Abstract
Sudden cardiac death is the most common cause of mortality among patients with end stage kidney disease maintained on hemodialysis. To examine whether this increased risk is also seen with less advanced kidney disease we studied the relationship between glomerular filtration rate and risk of sudden cardiac death in patients with moderate kidney disease and known coronary artery disease. This retrospective longitudinal study encompassed 19,440 consecutive patients who underwent cardiac catheterization at a single academic institution. There were 522 adjudicated sudden cardiac death events yielding an overall rate of 4.6 events per 1000 patient years. This figure reflected rates of 3.8 events in 14,652 patients with estimated glomerular filtration rates (eGFR) ≥60 (stage 2 CKD or better) and 7.9 events in 4788 patients with glomerular filtration rates <60 (stage 3–5 CKD), all normalized to 1000 patient years. After adjusting for differences in known cardiac risk factors and other covariates in a multivariate Cox proportional hazards model, the eGFR was independently associated with sudden cardiac death (HR 1.11 per 10 ml/min decline in the eGFR). Our analysis found that reductions in the eGFR in CKD stages 3–5 are associated with a progressive increase in risk of sudden cardiac death in patients with coronary artery disease. Additional studies are needed to better characterize the mechanisms by which reduced kidney function increases this risk.
Chronic kidney disease (CKD) affects more than 20 million people in the United States, roughly 13% of the population, and 485,000 patients have end-stage renal disease (ESRD) requiring renal replacement therapy.1 Patients with all stages of CKD have a high prevalence of cardiovascular morbidity, but the risk of cardiovascular mortality is highest in patients with ESRD whose risk is 30 times greater than that of the general population.2–4 Among patients with ESRD, the leading cause of cardiovascular mortality is sudden cardiac death (SCD), defined as death resulting from the sudden, unexpected cessation of cardiac activity with hemodynamic collapse.2,5,6 Although the risk of SCD among ESRD patients is well documented, it is unclear whether this risk results primarily from the dialysis procedure or from a diminished glomerular filtration rate (GFR) independent of other known SCD risk factors.
In certain populations, a decreased GFR seems to be associated with an increased risk of SCD. In patients presenting with an acute myocardial infarction complicated by left ventricular dysfunction and/or heart failure who were enrolled in the VALsartan In Acute myocardial iNfarcTion (VALIANT) trial, a diminished GFR was independently associated with an increased risk of cardiovascular death.4 Resuscitation from cardiac arrest was also included as an outcome in this study, but the number of resuscitation events was too small to allow a clear characterization of the relationship between these events and CKD. In a subgroup analysis of patients with advanced heart failure and reduced left ventricular ejection fraction enrolled in the Multicenter Automatic Defibrillator Implantation Trial-II (MADIT-II), increased SCD risk was observed in subjects with lower GFR.7,8 More recently, in a cohort of postmenopausal women with coronary heart disease, declining GFR was found to be an independent predictor of SCD.9 Even though the mechanisms that confer this risk are not yet defined, these observations made in restricted populations suggest that a diminished GFR may be predictive of SCD.
We conducted this retrospective study to examine the risk of SCD in a large cohort of patients with CKD. We used the Duke Databank for Cardiovascular Disease (DDCD), a large database of patients undergoing a cardiac procedure at Duke Hospital that provides long-term follow-up data on patients with documented coronary artery disease (CAD). We hypothesized that decrements of GFR are associated with an increased risk of SCD and that this association is independent of known cardiac risk factors, including severity of preexisting cardiac disease.
RESULTS
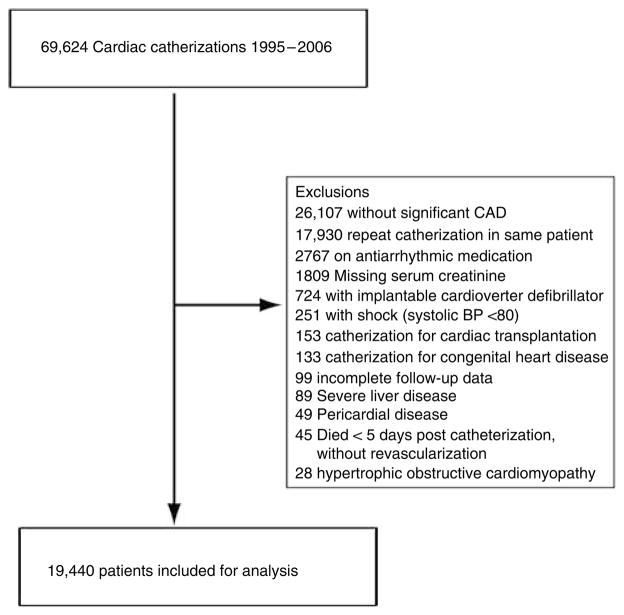
From 1 January 1995 through 30 June 2006, 69,624 cardiac catheterizations on 51,694 patients were recorded in DDCD. After excluding patients not eligible for this analysis, 19,440 patients were included in the study cohort (Figure 1). Table 1 depicts the baseline characteristics of patients by estimated GFR (eGFR). The median age of patients in the cohort was 63 years, 66% were male, 77% were Caucasian, 65% were hypertensive, 29% were diabetic, and 59% had hyperlipidemia. A total of 4788 (24.6%) patients had an eGFR <60 ml/min at the time of cardiac catheterization. A total of 249 (1.3%) patients were receiving dialysis therapy at the time of cardiac catheterization.
Figure 1. Study flow diagram illustrating cohort entry criteria and exclusions.
A total of 19,440 patients were included from among all patients undergoing cardiac catheterization over the 12-year study period after the exclusions listed above.
Table 1.
Baseline characteristics of the study cohort
| GFR ≥60 ml/min | GFR 15–59 ml/min | GFR <15 ml/min | Total | P-value* | |
|---|---|---|---|---|---|
| Number | 14,652 | 4364 | 424 | 19,440 | |
| Median age (IQR) | 60 (52, 69) | 71 (64, 77) | 61 (52, 69) | 63 (54, 72) | <0.001a,c |
| % Male | 70.45 | 51.40 | 51.42 | 65.76 | <0.001a,b |
| % Caucasian | 77.19 | 79.87 | 40.77 | 76.98 | <0.001a,b,c |
| Median systolic pressure (IQR) | 141 (124, 160) | 149 (130, 170) | 157 (136, 175) | 143 (126, 162) | <0.001a,b,c |
| Median diastolic pressure (IQR) | 79 (70, 88) | 78 (68, 87) | 81 (70, 93) | 79 (69, 88) | <0.001a,b,c |
| Median pulse (IQR) | 69 (60, 80) | 70 (61, 80) | 75 (67, 85) | 70 (61, 80) | <0.001a,b,c |
| % Hypertensive | 61.79 | 75.53 | 89.39 | 65.47 | <0.001a,b,c |
| % Diabetic | 26.49 | 35.70 | 62.97 | 29.36 | <0.001a,b,c |
| % Hyperlipidemia | 58.65 | 59.46 | 51.89 | 58.68 | 0.010b,c |
| % Tobacco use | 60.95 | 48.21 | 35.38 | 57.53 | <0.001a,b,c |
| % History of congestive heart failure | 16.86 | 33.99 | 41.45 | 21.26 | <0.001a,b,c |
| New York Heart Association Class | <0.001a,b | ||||
| None | 85.83 | 69.54 | 62.95 | 81.73 | |
| I | 2.35 | 4.97 | 6.99 | 3.03 | |
| II | 4.33 | 6.74 | 5.96 | 4.90 | |
| III | 4.62 | 11.69 | 13.21 | 6.37 | |
| IV | 2.86 | 7.06 | 10.88 | 3.97 | |
| Median ejection fraction % (IQR) | 57 (47, 65) | 54 (41, 63) | 52 (40, 60) | 56 (45, 64) | <0.001a,b |
| % Peripheral vascular disease | 9.15 | 15.74 | 19.34 | 10.85 | <0.001a,b |
| % Cerebrovascular disease | 8.77 | 16.43 | 15.09 | 10.63 | <0.001a,b |
| % History of myocardial infarction | 46.18 | 44.39 | 37.50 | 45.59 | <0.001b,c |
| % Atrial fibrillation during hospitalization | 5.80 | 10.63 | 5.66 | 6.88 | <0.001a,c |
| % Previous coronary artery bypass grafting | 17.48 | 24.54 | 13.92 | 18.99 | <0.001a,c |
| % Previous percutaneous coronary intervention | 11.84 | 11.55 | 6.60 | 11.66 | 0.004b,c |
| Number of diseased vessels | <0.001a,b | ||||
| 1 | 47.69 | 35.70 | 31.84 | 44.66 | |
| 2 | 25.06 | 24.77 | 30.42 | 25.11 | |
| 3 | 27.25 | 39.53 | 37.74 | 30.23 | |
| % On dialysis | 0 | 0 | 58.73 | 1.28 | <0.001b,c |
| Median years to death or last known alive (IQR) | 6.1 (3.2, 9.1) | 4.2 (2.0, 7.4) | 2.1 (1.0, 4.2) | 5.5 (3.0, 8.8) | <0.001a,b,c |
| In hospital medications | |||||
| % Aspirin | 90.01 | 90.01 | 82.31 | 89.84 | <0.001b,c |
| % Statin | 53.41 | 53.32 | 42.92 | 53.16 | <0.001b,c |
| % β-Blockers | 78.28 | 77.41 | 77.83 | 78.07 | 0.472 |
| % ACEI/ARB | 55.11 | 57.86 | 51.42 | 55.64 | 0.001a |
| % Diuretics | 31.78 | 53.69 | 32.08 | 36.71 | <0.001a,c |
| % K-sparing diuretics | 1.37 | 3.41 | 0.94 | 1.82 | <0.001ac |
ACEI/ARB, angiotensin-converting enzyme inhibitor/angiotensin receptor blocker; GFR, glomerular filtration rate; IQR, interquartile range.
P-value < 0.01 for pairwise comparisons as follows:
GFR ≥60 vs GFR 15–59;
GFR ≥60 vs GFR<15; and
GFR=15–59 vs GFR<15.
Data reported as percentages or medians with IQR in parentheses. P-values reported using the Kruskal–Wallis test and Wilcoxon rank-sum test for continuous variables and the Pearson χ2-test for categorical variables.
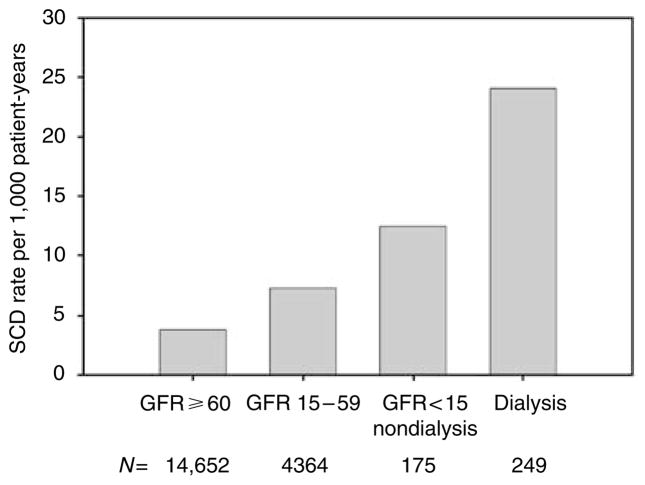
In the 12-year study period, we were able to ascertain vital status and to determine cause of death for 97.1% of all study participants. The median follow-up time was 5.5 years (interquartile range 3.0–8.8). There were 522 SCD events with an SCD rate of 4.6 per 1000 patient-years. For patients with an eGFR ≥60 ml/min, the SCD rate was 3.8 per 1000 patient-years; for patients with an eGFR 15–59 ml/min, it was 7.3 per 1000 patient-years. For those with eGFR <15 but not yet on dialysis at baseline, the rate increased to 12.6 per 1000 patient-years, and the rate nearly doubled for patients on dialysis to 24.2 per 1000 patient years (Figure 2). Of these events, 274 events were classified as witnessed sudden death, 60 were deaths after resuscitation, and 188 were unobserved deaths. The unadjusted hazard ratios for SCD are presented in Table 2. The risk of SCD was significantly higher for patients with an eGFR <60 ml/min compared with those with an eGFR ≥60 ml/min (P< 0.0001). The relationship between baseline eGFR and SCD risk is graphically depicted in Figure 3.
Figure 2. Rates of SCD by the baseline eGFR category.
Rates shown as events per 1000 patient-years and were as follows: eGFR ≥60 ml/min, 3.8 (95% CI: 0, 8); eGFR 15–59 ml/min, 7.3 (95% CI: 2, 13); eGFR < 15 not on dialysis, 12.5 (95% CI: 5, 20); and dialysis, 24.1 (95% CI: 14, 34). For all subsequent analyses, dialysis and non-dialysis patients with eGFR <15 were combined into a single group (eGFR <15).
Table 2.
Unadjusted hazard ratios for SCD by GFR
| Estimated GFR ml/min | N | Hazard ratio | 95% Confidence interval |
|---|---|---|---|
| ≥60 | 14,652 | Reference | Reference |
| 15–59 | 4364 | 1.88 | 1.56, 2.28 |
| <15 | 424 | 4.68 | 3.06, 7.17 |
GFR, glomerular filtration rate; SCD, sudden cardiac death.
Figure 3. Unadjusted SCD risk expressed as logarithm of the hazard ratio across the spectrum of eGFR.
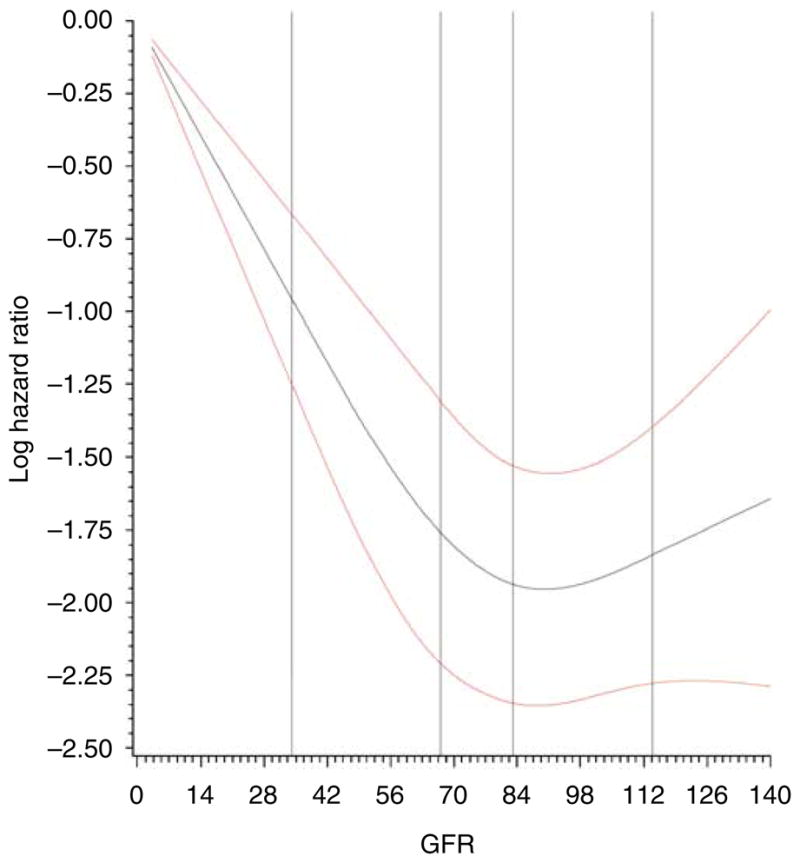
Red lines illustrate 95% confidence intervals. eGFR is inversely and linearly related to increased SCD risk. There does not appear to be an increasing benefit for SCD-free survival above GFR values over 90 ml/min/ 1.73m2.
The variables that were found to be significantly associated with SCD are listed in Table 3. Baseline eGFR was strongly associated with SCD, with an adjusted hazard ratio of 1.11 per 10 ml/min decrement in eGFR (95% CI: 1.06, 1.17), and accounted for ~11% of the predictive value of the model. In the adjusted model, eGFR had an independent and strong association with SCD roughly equivalent to the association observed with treatment of CAD with percutaneous intervention and stronger than associations observed with severity of CAD, CHF, and diabetes. Upon excluding patients with unobserved death, eGFR remained independently associated with the end point of witnessed SCD, with an adjusted hazard ratio of 1.16 (95% CI: 1.09, 1.23) for each 10 ml/min reduction in eGFR.
Table 3.
Adjusted hazard ratios for SCD
| Variable | Hazard ratio | 95% Confidence interval | Wald χ2 | P-value |
|---|---|---|---|---|
| CABG treatment | 0.41 | 0.31, 0.56 | 34.0 | <0.001 |
| GFRa (HR per 10 ml/min decrease) | 1.11 | 1.06, 1.17 | 18.0 | <0.001 |
| PCI treatment | 0.63 | 0.50, 0.78 | 17.4 | <0.001 |
| History of diabetes | 1.49 | 1.19, 1.87 | 12.3 | <0.001 |
| In hospital diuretic use | 1.55 | 1.21, 1.98 | 12.1 | <0.001 |
| History of COPD | 1.61 | 1.21, 2.13 | 10.7 | 0.001 |
| History of myocardial infarction | 1.34 | 1.11, 1.62 | 9.1 | 0.003 |
| In hospital ACEI/ARB use | 1.36 | 1.10, 1.68 | 8.0 | 0.005 |
| Number of diseased coronary vessels | 1.25 | 1.06, 1.47 | 7.0 | 0.008 |
| Smoking history | 1.30 | 1.06, 1.60 | 6.3 | 0.012 |
| History of hyperlipidemia | 0.80 | 0.67, 0.97 | 5.5 | 0.019 |
| New York Heart Association Class (HR per 1 increase; classes III and IV combined) | 1.10 | 1.01, 1.20 | 5.1 | 0.024 |
| History of peripheral vascular disease | 1.31 | 1.02, 1.66 | 4.6 | 0.032 |
| Any valvular heart disease | 1.30 | 1.02, 1.66 | 4.4 | 0.036 |
AEI/ARB, angiotensin-converting enzyme inhibitor/angiotensin receptor blocker; CABG, coronary artery bypass grafting; CAD, coronary artery disease; COPD, chronic obstructive pulmonary disease; eGFR, estimated GFR; GFR, glomerular filtration rate; HR, hazard ratio; PCI, percutaneous intervention; SCD, sudden cardiac death.
Overall model χ2=383.2. All variables listed above included in the adjusted model as well as age, gender, and propensity scores for PCI, CABG, and medical treatment only after catheterization.
GFR values above 90 were truncated at 90 to satisfy linearity assumption.
HRs reported using Cox proportional hazards regression modeling. All variables that were significantly associated with SCD are listed in order of influence in the adjusted model. As illustrated by Wald χ2 values, eGFR had an independent and strong association with SCD equivalent to the association between severity of CAD, CHF, and diabetes.
DISCUSSION
This study shows that CKD is strongly and independently associated with SCD in patients known to have CAD. After accounting for case-mix factors, medications, clinical variables, and known cardiac risk factors, each 10 ml/min decrement in eGFR the risk for SCD increased by 11%. Furthermore, a 10 ml/min decrement in eGFR had a stronger association with SCD than all other variables examined except for treatment of CAD with CABG. Even when SCD was defined strictly as witnessed SCD events, the risk associated with decreased eGFR persisted.
In the 19,440 patients included in this study, we characterized 522 events as SCD over a 12-year interval. The event rate at 1-year post-catheterization was 0.7%. This is similar to the SCD annual event rates estimated for the general population (0.2%), for those patients with known cardiovascular risk factors (0.5%), and in women followed in the HERS trial (0.5–1.7%).9–11 This study extends initial observations that were made in smaller restricted populations to a larger, more diverse cohort. Our study provides more evidence that patients with CKD have an increased risk of SCD and that this risk begins as early as stage 3 CKD, or eGFR < 60 ml/min.
Why patients with CKD are at an increased risk for SCD is largely speculative, but it is likely mediated, at least in part, by structural changes in the heart caused by CKD. The prevalence of left ventricular hypertrophy is particularly high among patients with CKD.12 ‘Uremic cardiomyopathy,’ a condition seen in patients with advanced CKD, includes left ventricular hypertrophy, dilation, and systolic dysfunction.13–15 Other ultrastructural abnormalities have been observed in advanced CKD patients. A decreased GFR has been proposed to cause endocardial as well as diffuse myocardial fibrosis that could enhance the risk of life-threatening ventricular arrhythmias and SCD.15 These cardiac morphological changes could be the primary mediators of the kidney-associated risk of SCD.12–14 Alternatively, patients with CKD tend to be less likely to have cardiac interventions,16 and this practice may play a role in the observed excess SCD risk. In this study, we found that the relationship between GFR and risk of SCD persisted even after accounting for medication use at the time of catheterization and revascularization procedures after catheterization.
The risk of SCD in patients with CKD could also be mediated by dynamic metabolic and physiological changes that are known to be present. These changes include, but are not limited to (1) the metabolic derangements of a uremic milieu such as hyperkalemia, metabolic acidosis, anemia, and secondary hyperparathyroidism (Coresh et al.17 and Foley and Wang18); (2) electrophysiological abnormalities such as triggered automaticity and ventricular repolarization abnormalities(Meier et al.19); (3) transient functional changes that result from volume overload; and (4) a generalized micro-inflammatory state characterized by hypoalbuminemia, elevated homocysteine, and higher levels of serum inflammatory markers, which may contribute to arrhythmogenesis.20 Once CKD progresses to ESRD, hemodynamic rigors and biochemical shifts associated with conventional renal replacement therapies such as hemodialysis could trigger additional SCDs. Indeed, this study suggests that an additive risk is conferred by dialytic therapy because the SCD rate for dialysis patients far exceeded the SCD rate of patients with an eGFR <15 but not yet on dialysis (Figure 2). However, this study clearly indicates that the risk of sudden death is high in CKD patients long before they ever develop ESRD.
This study has several important strengths. The cohort of patients is large, and patients are well characterized. The demographics of the study group, namely 66% males, 23% non-Caucasian, 29% diabetic, resemble those of the CKD population in the United States.21 Unlike other reports, this study examines associations among earlier stages of CKD. In addition, the causes of death were adjudicated by two blinded clinicians based on first-hand interviews with observers and medical chart reviews.
Our study has several limitations. First, only patients with known, significant CAD were included; hence, we cannot completely exclude the possibility that a different relationship may exist in among patients without significant CAD. Second, we used serum creatinine at the time of catheterization and the Modification of Diet in Renal Disease (MDRD) equation to estimate GFR. Given the often progressive nature of CKD, some of the SCD events may have occurred at later stages of CKD or during renal replacement therapy. In addition, estimating equations using serum creatinine are known to be imperfect, and the study population examined here differs substantially from the original MDRD study population of nonhospitalized, mostly non-diabetic, Caucasian patients. Therefore, we cannot exclude the possibility that patients were improperly categorized due to errors in GFR estimates.22 In particular, the MDRD equation is known to be less accurate in populations with normal or near-normal GFR.23 Third, because our cohort included only patients who underwent a cardiac catheterization, patients with more advanced CKD were underrepresented in the database most likely because of concerns regarding the effect of contrast dye on renal function. Fourth, although our analysis accounted for important post-catheterization therapies such as revascularization procedures, we did not ascertain other therapies (such as medications) that may have been instituted later and may have affected SCD risk. However, the goal of this analysis was to address the risk of SCD among patients with baseline CKD, and future studies should explore how this risk relates to the use of available medical therapies. Finally, as with all retrospective studies, unforeseen and unmeasured confounders could have resulted in bias. In particular, 24% of the study cohort had missing data on ejection fraction, an important predictor of SCD risk, which is routinely measured during catheterization by ventriculogram, but was likely not performed in advanced CKD patients because of concerns for contrast nephropathy. Nevertheless, after supplementing missing data with ejection fraction reported from concurrent echocardiograms, the median ejection fraction did not differ by more than 5% between any group, which is within the expected inter-observer variability for ejection fraction measured by echocardiogram and therefore unlikely to have significantly affected the study results.24 However, we had detailed information regarding other important covariates including severity of CAD, clinical diagnosis of CHF, and early post-catheterization revascularization, and we excluded patients with major potential confounders such as the use of an implantable automated defibrillator and antiarrhythmic medications.
We conclude from this study that diminished kidney function carries a strong, independent, and incremental risk for SCD in patients with underlying CAD. Efforts to reduce progression of kidney disease should be prioritized in order to reduce the accompanying risk of cardiovascular death. Studies are required to better characterize the mechanisms through which CKD increases the risk of SCD.
MATERIALS AND METHODS
Description of data source
Patients for this retrospective cohort study were identified using the DDCD. This database compiles data on the clinical course of all patients who undergo a cardiac catheterization, an interventional cardiac procedure, or a coronary artery bypass surgery at Duke University Medical Center. Patient information that is prospectively collected by this database includes symptoms at the time of cardiac procedures, co-morbidities, primary diagnoses, medications, and cardiac procedure results, including severity of CAD and measures of left ventricular function.25 In patients with clinically significant CAD (defined as having at least one vessel with stenosis ≥75%), the DDCD routinely collects follow-up data on mortality, cardiovascular events, hospitalizations, and medications using mailed questionnaires at 6 months, 1 year, and annually thereafter. Patients who do not respond to the mailed questionnaire are then surveyed by phone. Patients not successfully contacted through the aforementioned mechanisms have their vital status determined through a search of the National Death Index (NDI). The institutional human subjects review committee reviewed and approved the study.
Participants and study design
Our study cohort consisted of consecutive patients with clinically significant CAD who were enrolled in the database from 1 January 1995 to 30 June 2006. Patients with a serum creatinine measurement within 30 days preceding the day of catheterization who had long-term follow-up were included in this analysis. Only patients with stable serum creatinine undergo elective catheterization, and patients are maximally hydrated before the procedure according to the standard of care at our institution. All laboratory testing was performed at a single institution’s core laboratories. Serum creatinine was determined using the enzymatic Jaffé method. Patients were excluded from the study cohort if the cardiac catheterization was performed to evaluate congenital or pericardial disease, hypertrophic cardiomyopathy, or for assessment before organ transplantation. As the focus of our analysis was to study the independent effect of reduced GFR on SCD risk, we also chose to exclude patients with a prior history of arrhythmia and those receiving antiarrhythmic therapy including an implantable cardioverter defibrillator at the time of catheterization. Other specific exclusion criteria are shown in Figure 1.
The eGFR at baseline was estimated for all patients using the modified MDRD equation26 (186 (serum creatinine in mg per 100 ml)−1.154 (age in years)−0.203 × 0.742 for females × 1.21 for black race) and the last recorded serum creatinine before cardiac catheterization. Study patients were allocated to one of three groups based on the estimated pre-cardiac catheterization eGFR: (1) eGFR ≥60, (2) eGFR 15–59, and (3) eGFR < 15 or receiving dialysis therapy. For analyses using eGFR as a continuous variable, patients on dialysis were assigned the median eGFR value of the rest of the non-dialysis subjects in the GFR < 15 group. eGFR was expressed as ml/min per 1.73 m2.
Primary end point
The primary end point of this analysis is SCD. In patients with significant CAD, data on cause of death are collected through mailed questionnaires or during phone surveys of surviving family members. Cause of death is further verified using available hospital records, death certificates, and query of the NDI. For this study, SCD was defined as a composite of the following: (1) sudden death defined as death from cardiac or unknown causes that occurs instantaneously or within 60 min of the onset of symptoms; (2) post-resuscitation death includes patients who meet the criteria for sudden death and are temporarily resuscitated but subsequently die more than 60 min from the onset of symptoms leading to the arrest; and (3) unobserved death is defined as death occurring in patients last seen alive more than 60 min before the discovery of death and the circumstances directly leading to the death are unknown. Deaths coded as SCD on the death certificate or the NDI without other supporting evidence regarding the circumstances of death were not considered SCD in this study. Two independent reviewers adjudicated all deaths.
Statistical analysis
Baseline characteristics were compared using the Kruskal–Wallis test and Wilcoxon rank-sum test for continuous variables and the Pearson χ2-test for categorical variables. The log-rank test was used to compare unadjusted SCD rates across eGFR groups. Patients were censored for any of the following: alive at the end of observation period (28 February 2008), lost to follow-up, and death not due to SCD. Unadjusted and adjusted results were examined using Cox proportional hazards modeling.27 Unadjusted hazard ratios for SCD were calculated using the group with an eGFR ≥60 ml/min as the reference group. Model variables were selected according to three criteria: statistical strength of association with the outcome (unadjusted association P<0.1), prior studies, and clinical insight regarding factors likely to contribute to adverse outcomes. Candidate variables included age, race, gender, severity of CHF, severity of CAD, diabetes mellitus, history of smoking, peripheral vascular disease, cerebrovascular disease, history of hypertension, valvular heart disease, history of prior revascularization with CABG or percutaneous intervention, body mass index, blood pressure and pulse at the time of catheterization, history of myocardial infarction, and in-hospital medications. The regression assumption of linearity in the Cox proportional hazards model was explicitly tested for both continuous and ordinal variables, and transformations were made as appropriate. Variables were added in a forward stepwise approach. We conducted a sensitivity analysis that only included witnessed sudden death as the end point (excluding unobserved death).
Patients were assigned to percutaneous intervention or CABG treatment groups, respectively, if they underwent these procedures within 30 days of the initial cardiac catheterization. Patients who did not undergo revascularization within 30 days were designated in the medical group. Patients who died within 5 days of the initial catheterization without revascularization (the median time to percutaneous intervention or CABG at Duke) were excluded from the analysis to avoid attributing early deaths to the medically treated cohort. In addition, because revascularization was not randomly assigned, we adjusted for propensity to select revascularization as a treatment option. From this analysis, we created a ‘propensity score’ for each patient representing that patient’s probability of selection for the treatment being modeled.28 Clinical information generally available to a clinician were used as candidate variables in developing the propensity model. These propensity scores were used as covariates in the final survival model.
All tests were two-sided and were carried out using SAS 8.2 (SAS Institute, Cary, NC, USA). The results were declared significant at a P-value of < 0.05.
Acknowledgments
This work was presented at the American Society of Nephrology Annual Meeting in November 2008. Dr Pun is supported by a National Institutes of Health Grant no. 1KL2-RR-024127-01
Footnotes
DISCLOSURE
All the authors declared no competing interests.
References
- 1.Coresh J, Selvin E, Stevens LA, et al. Prevalence of chronic kidney disease in the United States. JAMA. 2007;298:2038–2047. doi: 10.1001/jama.298.17.2038. [DOI] [PubMed] [Google Scholar]
- 2.National Institutes of Health. National Institute of Diabetes and Digestive and Kidney Diseases. National Institutes of Health; Bethesda: 2005. USRDS Annual Data Report. [Google Scholar]
- 3.Go AS, Chertow GM, Fan D, et al. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351:1296–1305. doi: 10.1056/NEJMoa041031. [DOI] [PubMed] [Google Scholar]
- 4.Anavekar NS, McMurray JJ, Velazquez EJ, et al. Relation between renal dysfunction and cardiovascular outcomes after myocardial infarction. N Engl J Med. 2004;351:1285–1295. doi: 10.1056/NEJMoa041365. [DOI] [PubMed] [Google Scholar]
- 5.Herzog CA. Sudden cardiac death and acute myocardial infarction in dialysis patients: perspectives of a cardiologist. Semin Nephrol. 2005;25:363–366. doi: 10.1016/j.semnephrol.2005.05.003. [DOI] [PubMed] [Google Scholar]
- 6.Huikuri HV, Castellanos A, Myerburg RJ. Sudden death due to cardiac arrhythmias. N Engl J Med. 2001;345:1473–1482. doi: 10.1056/NEJMra000650. [DOI] [PubMed] [Google Scholar]
- 7.Chonchol M, Goldenberg I, Moss AJ, et al. Risk factors for sudden cardiac death in patients with chronic renal insufficiency and left ventricular dysfunction. Am J Nephrol. 2007;27:7–14. doi: 10.1159/000098431. [DOI] [PubMed] [Google Scholar]
- 8.Goldenberg I, Moss AJ, McNitt S, et al. Relations among renal function, risk of sudden cardiac death, and benefit of the implanted cardiac defibrillator in patients with ischemic left ventricular dysfunction. Am J Cardiol. 2006;98:485–490. doi: 10.1016/j.amjcard.2006.03.025. [DOI] [PubMed] [Google Scholar]
- 9.Deo R, Lin F, Vittinghoff E, et al. Kidney dysfunction and sudden cardiac death among women with coronary heart disease. Hypertension. 2008 doi: 10.1161/HYPERTENSIONAHA.107.103804. [DOI] [PubMed] [Google Scholar]
- 10.Zipes DP, Wellens HJ. Sudden cardiac death. Circulation. 1998;98:2334–2351. doi: 10.1161/01.cir.98.21.2334. [DOI] [PubMed] [Google Scholar]
- 11.Rea TD, Pearce RM, Raghunathan TE, et al. Incidence of out-of-hospital cardiac arrest. Am J Cardiol. 2004;93:1455–1460. doi: 10.1016/j.amjcard.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 12.Stewart GA, Gansevoort RT, Mark PB, et al. Electrocardiographic abnormalities and uremic cardiomyopathy. Kidney Int. 2005;67:217–226. doi: 10.1111/j.1523-1755.2005.00072.x. [DOI] [PubMed] [Google Scholar]
- 13.Ritz E, McClellan WM. Overview: increased cardiovascular risk in patients with minor renal dysfunction: an emerging issue with far-reaching consequences. J Am Soc Nephrol. 2004;15:513–516. doi: 10.1097/01.asn.0000115398.92270.30. [DOI] [PubMed] [Google Scholar]
- 14.Ritz E, Wanner C. The challenge of sudden death in dialysis patients. Clin J Am Soc Nephrol. 2008;3:920–929. doi: 10.2215/CJN.04571007. [DOI] [PubMed] [Google Scholar]
- 15.Mark PB, Johnston N, Groenning BA, et al. Redefinition of uremic cardiomyopathy by contrast-enhanced cardiac magnetic resonance imaging. Kidney Int. 2006;69:1839–1845. doi: 10.1038/sj.ki.5000249. [DOI] [PubMed] [Google Scholar]
- 16.Shlipak MG, Heidenreich PA, Noguchi H, et al. Association of renal insufficiency with treatment and outcomes after myocardial infarction in elderly patients. Ann Intern Med. 2002;137:555–562. doi: 10.7326/0003-4819-137-7-200210010-00006. [DOI] [PubMed] [Google Scholar]
- 17.Coresh J, Astor BC, Greene T, et al. Prevalence of chronic kidney disease and decreased kidney function in the adult US population: Third National Health and Nutrition Examination Survey. Am J Kidney Dis. 2003;41:1–12. doi: 10.1053/ajkd.2003.50007. [DOI] [PubMed] [Google Scholar]
- 18.Foley RN, Wang C, Collins AJ. Cardiovascular risk factor profiles and kidney function stage in the US general population: the NHANES III study. Mayo Clin Proc. 2005;80:1270–1277. doi: 10.4065/80.10.1270. [DOI] [PubMed] [Google Scholar]
- 19.Meier P, Vogt P, Blanc E. Ventricular arrhythmias and sudden cardiac death in end-stage renal disease patients on chronic hemodialysis. Nephron. 2001;87:199–214. doi: 10.1159/000045917. [DOI] [PubMed] [Google Scholar]
- 20.Manjunath G, Tighiouart H, Ibrahim H, et al. Level of kidney function as a risk factor for atherosclerotic cardiovascular outcomes in the community. J Am Coll Cardiol. 2003;41:47–55. doi: 10.1016/s0735-1097(02)02663-3. [DOI] [PubMed] [Google Scholar]
- 21.Whaley-Connell AT, Sowers JR, Stevens LA, et al. CKD in the United States: Kidney Early Evaluation Program (KEEP) and National Health and Nutrition Examination Survey (NHANES) 1999–2004. Am J Kidney Dis. 2008;51 :S13–S20. doi: 10.1053/j.ajkd.2007.12.016. [DOI] [PubMed] [Google Scholar]
- 22.Rule AD, Larson TS, Bergstralh EJ, et al. Using serum creatinine to estimate glomerular filtration rate: accuracy in good health and in chronic kidney disease. Ann Intern Med. 2004;141:929–937. doi: 10.7326/0003-4819-141-12-200412210-00009. [DOI] [PubMed] [Google Scholar]
- 23.Poggio ED, Wang X, Greene T, et al. Performance of the modification of diet in renal disease and Cockcroft–Gault equations in the estimation of GFR in health and in chronic kidney disease. J Am Soc Nephrol. 2005;16:459–466. doi: 10.1681/ASN.2004060447. [DOI] [PubMed] [Google Scholar]
- 24.Otterstad JE, Froeland G, St John Sutton M, et al. Accuracy and reproducibility of biplane two-dimensional echocardiographic measurements of left ventricular dimensions and function. Eur Heart J. 1997;18:507–513. doi: 10.1093/oxfordjournals.eurheartj.a015273. [DOI] [PubMed] [Google Scholar]
- 25.Reddan DN, Szczech LA, Tuttle RH, et al. Chronic kidney disease, mortality, and treatment strategies among patients with clinically significant coronary artery disease. J Am Soc Nephrol. 2003;14:2373–2380. doi: 10.1097/01.asn.0000083900.92829.f5. [DOI] [PubMed] [Google Scholar]
- 26.Levey AS, Bosch JP, Lewis JB, et al. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999;130:461–470. doi: 10.7326/0003-4819-130-6-199903160-00002. [DOI] [PubMed] [Google Scholar]
- 27.Cox D, Oaks D. Analysis of Survival Data. Chapman and Hall; London: 1984. [Google Scholar]
- 28.Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55. [Google Scholar]