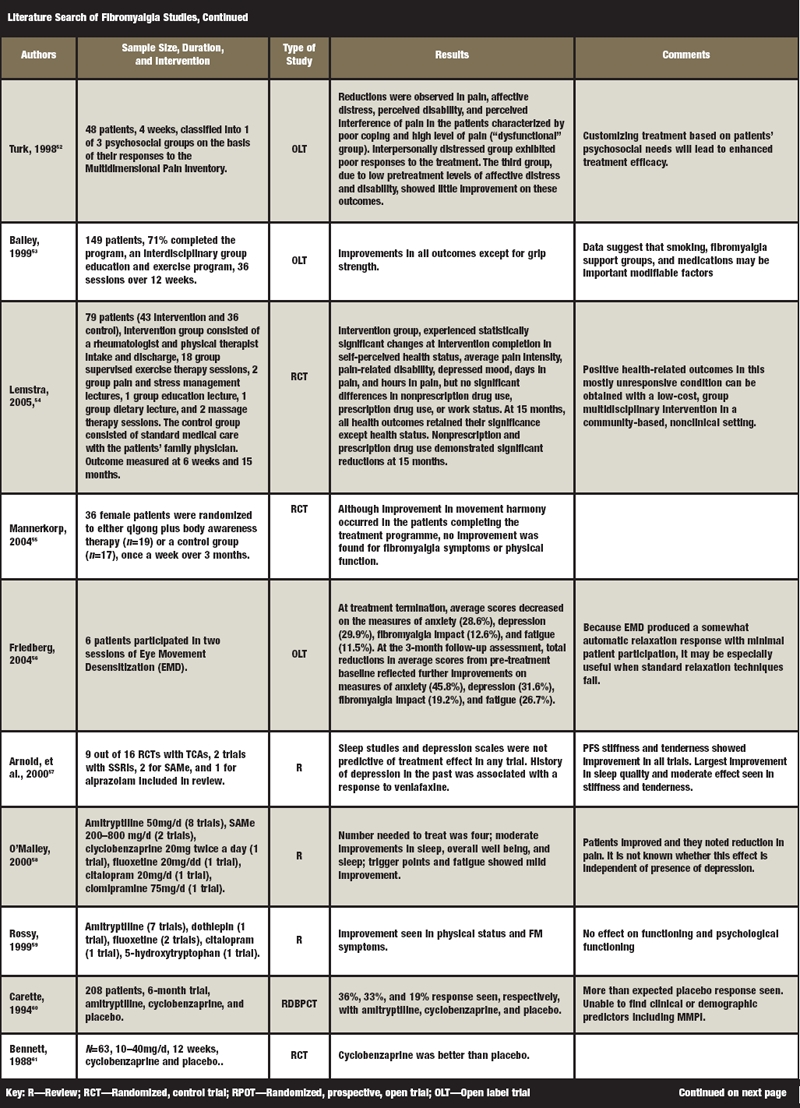
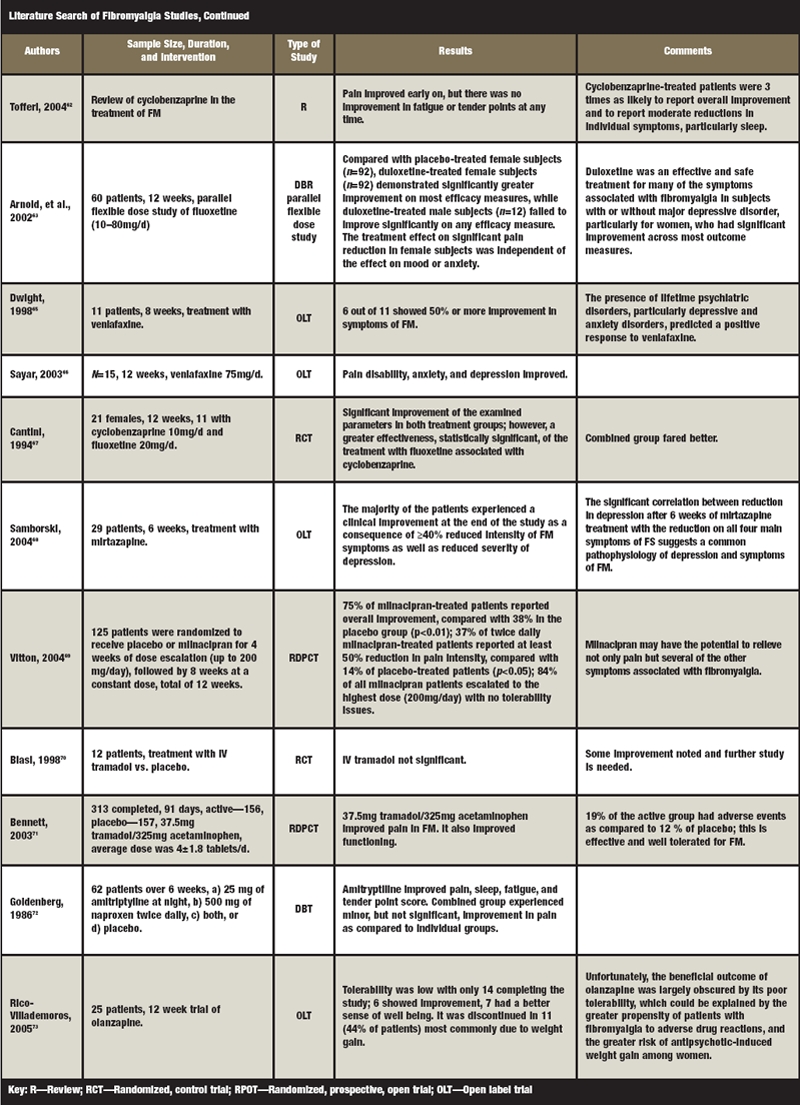
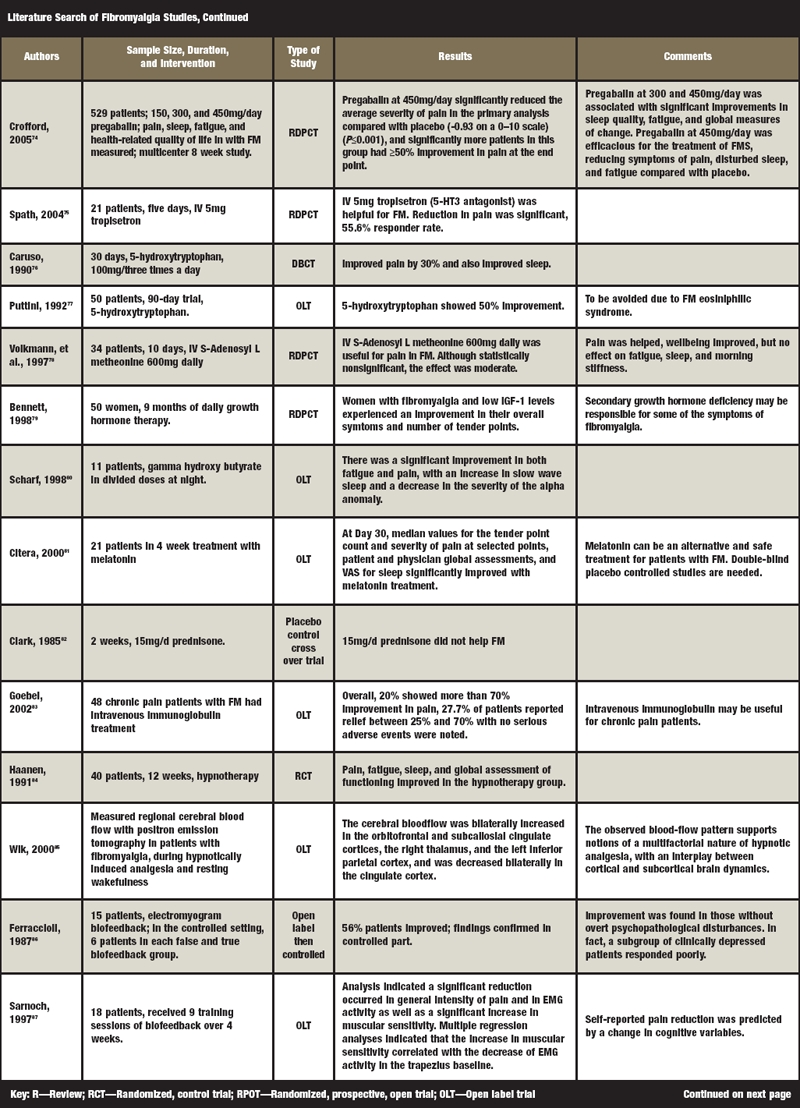
A concise listing of available literature regarding FM treatment is available in Table 1, and we summarize our findings in the final section of this paper for ease of reading. The next sections are narrative in nature and specifically discuss FM studies in an evidence-based manner in order for readers to better understand the specifics and scientific validity of the studies mentioned.
Due to the unknown and mixed etiology of FM, there have been multiple pharmacological and nonpharmacological treatments used to treat fibromyalgia, leading to intermediate results. Self-medication is very common among patients with FM. In an outpatient clinic, a survey asking patients with FM regarding the use of Complementary and Alternative Medications (CAM) for relief of symptoms illustrated that 98 percent of the patients had used some form of CAM in the last six months. The 10 most frequently used CAM treatments were exercise for a specific medical problem (48%), spiritual healing (prayers) (45%), massage therapy (44%), chiropractic treatments (37%), vitamin C (35%), vitamin E (31%), magnesium (29%), vitamin B complex (25%), green tea (24%), and weight-loss programs (20%).23
A recent comprehensive review was published as an attempt to establish guidelines for the management of FM.24 We will draw information from this paper and add the latest updates below. The outcome measures used in most studies mainly include the number of tender points and functionality assessed by the Fibromyalgia Impact Questionnaire (FIQ).
Non-pharmacological interventions. In general, the literature on Complementary and Alternative Medicine (CAM) therapy for FM is characterized by small, poor-quality studies that use many different outcome measures. A recent systematic review of FM therapy found that non-pharmacologic interventions were at least as effective as pharmacologic interventions.25
Patient education seems to be a useful tool, proving to be beneficial for patients in understanding and managing FM. Randomized, controlled trials in this area have shown that with the help of written material and group discussions, patient education improves pain, fatigue, sleep, and functionality (e.g., walking). Six to 17 weekly sessions have shown to be helpful. The patients who received education regarding the illness showed improvement in self-efficacy, FIQ, and the six-minute walk, as compared to the control group, which were waitlisted for treatment.26
Various types of exercise have been used for the treatment of FM, such as high intensity exercise, aerobic exercise, muscle strengthening exercise, and pool exercises (aqua therapy). These techniques have shown to be useful in FM patients for decreasing pain and improving functionality.27–35 A systemic review of all exercise trials36 for FM suggested that there is often improvement in aerobic performance, tender point pain threshold, and lessening of pain with exercise. Aerobic training is associated with better improvement than stretching exercises alone.37,38 Addition of education regarding FM tends to be more helpful than exercise alone or being on a treatment waiting list.26 Aerobic training and biofeedback as a combination were also more effective than the non-treated control group.39 Meditation, relaxation, and stress management40–42 have been shown to be helpful for pain improvement in FM patients. The above suggests that multimodal treatments may have the greatest effect.
Randomized, controlled trials of cognitive behavior therapy (CBT) with longitudinal data over 6 to 30 months found statistically decreased pain severity and improved functioning in FM.43–46 Systematic reviews have confirmed that CBT may improve all four components of FM (pain, fatigue, mood, and function).47
There is strong evidence that multidisciplinary treatment is effective in treating FM and, theoretically, it has the best response rates. Five randomized controlled trials of multidisciplinary treatment that combined education, CBT, or both with exercise were found beneficial for patient self-efficiency, significant decreases in pain, and improvements on a six-minute walk.26,34,35,40,48,49 One study observed the effects of six-week biofeedback therapy in combination with education, CBT, and exercise, and found that the combination of treatments is better than the education control group on self-efficiency and tender points.39 Positive changes has been noted in pain severity, FIQ, self-efficiency, and the six-minute walk, as well.43,44,50–53 After treatment, the beneficial effects seen with this multimodal treatment strategy were maintained in three out of five trials over a period of two years. In one key study, 43 patients were given a combined intervention in the form of a rheumatologist and physical therapist intake and discharge, 18 groups of supervised exercise therapy sessions, two groups of pain and stress management lectures, one group education lecture, one group dietary lecture, and two massage therapy sessions.54 The intervention group showed improvement in self-perceived health status, average pain intensity, pain-related disability, depressed mood, days in pain, and hours in pain, but no significant differences in nonprescription drug use, prescription drug use, or work status. These changes were maintained over 15 months, again suggesting the long-term effectiveness of multidisciplinary therapy.
Other therapies, such as qihong therapy with body awareness, have been tried, but no positive effect was found on FM symptoms and functioning.55 Eye movement desensitization and reprogramming (EMDR) in an open trial of only six patients helped the relaxation process when other relaxation processes failed.56
Pharmacological management. At least three metanalyses have looked at the efficacy of tricyclic antidepressants for FM. The results are mixed with two metanalyses suggesting that they do improve most of the symptoms of FM and one suggesting that even though the symptoms improved, the functionality of the patients did not show any improvement. A metanalysis57 confirmed trial data and concluded that tricyclic antidepressants, particularly in low doses (25–50mg/d), were effective for improving pain, sleep, fatigue, and depressive symptoms of fibromyalgia, with 25 to 37 percent of the patients tending to show improvement in symptoms. Most of the studies in this analysis included 6 to 12 weeks of treatment. A second metanalysis suggested improvement in all symptoms except tender point pain with low dose amitryptiline.58 A third review of medication use for FM included seven amitryptiline, two dothiepin, one citalopram, one 5-hydroxytryptophan, and two fluoxetine studies, showing that although medication was useful for improving physical status and FM symptoms, overall functionality did not improve despite medication use.59
Another tricyclic compound, cyclobenzaprine (10–40mg/d), which is used as a muscle relaxant, has been shown in multiple randomized, controlled trials (RCT)60,61 and one meta-analysis62 to be fairly effective for symptoms and functionality in FM. The improvement was not maintained over a period of six months for any of the tricyclic agents in limited studies.60
The newer antidepressants—fluoxetine, sertraline, venlafaxine, and duloxetine—have been shown to have moderate effectiveness for treating FM.63,64 The dosages used for the fluoxetine and duloxetine tended to be higher (80mg/d and 120mg/d, respectively). Lower dosages, such as 20mg of fluoxetine, were found to be not as effective. Venlafaxine at high doses (>150mg/d) was helpful for FM.65,66 A combination of fluoxetine (20mg/d) and cyclobenzaprine (10mg/d) seemed to help better than either agent alone.67
Mirtazapine, a noradrenergic, serotonergic, and histaminergic anitideprassant, improved FM symptoms in more than 40 percent of patients in open trials, but the results have yet to be replicated in controlled trials.68 As the improvement in symptoms of FM coincided with improvement in symptoms of depression, a common pathophysiology of these two may be possible. Of the patients treated with milnacipran, which is a highly noradrenergic serotonin norepinephrine reuptake inhibitor available in Europe, at 200mg/d, 75 percent reported overall improvement, compared with 38 percent in the placebo group. Thirty-seven percent of twice-daily milnacipran-treated patients reported at least 50-percent reduction in pain intensity, compared with 14 percent of placebo-treated patients (p<0.05).69
In RCTs, tramadol (20–300mg/d) with or without acetaminophen has been shown to reduce FM pain.70,71 In the long-term treatment of fibromyalgia, NSAIDS have been found useful only in combination with tricyclic antidepressants, and monotherapy results have been disappointing.72 There is no controlled data on the use of opioids for FM, although they are sometimes utilized in tertiary treatment. Most of these successful studies targeted and improved pain and tender points.
In an open trial using the second generation antipsychotic olanzapine for FM symptoms, tolerability was poor, with 44 percent discontinuing the medication, mainly due to weight gain. However, 6 out of 14 patients who completed the trial showed improvement in symptoms.73 Again, controlled trials are needed to validate the use of atypical antipsychotics in FM due to high incidences of metabolic side effects seen from medications.
Pregabalin is the only anticonvulsant that has been studied and found effective for FM. In one RCT,74 at a dosage of 450mg/d, pain, sleep, fatigue, and functionality improved in the treatment group.
Tropisetron (serotonin antagonist) and serotonin precursors have successfully shown improvement in symptoms of FM in three RCTs.75–77 S-adenosylmetheonine (SAMe) showed improvement in one RCT78 but was equivalent to placebo in another study. Women with FM with low insulin-like growth factor-1 (IGF) levels experienced an improvement in their overall symptoms and number of tender points after nine months of daily growth hormone therapy. This suggests that a secondary growth hormone deficiency may be responsible for some of the symptoms of FM.79 Gamma-hydroxybutyrate has been shown to be useful for improvement in fatigue and pain. It causes an increase in slow wave sleep and decrease in the severity of alpha sleep in FM patients.80 Thyroid hormone, dehydroepiandrosterone, melatonin, calcitonin dietary modifications, nutritional supplements, magnesium, herbal therapy, or vitamin therapy do not have sufficient data for us to comment on their efficicacy in FM.81 Prednisilone and guanefisin have shown to be noneffective for FM.82
Intravenous immunoglobulin injections for chronic pain were useful in reducing more than 70 percent of the pain in 1 out of 5 patients with multiple pain syndromes.83 Well-controlled studies focusing only on FM patients are needed to further validate its use.
Miscellaneous techniques. There is some evidence to support the use of relaxation techniques, biofeedback, and hypnosis in patients with FM. Eight sessions of hypnotherapy delivered over 12 weeks improved pain ratings, fatigue, sleep, and global assessment.84 A study using hypnotically induced analgesia found that patients experienced less pain during hypnosis than at rest.85 Electromyogram biofeedback was moderately effective in decreasing pain ratings and tender point counts.86,87 One study showed that hydrogalvanic baths and relaxation therapy did not help sleep and pain in FM patients.88 There are no randomized, controlled trials using trigger point and tender-point injections in patients with FM.
A review of seven studies using acupuncture in patients with FM reported increased pain thresholds, decreased pain ratings, and decreased medication use with acupuncture treatment.89 These results are often mixed with some trials showing acupuncture to be helpful.90,91
Chiropractic spinal manipulation and soft-tissue massage decreased tenderness in patients with FM.92,93 Both of these were open trials, and only the massage trial had a comparison group.
Connective tissue manipulation and massage produced positive results by reducing depression, pain intensity, and amount of analgesics used.93 A combination of diathermy ultrasound and inferential current improved pain levels and sleep compared to sham treatment.94 An Israeli RCT concluded that medicinal baths (Dead Sea sulfur baths) resulted in relief of FM-related symptoms of pain, fatigue, stiffness, and tender points.95 One review suggested that spa therapy would be useful as an adjunct to conventional treatment in FM patients.96
Discussion
To summarize, there is very strong evidence to support the use of low-dose tricyclic medications, such as amitriptyline and cyclobenzaprine, as well as cardiovascular exercise, CBT, patient education, or a combination of these for the management of FM. There is moderate evidence that tramadol, SSRIs, SNRIs, sodium oxybate, and certain anticonvulsants are effective, but the studies for newer agents are still ongoing. Moderate evidence also exists for the effectiveness of strength training exercise, acupuncture, hypnotherapy, biofeedback, massage, and warm water baths. As mentioned above, it appears that combinations of many modalities may offer the best treatment options and outcomes for patients with FM.
Controlled trials exist and suggest that some approaches are significantly beneficial. Furthermore, the finding that multiple treatment modalities that target various areas of life, including biological, psychological, and social aspects, are needed to reasonably treat fibromyalgia patients leads one to the theory that FM has a complex multifactorial etiology, possibly comparable to the biopsychosical model often employed in treating major depressive disorder (MDD) and other psychiatric illnesses. In regards to treating FM in psychiatric practice, we offer the following explanations and suggestions:
Borrowing from the thoughtful pharmacodynamic theory work of Stephen Stahl,97–99 there may be some underlying neurocircuitry malfunction associated with the production of key symptoms in Fibromyalgia. For example, fatigue, lethargy, and poor concentration are symptoms often associated with both FM and MDD. Both disorders are complex in symptom variability and heterogeneity and etiology. In MDD, the under-functioning of the norepinephrine system is felt to create some of these depressive symptoms. The corollary exists then that a noradrenergic-enhancing antidepressant may be able to reverse fatigue. If such an antidepressant could help fatigue associated with MDD, then it is possible that the same CNS mechanism or circuit is underperforming in FM-induced fatigue, and facilitating it may be helpful in treating. The evidence above suggests that norepinephrine-enhancing SNRIs are helpful here. Another neural circuit of interest may be that of histamine, which projects to the frontal cortex where executive functioning and perception of arousal state occur. CNS facilitation by presumably pro-histaminergic drugs, like modafinil, may treat fatigue associated with multiple medical conditions (obstructive apnea, Parkinson's disease), which may lend to its use in the treatment of FM fatigue in a similar manner.100,101 This example of using pharmacodynamic knowledge, i.e., the perception that fatigue is not only dependent on peripheral stimuli but also on the person's psychological threshold to manage fatigue and the brain's ability to interpret fatigue, could be useful to help reduce FM fatigue symptoms by increasing norepinephrine or histamine transmission. This approach would allow the clinician to choose complex medication regimens in order to reverse specific target FM symptoms comparable to our approach in MDD patients. Finally, instead of trying to promote wakefulness and appropriate energy during the daytime in FM as above, one could address the relative lack of slow wave, deep sleep in these patients at night and utilize an agent, such as sodium oxybate, which has shown to improve morning alertness and quality of sleep in patients with FM. There are controlled trials of this agent in FM to support its use.102,103 Again, one may use a different drug on a different set of neural circuits to allow better sleep (antihistamine products or GABA enhancing sedatives) and improved energy in FM as well, though there is less evidence here in the literature. This well-thought out combination of medication is rational polypharmacy for some patients. This approach is widely accepted in treating MDD for reasons noted above, and should strongly be considered when treating FM as well.
In regards to pain management, the same principles of fatigue management may be applied. There is reasonable controlled data showing that some forms of physical therapy are helpful in treating pain associated with FM. Assuming this is one of the safest treatments discussed, exercise is a good starting point for any clinician. If physical therapy fails to gain remission from FM symptoms, then an evidence-based approach that utilizes a second treatment modality not clearly related or overlapping with exercise might occur next. For example, instead of adding aerobic exercise, one could try CBT or biofeedback if available. Another path might lead toward using a medication that has supportive data, such as adding a tricyclic or an SNRI (e.g., duloxetine) to facilitate serotonin and norepinephrine. These drugs facilitate two neurotransmitters that are felt to be effective in either decreasing the peripheral pain signal upon entry to the CNS or allowing the brain to interpret these signals in a less severe manner. Again, the patient now has an exercise-based approach and a nonoverlapping pharmacodynamic approach to treating their FM. If the patient is still failing to reach remission from the FM target symptom of pain, then another additive approach could include the use of an antiepileptic/nocioceptive agent, such as pregabalin, to dampen peripheral pain signals via calcium channel modulation or tramadol to prompt an opiate-like response to dampen pain. Again, the theory is to use rational polypharmacy where medications with nonoverlapping mechanisms are added together to obtain an additive or synergistic effect. This practice, again, is similar to that used in treating MDD to full remission. However, the average psychiatrist may have to increase his or her comfort level in using some of these non-traditional psychotropics and also get used to using more off-label prescribing practices after assessing the literature available to support these practices.
Typically, the psychiatrist is not the primary provider for the FM patient. Psychiatrists are often asked to consult to rule out psychopathology and provide treatment if any exists. Certainly if there is a clear and comorbid mental illness, this is the domain of the psychopharmacologist, and usual practice guidelines should be followed for the specific psychiatric disorder being treated. However, the pain management aspect of care is often delegated to the primary care physician or rheumatologist. If this is the case, one may not delve completely into the rational polypharmacy practices noted above, but should continue to treat any Axis I/II conditions aggressively either with usual monotherapy or polypharmacy as needed. We suggest that psychiatrists challenge themselves and their countertransference towards these ‘somatic' patients who are often difficult to manage. There are clearly patients with FM who do not have any psychiatric comorbidity but develop depression, anxiety, regression toward Axis II conditions as a response to intractable pain and social dysfunction. There is a group that also develops pain from their primary psychological condition. Either way, aggressive psychiatric, psychological, or somatic treatment is warranted. The more complex the case, the more multimodal the treatment. We again would suggest a target symptom approach whereby each chief complaint symptom associated with FM is addressed. Monotherapy should be strived for, but the willingness to the psychiatrist to set up a good referral network with clinicians who offer these other treatment options, or to gain skill at using these alternative options, should be a clear goal in FM patient management.
References
- 1.Lawrence RC, Helmick CG, Arnett FC, et al. Estimates of the prevalence of arthritis and selected musculoskeletal disorders in the United States. Arthritis Rheum. 1998;41(5):778–99. doi: 10.1002/1529-0131(199805)41:5<778::AID-ART4>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 2.Wolfe F, Smythe HA, Yunus MB, et al. The American College of Rheumatology 1990 criteria for the classification of fibromyalgia. Report of the Multicenter Criteria Committee. Arthritis Rheum. 1990;33(2):160–72. doi: 10.1002/art.1780330203. [DOI] [PubMed] [Google Scholar]
- 3.Wolfe F, Ross K, Anderson J, Russell IJ, Hebert L. The prevalence and characteristics of fibromyalgia in the general population. Arthritis Rheum. 1995;38(1):19–28. doi: 10.1002/art.1780380104. [DOI] [PubMed] [Google Scholar]
- 4.National Fibromyalgia Research Association. Fibromyalgia syndrome diagnostic criteria. [June 8, 2005]. Available at: www.nfra.net/Diagnost.htm.
- 5.Gowers WR. Lumbago: Its lessons and analogues. Br Med J. 1904;1:117. doi: 10.1136/bmj.1.2246.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goldenberg DL. Psychological symptoms and psychiatric diagnosis in patients with fibromyalgia. J Rheumatol Suppl. 1989;19:127–30. [PubMed] [Google Scholar]
- 7.Yunus MB, Ahles TA, Aldag JC, Masi AT. Relationship of clinical features with psychological status in primary fibromyalgia. Arthritis Rheum. 1991;34(1):15–21. doi: 10.1002/art.1780340104. [DOI] [PubMed] [Google Scholar]
- 8.Dunne FJ, Dunne CA. Fibromyalgia syndrome and psychiatric disorder. Br J Hosp Med. 1995;54(5):194–7. [PubMed] [Google Scholar]
- 9.Drewes AM, Andreasen A, Schroder HD, et al. Pathology of skeletal muscle in fibromyalgia: A histo-immuno-chemical and ultrastructural study. Br J Rheumatol. 1993;32(6):479–83. doi: 10.1093/rheumatology/32.6.479. [DOI] [PubMed] [Google Scholar]
- 10.Russell IJ, Orr MD, Littman B, et al. Elevated cerebrospinal fluid levels of substance P in patients with the fibromyalgia syndrome. Arthritis Rheum. 1994;37(11):1593–601. doi: 10.1002/art.1780371106. [DOI] [PubMed] [Google Scholar]
- 11.Wallace DJ, Linker-Israeli M, Hallegua D, et al. Cytokines play an aetiopathogenetic role in fibromyalgia: A hypothesis and pilot study. Rheumatology. 2001;40(7):743–9. doi: 10.1093/rheumatology/40.7.743. (Oxford) [DOI] [PubMed] [Google Scholar]
- 12.Moldofsky H, Scarisbrick P, England R, Smythe H. Musculosketal symptoms and non-REM sleep disturbance in patients with “fibrositis syndrome” and healthy subjects. Psychosom Med. 1975;37(4):341–51. doi: 10.1097/00006842-197507000-00008. [DOI] [PubMed] [Google Scholar]
- 13.McCain GA, Bell DA, Mai FM, Halliday PD. A controlled study of the effects of a supervised cardiovascular fitness training program on the manifestations of primary fibromyalgia. Arthritis Rheum. 1988;31(9):1135–41. doi: 10.1002/art.1780310908. [DOI] [PubMed] [Google Scholar]
- 14.Crofford LJ, Pillemer SR, Kalogeras KT, et al. Hypothalamic-pituitary-adrenal axis perturbations in patients with fibromyalgia. Arthritis Rheum. 1994;37(11):1583–92. doi: 10.1002/art.1780371105. [DOI] [PubMed] [Google Scholar]
- 15.Moldofsky H. Sleep, neuroimmune, and neuroendocrine functions in fibromyalgia and chronic fatigue syndrome. Adv Neuroimmunol. 1995;5(1):39–56. doi: 10.1016/0960-5428(94)00048-s. [DOI] [PubMed] [Google Scholar]
- 16.Pellegrino MJ, Waylonis GW, Sommer A. Familial occurrence of primary fibromyalgia. Arch Phys Med Rehabil. 1989;70(1):61–3. [PubMed] [Google Scholar]
- 17.National Fibromyalgia Research Association. The American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia. [June 8, 2005]. Available at: www.nfra.net/Diagnost.htm.
- 18.Epstein SA, Kay G, Clauw D, et al. Psychiatric disorders in patients with fibromyalgia. A multicenter investigation. Psychosomatics. 1999;40(1):57–63. doi: 10.1016/S0033-3182(99)71272-7. [DOI] [PubMed] [Google Scholar]
- 19.Thieme K, Turk DC, Flor H. Comorbid depression and anxiety in fibromyalgia syndrome: Relationship to somatic and psychosocial variables. Psychosom Med. 2004;66(6):837–44. doi: 10.1097/01.psy.0000146329.63158.40. [DOI] [PubMed] [Google Scholar]
- 20.Bernatsky S, Dobkin PL, De Civita M, Penrod JR. Comorbidity and physician use in fibromyalgia. Swiss Med Wkly. 2005;135(5-6):76–81. doi: 10.4414/smw.2005.10774. [DOI] [PubMed] [Google Scholar]
- 21.Fibromyalgia Information from the Medical Professionals. Fibromyalgia impact questionnaire (FIQ) [June 8, 2005]. Available at: www.myalgia.com/FIQ/FIQ.htm.
- 22.Burckhardt CS, Clark SR, Bennett RM. The fibromyalgia impact questionnaire (FIQ): Development and validation. J Rheumatol. 1991;18:728–33. [PubMed] [Google Scholar]
- 23.Wahner-Roedler DL, Elkin PL, Vincent A, et al. Use of complementary and alternative medical therapies by patients referred to a fibromyalgia treatment program at a tertiary care center. Mayo Clin Proc. 2005;80(1):55–60. doi: 10.1016/S0025-6196(11)62958-3. [DOI] [PubMed] [Google Scholar]
- 24.Goldenberg DL, Burckhardt C, Crofford L. Management of fibromyalgia syndrome. J Am Med Assoc. 2004;292(19):2388–95. doi: 10.1001/jama.292.19.2388. [DOI] [PubMed] [Google Scholar]
- 25.Ebell MH, Beck E. Clinical inquiries. How effective are complementary/alternative medicine (CAM) therapies for fibromyalgia? J Fam Pract. 2001;50(5):400–1. [PubMed] [Google Scholar]
- 26.Gowans SE, deHueck A, Voss S, Richardson M. A randomized, controlled trial of exercise and education for individuals with fibromyalgia. Arthritis Care Res. 1999;12(2):120–8. doi: 10.1002/1529-0131(199904)12:2<120::aid-art7>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 27.McCain GA, Bell DA, Mai FM, Halliday PD. A controlled study of the effects of a supervised cardiovascular fitness training program on the manifestations of primary fibromyalgia. Arthritis Rheum. 1988;31(9):1135–41. doi: 10.1002/art.1780310908. [DOI] [PubMed] [Google Scholar]
- 28.McCain GA. Role of physical fitness training in the fibrositis/fibromyalgia syndrome. Am J Med. 1986;81(3A):73–7. doi: 10.1016/0002-9343(86)90881-8. [DOI] [PubMed] [Google Scholar]
- 29.Gowans SE, deHueck A, Voss S, et al. Effect of a randomized, controlled trial of exercise on mood and physical function in individuals with fibromyalgia. Arthritis Rheum. 2001;45(6):519–29. doi: 10.1002/1529-0131(200112)45:6<519::aid-art377>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 30.Gowans SE, DeHueck A, Abbey SE. Measuring exercise-induced mood changes in fibromyalgia: a comparison of several measures. Arthritis Rheum. 2002;47(6):603–9. doi: 10.1002/art.10789. [DOI] [PubMed] [Google Scholar]
- 31.Jentoft ES, Kvalvik AG, Mengshoel AM. Effects of pool-based and land-based aerobic exercise on women with fibromyalgia/chronic widespread muscle pain. Arthritis Rheum. 2001;45(1):42–7. doi: 10.1002/1529-0131(200102)45:1<42::AID-ANR82>3.0.CO;2-A. [DOI] [PubMed] [Google Scholar]
- 32.Schachter CL, Busch AJ, Peloso PM, Sheppard MS. Effects of short versus long bouts of aerobic exercise in sedentary women with fibromyalgia: A randomized controlled trial. Phys Ther. 2003;83(4):340–58. [PubMed] [Google Scholar]
- 33.Jones KD, Burckhardt CS, Clark SR, et al. A randomized controlled trial of muscle strengthening versus flexibility training in fibromyalgia. J Rheumatol. 2002;29(5):1041–8. [PubMed] [Google Scholar]
- 34.Mannerkorpi K, Nyberg B, Ahlmen M, Ekdahl C. Pool exercise combined with an education program for patients with fibromyalgia syndrome. A prospective, randomized study. J Rheumatol. 2000;(10):2473–81. [PubMed] [Google Scholar]
- 35.Mannerkorpi K, Ahlmen M, Ekdahl C. Six- and 24-month follow-up of pool exercise therapy and education for patients with fibromyalgia. Scand J Rheumatol. 2002;31(5):306–10. doi: 10.1080/030097402760375223. [DOI] [PubMed] [Google Scholar]
- 36.Busch A, Schachter CL, Peloso PM, Bombardier C. Exercise for treating fibromyalgia syndrome. Cochrane Database Syst Rev. 2002;(3):CD003786. doi: 10.1002/14651858.CD003786. [DOI] [PubMed] [Google Scholar]
- 37.Mannerkorpi K, Iversen MD. Physical exercise in fibromyalgia and related syndromes. Best Pract Res Clin Rheumatol. 2003;17(4):629–47. doi: 10.1016/s1521-6942(03)00038-x. [DOI] [PubMed] [Google Scholar]
- 38.Valim V, Oliveira L, Suda A, et al. Aerobic fitness effects in fibromyalgia. J Rheumatol. 2003;30(5):1060–9. [PubMed] [Google Scholar]
- 39.Buckelew SP, Conway R, Parker J, et al. Biofeedback/relaxation training and exercise interventions for fibromyalgia: A prospective trial. Arthritis Care Res. 1998;11(3):196–209. doi: 10.1002/art.1790110307. [DOI] [PubMed] [Google Scholar]
- 40.Keel PJ, Bodoky C, Gerhard U, Muller W. Comparison of integrated group therapy and group relaxation training for fibromyalgia. Clin J Pain. 1998;14(3):232–8. doi: 10.1097/00002508-199809000-00010. [DOI] [PubMed] [Google Scholar]
- 41.Kaplan KH, Goldenberg DL, Galvin-Nadeau M. The impact of a meditation-based stress reduction program on fibromyalgia. Gen Hosp Psychiatry. 1993;15(5):284–9. doi: 10.1016/0163-8343(93)90020-o. [DOI] [PubMed] [Google Scholar]
- 42.De Gier M, Peters ML, Vlaeyen JW. Fear of pain, physical performance, and attentional processes in patients with fibromyalgia. Pain. 2003;104(1-2):121–30. doi: 10.1016/s0304-3959(02)00487-6. [DOI] [PubMed] [Google Scholar]
- 43.Nielson WR, Walker C, McCain GA. Cognitive behavioral treatment of fibromyalgia syndrome: Preliminary findings. J Rheumatol. 1992;19(1):98–103. [PubMed] [Google Scholar]
- 44.Creamer P, Singh BB, Hochberg MC, Berman BM. Sustained improvement produced by nonpharmacologic intervention in fibromyalgia: Results of a pilot study. Arthritis Care Res. 2000;13(4):198–204. doi: 10.1002/1529-0131(200008)13:4<198::aid-anr4>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 45.Hadhazy VA, Ezzo J, Creamer P, Berman BM. Mind-body therapies for the treatment of fibromyalgia. A systematic review. J Rheumatol. 2000;27(12):2911–8. [PubMed] [Google Scholar]
- 46.Singh BB, Berman BM, Hadhazy VA, Creamer P. A pilot study of cognitive behavioral therapy in fibromyalgia. Altern Ther Health Med. 1998;4(2):67–70. [PubMed] [Google Scholar]
- 47.Williams DA, Cary MA, Groner KH, et al. Improving physical functional status in patients with fibromyalgia: A brief cognitive behavioral intervention. J Rheumatol. 2002;29(6):1280–6. [PubMed] [Google Scholar]
- 48.King SJ, Wessel J, Bhambhani Y, Sholter D, Maksymowych W. The effects of exercise and education, individually or combined, in women with fibromyalgia. J Rheumatol. 2002;29(12):2620–7. [PubMed] [Google Scholar]
- 49.Pfeiffer A, Thompson JM, Nelson A, et al. Effects of a 1.5-day multidisciplinary outpatient treatment program for fibromyalgia: A pilot study. Am J Phys Med Rehabil. 2003;82(3):186–91. doi: 10.1097/01.PHM.0000046625.72055.35. [DOI] [PubMed] [Google Scholar]
- 50.Mengshoel AM, Forseth KO, Haugen M, et al. Multidisciplinary approach to fibromyalgia. A pilot study. Clin Rheumatol. 1995;14(2):165–70. doi: 10.1007/BF02214937. [DOI] [PubMed] [Google Scholar]
- 51.Bennett RM. Multidisciplinary group programs to treat fibromyalgia patients. Rheum Dis Clin North Am. 1996;22(2):351–67. doi: 10.1016/s0889-857x(05)70276-3. [DOI] [PubMed] [Google Scholar]
- 52.Turk DC, Okifuji A, Sinclair JD, Starz TW. Differential responses by psychosocial subgroups of fibromyalgia syndrome patients to an interdisciplinary treatment. Arthritis Care Res. 1998;11(5):397–404. doi: 10.1002/art.1790110511. [DOI] [PubMed] [Google Scholar]
- 53.Bailey A, Starr L, Alderson M, Moreland J. A comparative evaluation of a fibromyalgia rehabilitation program. Arthritis Care Res. 1999;12(5):336–40. doi: 10.1002/1529-0131(199910)12:5<336::aid-art5>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 54.Lemstra M, Olszynski WP. The effectiveness of multidisciplinary rehabilitation in the treatment of fibromyalgia: A randomized controlled trial. Clin J Pain. 2005;21(2):166–74. doi: 10.1097/00002508-200503000-00008. [DOI] [PubMed] [Google Scholar]
- 55.Mannerkorpi K, Arndorw M. Efficacy and feasibility of a combination of body awareness therapy and qigong in patients with fibromyalgia: A pilot study. J Rehabil Med. 2004;36(6):279–81. doi: 10.1080/16501970410031912. [DOI] [PubMed] [Google Scholar]
- 56.Friedberg F. Eye movement desensitization in fibromyalgia: A pilot study. Complement Ther Nurs Midwifery. 2004;10(4):245–9. doi: 10.1016/j.ctnm.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 57.Arnold LM, Keck PE, Jr, Welge JA. Antidepressant treatment of fibromyalgia: A meta-analysis and review. Psychosomatics. 2000;41(2):104–13. doi: 10.1176/appi.psy.41.2.104. [DOI] [PubMed] [Google Scholar]
- 58.O'Malley PG, Balden E, Tomkins G, et al. Treatment of fibromyalgia with antidepressants: A meta-analysis. J Gen Intern Med. 2000;15(9):659–66. doi: 10.1046/j.1525-1497.2000.06279.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rossy LA, Buckelew SP, Dorr N, et al. A meta-analysis of fibromyalgia treatment interventions. Ann Behav Med. 1999;21(2):180–91. doi: 10.1007/BF02908299. [DOI] [PubMed] [Google Scholar]
- 60.Carette S, Bell MJ, Reynolds WJ, et al. Comparison of amitriptyline, cyclobenzaprine, and placebo in the treatment of fibromyalgia: A randomized, double-blind clinical trial. Arthritis Rheum. 1994;37(1):32–40. doi: 10.1002/art.1780370106. [DOI] [PubMed] [Google Scholar]
- 61.Bennett RM, Gatter RA, Campbell SM, et al. A comparison of cyclobenzaprine and placebo in the management of fibrositis. A double-blind, controlled study. Arthritis Rheum. 1988;31(12):1535–42. doi: 10.1002/art.1780311210. [DOI] [PubMed] [Google Scholar]
- 62.Tofferi JK, Jackson JL, O'Malley PG. Treatment of fibromyalgia with cyclobenzaprine: A meta-analysis. Arthritis Rheum. 2004;51(1):9–13. doi: 10.1002/art.20076. [DOI] [PubMed] [Google Scholar]
- 63.Arnold LM, Hess EV, Hudson JI, et al. A randomized, placebo-controlled, double-blind, flexible-dose study of fluoxetine in the treatment of women with fibromyalgia. Am J Med. 2002;112(3):191–7. doi: 10.1016/s0002-9343(01)01089-0. [DOI] [PubMed] [Google Scholar]
- 64.Arnold LM, Lu Y, Crofford LJ, et al. A double-blind, multicenter trial comparing duloxetine with placebo in the treatment of fibromyalgia patients with or without major depressive disorder. Arthritis Rheum. 2004;50(9):2974–84. doi: 10.1002/art.20485. [DOI] [PubMed] [Google Scholar]
- 65.Dwight MM, Arnold LM, O'Brien H, et al. An open clinical trial of venlafaxine treatment of fibromyalgia. Psychosomatics. 1998;39(1):14–7. doi: 10.1016/S0033-3182(98)71375-1. [DOI] [PubMed] [Google Scholar]
- 66.Sayar K, Aksu G, Ak I, Tosun M. Venlafaxine treatment of fibromyalgia. Ann Pharmacother. 2003;37(11):1561–5. doi: 10.1345/aph.1D112. [DOI] [PubMed] [Google Scholar]
- 67.Cantini F, Bellandi F, Niccoli L, Di Munno O. Fluoxetin combined with cyclobenzaprine in the treatment of fibromyalgia. Minerva Med. 1994;85(3):97–100. [PubMed] [Google Scholar]
- 68.Samborski W, Lezanska-Szpera M, Rybakowski JK. Effects of antidepressant mirtazapine on fibromyalgia symptoms. Rocz Akad Med Bialymst. 2004;49:265–9. [PubMed] [Google Scholar]
- 69.Vitton O, Gendreau M, Gendreau J, et al. A double-blind, placebo-controlled trial of milnacipran in the treatment of fibromyalgia. Hum Psychopharmacol. 2004;19(Suppl 1):S27–35. doi: 10.1002/hup.622. [DOI] [PubMed] [Google Scholar]
- 70.Biasi G, Manca S, Manganelli S, Marcolongo R. Tramadol in the fibromyalgia syndrome: A controlled clinical trial versus placebo. Int J Clin Pharmacol Res. 1998;18(1):13–9. [PubMed] [Google Scholar]
- 71.Bennett RM, Kamin M, Karim R, Rosenthal N. Tramadol and acetaminophen combination tablets in the treatment of fibromyalgia pain: A double-blind, randomized, placebo-controlled study. Am J Med. 2003;114(7):537–45. doi: 10.1016/s0002-9343(03)00116-5. [DOI] [PubMed] [Google Scholar]
- 72.Goldenberg DL, Felson DT, Dinerman H. A randomized, controlled trial of amitriptyline and naproxen in the treatment of patients with fibromyalgia. Arthritis Rheum. 1986;29(11):1371–7. doi: 10.1002/art.1780291110. [DOI] [PubMed] [Google Scholar]
- 73.Rico-Villademoros F, Hidalgo J, Dominguez I, et al. Atypical antipsychotics in the treatment of fibromyalgia: A case series with olanzapine. Prog Neuropsychopharmacol Biol Psychiatry. 2005;29(1):161–4. doi: 10.1016/j.pnpbp.2004.08.012. [DOI] [PubMed] [Google Scholar]
- 74.Crofford LJ, Rowbotham MC, Mease PJ. Pregabalin 1008-105 Study Group,et al. Pregabalin for the treatment of fibromyalgia syndrome: Results of a randomized, double-blind, placebo-controlled trial. Arthritis Rheum. 2005;52(4):1264–73. doi: 10.1002/art.20983. [DOI] [PubMed] [Google Scholar]
- 75.Spath M, Stratz T, Farber L, et al. Treatment of fibromyalgia with tropisetron—Dose and efficacy correlations. Scand J Rheumatol Suppl. 2004;(119):63–6. doi: 10.1080/03009740410007087. [DOI] [PubMed] [Google Scholar]
- 76.Caruso I, Sarzi Puttini P, Cazzola M, Azzolini V. Double-blind study of 5-hydroxytryptophan versus placebo in the treatment of primary fibromyalgia syndrome. J Int Med Res. 1990;18(3):201–9. doi: 10.1177/030006059001800304. [DOI] [PubMed] [Google Scholar]
- 77.Puttini PS, Caruso I. Primary fibromyalgia syndrome and 5-hydroxy-L-tryptophan: A 90-day open study. J Int Med Res. 1992;20(2):182–9. doi: 10.1177/030006059202000210. [DOI] [PubMed] [Google Scholar]
- 78.Volkmann H, Norregaard J, Jacobsen S, et al. Double-blind, placebo-controlled cross-over study of intravenous S-adenosyl-L-methionine in patients with fibromyalgia. Scand J Rheumatol. 1997;26(3):206–11. doi: 10.3109/03009749709065682. [DOI] [PubMed] [Google Scholar]
- 79.Bennett RM, Clark SC, Walczyk J. A randomized, double-blind, placebo-controlled study of growth hormone in the treatment of fibromyalgia. Am J Med. 1998;104(3):227–31. doi: 10.1016/s0002-9343(97)00351-3. [DOI] [PubMed] [Google Scholar]
- 80.Scharf MB, Hauck M, Stover R, et al. Effect of gamma-hydroxybutyrate on pain, fatigue, and the alpha sleep anomaly in patients with fibromyalgia: Preliminary report. J Rheumatol. 1998;25(10):1986–90. [PubMed] [Google Scholar]
- 81.Citera G, Arias MA, Maldonado-Cocco JA, et al. The effect of melatonin in patients with fibromyalgia: A pilot study. Clin Rheumatol. 2000;19(1):9–13. doi: 10.1007/s100670050003. [DOI] [PubMed] [Google Scholar]
- 82.Clark S, Tindall E, Bennett RM. A double-blind crossover trial of prednisone versus placebo in the treatment of fibrositis. J Rheumatol. 1985;12(5):980–3. [PubMed] [Google Scholar]
- 83.Goebel A, Netal S, Schedel R, Sprotte G. Human pooled immunoglobulin in the treatment of chronic pain syndromes. Pain Med. 2002;3(2):119–27. doi: 10.1046/j.1526-4637.2002.02018.x. [DOI] [PubMed] [Google Scholar]
- 84.Haanen HC, Hoenderdos HT, van Romunde LK, et al. Controlled trial of hypnotherapy in the treatment of refractory fibromyalgia. J Rheumatol. 1991;18(1):72–5. [PubMed] [Google Scholar]
- 85.Wik G, Fischer H, Bragee B, et al. Functional anatomy of hypnotic analgesia: A PET study of patients with fibromyalgia. Eur J Pain. 1999;3(1):7–12. doi: 10.1053/eujp.1998.0093. [DOI] [PubMed] [Google Scholar]
- 86.Ferraccioli G, Ghirelli L, Scita F, et al. EMG-biofeedback training in fibromyalgia syndrome. J Rheumatol. 1987;14(4):820–5. [PubMed] [Google Scholar]
- 87.Sarnoch H, Adler F, Scholz OB. Relevance of muscular sensitivity, muscular activity, and cognitive variables for pain reduction associated with EMG biofeedback in fibromyalgia. Percept Mot Skills. 1997;84(3 Pt 1):1043–50. doi: 10.2466/pms.1997.84.3.1043. [DOI] [PubMed] [Google Scholar]
- 88.Gunther V, Mur E, Kinigadner U, Miller C. Fibromyalgia: The effect of relaxation and hydrogalvanic bath therapy on the subjective pain experience. Clin Rheumatol. 1994;13(4):573–8. doi: 10.1007/BF02242996. [DOI] [PubMed] [Google Scholar]
- 89.Berman BM, Ezzo J, Hadhazy V, Swyers JP. Is acupuncture effective in the treatment of fibromyalgia? J Fam Pract. 1999;48(3):213–8. [PubMed] [Google Scholar]
- 90.Deluze C, Bosia L, Zirbs A, et al. Electroacupuncture in fibromyalgia: Results of a controlled trial. BMJ. 1992;305(6864):1249–52. doi: 10.1136/bmj.305.6864.1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Assefi NP, Sherman KJ, Jacobsen C, G, et al. A randomized clinical trial of acupuncture compared with sham acupuncture in fibromyalgia. Ann Intern Med. 2005;143(1):I24. doi: 10.7326/0003-4819-143-1-200507050-00005. [DOI] [PubMed] [Google Scholar]
- 92.Blunt KL, Rajwani MH, Guerriero RC. The effectiveness of chiropractic management of fibromyalgia patients: A pilot study. J Manipulative Physiol Ther. 1997;20(6):389–99. [PubMed] [Google Scholar]
- 93.Brattberg G. Connective tissue massage in the treatment of fibromyalgia. Eur J Pain. 1999;3(3):235–44. doi: 10.1053/eujp.1999.0123. [DOI] [PubMed] [Google Scholar]
- 94.Almeida TF, Roizenblatt S, Benedito-Silva AA, Tufik S. The effect of combined therapy (ultrasound and interferential current) on pain and sleep in fibromyalgia. Pain. 2003;104(3):665–72. doi: 10.1016/S0304-3959(03)00139-8. [DOI] [PubMed] [Google Scholar]
- 95.Buskila D, Abu-Shakra M, Neumann L, et al. Balneotherapy for fibromyalgia at the Dead Sea. Rheumatol Int. 2001;20(3):105–8. doi: 10.1007/s002960000085. [DOI] [PubMed] [Google Scholar]
- 96.Sukenik S, Flusser D, Abu-Shakra M. The role of spa therapy in various rheumatic diseases. Rheum Dis Clin North Am. 1999;25(4):883–97. doi: 10.1016/s0889-857x(05)70108-3. [DOI] [PubMed] [Google Scholar]
- 97.Demyttenaere K, De Fruyt J, Stahl SM. The many faces of fatigue in major depressive disorder. Int J Neuropsychopharmacol. 2005;8(1):93–105. doi: 10.1017/S1461145704004729. [DOI] [PubMed] [Google Scholar]
- 98.Stahl SM. Symptoms and circuits, part 1: Major depressive disorder. J Clin Psychiatry. 2003;64(11):1282–3. doi: 10.4088/jcp.v64n1101. [DOI] [PubMed] [Google Scholar]
- 99.Stahl SM. Deconstructing psychiatric disorders, part 2: An emerging, neurobiologically based therapeutic strategy for the modern psychopharmacologist. J Clin Psychiatry. 2003;64(10):1145–6. [PubMed] [Google Scholar]
- 100.Black JE, Hirshkowitz M. Modafinil for treatment of residual excessive sleepiness in nasal continuous positive airway pressure-treated obstructive sleep apnea/hypopnea syndrome. Sleep. 2005;28(4):464–71. doi: 10.1093/sleep/28.4.464. [DOI] [PubMed] [Google Scholar]
- 101.Ondo WG, Fayle R, Atassi F, Jankovic J. Modafinil for daytime somnolence in Parkinson's disease: Double-blind, placebo-controlled parallel trial. J Neurol Neurosurg Psychiatry. 2005;76(12):1636–9. doi: 10.1136/jnnp.2005.065870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Scharf MB, Baumann M, Berkowitz DV. The effects of sodium oxybate on clinical symptoms and sleep patterns in patients with fibromyalgia. J Rheumatol. 2003;30(5):1070–4. [PubMed] [Google Scholar]
- 103.Scharf MB, Hauck M, Stover R, et al. Effect of gamma-hydroxybutyrate on pain, fatigue, and the alpha sleep anomaly in patients with fibromyalgia. Preliminary report. J Rheumatol. 1998;25(10):1986–90. [PubMed] [Google Scholar]


